Abstract
MITF is a known gene underlying autosomal dominant hearing loss, Waardenburg syndrome (WS). Biallelic MITF mutations have been found associated with a rare hearing loss syndrome consisting eye abnormalities and albinism; and a more severe type of WS whose heterozygous parents were affected with classic WS in both cases. The aims of this study were to identify a new candidate gene causing autosomal recessive nonsyndromic hearing loss (ARNSHL) and confirm its causation by finding additional families affected with the candidate gene and supporting evidences from functional analyses. By using whole exome sequencing, we identified a homozygous c.1022G>A: p.Arg341His variant of MITF, which co-segregated with the hearing loss in five affected children of a consanguineous hearing couple. Targeted exome sequencing in a cohort of 130 NSHL individuals, using our in-house gene panel revealed a second family with c.1021C>T: p.Arg341Cys MITF variant. Functional studies confirmed that the Arg341His and Arg341Cys alleles yielded a normal sized MITF protein, with aberrant cytosolic localization as supported by the molecular model and the reporter assay. In conclusion, we demonstrate MITF as a new cause of ARNSHL, with heterozygous individuals free of symptoms. MITF should be included in clinical testing for NSHL, though it is rare.
Subject terms: Molecular biology, Molecular medicine, Genetics, Genotype, Mutation, Sequencing
Introduction
Congenital hearing loss is a prevalent disorder found in 1–2 per 1,000 live births, with more than half of the cases caused by genetic abnormalities1,2. Nonsyndromic sensorineural hearing loss (NSHL) accounts for 70% of genetic sensorineural hearing loss (HL), with only 30% being genetic syndromes1–3. Common syndromic sensorineural HL (SSHL) includes Usher syndrome, Waardenburg syndrome, and Pendred syndrome2,3.
Over 119 nuclear genes are associated with NSHL2,3. Seventy six of these genes contribute to autosomal recessive NSHL (ARNSHL), whereas variants in 47 and 5 genes underlie autosomal dominant NSHL (ADNSHL) and X-linked NSHL, respectively2,3. Variants in some genes can result in both syndromic and nonsyndromic, and both autosomal dominant and autosomal recessive sensorineural HL. Most families with ARNSHL have severe congenital onset, a negative family history of hearing loss, and consanguinity1,2. The most prevalent genetic causes of ARNSHL are GJB2 and SLC26A4 variants, accounting for 20% of congenital hearing loss, followed by variants in MYO15A, OTOF, CDH23, and TMC11–3. Many variants in mtDNA are also shown to cause maternally-inherited NSHL. Digenic inheritance in NSHL is not prevalent, with the most evident example being mutations in GJB2 and GJB64. Genetic diagnosis of NSHL is a challenging task because of its high genetic heterogeneity.
Next generation sequencing (NGS) is a powerful tool for the identification of new disease-causing gene(s), especially in small pedigrees and sporadic cases. Many studies using targeted exome sequencing have reported various diagnostic rates for hereditary hearing loss based on different populations and approaches with overall diagnostic rate approximately 40%5–9. However, given its high heterogeneity, the number of new disease-causing gene variants for NSHL continues to grow.
The human microphthalmia-associated transcription factor (MITF) gene is a major regulator of melanocyte development, differentiation, and cell survival10. Heterozygous MITF mutations cause Waardenburg syndrome, type 2A (WS2A) and Tietz (or Tietz albinism-deafness) syndrome, with autosomal dominant inheritance10. WS2A patients exhibit congenital deafness, blue iris, patchy depigmentation of the skin and eyes (white foelock and heterochromia iridis), but no dystopia canthorum10. Patients with Tietz syndrome have congenital sensorineural HL, blue iris without heterochromia iridis, and skin and hair color lighter than those of their relatives10.
In this study, we aimed to identify a new candidate gene causing ARNSHL and confirm its causation by finding additional families associated with this gene using our in-house targeted exome sequencing in a cohort of 130 individuals affected with NSHL. We also performed multiple functional analyses to find supporting evidences. We demonstrate MITF as the cause of ARNSHL, with heterozygous individuals free of symptoms, as supported by findings of two families and evidences from functional characterization. Our data also suggest that MITF is a rare cause of ARNSHL.
Results
Clinical phenotypes of Family-1 and clinical exome data
Family-1 consisted of a consanguineous hearing couple, five deaf and two normal hearing children. Affected individuals IV-1, IV-2, IV-4 and IV-5 were found to have deaf-mutism (Fig. 1a). They were normal on physical examination of color of hair, iris and skin; inner canthal distances; thyroid glands; visual acuity as screened by the Snellen chart; and visual field confrontation using a simple Donders’ test. There was no known history of recurrent syncope, thyroid, cardiac, or kidney problems. None had auditory rehabilitation. Complete blood counts, thyroid function tests, blood urea nitrogen and creatinine levels, and urinalysis all showed normal results. Individual IV-1 refused to have blood taken.
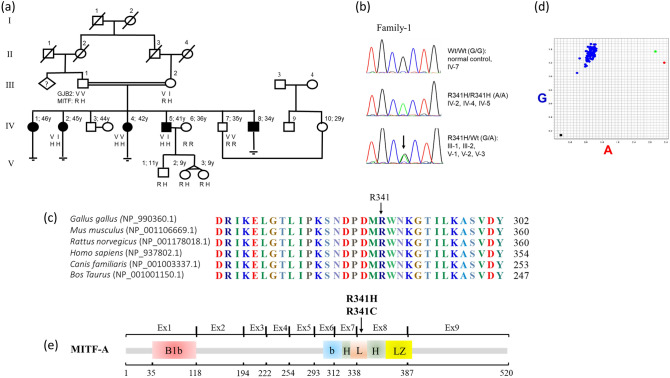
Figure 1.
Family-1 and Arg341His. (a) Pedigree showing consanguinity between individual III-1 and III-2. Black-filled squares and circles indicate hearing impaired males and females, respectively. (b) Chromatogram displaying wild-type (GG), homozygous (AA), and heterozygous (GA) at nt 1,022, with the homozygous variants co-segregating with hearing loss phenotype. (c) Protein sequence alignment of vertebrate MITF; noted the highly conserved Arg341 residue across various species. (d) Allelic discrimination plot obtained from real-time PCR using TaqMan SNP genotyping of MITF c.1022G/A. The allelogram showing the blue, green, and red dots representing specimens with GG, GA, and AA genotypes, in orderly; and the black square (left lower corner) denoting a blank control. The GA- and AA-positive specimens were from carrier and affected individuals of Family-1, respectively. Among 228 control individuals screened, only the wild-type GG genotype was found. (e) Arg341His/Cys is located in the loop segment of the basic helix-loop-helix (bHLH) domain of MITF-A.
