Abstract
Background
Laparoscopic peritoneal dialysis catheter placement has expanded indications, although a relative paucity of data exists about the best configuration for improving outcomes. The purpose of this study is to investigate the role of different catheter configurations and pelvic fixation on catheter and patient outcomes.
Methods
Retrospective chart review of patients undergoing peritoneal dialysis catheter implantation between January 1, 2013, and December 31, 2016. All procedures were conducted laparoscopically at a single center. Statistical analyses were conducted using Stata/SE 14.2.
Results
Buried catheter configuration was a statistically significant predictor of peritonitis compared to unburied configuration (P = 0.008). Buried catheter was exteriorized at 100 days (SD 107.8). A longer length of time to exteriorization significantly correlated with peritonitis, need for revision, and need for revision pelvic fixation (P < 0.05). Additionally, initial pelvic fixation was a significant predictor of revision (HR 3.94).
Conclusions
Peritoneal dialysis catheter placement via a laparoscopic approach can be successfully performed in a diverse patient mix with positive results. However, buried catheter configuration and prophylactic pelvic fixation should be carefully employed in select patients.
INTRODUCTION
End-stage renal disease (ESRD) imparts a significant economic burden and requires a complex infrastructure to maintain patients on dialysis. According to the November 2016 US Renal Data System Report published by the National Institute of Diabetes and Digestive and Kidney Disease, there were 678,383 existing cases of ESRD in the United States in 2014, with an unadjusted incidence rate of 370 per million per year [1].
Hemodialysis (HD) and peritoneal dialysis (PD) are considered in the management of ESRD, with the former more commonly utilized in the United States [1]. However, recent reports indicate that PD is rising in popularity and serves as an attractive option for ESRD, likely due to its ease of use, greater patient independence, and lower expense [2], [3]. According to a global trends study, 197,000 patients (11% of the dialysis population) are treated with PD worldwide, with an increasing rate of use in both developing and developed countries [4]. Given this trend, PD has increasingly become the focus of study with the goal of improving its initiation and longitudinal delivery for ESRD patients.
Over the past few decades, there have been significant advancements in optimizing the implementation of PD. Clinical practice has shifted from an open approach for catheter insertion to a less invasive laparoscopic approach. With the laparoscope, selective patients can undergo omentopexy by using basic intracorporeal suturing techniques. This involves attachment of the omentum to the abdominal wall, reducing the incidence of omental entrapment, catheter migration, outflow obstruction, and risk of herniation [5], [6], [7], [8]. In addition, fixing the catheter itself to the abdominal wall has also been used to secure the intra-abdominal position and prevent migration. Burying a PD catheter while the patient is approaching dialysis further allows us to externalize it when needed in an effort to avoid tunneled dialysis catheter placement. This technique is in contradistinction to the immediate use catheter that is externalized at the time of implantation.
Despite the potential value of laparoscopy to expand the indications of PD catheter placement, little data has been published on the role of catheter configuration and laparoscopic placement with catheter fixation in the pelvis affecting short-term and long-term outcomes. This paper investigated this topic in order to analyze the impact of advancements in peritoneal dialysis catheter placement and how it affects patient outcomes.
MATERIALS AND METHODS
Study design. A retrospective review of all patients undergoing PD catheter placement at a large multisite tertiary care center (University of Pittsburgh Medical Center) between January 1, 2013, and December 31, 2016, was carried out. All procedures were conducted with laparoscopic assistance by a single vascular surgeon. Patient data was extracted through chart review with follow-up until February 1, 2017. Information collected includes patient demographics, comorbidities, medications, history of abdominal surgeries, catheter characteristics (placement configuration and use of pelvic fixation), successful initial use, revision status (need for revision, number of revisions, and dates of revisions), peritonitis status, and catheter survival status (with date of removal).
