Abstract
Background
International rotations with hands-on experience are commonly cited as a potential supplement to the current experience of surgical trainees in trauma; however, quantification of this experience remains unclear.
Methods
A link to an online survey was distributed by electronic mail to physicians who rotated for any period of time at the Trauma Unit of the Groote-Shuur Hospital of the University of Cape Town from January 1, 2006, to December 2016.
Results
Of 160 participants, 75 (47%) completed the survey. A high proportion (45%) had performed less than 25 trauma-related surgical procedures during their previous training. Most (56%) performed ≥ 10 trauma laparotomies and sternotomies/thoracotomies during their rotation, whereas 43% performed ≥ 5 vascular procedures. The level of perceived confidence in managing trauma patients increased significantly from a median of 3/10 to 7/10 (P < .05).
Conclusion
Rotations at large-volume trauma centers abroad offer the opportunity for a hands-on operative experience and may enhance the confidence of surgical trainees. Further standardization of these opportunities may result in a larger-scale participation of graduate residents and fellows.
Highlights
-
•
This is a survey of physicians who participated in an international rotation at the Groote Schuur Hospital of the University of Cape Town.
-
•
With this survey, we found that most participants performed in excess of 10 trauma laparotomies and thoracotomies/sternotomies.
-
•
A large proportion performed 5 or more peripheral vascular procedures.
-
•
These findings are combined with a significantly increased confidence in managing trauma patients.
-
•
This report may serve in the planning of sponsored international rotations to increase the operative exposure in trauma surgery.
1. Introduction
Adequate exposure of general surgery residents in the United States to trauma-related surgical procedures during their training remains a complex problem that surgical educators; program directors: and the leadership of the Accreditation Council for Graduate Medical Education, the American College of Surgeons, and the American Board of Surgery are constantly attempting to define and address. This underexposure to open trauma surgery is not unique to surgical trainees in the United States, as concerns about adequate training are increasingly raised in other developed countries as well, including Canada [1]. In several countries of Europe, trauma surgery is considered a branch of orthopedic surgery, and involvement with truncal injuries may vary. The lack of large registries to quantify operative experience during training in these countries, as well as the variation in the development of trauma systems [2], complicates the matter of surgical training even further.
In the United States, based on data from the last 3 decades, an increasing number of graduates complete their training with a decreasing number of open surgical procedures involving trauma patients [3,4]. Several factors may contribute to this decreasing exposure, including the 80-hour work restriction rules, the increased utilization of nonoperative management in trauma, the introduction of endovascular solutions to control bleeding, and the increased trend for subspecialization. Adequate exposure of general surgeons to operative trauma is of paramount importance for when nonoperative management fails and for those practicing in austere regions where the general surgeon is expected to provide broad and comprehensive care.
This perceived gap of inadequate exposure to trauma surgery has led to the development of various focused and hands-on courses such as the Advanced Trauma Operative Management [5] and the Advanced Surgical Skills for Exposure in Trauma [6]. Although these courses provide improvement in self-confidence, knowledge, and judgement among participating residents [[7], [8], [9]], by no means do they provide a panacea for the problem of underexposure to open trauma surgery. As a result of the perception of inadequate surgical training and performance insecurity, currently more than 3 of 4 graduates seek additional training in the form of a subspecialty fellowship [10]. However, even with the increasing number of fellowship trained surgeons, most program directors of Acute Care Surgery and Surgical Critical Care programs agreed in a recent survey that there is a need for additional operative exposure in trauma, and they recognized that international fellow rotations could be a tool to enhance this exposure [11]. Although these rotations are not standardized and commonly are not incorporated into a general surgery or subspecialty fellowship training, they provide ample opportunity for surgical exposure due to the high demand for surgeons, the limited resources, and several other socioeconomic factors that allow for the opportunity for management of a patient population with different needs and that is at a high risk for an injury.
Groote Schuur Hospital (GSH) is the chief academic hospital of the University of Cape Town in South Africa. Being an internationally acclaimed research institution and world-renowned for the care of trauma patients, this hospital attracts a large number of rotating international medical students, residents, and fellows who seek additional experience in trauma surgery. Using a standardized survey, we sought to investigate the aims of international rotating physicians and the perceived benefits accrued during the time spent at the Trauma Unit of the GSH. We also sought to quantify the operative exposure during these rotations and the overall impact on the confidence levels in performing trauma-related procedures. We hypothesized that despite the significant variability in surgical training across the world, rotating physicians enhance their confidence in performing trauma surgery.