Dilated fundal examination, an audiological study, and a temporal bone CT scan were declined by the affected individuals. Both parents were normal on physical examination and blood and urine tests were normal. They reported no substantial health problem or premature greying of hair. Based on this data, we concluded that this family represents profound congenital NSHL inherited in an autosomal recessive manner.
Targeted exome analysis using a commercially available gene panel (70 genes; OtoGenome) revealed heterozygous p.Val37Ile GJB2 mutation in the affected individual IV-5. This analysis confirmed our previous finding and supported the exclusion of GJB2 and the other genes in the panel as the cause of NSHL in this family. We therefore aimed to identify a new candidate gene.
Whole exome sequencing (WES) data of Family-1
Specimens from affected individuals (IV-2, IV-4 and IV-5) and an unaffected sib (IV-7) were chosen for WES. We first filtered for homozygous variants in each patient and for heterozygous variants in the unaffected sib. Variants on chromosomes X and Y; synonymous SNVs; likely non-disease-causing variants (intronic, intergenic, 3′-UTR, 5′-UTR, downstream, upstream and in ncRNA), and common variants present in the 1000Genome database with allele frequency > 0.03 were discarded (Table 1). These steps left 36, 43, and 31 homozygous insertion, deletion, and exonic and splicing variants in affected individuals IV-2, IV-4, and IV-5, respectively. Among these, only 28 variants were shared by all three affected sibs. Twenty-seven out of 28 genes were also present in the homozygous state in the unaffected sib, excluding them as being the causative gene. The single variant that remained and that was absent in the unaffected sib was a novel MITF allele, c.1022G>A: p.Arg341His in exon 9 of MITF-isoform A (NM_198159.2), corresponding to c.719G>A: p.Arg240His in exon 8 of MITF-isoform M (NM_000248.1).
Table 1.
Number of variants remaining after stepwise filtering.
| Filtering criteria | Number of variants remaining | |||
|---|---|---|---|---|
| IV-2 | IV-4 | IV-5 | IV-7 | |
| Total variants | 73,535 | 71,858 | 72,274 | 72,620 |
| Homozygous variants only | 35,173 | 34,222 | 35,563 | NA |
| Heterozygous variants only | NA | NA | NA | 37,401 |
| After excluding variants on chromosome X and Y | 34,424 | 33,481 | 34,617 | 37,318 |
| After excluding synonymous SNVs | 29,963 | 28,992 | 30,053 | 31,816 |
| Insertion/deletion, exonic, splicing onlya | 4,277 | 4,195 | 4,397 | 5,316 |
| After excluding variants in 1000Genome with AF > 0.03b | 36 | 43 | 31 | 119 |
| Homozygous variants shared among affected persons | 28c | 28 | 28 | NA |
| Homozygous variants shared among affected persons, but heterozygous/wild-typed in the hearing subject | 1 | 1 | 1 | NA |
AF allele frequency, NA not applicable.
aExcluding intronic, intergenic, 3′-UTR, 5′-UTR, downstream, upstream and ncRNA.
bAs of Oct 2011.
c27 genes shared by all three affected but not shared with the unaffected sib include ATXN1, CDCP2, FOXI3, KIF1A, CCDC66, DCP1A, EOMES, SEMA3B, FBXL21, SRA1, MAP3K4, TBP, MAFA, PRUNE2, EFEMP2, MAML2, TMEM132A, PLBD1, IFI27, RIN3, OTUD7A, PCSK6, BPTF, COPZ2, KCNC3, RALY, PRDM15.
Phen-Gen analysis indicated MITF as the most probable candidate gene as it had the highest damaging score of 0.0885690996, while the genes ranking 2–17 had far lower damaging scores, ranging from 0.0055963440 to 0.0000022778 (Supplementary Table S2).
Moreover, the analysis of 144 known hearing loss genes in each individual WES data using compound heterozygosity model was also carried out. The analyses led to an identification of 16 variants in 15 genes. Among these variants, only three were pathogenic or likely pathogenic according to the 2015 American College of Medical Genetics (ACMG) guideline for variant classification11. These included heterozygous p.Val37Ile of GJB2 in two affected individuals; heterozygous p.Pro1791Arg of TECTA in one deaf individual; and p.Arg341His of MITF gene in all three affected persons. Compound heterozygosity or homozygosity of pathogenic/likely pathogenic mutations other than of the MITF variants was not found (Supplementary Table S1). In addition, we checked the exome data for potential missing call/segment, by using IGV and did not identify lost alleles (Supplementary Figure S1).
Homozygous Arg341His co-segregated with hearing loss phenotype in Family-1
Sequencing of additional family-1 members confirmed the affected individuals to be homozygous for MITF Arg341His, both parents to be heterozygous for MITF Arg341His, and hearing relatives to be wild-type or heterozygous for MITF Arg341His (Fig. 1b). These data further support the hypothesis of autosomal recessive inheritance of HL in this family. Bioinformatic analysis indicated a likely pathogenic property of p.Arg341His, with a SIFT score of 0.00, a PolyPhen score of 1.00, a MutationTaster score of 0.99+, and no splicing defect (splice score 0.99).
Alignment of multiple vertebrate protein sequences (chicken, mouse, rat, human, dog, and cow) using Clustal Omega Software (https://www.ebi.ac.uk/Tools/msa/clustalo) revealed high conservation of residue 341Arg (Fig. 1c). p.Arg341His was not present in 756 control chromosomes of the in-house WES database, as screened by TaqMan assays (Fig. 1d). This variant is located in the loop segment (aa 332–346 isoform MITF-A) of the basic helix-loop-helix (bHLH) domain of MITF (Fig. 1e)12.
Additional family and Arg341Cys MITF mutation
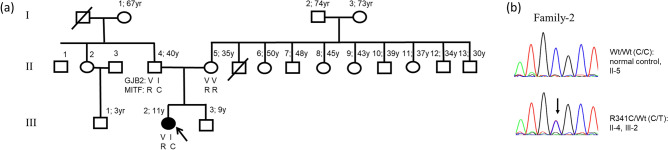
By screening 130 individuals affected with NSHL using our in-house targeted exome sequencing, it revealed another family (Family-2) with a sporadic patient who had a heterozygous MITF mutation, c.1021C>T: p.Arg341Cys of isoform MITF-A, and a heterozygous GJB2 mutation, c.109G>A: p.Val37Ile (Fig. 2). The patient (individual III-3), an 11-year-old girl, had normal colored iris and fine, sparse and reddish-brown hair. The remaining physical examinations were normal. The patient was noted to have profound (110 dB) sensorineural hearing loss at age 9 months and received a cochlear implant at the age of 3 years. Blood and urine tests indicated normal kidney and thyroid functions. A temporal bone CT scan was normal. Both parents appeared normal and reported no pigmentation abnormality in either side of the family. WS and Teitz syndrome were unlikely because there was no blue iris or patchy depigmentation in either the patient or the father. In addition, fine and sparse hair is not a feature of either syndrome. We, therefore, concluded that this patient had NSHL.