Surgical Technique. The patient was placed in a supine position on the operating table, general anesthesia was administered, and the abdomen was prepped and draped in a sterile fashion. A 1 cm incision was made approximately 2 fingerbreadths below the subcostal margin and the surgeon entered the abdomen using a 5 mm Optiview port (Ethicon Inc, Somerville, NJ). The abdomen was subsequently insufflated, a second 2 cm incision was made just lateral to the umbilicus, and another 5 mm Optiview port was inserted at a 60° angle aiming towards the pelvis. The pigtail catheter (Medtronic, Minneapolis, MN) was subsequently unfurled deep in the pelvis. The abdomen was then deflated and the two portions of the catheter were attached with a titanium coupler followed by subsequent tunneling of the catheter to the subcostal incision and then out laterally onto the abdomen. A depiction of the laparoscopic implantation technique is shown in Fig 1.
Fig 1.
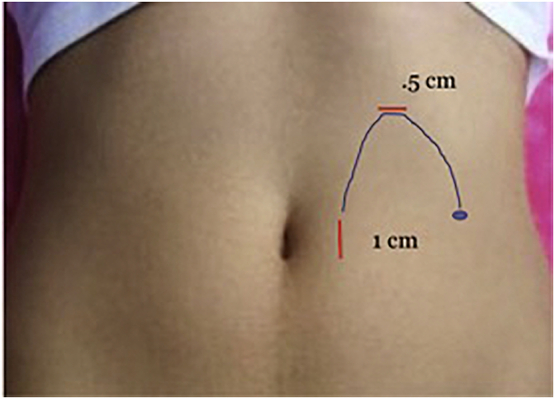
Laparoscopic implantation technique. The red lines indicate the location of the insertion of the Optiview ports. The blue line indicates the trajectory of the catheter implantation and the blue dot indicates the location of catheter exit.
For the unburied catheter configuration, the catheter was tunneled from the subcostal incision to the predetermined exit point above the belt line (as decided during the pre-operative evaluation of the patient in the sitting position). For buried catheter placement, the catheter was tunneled underneath the skin with the metal trocar and an incision was made laterally on the abdomen for tunneling. The catheter was then tested and ligated, allowing it to retract under the skin. This allowed easy access for the externalization procedure at a later date. When the catheter was pexied, a Carter-Thomason device (CooperSurgical, Inc, Trumbull, CT) was used to secure the catheter into the pelvis.
After placement, the catheter was flushed with 240 mL of normal saline to check for easy injection and spontaneous drainage. Lastly, the catheter was ligated and allowed to retract under the skin. All wounds were irrigated and then closed with 3-0 absorbable braided sutures followed by a running subcuticular monofilament for the final skin closure. Fig 2 shows the configuration of a functioning peritoneal dialysis catheter.
Fig 2.

Functioning peritoneal dialysis catheter. This is the configuration of a functioning peritoneal dialysis catheter.
Statistical analyses. Student’s t test was used for continuous variables and chi-squared test was used for categorical variables. Pearson correlation analysis was used for analyzing the association between continuous variables. Pearson χ2 analysis was used for analyzing the association between categorical variables. Multivariate analysis was used for analyzing the association between continuous and categorical variables. Kaplan-Meier and Cox regression analysis were used for analyzing outcome predictors. All statistical analyses were conducted using Stata/SE 14.2 (StataCorp, College Station, TX). The key outcomes were successful initial catheter use, need for catheter revision, development of peritonitis, and catheter survival.
RESULTS
The study cohort consisted of 165 patients, 93 (56%) of whom were male. Mean age was 58.5 years (SD 14.6, range 20–89) and mean body mass index (BMI) was 30.2 kg/m2 (SD 6.6, range 19.2–50.7). Eighty-four (50.9%) patients had a history of prior abdominal operations. These results are summarized in Table 1. BMI classification was found to be statistically significant between the buried and unburied groups, with the buried group being more significantly associated with patients from a higher BMI class.
Table 1.