2. Material and Methods
2.1. Description of the Trauma Unit and the International Rotation
The Trauma Unit at the GSH is a leading academic authority that has contributed to the advancement of trauma systems and care in Cape Town and in South Africa as a whole. With more than 12,000 trauma patients evaluated every year [12], this unit stands among the busiest trauma centers in the world. The large volume of trauma patients allows for research that results in pioneer changes in the care of the injured, especially after penetrating trauma [[13], [14], [15]]. In addition, it attracts a number of international medical students, residents, fellows, and even physicians or surgeons in practice who seek to boost their experience and knowledge in trauma surgery.
The GSH is 1 of the 2 tertiary referral centers for trauma in Cape Town and is part of the Associated Academic Hospitals’ group. Patients visiting the emergency department (ED) are directed either to the Trauma Unit or the Medical Unit depending on whether they have suffered an acute injury. In the Trauma Unit, patients are triaged into 1 of 3 distinct zones, depending of the acuity of their condition: red (or “Resuscitation”) for high, yellow for medium, and green for low acuity. A procedure room is also available for bedside procedures including chest tube placement, wound repair, cast placement, and other minor surgical procedures. Subspecialty consultations are available upon request and include Orthopedic, Vascular, Cardiothoracic, and Neurosurgery. The Radiology suite and Blood Bank are both in close proximity. A neurosurgical intensive care unit (ICU) is available for traumatic brain injury patients, and a medical/surgical ICU is available for other trauma patients who are in extremis; however, availability of beds is limited. Step-down unit with 6 beds is available for patients requiring higher level of care and for postoperative patients. In the ED, the unit is staffed by residents in surgery and emergency medicine, in addition to medical students. A surgical registrar (equivalent to a senior or a chief resident in the United States) is on in-house call for 24 hours, along with an attending surgeon.
Foreign physicians who desire hands-on experience are required to apply to the Health Professions Council of South Africa for a Medical Practitioner license. An alternative would be a rotation where the physician can only observe but not actively participate in the care of patients. The time allocated for these rotations varies depending on the applicant’s goals and prior experience. Participants can be allowed to be the registrar on call after a period of evaluation by the unit’s faculty. This opportunity is mostly considered for physicians who spend a period of at least 6 months at the unit, including a period of service in the ED where they become familiar with the daily operations of the unit and the hospital in general. Otherwise, they are included in the call schedule to remain in-house with the registrar on call. Depending on the anticipated complexity of the procedure and the patient’s injury, surgical procedures are performed by the registrar and the visiting physician, with or without the presence of the attending surgeon on call.
Visiting physicians are offered research opportunities and mentorship. They also participate in the unit’s curriculum which includes weekly educational sessions, lectures, journal club, and morbidity and mortality conferences.
2.2. Study Design
A list of electronic mail addresses was compiled and included all physicians who rotated for any period of time at the Trauma Unit of the GSH of the University of Cape Town from January 1, 2006, to December 2016. Medical students were excluded. An online survey was then developed on the Web site Typeform, and the link to the survey was then distributed by electronic mail. The survey instrument was slightly modified for participants from countries outside the United States because of differences in surgical training. These modifications included mostly how the level of training was named (ie, senior/chief resident vs registrar). Participants were divided into those who graduated from the United States (US grads) and those who did not (non–US grads). Anonymity was fully maintained, and completion of the survey was voluntary.
Two notifications were sent over a period of 30 days, and the survey was open for a period of 60 days. When electronic mail addresses were inaccurate or reported to be not in use, an attempt was made with an online search to locate a potential electronic mail address that could be currently in use.
2.3. Survey Instrument
The survey instrument included 31 questions that focused on demographics, the level of training, the participant’s training program characteristics, the purpose of the rotation, the operative and other experience attained during the rotation, and finally the financial and family aspects involved. A proportion of the questions required a single response, whereas others allowed for multiple responses. The time required to complete the survey was estimated to be approximately 15 minutes, and participants were allowed to save their responses to complete the survey at a later time.
2.4. Statistical Analysis
Descriptive statistics were used, mostly as frequency distributions for the questionnaire responses. A paired sample t test was performed to assess the statistical significance in the change of confidence levels in performing surgical procedures before and after the rotation. All statistical analyses were performed using the IBM SPSS Statistics for Windows, Version 20.0 (IBM Corp, Armonk, NY).