Figure 2.
Family-2 and Arg341Cys. (a) Pedigree, black-filled circle indicates hearing impaired female, respectively. (b) Sanger sequences showing wild-type and heterozygous C to T at nt1021; and the heterozygous variant found in the patient and father only.
The in silico analysis indicated likely pathogenicity of p.Arg341Cys with no effect on splicing (SIFT score 0.00; PolyPhen score 1.00; MutationTaster score 0.99+; and splice score 0.99). This variant was not present in our control WES database.
To identify other MITF or GJB2 mutations possibly missed by the gene panel testing, we performed PCR-Sanger sequencing of all ten MITF and two GJB2 exons in the patient and both parents (Supplementary Tables S3 and S4). The results confirmed that the patient and her father were double heterozygous for MITF-Arg341His and GJB2-Val37Ile, while the mother carried no mutation. Moreover, the copy number variation (CNV) analysis performed in the affected individual of Family-2 did not reveal microdeletion/duplication of chromosomal segment involving the MITF gene. Additionally, PCR-sequencing of the TYR gene was performed and revealed no pathogenic variant (Supplementary Table S5).
Functional consequence of the Arg341His and Arg341Cys MITF mutations
After MITF was revealed as a new candidate, we performed reporter, Western blot, and immunofluorescence assays to investigate the functional consequences of the identified variants, using melanoma (G361) and mouse embryonic fibroblast (NIH/3T3) cells.
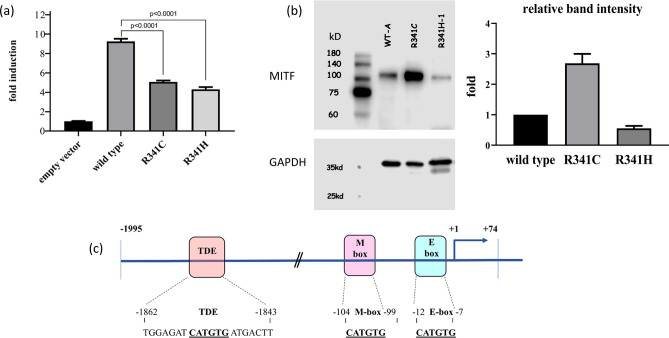
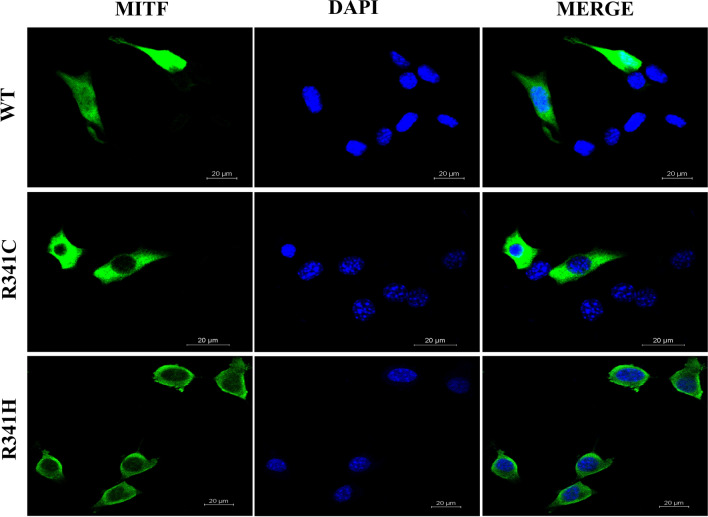
Overexpression of Arg341His and Arg341Cys induced TYR promotor activity to only 46% and 54% of the wild-type expression level, respectively (Fig. 3a). Western blotting revealed normal sized Arg341His and Arg341Cys MITF proteins but a significantly increased amount of the Arg341Cys protein was expressed and a slightly decreased quantity of the Arg341His variant was expressed compared with wild-type MITF (Fig. 3b and Supplementary Figure S2). An immunofluorescence study indicated that both Arg341His and Arg341Cys MITF were localized solely in the cytoplasm compared with nuclear localization of wild-type MITF (Fig. 4).
Figure 3.
Reporter assay and western blot analysis (a) The basal luciferase level of the empty vector was 32. Overexpression of wild-type MITF induced TYR promoter activity by up to 9.4-fold (300/32), R341C at 5.1-fold (164/32 or 54%), and R341H at 4.3-fold (139/32 or 46%), respectively, (p < 0.0001 by one-way ANOVA). (b) Western blot analysis. Left panel: upper image demonstrating the blot of MITF, from left to right, molecular size marker; wildtype MITF-isoform A, R341C, and R341H variants (labeled as R341H-1), the wild-type, R341C and R341H protein with normal predicted size. Lower image of the left panel showing the blot of GAPDH used as a loading control for normalization for wildtype MITF and each variant. Noted almost equivalent amount of the GAPDH in all lanes. Detail of GAPDH staining was described in the Supplementary Figure S1. Brightness and contrast of the upper and lower images were not modified from its original appearances The right panel denoting a greater amount of the R341C protein and a decreased quantity of the R341H protein expressed, compared with the wild type [p-value 0.0011 and 0.0898, respectively, using ANOVA with post hoc (Tukey) test]. The relative level of band intensity of wild-type MITF was set as 1. (c) Diagram showing the Luc-reporter constructs, with putative MITF binding sites shown as a filled box (Tyrosinase distal enhancer or TDE, M-box, E-box).
Figure 4.
Subcellular localization of wild-type and mutant MITF proteins. The studied proteins are in green (left panel), DAPI-stained nuclei are shown in blue (middle panel), and the merged images are shown on the right panel. Note the nuclear localization of the wild-type MITF and the exclusively cytosolic localization of the R341C (Arg341Cys) and R341H (Arg341His) variants.