Patient demographics
| Variable | N (%) | Rate of initial successful use (%) | Revision rate (%) | Buried vs. unburied configuration (P value) | Pelvic fixation versus no pelvic fixation (P value) |
|---|---|---|---|---|---|
| Gender | .15 | .50 | |||
| Male | 93 (56.4) | ||||
| Female | 72 (43.6) | ||||
| BMI (kg/m2) | .019 | .16 | |||
| Class 1 (< 18.5) | 0 (0) | 0/0 (0) | 0/0 (0%) | ||
| Class 2 (18.5–24.9) | 36 (21.8) | 29/32 (90.6) | 22/36 (61.1) | ||
| Class 3 (25.0–29.9) | 52 (31.5) | 41/48 (85.4) | 18/52 (34.6) | ||
| Class 4 (30.0–34.9) | 42 (25.5) | 31/36 (86.1) | 15/42 (35.7) | ||
| Class 5 (35.0–39.9) | 17 (10.3) | 13/15 (86.7) | 9/17 (52.9) | ||
| Class 6 (≥ 40) | 18 (10.9) | 17/17 (100) | 3/18 (16.7) | ||
| Prior abdominal surgery | .40 | .92 | |||
| Yes | 84 (50.9) | ||||
| No | 81 (40.1) |
One-hundred fifteen patients (69.7%) received a buried catheter placement that was exteriorized at a later date and 50 patients (30.3%) received an unburied catheter placement ready for immediate use. Twenty-nine patients (17.6%) underwent pelvic fixation, with 13 (44.8%) of those pexied during the initial placement. One hundred five patients (63.6%) required no revision after initial catheter placement, 36 patients (21.8%) required one revision, and 23 patients (13.9%) required more than one revision. The overall revision success rate was 61.0%. One hundred thirty-one patients (88.5%) had first successful catheter use without need for immediate revision to allow for proper functionality, with 49 (37.4%) of those requiring one or more subsequent revisions at a later date after discovery of a catheter complication. Mean catheter survival, measured from the date of catheter placement to removal, was 536 days (SD 401.3). Mean time till first revision for those 59 patients requiring revision was 362 days (SD 459.9).
Peritonitis occurred in 19 patients (12.8%) (18/102 in the buried group and 1/47 in the unburied group) at a mean of 481 days (SD 341.3). All 19 catheters (except one due to lack of definitive data found on catheter removal) were eventually removed after the failure to respond to antibiotics. A statistically significant association was found between buried catheter configuration and the incidence of peritonitis (P = .008). However, buried catheter configuration was not significantly associated with revision or first successful catheter use. The buried catheter was exteriorized at a mean of 100 days (SD 107.8). These results are summarized in Table 2.
Table 2.
Catheter characteristics and outcomes
| Variable | Buried N (%) | Unburied N (%) | P value |
|---|---|---|---|
| Catheter Configuration | 115 (69.7) | 50 (30.3) | |
| Initial Pelvic Fixation | 6 (5.22) | 7 (14.0) | .054 |
| Revision Count | |||
| 0 | 74 (64.3) | 31 (62.0) | |
| 1 | 24 (20.9) | 12 (24.0) | |
| 2 | 12 (10.4) | 5 (10.0) | .893 |
| 3 | 3 (2.60) | 1 (2.00) | |
| 4 | 2 (1.74) | 0 (0) | |
| Revision pelvic fixation | 11 (9.57) | 7 (14.0) | .411 |
| First successful use | 89 (77.4) | 42 (84.0) | .224 |
| Need for revision | 41 (35.7) | 18 (36.0) | .966 |
| Peritonitis | 18 (15.7) | 1 (2.00) | .008 |
| Catheter removal | 53 (46.1) | 16 (32.0) | .047 |
By logistic regression, a longer length of time until exteriorization significantly correlated with the incidence of peritonitis, need for revision, and need for a revision pelvic fixation (P < .05). However, it did not significantly correlate with time to first revision or days of catheter survival by Pearson’s correlation analysis. While initial pelvic fixation was not associated with first successful catheter use, it was found to be the only significant predictor of revision by Cox regression analysis (HR 3.94). Lastly, BMI ≥ 30 (46.7% of patients) or prior history of abdominal surgeries did not significantly affect rates of successful use, need for revision, or peritonitis.