3. Results
A total of 230 physicians rotated at the Trauma Unit over the 11-year study period. Of those, 52 (22.6%) had no electronic mail available, whereas 28 had an inaccurate mail or their mail was currently not in use. With an online search, the electronic address of 10 of these physicians was able to be retrieved. Of the 160 eligible participants, 75 (46.9%) completed the online survey. Of those, 34 (45.3%) were US grads and the remaining 41 (54.7%) were non–US grads (n = 6 or 14.6% from the United Kingdom, n = 4 or 9.8% from Canada, n = 7 or 17.1% from the Netherlands, and the remaining 24 or 58.5% from other countries).
Most participants were male (n = 59 or 78.7%) and between the ages of 30 and 35 years (n = 43 or 57.3%). Approximately half (n = 37, 49.4%) joined the unit between 2013 and 2016. The time spent in the unit was almost equally divided between 1–2 months (n = 17 or 22.7%), 3–4 months (n = 17 or 22.7%), and 5–6 months (n = 16 or 21.3%). Only 6 physicians (8.0%) remained in the unit for less than a month, whereas 8 (10.7%) spent more than a year. A total of 32 physicians (42.7%) had completed at least 4 years of surgical training at the time of their participation in the rotation, whereas 22 (29.3%) had completed 3 years or less. Eight (10.7%) had completed a fellowship training including surgical critical care, trauma, and/or vascular surgery. Most were (n = 48/70 or 68.6%) trained at a program with less than 2500 annual trauma admissions, and 34 (45.3%) had performed less than 25 trauma-related surgical procedures during their training and prior to their rotation at the Trauma Unit. The most commonly cited reason for participating in this rotation was “I felt that I needed more experience in managing penetrating trauma patients” (n = 37 or 49.3%) followed by “I was interested in exploring other trauma systems” (n = 30 or 40.0%).
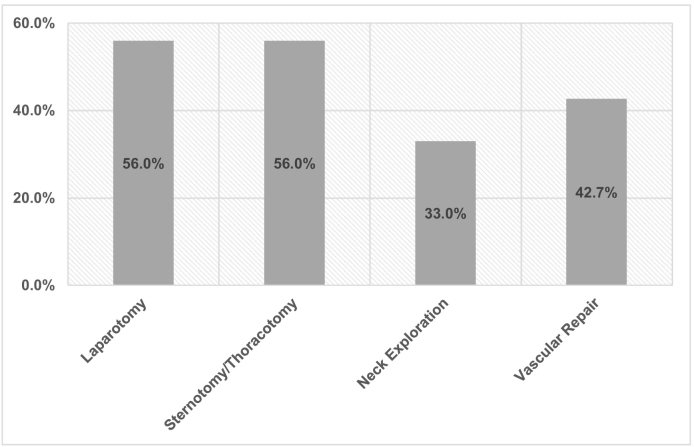
A complete log of surgical cases was maintained by 30 (40.0%) participants, with 16 (21.3%) maintaining a partial log. Figure 1 outlines the estimated number of procedures performed during the rotation for trauma laparotomy, trauma sternotomy/thoracotomy, neck exploration for trauma, and vascular repair for trauma. Almost 6 of 10 participants performed 10 or more trauma laparotomies and sternotomies/thoracotomies during their rotation, whereas more than 4 of 10 performed 5 or more vascular procedures. On a scale from 1 to 10, with 1 being extremely low and 10 being extremely high, the volume of cases was perceived to be 7.6 ± 1.8 (median: 8) by the rotating physicians. Similarly, the diversity of cases was perceived to be 7.7 ± 1.8 (median: 8).
Fig 1.
Proportion of participants who performed more than 10 cases of laparotomy and sternotomy/thoracotomy and more than 5 cases of neck exploration and vascular repair during their rotations.