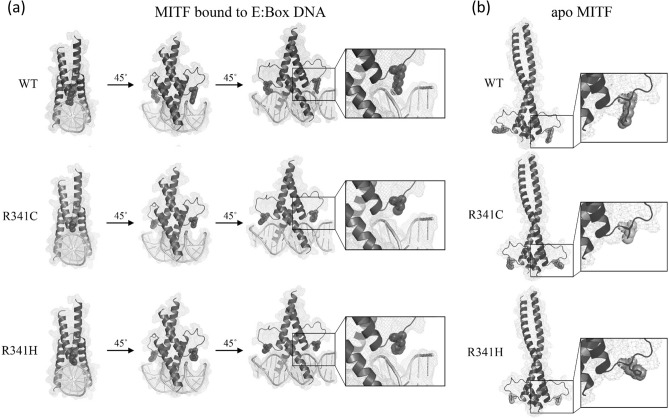
Molecular model of Arg341His and Arg341Cys
The potential effect of substitutions at Arg341 was examined using homology models for MITF bound to the E-Box DNA element as well as the apo form. This analysis indicated that Arg341 (MITF-A isoform) is not present at the dimer interface in either the apo or DNA bound forms (Fig. 5). Instead, Arg341 is located near the DNA binding domain and makes contacts with the E-Box DNA element. The corresponding residue in MITF-M, Arg240, has been reported to not make base specific contacts but interacts with the phosphate backbone on the E-Box element10. The Arg341Cys and Arg341His substitutions abrogate this contact between MITF and the DNA. Thus, mutation of Arg341 may reduce the binding affinity of MITF to this DNA element, although the impact of loss of the Arg341 contact with the sugar-phosphate backbone is unknown.
Figure 5.
Molecular modelling of wild-type, Arg341Cys, and Arg341His MITF. Homology models of wild-type, Arg341Cys, and Arg341His MITF constructed using Mus musculus MITF:E-box complex (4atk) and apo MITF (4ath) as templates. The Arg341 residues, as well as Cys and His substitutions, are shown with space-filled visualizations. (a) The model of MITF bound to DNA contains residues 308–369. The three views are 45° rotations of the model. The boxed region is magnified to show DNA interaction details of Arg341 and the loss of these contacts in the Arg341Cys and Arg341His mutants. (b) The model of apo MITF contains residues 318–396. One view is shown with the region surrounding residue 341 magnified. SWISS-MODEL was used to generate the structural models of wild-type and mutant MITF proteins which then were viewed using the PyMOL Molecular Graphics System, version 2.0.6 (https://pymol.org/2/).
Discussion
We demonstrated MITF to be a new causative gene for ARNSHL based on the following evidence: (1) other known genes were excluded; (2) MITF variants were a recurrent phenomenon in multiple affected families; (3) cosegregation of the homozygous variants with hearing loss, in the absence of homozygous mutations in hearing relatives and a control population; (4) deleterious effects of the mutations, as shown by in silico analysis and molecular modeling, disrupted expression of a downstream gene, and aberrant subcellular localization; and (5) the known roles of MITF in cochlear melanocytes. Two MITF mutations were identified: p.Arg341His and p.Arg341Cys.
Only four individuals from Family-1 were selected for WES. The following selection strategies were considered: (A) two affected sibs and both parents; (B) two affected sibs and one unaffected sib and one parent; and (C) three affected sibs and one unaffected sib. For option A, the chance of two affected sibs sharing any homozygous variant while both parents were heterozygous was 6.25% or 1/16 (1/4 × 1/4 × 1 × 1), regardless of the variants being benign or pathogenic. For option B, the chance of two affected sibs sharing a homozygous variant whilst the parent being a carrier and the unaffected sib not harboring the homozygous variant was 4.69% or 3/64 (1/4 × 1/4 × 1 × 3/4). For option C, the probability of three affected sibs sharing a homozygous variant while the unaffected sib carrying a heterozygous or wild-type sequence was 1.17% or 3/256 (1/4 × 1/4 × 1/4 × 3/4). Therefore, we chose option C, which provided the lowest chance of a false candidate.
In Family-1, besides MITF, none of the genes detected by Phen-Gen overlapped with those filtered by manual analysis. By using Phen-Gen, we can avoid human error when filtering the data of each individual before segregation analysis. Phen-Gen has a 52% advantage over a genotype-only approach13.
Hearing impaired individuals in family-2 is likely having recessive mutations on both alleles of the MITF gene, p.Arg341Cys inherited from the father and another yet unidentified pathogenic allele which could be inherited from the mother or a de novo variant. Based on this assumption and the result of DNA binding activity of the p.R341C, it supports that family-2 also fits with the autosomal recessive model.
Human MITF binds DNA as a homodimer and as a heterodimer with the TEE family of bHLHZip transcription factors10. Over 77 MITF mutations have been reported to cause WS2A and Teitz syndrome (HGMD https://protal.biobase) with around 50% being missense variants. Truncating and splice site MITF mutations occur throughout the gene while missense and in-frame mutations were more confined to exons 8 and 9 of MITF-A isoform (or exons 7 and 8 for MITF-M)14. Functional analysis data of MITF variants are limited. A recent study showed that missense (p.Arg217Ile) mutations of MITF resulted in WS2A through a dominant negative effect, whereas a frameshift mutation c.575delC (p.Thr192LysfsTer20) showed a haploinsufficiency mechanism15.
The significant reduction of downstream TYR gene expression caused by Arg341His and Arg341Cys supported the pathogenic nature of these MITF variants (Fig. 3a). The normal molecular weight of the Arg341His/Cys MITF variants confirmed no protein truncation associated with these changes. We could not explain why and how the Arg341Cys led to increased protein expression of the mutant allele.
The Arg341 residue is present on the exterior of the MITF protein in both apo and DNA bound forms. This suggests that Arg341Cys and Arg341His mutations are unlikely to have a significant impact on the overall structure of MITF. In addition, Arg341 is not present within the dimer interface indicating that dimer formation is unlikely to be altered due to the Arg341Cys and Arg341His mutations. While Arg341 does make contacts with the sugar-phosphate backbone of DNA when bound to the E-Box element it is unlikely that loss of this interaction alone promotes cytoplasmic localization of MITF. No association between loss of DNA binding and cytoplasmic localization has been demonstrated. Mutant forms of MITF lacking the complete DNA binding domain are retained within the nucleus16. Instead it seems possible that Arg341 may be part of a nuclear localization signal. Basic regions surrounding Arg341 (corresponding to Arg240 in MITF-M) have been demonstrated to promote nuclear localization. Residues in MITF-M that enhance nuclear localization include Arg and Lys residues between amino acids 197–206 and 255–26515–17. Mutations of Arg and Lys residues within either of these regions increase the fraction of MITF in the cytosol, similar to the effect seen with Arg341Cys and Arg341His variants. The identification of Arg341His was novel when we discovered it but it has since been listed as a variant of unknown significance for a non-specified condition in the ClinVar database (VCV000505101.1).