DISCUSSION
Peritoneal dialysis has been gaining popularity as an attractive modality compared to HD for the management of patients with ESRD due to its lower cost and improved patient quality of life, especially in developing countries with limited access to hemodialysis centers [4]. The economic benefits of administering and maintaining patients on PD, as compared to HD, is beneficial from a health systems perspective, reducing a significant portion of the burden of cost that accompanies ESRD management, both in the short-term and long-term setting. Berger et al [3] reported a two times higher likelihood of hospitalization in the first 12 months after initiation of HD as opposed to PD, with median healthcare costs higher by $43,510 for HD. Atapour et al [9] likewise found a statistically significant difference between HD and PD in terms of factors such as diagnostic tests, drugs, and hospitalization, with higher costs for HD.
Several papers have been published on the role of different surgical techniques for peritoneal dialysis catheter placement on patient outcomes. Manipulation of the omentum has been employed in this context, with omentectomy involving excision of part of the omentum and omentopexy involving attachment of the omentum to the abdominal wall, both performed with the goal of reducing omental entrapment of the catheter. A shift from the use of omentectomy to omentopexy was seen with better catheter outcomes for the latter from the standpoint of flow obstruction when employed in select patients [10]. Another study also showed a higher rate of dysfunction-free and overall catheter survival in patients who underwent advanced laparoscopy utilizing rectus sheath tunneling, selective omentopexy, and adhesiolysis [11]. Additionally, laparoscopic technique was found to have a lower incidence of catheter replacement or revision when compared to the traditional open technique [12]. Despite this evidence, the definitive influence of omentopexy still remains to be determined with a prospective study.
On the other hand, the role of pelvic fixation, which involves securing the catheter tip into the pelvis, has not been studied as extensively. A small cohort study consisting of 19 patients who underwent catheter placement with suture fixation in the pelvis showed loss of function in only one of the catheters in the long-term setting [13]. Another study showed a longer time to catheter migration with pelvic fixation as opposed to the open placement technique, but a lack of effect on catheter survival [14]. Some of these findings were confirmed in a study conducted in children, which found a lower number of exit site infections and longer time to catheter migration with pelvic fixation as opposed to the open placement technique [15]. A larger cohort study of 82 patients who underwent preperitoneal tunneling and catheter fixation in the pelvis showed seven patients who presented with catheter migration needing laparoscopic reintervention [16]. In light of these papers, our analyses contribute to the growing literature on the topic of initial pelvic fixation by reporting its role as the single most important predictor of need for subsequent catheter revision. This finding has not been previously reported in the literature. One explanation of this would be that the catheter was initially functioning when first tested in the operating room and was secured in the pelvis in an attempt to remedy dysfunction. This would place this group of patients at higher risk for catheter failure and subsequent need for revision. We believe this is a significant finding that should be investigated further in order to determine the functionality of pelvic fixation in the short-term and long-term setting that can potentially affect catheter survival. However, one of the primary limitations of our dataset is its retrospective nature, the limited number of patients who underwent pelvic fixation, and the clinical indications which were clinician-dependent that impedes determination of the context of fixation. While pelvic fixation has been deemed safe and useful as per previous literature, it needs to be investigated in a larger prospective study to evaluate its utility in PD catheter placement.
The role of catheter configuration on patient outcomes has been studied to a limited degree as well. Data presented in a prospective study looking at subcutaneously buried versus unburied catheter placement technique showed an overall similar risk of peritonitis development [17]. Comparable findings were reported by another prospective study investigating the Moncrief-Popovich design and insertion technique, showing no difference in incidence of peritonitis [18]. Another observational study showed a reduced rate of surgical, mechanical, and infectious complications with the buried placement technique, although the primarily descriptive nature of the study limited its validity as well as reproducibility [19].