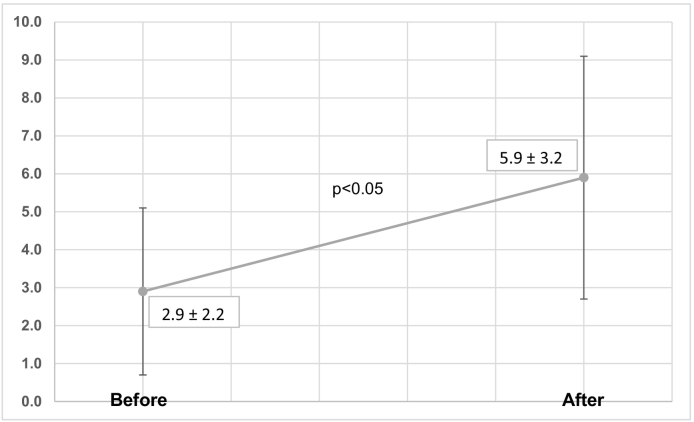
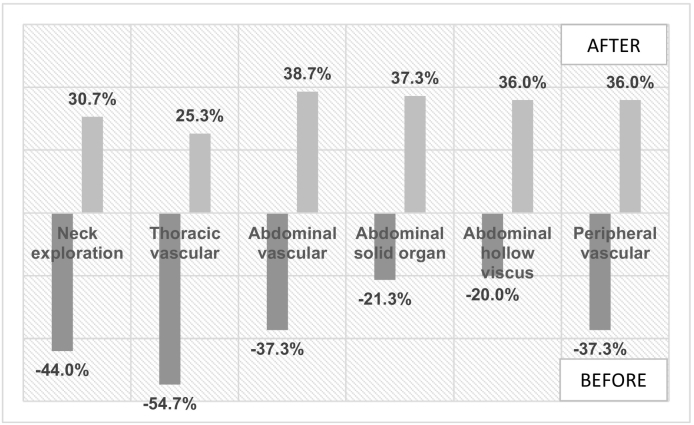
Participants were asked about their levels of confidence on a scale from 1 to 10 in performing trauma procedures before and after their rotation. Most (n = 69 or 89.3%) had a level of confidence that was less than 6 prior to their rotation. This figure changed to 88.0% (n = 68) of participants reporting a confidence level that exceeded 5. Figure 2 depicts the change in the confidence level from a median of 3 to 7 (P < .05). Performing thoracic vascular procedures was reported by most as the procedures that physicians were least comfortable performing prior to their rotation. Figure 3 outlines the surgical procedures that participants were least comfortable with prior to their rotation and the procedures that they gained confidence in performing after their rotation.
Fig 2.
Level of confidence in performing trauma-related surgical procedures before and after the international rotation (data depicted represent means ± standard deviations).
Fig 3.
Trauma-related surgical procedures that participants reported being least confident performing prior and procedures they reported becoming more confident performing after their rotation.
More than a third of participants (n = 27 or 36.0) engaged in research activities, with 21 of them (77.8%) publishing at least 1 peer-review article. Interestingly, 14 participants (18.7%) reported repeating another rotation at the Trauma Unit at a later time. Twenty (26.7%) reported that they currently do not practice Trauma Surgery, whereas only 5 (6.7%) reported practicing exclusively trauma surgery. A total of 18 participants (24.0%) are currently practicing at academic hospitals.
As for the expense coverage during their rotation, 32 of 69 (46.4%) participants were partially or fully sponsored by their own institution, whereas 31 of 69 (44.9%) used their own savings. Sixteen (21.3%) estimated that their expenses did not exceed $5000, whereas 27 (36.0%) estimated that they spent more than $10,000 during their stay. Thirty-eight (38/73 or 52.1%) were accompanied by family during part or their entire rotation.
4. Discussion
In this electronic survey of physicians who participated in an international rotation at a large trauma center in South Africa, we found that the most common reasons for participation were the need for additional experience in the management of penetrating trauma and the interest in exploring different trauma systems. Almost half of the participants had performed less than 25 operative trauma cases prior to their rotation, independent of their level of training. Abdominal solid organ and hollow viscus surgeries were the procedures that physicians were most confident performing prior to their rotation. However, more than 50% reported having decreased confidence performing thoracic vascular procedures, whereas more than 40% reported decreased confidence performing neck explorations. During their international rotation, most (approximately 60%) performed 10 or more trauma laparotomies and sternotomies/thoracotomies, whereas more than 40% performed 5 or more vascular procedures. This international rotation resulted in a significant boost in confidence in performing operative trauma procedures.
With a population that approximates 57 million, South Africa is one of the most populated countries in sub-Saharan Africa [16]. Despite significant socioeconomic transformation over the last 2 decades and despite being the most developed economy in the region [17], the country continues to face an epidemic of crime and violence. The murder rate of approximately 33 per 100,000 citizens ranks South Africa as the eighth most violent country in the world [18]. Between 2016 and 2017, an average of 467 assaults with the intent to inflict grievous bodily harm was recorded every day [19]. In addition to the violent deaths and injuries, the country is also struggling with a national burden from road traffic–related deaths, which continue to exceed 14,000 annually, with approximately 40% involving pedestrians [20,21]. The levels of violence have an enormous cost that exceeds 22% of the country’s gross domestic product [18], whereas road traffic accidents cost more than 3% of the gross domestic product [22]. These figures were the driving force for the development of trauma systems focusing on prevention and improving outcomes [23]. Trauma surgeons needed to acclimate to a high-volume demanding environment with relatively limited resources, especially with researching the role of nonoperative management of traumatic injuries [[13], [14], [15],24,25], which is now widely adopted [26,27]. The development of partnerships and collaborations with trauma centers across the globe allowed for international students and physicians to have a hands-on experience in trauma surgery that is increasingly declining in other developing and developed countries.