The MITF gene functions to regulate melanin production through tyrosinase and is also directly involved in the molecular process of hearing. In the inner ear, melanocytes are present in the intermediate layer of the stria vascularis. These melanocytes, so called intermediate cells possess a functional Na+-K+-ATPase, which controls the ion and material transport necessary for the maintenance of normal volumes and ion concentrations (recycling) of the endolymph. Therefore, it is essential in regulating the integrity of the stria vascularis and for maintaining normal hearing thresholds18. Only melanocytes in the inner ear possess this function whereas melanocytes in other pigmented tissues lack such a role18. In mice, depletion of the intermediate cells causes a substantial reduction in endocochlear potentials, severe degeneration of the endolymphatic space, and collapse and loss of sensory hair cells, accompanied by significant hearing loss18,19.
Mutations of MITF yielding diverging mechanisms but resulting in a similar phenotype have been recently demonstrated in melanoma, in that MITF knockdown and overexpression in murine and human melanoma cells showed opposing mechanisms, decrease or increase of immune cell migration and vice versa20. In our case of HL, different mechanisms of MITF mutations, impaired Na+-K+-ATPase function only or with defective melanin production, could lead to the same phenotype of hearing defect, though with some phenotypic variation, nonsyndromeic or syndromic type. This could be attributed to differences in genetic background, potential genetic redundancy or compensation of other associated genes depending on the defective mechanism involved of the particular MITF variant(s), and diverging individual mutations (dominant negative effect, haploinsufficiency or loss-of-function) rather than the gene itself.
Due to loss of function and Arg341His/Cys being located outside the DNA binding domain, it is unlikely that heterozygosity for Arg341His/Cys would disrupt DNA-binding ability. It is, therefore, very unlikely to disturb the neural crest-derived cochlear melanocytes in the early embryo stage or to cause the WS2A phenotype10.
Homozygosity for Arg341His/Cys may not disrupt in vivo TYR expression to below the critical level that can lead to albinism phenotypes. In addition to MITF, there are other genes, such as OTX2, TP53, and LEF1, that regulate TYR gene expression21–23. It is possible that the deleterious effect of p.Arg341His/Cys MITF on TYR expression can be overcome by the aforementioned genes. In contrast, a lack of genetic compensation for Na+-K+-ATPase function in cochlear monocytes can disrupt the endocochlear potential (EP) and results in NSHL24,25.
To our knowledge, this is the first time that biallelic mutations of MITF have been shown to cause NSHL with autosomal recessive inheritance, with heterozygous individuals free of symptoms. Biallelic MITF mutations were also shown to cause the rare syndrome, COMMAD (coloboma, osteopetrosis, microphthalmia, macrocephaly, albinism—oculocutaneous type, and deafness) in two unrelated children whose heterozygous parents were affected with classic WS2A26, while children in another family had a WS4-like phenotype but with more severe depigmentation of hair and skin while their parents were mildly affected27. Incomplete dominance was proposed as a mode of genetic inheritance for these two families26,27.
There are examples of severe phenotypes caused by heterozygous mutations, through gain of function or dominant negative mechanisms, whereas homozygous variants of the same gene can lead to a less severe phenotype due to loss of function. One example associated with HL is heterozygous GJB2 (Cx26) mutations resulting in an autosomal dominant syndromic HL, keratitis-ichthyosis-deafness (KID), and a homozygous GJB2 mutation causing ARNSHL28–30.
There are a number of limitations to the present study. Firstly, a thorough ophthalmological examination and temporal bone CT scan was not performed on affected individuals from Family-1; therefore, concealed associated defects cannot be completely ruled out. Secondly, cellular physiology was not studied to investigate the effect of the mutant MITF on Na+-K+-ATPase functions. Thirdly, the unidentified allele in Family-2 could be missed because WES/gene panel study and conventional sequencing cannot detect point mutation in the promotor region or deep introns, and the platform of CNV used in this study is not designed with dense probe for detection of a single/few exons deletion/duplication.
NSHL due to digenic inheritance between MITF and GJB2 genes was previously proposed in a single sporadic patient with NSHL31. Our data does not support digenic inheritance between MITF and GJB2, at least for Arg341His/Cys paired with Val37Ile because the HL phenotype was not observed in several individuals with this double heterozygosity. The presence of the GJB2-Val37Ile allele in our patients could represent a coincidental finding because the Val37Ile variant is prevalent in the Thai population with an allele frequency of 8.5%32. A different mutation at the codon 341, heterozygous p.Arg341Gly compounded with an unidentified mutation in the other allele has been reported in two hearing-impaired siblings from a consanguineous family, whereas both parents showed normal physical and hearing phenotypes, and only the mother carried Arg341Gly33.
In conclusion, we demonstrated that MITF can cause ARNSHL. Our data expand the list of genes underlying NSHL and indicate a new inheritance pattern of MITF. Digenic inheritance between MITF and another gene is possible and requires further characterization.
Methods
Patients and clinical exome analysis
Affected individual, IV-5, was previously evaluated and found to be heterozygous for a p.Val37Ile (c.109G>A) GJB2 allele but to not carry the GJB2 IVS1 + 1G>A variant. Mutation analysis including gap PCR for the 342-kb deletion delGJB6-D13S1850 and delGJB6-D13S1854 of GJB6 (Cx30), and direct sequencing of GJB3 (Cx31), SLC26A4, and MTRNR1 (a 12s rRNA gene: mtA1555G and mtC1494T) revealed no pathogenic variants34,35. DNA from individual IV-5 was analyzed using a hearing loss gene panel consisting of 70 HL genes (OtoGenome, Laboratory for Molecular Medicine, Cambridge, MA, USA, Supplementary information). This analysis identified the heterozygous p.Val37Ile mutation, validating our initial finding and supporting the exclusion of GJB2 and the other genes in the panel as underlying HL in this family. We therefore aimed to identify a new candidate gene.
Following identification of the candidate gene, we conducted a separate parallel mutation screening in a cohort of 130 individuals affected with early onset NSHL, using our in-house gene panel comprising 64 genes, including the candidate gene.
Each participating subject provided written informed consent, following approval of the protocol by the Ramathibodi Hospital Human Research Ethics Committee (protocols ID 07-56-66; 11-57-29; and 1324; MURA2020/367). All the experiment protocols involving humans were in accordance to international guidelines of Declaration of Helsinki.
Whole exome sequencing and analysis
DNA were subjected to WES using Illumina HiSeq 2000 (Macrogen, South Korea) with Agilent’s SureSelect for target enrichment and 100 bp Pair End mode (125× coverage). The exome data were quality assessed with the FastQC package and by read alignment against a reference genome (hg19 from UCSC genome browser database) using BWA version 0.5.9 (SAMTOOLS for variant identification; ANNOVAR for variant annotation).