In comparison, our analyses included a large patient cohort over the course of four years. Our results showcase an objective experience of catheter placement at a single center, providing evidence for a significant impact of catheter configuration on the development of a potentially lethal infectious complication. It is important to recognize this trend in order to avoid peritonitis in an already compromised patient population that presents with multiple comorbidities that could complicate management. A possible source of infection leading to peritonitis is the requirement of skin manipulation two times (first at insertion and then again at exteriorization) as opposed to singular manipulation in an unburied catheter, which potentially increases the risk of exposure to microbes to the catheter entry site and eventually the peritoneal cavity. Given the limited number of studies that has been conducted investigating this issue, our results present an impetus requiring further research for determination of patient risk and outcomes.
Furthermore, our findings indicating a statistically significant correlation between timing of catheter exteriorization in the buried configuration group and the incidence of peritonitis, need for revision, and need for a revision catheter fixation point to a previously undiscovered influence of catheter configuration and length of subcutaneous burying on patient outcomes. The dual skin manipulation coupled with long-term burying of a foreign device in a patient’s abdominal wall can impart a potentially harmful complication that needs to be taken into consideration for cautious selection of patients meeting criteria for peritoneal dialysis. The higher incidence of peritonitis in the buried configuration group associated with greater lengths of burying may even provide evidence for the utility of burying the catheter primarily in patients who are very close to dialysis.
While both pelvic fixation and buried catheter configuration have been studied in the past and deemed to be safe techniques employed for PD catheter placement, our findings provide evidence to show certain drawbacks that need to be further investigated in a prospective manner. Nevertheless, our dataset which included all patients who underwent laparoscopic placement of a PD catheter support the use of this minimally-invasive technique in a patient cohort that presents with multiple comorbidities, making PD placement a safe and reliable method that can be utilized in a diverse patient mix. While the use of advanced techniques such as pelvic fixation are still under development and prone to complications, laparoscopic PD placement has paved the way for the implementation of this form of dialysis in a wider patient population.
In conclusion, PD catheter placement via laparoscopy has become the standard of care for most clinical practices. It is a technique that can be effectively performed in a heterogeneous patient population with favorable results, as shown in our study. However, given its association with peritonitis, the use of buried catheters should be avoided if at all possible. We would recommend placement of unburied catheters when patients near dialysis in order to avoid this complication. Our data would suggest that pelvic fixation at the initial catheter placement should be used sparingly as it is a predictor of catheter failure and need for revision.
DECLARATIONS
Author contribution
Study conception and design: Pandya, Hager; Acquisition of data: Pandya; Analysis and interpretation of data: Pandya, Wagner; Drafting of manuscript: Pandya, Wagner, Hager;
Critical revision: Pandya, Wagner, Yuo, Eslami, Singh, Hager.
Declaration of competing interest
None.
Funding sources
None.
Financial disclosures
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
None.