Although the face of emergency surgery has changed, with the focus on development of minimally invasive surgical skills to address common problems in acute care surgery [[28], [29], [30]], the need for developing competency in open surgical procedures, especially for patients in extremis, remains a necessity. This not only applies to trauma surgery but includes other subspecialties such as hepatobiliary surgery [31]. In The National Academies of Science, Engineering and Medicine landmark report that called for an ambitious roadmap to achieve zero preventable injury deaths, one of the recommendations referred to the development of military and civilian trauma workforce training and readiness [32]. The constantly declining operative volume not only in general surgery programs [3,4,33] but also in subspecialty fellowships [34] adds to the challenges associated with this goal. Although it is exceedingly difficult to study the impact of surgical competence on outcomes, it is widely accepted that these 2 factors strongly correlate, and therefore achieving surgical competence through appropriate training venues is a necessary part of achieving improved outcomes and decreasing the risk for preventable deaths.
Various programs that aim at integrating health care services with training at underdeveloped countries are currently available [11,[34], [35], [36], [37], [38], [39]]. In fact, in a recent survey by Ferrada et al, almost 80% of program directors reported that their surgical critical care and trauma surgery fellowship program offers an international rotation, although it is unclear how often this opportunity is used [34]. In addition, most program directors thought that this experience, in addition to supplementing operative exposure, would provide research opportunities, collaborations, and a better understanding of trauma systems globally. The training challenges of the future generation of trauma surgeons are complex and may require many different solutions. Promoting collaborations is important to allow for utilization of currently available resources that can offer potential solutions. These opportunities may even serve specific needs, such as operative experience in vascular trauma [3,40], as in our survey, almost 4 of 10 participants reported performing 5 or more vascular procedures during their rotation.
In considering participation in the international rotation, a few issues need to be reviewed. The high levels of violence and crime may pose a significant risk for international physicians. Dedicated housing, advice from locals and from previous rotating physicians, and common sense low-risk daily habits can be an invaluable source to increase safety. Funding is another considerable barrier for physicians to seek this experience. Sponsorships by training programs and other authorities, including the American College of Surgeons, may facilitate further the training of future trauma surgeons. Standardization of the educational curriculum of these rotations is necessary to allow them to potentially become an integral part of resident and/or fellow training. This may require a minimum period of participation to allow for the accepting institution to implement a proposed curriculum. Common evaluation process and feedback may be lacking. Lastly, one of the most important challenges would be to help trainees understand the differences in trauma systems and available resources and identify the practices that can or cannot be adopted in the daily management of trauma patients, especially given the possible difference in outcomes of specific patient populations [41].
The face of trauma surgery has dramatically changed over the last decade. Despite concerns about the care of severely injured patients in the future, there are no quantifiable data to indicate that the mortality rate for these patients is increasing. In fact, quite the opposite is being observed. It is possible that despite the decreasing operative exposure in trauma, trainees are developing excellent resuscitation skills and are mastering nonoperative management. Maybe, in fact, they are using nonoperative invasive options (interventional radiology etc) available to them to their full extent and in the best possible way. But no one can doubt the fact that rarely performed operative procedures are more likely to result in a bad outcome if performed by a surgeon unfamiliar with performing them. It is very possible that continuous involvement and availability of older-generation trauma surgeons may dilute these bad outcomes in severely injured patients and especially at large trauma centers that are more likely to be on the receiving end of these patients; however, this allows newer-generation surgeons the opportunity to gain experience working with their more experienced colleagues and essentially learn on the job. Another source of expertise comes from surgeons who were deployed to areas of conflicts during the last 15 years. As these surgeons are retiring from the armed forces, they are becoming part of trauma surgery teams with invaluable input and expertise. The number of surgeries that our trainees perform should not be the only parameter to be evaluated. This is definitely a complex issue, and with this survey, we bring up one of the options that could be used in our attempt to find viable solutions to this problem.
Despite the interesting findings of this survey, the reported data should be interpreted with caution given the inherent limitations of an electronic survey, including selection, recall, and response bias. Despite the relatively high response rate for similar surveys, only about half of eligible participants answered the questionnaire in full. The number of reported operative procedures could not be verified, and the degree of participation (ie, primary surgeon vs first or second assistant) could not be elucidated. The perceived increased level of confidence in performing trauma-related surgical procedure does not necessarily translate into surgical competence.
