Abstract
Background
The aim of this study was to evaluate the long-term follow-up results of different management modalities in treating primary uncomplicated lower limb female varicosities.
Methods
A prospective study took place within a 3-year period from June 2010 until May 2012. Patients were divided into 3 groups: group I (n = 35) included those who underwent open surgical treatment. Group II (n = 25) included those who subjected to ultrasound-guided foam sclerotherapy (USGFS). While group III (n = 20) included those who treated with endovenous laser therapy (EVLT). The patients were followed up for 6 years.
Results
All selected patients were female aged from 35-62 years with a mean of 47 ± 7.6 years. Thirty-five patients (43.75%) were treated surgically by saphenofemoral junction disconnection (SFJD), and great saphenous vein (GSV) stripping; 25 patients (31.25%) with ultrasound-guided foam sclerotherapy and the remaining 20 patients (25%) were treated with endovenous laser therapy. A significant success rate of GSV ablation was obtained for the endovenous laser therapy treated group over the ultrasound-guided foam sclerotherapy treated patients (P = .023). There was no significant difference between the surgically treated group and those group treated with endovenous laser therapy (P = .85). Recurrence was observed following long-term follow-up after 6 years in 8.5% in group I, 36% in group II, and 10% in group III, respectively. Venous clinical severity score (VCSS) and health-related quality of life score (HRQOLS) improved significantly in all treated groups.
Conclusions
Long-term follow-up of patients with primary superficial varicosities among females is mandatory to elucidate the postoperative recurrence, especially those who underwent ultrasound-guided foam sclerotherapy. In addition to the observation of the development of newly formed varicosities in susceptible individuals which might develop later following long-term follow-up.
INTRODUCTION
Most patients with venous insufficiency presented with varicose veins. Lower limb superficial varicosities were considered as one of the chronic common venous problems affecting females more than males with an incidence of 20–60% of the whole population. Patients with varicose veins can be presented with ankle edema, disfigurement, chronic eczema, disability, ulceration, bleeding, foot deformities and impairment in the life quality [1], [2], [3]. Different management options have evolved in its treatment besides the traditional tools [4]. Moreover, these different modalities of treating varicose veins are encountered according to the topographic data that include; axial vein varicosities i.e. the long and short saphenous veins, collateral varicosities, incompetent perforator, spider and telangiectatic veins [5]. The aim of superficial varicose vein treatment was to correct the anatomical and hemodynamic disorders caused by its development [6]. Varicosities of the great saphenous vein (GSV) can be surgically treated using saphenofemoral junction disconnection (SFJD), ligation and stripping; in addition to, multiple hook phlebectomies [7], [8], [9], [10], [11], [12]. Furthermore, the minimally invasive EVLT has been adopted with the aim of having equal or better results than SFJD and stripping technique [13], [14], [15]. On the other hand, injection of sclerosing materials as foam under ultrasound guidance has also gained wide popularity [16], [17]. Based on the current guidelines [16], [18], [19], short or mid-term follow-up was recommended for patients treated with EVLT as a result of GSV reflux. Nowadays, and because of the high incidence of recurrent varicosities, long-term follow-up is mandatory, to evaluate the results of different management modalities.