Variants having minor allele frequencies > 0.03 in the 1,000 Genomes Project (November 2010 and October 2011 releases) and in our in-house database of 150 Thai exomes were filtered out. Only rare functional variants, including missense, nonsense, frameshift, non-frameshift, and splice site variants, were kept then separated into two groups, homozygous and heterozygous alleles, for subsequent manual inspection. Two scenarios were applied as follow: first, homozygous mutation in affected individuals, and heterozygous or wild-typed for unaffected persons; and second, compound heterozygous mutations for affected offspring, and heterozygous or wild-typed for unaffected persons. A total of 144 known hearing loss genes were analyzed (Supplementary information).
Computational (in silico) predictive programs, namely SIFT, PolyPhen-2, MutationTaster, Splice Site Prediction by Neural Network; and mutation/variant databases including ClinVar and the Human Genome Mutation Database (HGMD), were used to determine pathogenicity of the variants identified. Sanger sequencing was performed to verify the variants detected.
Phen-Gen online tool was used to identify causative genes. Individuals’ annotated variant files were combined into one file using CombineVariants tools (GATK, Genome analysis toolkits) and the phenotype data file (PED) was created using PLINK application13. The standard human phenotype ontology, congenital sensorineural hearing impairment with HPO:0008527 was employed. The new combined genotype file, HPO and PED files were then submitted together to PHEN-GEN (https://phen-gen.org/).
Screening for mutation(s) identified in a control population
A real-time PCR (Taqman) assay was performed on 228 DNA specimens from regular blood donors, using 7,500 Real-Time PCR System (Applied Biosystems). The hydrolysis probes and primers were designed according to the MITF gene sequence (GenBank NM_198159.2). The probes for detecting the wild-type and the Arg341His mutant alleles were tagged with 6-FAM and VIC, respectively, at the 5′ end. The primer and probe sequences were as follow: Forward primer 5′-GTTTTCCTCCATTTTCATCGCAGAG-3′; Reverse primer: 5′-TCCACGGATGCTTTAAGATG-GTT-3′; wild-type probe: 6-FAM 5′-CTTGTTCCAGCGCATGT-3′ MGB; mutant probe: VIC 5′-CCTTGTTCCAGTGCATGT-3′ MGB.
Each real-time PCR reaction contained 20 ng of gDNA, 0.9 μM of each primer, 0.25 μM of each probe and 5 μl of TaqMan Genotyping Master Mix (Applied Biosystems). The thermal profile included initial denaturation at 95 °C for 10 min, followed by 40 amplification cycles of denaturation at 92 °C for 15 s, and annealing and extension at 60 °C for 60 s.
Our in-house WES database from 150 unrelated individuals affected with disorders other than HL was checked for the presence of the variants identified. Reference sequences were as follow: NT_011520.11, NM_006941.3, NP_008872.1 for MITF isoform A; and NT_022495, NM_000248, NP_000239 for MITF isoform M.
Copy number variation (CNV) analysis
CNV analysis using single nucleotide polymorphism array (Illumina Infinium CytoSNP-850K BeadChip) was performed then analyzed by using BlueFuse Multi software v4.1.
Targeted-exome sequencing using our in-house gene panel
DNA was extracted from patients’ peripheral blood using Purgene DNA extraction kit. A 20 ng of genomic DNA were subjected to NGS using Ion AmpliSeq Designer (Thermo Fisher Scientific) with 100% coverage for all coding sequences of 64 HL associated genes. The targeted sequencing was performed using Ion Torrent system (Thermo Fisher Scientific) as per manufacturer's instructions. The NGS workflow consisted of library preparation step, template preparation step, and sequencing in Ion Proton semiconductor sequencer. Sequences were then analyzed using the SNP & Variation Suite (Golden Helix, Inc.). The target genes were as follow: ACTG1, CCDC50, CDH23, CEACAM16, CLDN14, COCH, COL11A2, CRYM, DFNA5, DFNB59, DIABLO (SMAC), DIAPH1, ESPN, ESRRB, EYA4, GIPC3, GJB2, GJB3, GJB6, GPSM2, GRHL2, GRXCR1, HGF, ILDR1, KCNQ4, LHFPL5, LOXHD1, LRTOMT, MARVELD2, MIR96, MITF, MSRB3, MYH14, MYH9, MYO15A, MYO1A, MYO3A, MYO6, MYO7A, OTOA, OTOF, PCDH15, POU3F4, POU4F3, PRPS1, PTPRQ, RDX, SERPINB6, SLC17A8, SLC26A4, SLC26A5, SMPX, STRC, TECTA, TJP2, TMC1, TMIE, TMPRSS3, TPRN, TRIOBP, USH1C, USH2A, WFS1, and WHRN.
Plasmids, cell culture, transfection, and reporter assay
The luciferase reporter containing the human TYR promotor (pGL3-Tyr-Luc; − 1995/+ 74) was kindly donated by Dr. Reinisalo, University of Eastern Finland, Finland (Fig. 3c)22. A wild-type MITF expression plasmid was prepared from a full length MITF-isoform A cDNA, which was obtained from pCMV3-C-GFPSpark-MITF (Sino Biological Inc., China) followed by HindIII and XbaI restriction digestion and ligation into pCMV10 3X Flag (N-terminal; Sigma, St Louis, WA, USA). Site-directed mutagenesis was performed using QuikChange II XL Site-Directed Mutagenesis Kit (Agilent, USA), according to the manufacturer’s protocol. All plasmid constructs were selected with diagnostic restriction digestion and verified by Sanger sequencing. Wild-type and mutant constructs were cloned into plasmid pCMV10 3X Flag and pCMV B-galactosidase (kindly provided by Dr. Jia-da Li, Central South University of China, China) before transient transfection for luciferase and beta-galactosidase activity assays, as previously described15.
A 1 × 105 melanoma (G361) or mouse embryonic fibroblast (NIH/3T3) cells were seeded into 6-well plates and cultivated in Dulbecco’s modified Eagle’s medium supplemented with 10% fetal bovine serum, 100 U/ml penicillin and 100 μg/ml streptomycin, under 5% CO2 at 37 °C for 24–48 h prior to transfection. Cells were 70–80% confluent on the day of transfection. The transfection mix was prepared using a ratio of 3 μl Lipofectamine 2000 for every 1 μg of total DNA transfected. pCMV10 3X Flag and pCMV B-galactosidase were used for normalization and monitoring the transfection efficiency, respectively.