In conclusion, an international rotation at a high-volume trauma center offers a unique hands-on experience that may enhance confidence and competence in the management of trauma patients and in performing trauma-related surgical procedures. These rotations can supplement the constantly declining volume of operative trauma in developed countries. Integrating these rotations into surgical training and ensuring not only standardization of the experience but also financial support will offer the future generation of trauma surgeons with a distinct opportunity to develop their skills and improve the outcomes of trauma patients.
Author Contribution
Study conception and design: Galinos Barmparas, MD; Andrew J. Nicol, MBChB, FCS, PhD. Acquisition of data: Galinos Barmparas, MD; Navpreet K. Dhillon, MD; Pradeep H. Navsaria, MBChB, FCS. Analysis and interpretation of data: Galinos Barmparas, MD; Navpreet Dhillon, MD; Pradeep H. Navsaria, MBChB, FCS. Literature Review: Galinos Barmparas, MD; Sorin Edu, MD, FCS. Drafting of manuscript: Galinos Barmparas, MD; Pradeep H. Navsaria, MBChB, FCS. Critical revision: Bruce L. Gewertz, MD; Eric J. Ley, MD; Daniel R. Margulies, MD; Andrew J. Nicol, MBChB, FCS, PhD.
Conflict of Interest
The authors have no conflicts of interest to report
Funding Sources
The authors have received no financial support in relation to this manuscript.
Contributor Information
Galinos Barmparas, Email: Galinos.Barmparas@cshs.org.
Pradeep H. Navsaria, Email: Pradeep.Navsaria@uct.ac.za.
Navpreet K. Dhillon, Email: Navpreet.Dhillon@cshs.org.
Sorin Edu, Email: Sorin.Edu@uct.ac.za.
Daniel R. Margulies, Email: Daniel.Margulies@cshs.org.
Eric J. Ley, Email: Eric.Ley@cshs.org.
Bruce L. Gewertz, Email: Bruce.Gewertz@cshs.org.
Andrew J. Nicol, Email: Andrew.Nicol@uct.ac.za.
References
- 1.Engels P.T., Bradley N.L., Ball C.G. The current state of resident trauma training: are we losing a generation? Can J Surg. 2018;61(3):153. doi: 10.1503/CJS.014417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kristiansen T., Søreide K., Ringdal K.G., Rehn M., Krüger A.J., Reite A. Trauma systems and early management of severe injuries in Scandinavia: review of the current state. Injury. 2010;41(5):444–452. doi: 10.1016/j.injury.2009.05.027. [DOI] [PubMed] [Google Scholar]
- 3.Strumwasser A., Grabo D., Inaba K., Matsushima K., Clark D., Benjamin E. Is your graduating general surgery resident qualified to take trauma call? A 15-year appraisal of the changes in general surgery education for trauma. J Trauma Acute Care Surg. 2017;82(3):470–480. doi: 10.1097/TA.0000000000001351. [DOI] [PubMed] [Google Scholar]
- 4.Drake F.T., Van Eaton E.G., Huntington C.R., Jurkovich G.J., Aarabi S., Gow K.W. ACGME case logs: surgery resident experience in operative trauma for two decades. J Trauma Acute Care Surg. 2012;73(6):1500–1506. doi: 10.1097/TA.0b013e318270d983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacobs L.M., Burns K.J., Kaban J.M., Gross R.I., Cortes V., Brautigam R.T. Development and evaluation of the advanced trauma operative management course. J Trauma-Injury Infect Crit Care. 2003;55(3):471–479. doi: 10.1097/01.ta.0000059445.84105.26. [DOI] [PubMed] [Google Scholar]
- 6.Kuhls D.A., Risucci D.A., Bowyer M.W., Luchette F.A. Advanced surgical skills for exposure in trauma: a new surgical skills cadaver course for surgery residents and fellows. J Trauma Acute Care Surg. 2013;74(2):664–670. doi: 10.1097/TA.0b013e31827d5e20. [DOI] [PubMed] [Google Scholar]
- 7.Ali J., Ahmed N., Jacobs L.M., Luk S.S. The Advanced Trauma Operative Management course in a Canadian residency program. Can J Surg. 2008;51(3):185–189. %3CGo. [PMC free article] [PubMed] [Google Scholar]
- 8.Kaban J.M., Stone Melvin E.J., Dayama A., Safadjou S., Reddy S.H., Simon R. Does resident trauma exposure affect advanced trauma operative management course experience? Am Surg. 2016;82(3):212–215. %3CGo. [PubMed] [Google Scholar]