References
- 1.United States Renal Data System . National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2016. 2016 USRDS annual data report: Epidemiology of kidney disease in the United States. [Google Scholar]
- 2.Tokgoz B. Clinical advantages of peritoneal dialysis. Perit Dial Int. 2009;29(Suppl. 2):S5961. [PubMed] [Google Scholar]
- 3.Berger A., Edelsberg J., Englese G.W. Cost comparison of peritoneal dialysis versus hemodialysis in end-stage renal disease. Am J Manag Care. 2009;15(8):509–518. [PubMed] [Google Scholar]
- 4.Jain A.K., Blake P., Cordy P., Garg A.X. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23(3):533–544. doi: 10.1681/ASN.2011060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hauch A.T., Lundberg P.W., Paramesh A.S. Laparoscopic techniques enable peritoneal dialysis in the difficult abdomen. JSLS. 2014;18(4) doi: 10.4293/JSLS.2014.002334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peppelenbosch A, van Kuijk WH, Bouvy ND, et al.. Peritoneal dialysis catheter placement technique and complications. NDT Plus. 2008;1(Suppl 4):iv23-iv28. [DOI] [PMC free article] [PubMed]
- 7.Ko J., Ra W., Bae T. Two-port laparoscopic placement of a peritoneal dialysis catheter with abdominal wall fixation. Surg Today. 2009;39(4):356–358. doi: 10.1007/s00595-008-3877-5. [DOI] [PubMed] [Google Scholar]
- 8.Park Y.S., Min S.I., Kim D.K. The outcomes of percutaneous versus open placement of peritoneal dialysis catheters. World J Surg. 2014;38(5):1058–1064. doi: 10.1007/s00268-013-2346-5. [DOI] [PubMed] [Google Scholar]
- 9.Atapour A., Eshaghian A., Taheri D., Dolatkhah S. Hemodialysis versus peritoneal dialysis, which is cost-effective? Saudi J Kidney Dis Transpl. 2015;26(5):962–965. doi: 10.4103/1319-2442.164578. [DOI] [PubMed] [Google Scholar]
- 10.Crabtree J.H. Selected best demonstrated practices in peritoneal dialysis access. Kidney Int Suppl. 2006;(103):S27–S37. doi: 10.1038/sj.ki.5001913. [DOI] [PubMed] [Google Scholar]
- 11.Krezalek M.A., Bonamici N., Lapin B. Laparoscopic peritoneal dialysis catheter insertion using rectus sheath tunnel and selective omentopexy significantly reduces catheter dysfunction and increases peritoneal dialysis longevity. Surgery. 2016;160(4):924–935. doi: 10.1016/j.surg.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 12.Gajjar AH, Rhoden DH, Kathuria P, et al. Peritoneal dialysis catheters: laparoscopic versus traditional placement techniques and outcomes. Am J Surg. 2007;194(6):872-875; discussion 875-876. [DOI] [PubMed]
- 13.Watson DI, Paterson D, Bannister K. Secure placement of peritoneal dialysis catheters using a laparoscopic technique. Surg Laparosc Endosc 1996 Feb;6(1):35-7. [PubMed]
- 14.Soontrapornchai P., Simapatanapong T. Comparison of open and laparoscopic secure placement of peritoneal dialysis catheters. Surg Endosc. 2005;19(1):137–139. doi: 10.1007/s00464-004-8156-y. [DOI] [PubMed] [Google Scholar]
- 15.Copeland D.R., Blaszak R.T., Tolleson J.S. Laparoscopic Tenckhoff catheter placement in children using a securing suture in the pelvis: comparison to the open approach. J Pediatr Surg. 2008;43(12):2256–2259. doi: 10.1016/j.jpedsurg.2008.08.056. [DOI] [PubMed] [Google Scholar]
- 16.Gunes M.E., Uzum G., Koc O. A modified method in laparoscopic peritoneal catheter implantation: the combination of preperitoneal tunneling and pelvic fixation. ISRN Surg. 2013;2013 doi: 10.1155/2013/248126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Daneilsson A., Blohmé L., Tranaeus A. A prospective randomized study of the effect of a subcutaneously "buried" peritoneal dialysis catheter technique versus standard technique on the incidence of peritonitis and exitsite infection. Perit Dial Int. 2002;22(2):2119. [PubMed] [Google Scholar]
- 18.Wu C.C., Su P.F., Chiang S.S. A prospective study to compare subcutaneously buried peritoneal dialysis catheter technique with conventional technique. Blood Purif. 2007;25(3):229–232. doi: 10.1159/000101027. [DOI] [PubMed] [Google Scholar]
- 19.Kawabata C., Kinugasa S., Kamijo Y. Correction of peritoneal catheter obstruction using a neonatal bronchoscope. Perit Dial Int. 2015;35(1):101–103. doi: 10.3747/pdi.2012.00288. [DOI] [PMC free article] [PubMed] [Google Scholar]