Twenty-four hours after transfection, lysates were prepared from the cultured G361 cells (Promega, USA) and then assayed for luciferase and B galactosidase activity using the Infinite 200 PRO plate reader (Tecan, Switzerland). All reporter assays were performed in triplicate, at least three times on different days, using different batches of cells. The G361 cells were kindly provided by Prof. Uraiwan Panich (Mahidol University) and the NIH3T3 cells were purchased from ATCC.
Western blot analysis
The MITF protein in transfected G361 cells was verified by western blot analysis using a mouse monoclonal anti-Flag M2 antibody. Cells cultured for 48 h were harvested and protein isolated using RIPA lysis buffer (Bio-Rad), supplemented with protease inhibitor cocktail (AppliChem, Germany) and 1 mM phenylmethylsulfonyl fluoride (Merck, Germany). The proteins (20 µg) were then subjected to SDS-PAGE (12%) and transferred onto a polyvinylidene fluoride membrane with pore size 0.22 µm. The membrane was blocked using blocking solution (3% bovine serum albumin in TBS plus 0.1% Tween-20) for 2 h and then stained with a mouse monoclonal anti-Flag M2 antibody (1:1,000 dilution, Sigma) at 4 °C overnight. A goat anti-mouse GAPDH antibody (Thermo Scientific) was used as a control for protein loading. After washing with washing buffer (TBS plus 0.1% Tween-20) for 15 min, four times, the membrane was stained for 1 h with a goat anti-mouse IgG secondary antibody conjugated with horseradish peroxidase (1:1,000 dilution, Thermo Fisher Scientific) at room temperature followed by four washes. Protein levels were measured using Luminata Forte Western HRP substrate (Merck, USA) with a C-DiGit Chemiluminescence Western Blot Scanner (LI-COR Bioscience).
Immunofluorescence study
NIH3T3 cells were transfected with 200 ng of pCMV10 3X Flag wild-type MITF or MITF variant expression plasmids following an established protocol15. At 48 h after transfection, the cells were fixed with 4% paraformaldehyde at room temperature for 30 min, permeabilized in PBS plus 0.2% Triton X-100 (Scharlau, Spain) for 1 h, blocked with blocking solution (PBS, 3% bovine serum albumin plus 5% goat serum) at room temperature for 1 h, stained with mouse monoclonal anti-Flag M2 primary antibody (1:600 dilution, Sigma) at 4 °C overnight, washed with PBS for three times, and then incubated for 2 h with DyLight 488 fluorescence-labeled secondary goat anti-mouse antibody (1:300 dilution, Thermo Fisher Scientific). The cells were incubated with 4,6-diamino-2-phenylindole (DAPI, Invitrogen) for 3 min before immunofluorescence analysis using a laser scanning confocal microscope (Nikon, Japan) and the NIS-Elements Viewer software package.
Molecular modeling
Structural models of human wild-type MITF and Arg341His and Arg341Cys MITF variants were generated with SWISS-MODEL36,37 using the Mus musculus MITF:E-box complex (4atk) and apo MITF (4ath) as templates10. Structures were viewed using the PyMOL Molecular Graphics System, version 2.0.6 (Schrödinger, LLC, NY, USA).
Supplementary information
Acknowledgements
We thank the patients’ families for their participation in this project; National Science and Technology Development Agency grant (NSTDA: Grant #P-13-00735) and a Mahidol University Grant (#134/2559) for funding this work to DW; and NRCT-Research University Network (RUN) grant to NJ; and Thailand Research Fund (TRF RSA6180082) to LTJ. We thank Dr. Mika Reinisalo and Prof. Jia-da Li for donating reagents; Prof. Uraiwan Panich for providing the melanoma cell lines. DW, NJ, and TT was/are recipients of the Research Career Development Awards from the Faculty of Medicine at Ramathibodi Hospital. We thank Jeremy Allen, PhD, from Edanz Group (https://www.edanzediting.com/ac) for editing a draft of this manuscript.
Author contributions
S.T. performed molecular and functional experiments and bioinformatic analysis and wrote the manuscript. S.N. and A.K. performed gene panel analysis. T.T. and K.L. collected and interpreted clinical data. L.T.J. performed molecular modeling analysis and wrote part of the manuscript. B.S. and A.J. supervised the bioinformatic analysis. N.J. supervised the functional study and performed cytogenomic microarray study. D.W. obtained research grants, designed the study concept, and critically revised the manuscript. All authors reviewed and approved the final manuscript.
Data availability
Data openly available in a public repository that issues datasets with DOIs.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
is available for this paper at 10.1038/s41598-020-69633-4.
References
- 1.Chang KW. Genetics of hearing loss—Nonsyndromic. Otolaryngol. Clin. N. Am. 2015;48:1063–1072. doi: 10.1016/j.otc.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 2.Korver AM, et al. Congenital hearing loss. Nat. Rev. Dis. Primers. 2017;3:16094. doi: 10.1038/nrdp.2016.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hereditary Hearing Loss Homepage. 2019. (Accessed 4 Jan 2020); https://hereditaryhearingloss.org
- 4.Yang T, et al. Transcriptional control of SLC26A4 is involved in Pendred syndrome and nonsyndromic enlargement of vestibular aqueduct (DFNB4) Am. J. Hum. Genet. 2007;80:1055–1063. doi: 10.1086/518314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cabanillas R, et al. Comprehensive genomic diagnosis of non-syndromic and syndromic hereditary hearing loss in Spanish patients. BMC Med. Genom. 2018;11:58. doi: 10.1186/s12920-018-0375-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sloan-Heggen CM, et al. Comprehensive genetic testing in the clinical evaluation of 1119 patients with hearing loss. Hum. Genet. 2016;135:441–450. doi: 10.1007/s00439-016-1648-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tekin D, et al. A next-generation sequencing gene panel (MiamiOtoGenes) for comprehensive analysis of deafness genes. Hear Res. 2016;333:179–184. doi: 10.1016/j.heares.2016.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang T, Wei X, Chai Y, Li L, Wu H. Genetic etiology study of the non-syndromic deafness in Chinese Hans by targeted next-generation sequencing. Orphanet. J. Rare Dis. 2013;8:85. doi: 10.1186/1750-1172-8-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seco CZ, et al. The diagnostic yield of whole-exome sequencing targeting a gene panel for hearing impairment in The Netherlands. Eur. J. Hum. Genet. 2017;25:308–314. doi: 10.1038/ejhg.2016.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pogenberg V, et al. Restricted leucine zipper dimerization and specificity of DNA recognition of the melanocyte master regulator MITF. Genes Dev. 2012;26:2647–2658. doi: 10.1101/gad.198192.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Richards S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015;17:405–424. doi: 10.1038/gim.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goding CR, Arnheiter H. MITF-the first 25 years. Genes Dev. 2019;33:983–1007. doi: 10.1101/gad.324657.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Javed A, Agrawal S, Ng PC. Phen-Gen: Combining phenotype and genotype to analyze rare disorders. Nat. Methods. 2014;11:935–937. doi: 10.1038/nmeth.3046. [DOI] [PubMed] [Google Scholar]