- 9.Bowyer M.W., Kuhls D.A., Haskin D., Sallee R.A., Henry S.M., Garcia G.D. Advanced surgical skills for exposure in trauma (ASSET): the first 25 courses. J Surg Res. 2013;183(2):553–558. doi: 10.1016/j.jss.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 10.Borman K.R., Vick L.R., Biester T.W., Mitchell M.E. Changing demographics of residents choosing fellowships: long-term data from the American Board of Surgery. J Am Coll Surg. 2008;206(5):782–789. doi: 10.1016/j.jamcollsurg.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 11.Ferrada P., Ferrada R., Aboutanos M., Ivatury R.R. International surgical rotation: a prodigious personal and professional maturation. Am Surg. 2015;81(5):E230–E231. %3CGo. [PubMed] [Google Scholar]
- 12.Nicol A., Knowlton L.M., Schuurman N., Matzopoulos R., Zargaran E., Cinnamon J. Trauma surveillance in Cape Town, South Africa: an analysis of 9236 consecutive trauma center admissions. JAMA Surg. 2014;149(6):549–556. doi: 10.1001/jamasurg.2013.5267. [DOI] [PubMed] [Google Scholar]
- 13.Navsaria P.H., Nicol A.J., Krige J.E., Edu S. Selective nonoperative management of liver gunshot injuries. Ann Surg. 2009;249(4):653–656. doi: 10.1097/SLA.0b013e31819ed98d. [DOI] [PubMed] [Google Scholar]
- 14.Navsaria P.H., Nicol A.J., Edu S., Gandhi R., Ball C.G. Selective nonoperative management in 1106 patients with abdominal gunshot wounds. Ann Surg. 2015;261(4):760–764. doi: 10.1097/SLA.0000000000000879. [DOI] [PubMed] [Google Scholar]
- 15.Nicol A.J., Navsaria P.H., Hommes M., Ball C.G., Edu S., Kahn D. Sternotomy or drainage for a hemopericardium after penetrating trauma. Ann Surg. 2014;259(3):438–442. doi: 10.1097/SLA.0b013e31829069a1. [DOI] [PubMed] [Google Scholar]
- 16.Martin VA. Mid-year population estimates 2017.; 2018. www.statssa.gov.zainfo@statssa.gov.za. .
- 17.World Bank Global economic prospects: sub-Saharan Africa a fragile recovery. 2017. http://pubdocs.worldbank.org/en/710231493655506452/Global-Economic-Prospects-June-2017-Regional-Overview-SSA.pdf
- 18.Global peace index: measuring peace in a complex world. 2017. www.economicsandpeace.org
- 19.Africa Check. FACTSHEET: South Africa’s crime statistics for 2016/17 | Africa Check. https://africacheck.org/factsheets/south-africas-crime-statistics-201617/ Published 2017.
- 20.Road Traffic Management Corporation Arrive alive. https://www.arrivealive.mobi/road-traffic-management-corporation
- 21.World Health Organizationi Global status report on road safety time for action. 2009. www.who.int/violence_injury_prevention
- 22.Roux D., Labuschagne F.J.J. Prepared for: road traffic management corporation research and development CSIR Built Environment Transport Management, Design and Systems. https://www.arrivealive.co.za/documents/Cost-of-Crashes-in-South-Africa-RTMC-September-2016.pdf
- 23.Goosen J., Bowley D.M., Degiannis E., Plani F. Trauma care systems in South Africa. Injury. 2003;34(9):704–708. doi: 10.1016/S0020-1383(03)00153-0. [DOI] [PubMed] [Google Scholar]
- 24.Degiannis E., Levy R.D., Velmahos G.C., Potokar T., Florizoone M.G., Saadia R. Gunshot injuries of the head of the pancreas: conservative approach. World J Surg. 1996;20(1):68–71. doi: 10.1007/s002689900012. discussion 72. http://www.ncbi.nlm.nih.gov/pubmed/8588416. Accessed December 4, 2018. [DOI] [PubMed] [Google Scholar]
- 25.Demetriades D., Charalambides D., Lakhoo M. Physical examination and selective conservative management in patients with penetrating injuries of the neck. Br J Surg. 1993;80(12):1534–1536. doi: 10.1002/bjs.1800801213. http://www.ncbi.nlm.nih.gov/pubmed/8298918. Accessed December 4, 2018. [DOI] [PubMed] [Google Scholar]
- 26.Karmy-Jones R., Namias N., Coimbra R., Moore E.E., Schreiber M., McIntyre R. Western Trauma Association critical decisions in trauma. J Trauma Acute Care Surg. 2014;77(6):994–1002. doi: 10.1097/TA.0000000000000426. [DOI] [PubMed] [Google Scholar]