- 14.Pingault V, et al. Review and update of mutations causing Waardenburg syndrome. Hum. Mutat. 2010;31:391–406. doi: 10.1002/humu.21211. [DOI] [PubMed] [Google Scholar]
- 15.Zhang H, et al. Functional analysis of MITF gene mutations associated with Waardenburg syndrome type 2. FEBS Lett. 2012;586:4126–4131. doi: 10.1016/j.febslet.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Fock V, et al. Subcellular localization and stability of MITF are modulated by the bHLH-Zip domain. Pigment Cell Melanoma Res. 2019;32:41–54. doi: 10.1111/pcmr.12721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Takebayashi K, et al. The recessive phenotype displayed by a dominant negative microphthalmia-associated transcription factor mutant is a result of impaired nucleation potential. Mol. Cell Biol. 1996;16:1203–1211. doi: 10.1128/MCB.16.3.1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tachibana M, et al. Ectopic expression of MITF, a gene for Waardenburg syndrome type 2, converts fibroblasts to cells with melanocyte characteristics. Nat Genet. 1996;14:50–54. doi: 10.1038/ng0996-50. [DOI] [PubMed] [Google Scholar]
- 19.Zhang W, et al. Perivascular-resident macrophage-like melanocytes in the inner ear are essential for the integrity of the intrastrial fluid-blood barrier. Proc. Natl. Acad. Sci. USA. 2012;109:10388–10393. doi: 10.1073/pnas.1205210109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wiedemann GM, et al. Microphthalmia-associated transcription factor (MITF) regulates immune cell migration into melanoma. Transl. Oncol. 2019;12:350–360. doi: 10.1016/j.tranon.2018.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khlgatian MK, et al. Tyrosinase gene expression is regulated by p53. J. Invest. Dermatol. 2002;118:126–132. doi: 10.1046/j.0022-202x.2001.01667.x. [DOI] [PubMed] [Google Scholar]
- 22.Reinisalo M, Putula J, Mannermaa E, Urtti A, Honkakoski P. Regulation of the human tyrosinase gene in retinal pigment epithelium cells: The significance of transcription factor orthodenticle homeobox 2 and its polymorphic binding site. Mol. Vis. 2012;18:38–54. [PMC free article] [PubMed] [Google Scholar]
- 23.Wang X, et al. LEF-1 regulates tyrosinase gene transcription in vitro. PLoS ONE. 2015;10:e0143142. doi: 10.1371/journal.pone.0143142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jin Z, Uhlen I, Wei-Jia K, Mao-li D. Cochlear homeostasis and its role in genetic deafness. J. Otol. 2009;4:15–22. doi: 10.1016/S1672-2930(09)50003-7. [DOI] [Google Scholar]
- 25.Steel KP, Barkway CH. Another role for melanocyte: their importance for normal stria vascularis development in mammalian inner ear. Development. 1989;107:453–463. doi: 10.1242/dev.107.3.453. [DOI] [PubMed] [Google Scholar]
- 26.George A, et al. Biallelic mutations in MITF cause coloboma, osteopetrosis, microphthalmia, macrocephaly, albinism, and deafness. Am. J. Hum. Genet. 2016;99:1388–1394. doi: 10.1016/j.ajhg.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pang X, et al. A homozygous MITF mutation leads to familial Waardenburg syndrome type 4. Am. J. Med. Genet. A. 2019;179:243–248. doi: 10.1002/ajmg.a.60693. [DOI] [PubMed] [Google Scholar]
- 28.Beltramello M, Piazza V, Bukauskas FF, Pozzan T, Mammano F. Impaired permeability to Ins(1,4,5)P3 in a mutant connexin underlies recessive hereditary deafness. Nat. Cell Biol. 2005;7:63–69. doi: 10.1038/ncb1205. [DOI] [PubMed] [Google Scholar]
- 29.de Zwart-Storm EA, et al. A novel missense mutation in GJB2 disturbs gap junction protein transport and causes focal palmoplantar keratoderma with deafness. J. Med. Genet. 2008;45:161–166. doi: 10.1136/jmg.2007.052332. [DOI] [PubMed] [Google Scholar]
- 30.Snoeckx RL, et al. GJB2 mutations and degree of hearing loss: A multicenter study. Am. J. Hum. Genet. 2005;77:945–957. doi: 10.1086/497996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim SY, et al. Unraveling of enigmatic hearing-impaired GJB2 single heterozygotes by massive parallel sequencing: DFNB1 or not? Medicine (Baltimore). 2016;95:e3029. doi: 10.1097/MD.0000000000003029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wattanasirichaigoon D, et al. High prevalence of V37I genetic variant in the connexin-26 (GJB2) gene among non-syndromic hearing-impaired and control Thai individuals. Clin. Genet. 2004;66:452–460. doi: 10.1111/j.1399-0004.2004.00325.x. [DOI] [PubMed] [Google Scholar]
- 33.Zhang Z, et al. A novel variant in MITF in a child from Yunnan-Guizhou Plateau with autosomal dominant inheritance of nonsyndromic hearing loss: A case report. Mol. Med. Rep. 2018;17:6054–6058. doi: 10.3892/mmr.2018.8627. [DOI] [PubMed] [Google Scholar]
- 34.del Castillo FJ, et al. A novel deletion involving the connexin-30 gene, del(GJB6-d13s1854), found in trans with mutations in the GJB2 gene (connexin-26) in subjects with DFNB1 non-syndromic hearing impairment. J. Med. Genet. 2005;42:588–594. doi: 10.1136/jmg.2004.028324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.del Castillo I, et al. A deletion involving the connexin 30 gene in nonsyndromic hearing impairment. N. Engl. J. Med. 2002;346:243–249. doi: 10.1056/NEJMoa012052. [DOI] [PubMed] [Google Scholar]
- 36.Bordoli L, et al. Protein structure homology modeling using SWISS-MODEL workspace. Nat. Protoc. 2009;4:1–13. doi: 10.1038/nprot.2008.197. [DOI] [PubMed] [Google Scholar]
- 37.Schwede T, Kopp J, Guex N, Peitsch MC. SWISS-MODEL: An automated protein homology-modeling server. Nucleic Acids Res. 2003;31:3381–3385. doi: 10.1093/nar/gkg520. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data openly available in a public repository that issues datasets with DOIs.