- 27.Sperry J.L., Moore E.E., Coimbra R., Croce M., Davis J.W., Karmy-Jones R. Western Trauma Association critical decisions in trauma. J Trauma Acute Care Surg. 2013;75(6):936–940. doi: 10.1097/TA.0b013e31829e20e3. [DOI] [PubMed] [Google Scholar]
- 28.Spain D.A., Miller F.B. Education and training of the future trauma surgeon in acute care surgery: trauma, critical care, and emergency surgery. Am J Surg. 2005;190(2):212–217. doi: 10.1016/j.amjsurg.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 29.Jurkovich G.J., Anderson K., Britt L.D., Born C.T., Cioffi W.G., Esposito T.J. The acute care surgery curriculum. J Trauma-Injury Infect Crit Care. 2007;62(3):553–556. doi: 10.1097/TA.0b013e3180327c18. [DOI] [Google Scholar]
- 30.Kelly E., Rogers Selwyn O.J. Graduate medical education in trauma/critical care and acute care surgery defining goals for a new workforce. Surg Clin North Am. 2012;92(4):1055. doi: 10.1016/j.suc.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 31.Park C.J., Armenia S.J., Cowles R.A. Trends in routine and complex hepatobiliary surgery among general and pediatric surgical residents: what is the next generation learning and is it enough? J Surg Educ. 2019;76(4):1005–1014. doi: 10.1016/j.jsurg.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 32.The National Academies of Science E and M (NASEM) A national trauma care system. 2016. http://nationalacademies.org/hmd/~/media/Files/ReportFiles/2016/Trauma-Care/Trauma-Care-Recs.pdf
- 33.Drake F.T., Aarabi S., Garland B.T., Huntington C.R., McAteer J.P., Richards M.K. Accreditation Council for Graduate Medical Education (ACGME) surgery resident operative logs. Ann Surg. 2017;265(5):923–929. doi: 10.1097/SLA.0000000000001738. [DOI] [PubMed] [Google Scholar]
- 34.Ferrada P., Ivatury R.R., Spain D.A., Davis K.A., Aboutanos M., Fildes J.J. International rotations: A valuable source to supplement operative experience for acute-care surgery, trauma, and surgical critical care fellows. J Trauma Acute Care Surg. 2017;82(1):51–57. doi: 10.1097/TA.0000000000001307. [DOI] [PubMed] [Google Scholar]
- 35.Leow J.J., Kingham T.P., Casey K.M., Kushner A.L. Global surgery: thoughts on an emerging surgical subspecialty for students and residents. J Surg Educ. 2010;67(3):143–148. doi: 10.1016/j.jsurg.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 36.Ginwalla R.F., Rustin R.B. The “global surgeon”: is it time for modifications in the American surgical training paradigm? J Surg Educ. 2015;72(4):e100–e103. doi: 10.1016/j.jsurg.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 37.Monroe-Wise A., Kibore M., Kiarie J., Nduati R., Mburu J., Drake F.T. The Clinical Education Partnership Initiative: an innovative approach to global health education. BMC Med Educ. 2014;14:1043. doi: 10.1186/s12909-014-0246-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Merchant A.I., Walters C.B., Valenzuela J., McQueen K.A., May A.K. Creating a global acute care surgery fellowship to meet international need. J Surg Educ. 2017;74(5):780–786. doi: 10.1016/j.jsurg.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 39.Boeck M.A., Nagarajan N., Swaroop M. The role of public health in a global surgery fellowship. J Surg Educ. 2015;72(5):776–777. doi: 10.1016/j.jsurg.2015.06.016. [DOI] [PubMed] [Google Scholar]
- 40.Yan H., Maximus S., Koopmann M., Keeley J., Smith B., de Virgilio C. Vascular trauma operative experience is inadequate in general surgery programs. Ann Vasc Surg. 2016;33:94–97. doi: 10.1016/j.aysg.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 41.Spence R.T., Scott J.W., Haider A., Navsaria P.H., Nicol A.J. Comparative assessment of in-hospital trauma mortality at a South African trauma center and matched patients treated in the United States. Surgery. 2017;162(3):620–627. doi: 10.1016/j.surg.2017.04.024. [DOI] [PubMed] [Google Scholar]