MATERIALS AND METHODS
The study was initially approved by our institutes’ research board (IRB) and ethical committee. Signed written informed consents were individually obtained from each participant. A 3-year prospective study was performed from June 2010 until May 2012. Consecutive symptomatic female patients were randomly selected from those complaining of primary non-complicated GSV varicosities with saphenofemoral junction (SFJ) incompetence, and above and below the knee communicator incompetence with GSV reflux associated with ≤ 5mm diameter. Reflux was determined as a reversed flow during >0.5 seconds after compression of the calf [4]. Eligible candidates who had given informed written consent were randomly selected and distributed into 3 groups by means of a random number table produced by Microsoft excel for receiving either surgery, ultrasound-guided foam sclerotherapy (USGFS) or EVLT. All of the treated patients had (CEAP C2-C4) venous disease and significant reflux in a segment of the GSV as determined by color duplex ultrasound (CDUS) examination. Excluded from this study were female patients with a previous history of deep vein thrombosis (DVT), lesser saphenous vein varicosities, recurrent varicosities, and patients with coexisting disease or disabilities that would preclude surgical treatment, varicose veins complicated by superficial thrombophlebitis/active or recurrent venous leg ulceration; below knee varicosities due to incompetent leg perforators. As well as, patients with telangiectatic or spider varicosities that required compression sclerotherapy, patients with a history of peripheral arterial disease, venous malformations, deep venous agenesis, use of anticoagulation therapy, pregnancy, heart failure, and patients with a known allergy to sclerosing materials. All patients were initially evaluated by a thorough medical history. Local clinical examination of the limb took place in each patient defining the clinical class (C) of the CEAP (Clinical Etiologic Anatomic Pathophysiologic) classification [20], as well as limb assessment by CDUS. Limbs were classified according to the CEAP classification (as mentioned by the North American Chapter of the Society for Vascular Surgery and the International Society) [21]. Patients were included if they have primary GSV insufficiency, in addition to SFJ incompetence with a reflux time 0.5 seconds measured within a distance of ≤ 20 cm in the proximal leg [22]. Accordingly, patients were classified into 3 groups; group I included those who underwent both surgical SFJD and GSV stripping. Group II involved those who were treated with USGFS, and finally, group III comprises those who underwent EVLT using Diode Laser (DL). Group I underwent surgical disconnection of the SFJ and stripping of the GSV. Group II treated by USGFS using polidocanol (Aethoxysklerol; Kreussler Pharma, Wiesbaden, Germany) as a cooled foam sclerosing agent in a dosage of 1–3%. The foam should be cooled as low as possible (1°C) as an ideal temperature. For patients with GSV superficial varicosities, 1% polidocanol foam was used. On the other hand, deeper GSV varicosities were given cooled foam in a 3% concentration. Moreover, the distal part of the GSV and other prominent veins were managed in separate subsequent sessions using the same technique (i.e. 60o leg elevation, cooled foam injection and calf bandage). Furthermore, the 1-week interval was carried out between every session [17]. GIII underwent EVLT using DL. With this type of laser, the vein was ablated using intense thermal energy generated using a laser light [19], [20], [21], [22], [23], [24]. The tip of the laser wire was positioned 15 mm distal to the SFJ under ultrasound guidance. The system of endovenous laser ablation was Diomed EVLT (Angio Dynamics, New York, NY). Over the red aiming beam, digital compression was applied during the procedure to allow adhesion of the wall of the vein ablated around the tip of the laser fiber. Successful post-procedural complete GSV ablation was achieved as proved by CDUS examination. Following the procedure, immediate compression garments were applied with a pressure ranged from 20–30 mmHg or 30–40 mmHg and left for about 6–12 weeks [25], [26], [27]. The patients were initially followed up in the early postoperative period after 1 week and 1 month. Then every 3 months for the first year, then biannually in the next 2 years, and finally every year for the following 6 years. The follow-up protocol included clinical history taking, local physical examination of the limb, as well as CDUS examination of the venous system of the affected limb. The CDUS examination stratified the GSV as completely ablated and obliterated (1), partially ablated with (2a) or without (2b) valvular incompetence, non-ablated non-obliterated (3). Moreover, the existence of DVT was expected as, both the superficial and deep venous system of the affected limb was thoroughly examined by CDUS [28]. The main objectives of the long-term follow-up were to determine the rate and incidence of GSV ablation, patient satisfaction, in addition to the detection of late post-treatment complications. The primary endpoint was absent or ablated GSV. A refluxing open segment of the treated GSV of 10 cm or more was considered as a technical failure to strip the vein, or post-procedural recanalization. Secondary endpoints were the existence of varicose veins (VV) during follow-up, the incidence of reoperations, changes in response to interventions using the venous clinical severity score (VCSS), in addition to the health-related quality of life score (HRQOLS). Clinical recurrence (defined as clinically obvious superficial varicosities ≤ 3 mm in diameter not present within 1-6 weeks, mostly evident during further follow-up [29].
Anatomic success. Successful ablation of the treated vein, as well as the extent of the obstructed, or patent part of the vein as proven with CDUS. Moreover, technical failure is considered if there is patency of the ablated saphenous vein documented by a periprocedural duplex image (˂3 days). While late patency following early occlusion indicates recanalization [30].
Hemodynamic success. The presence or absence of recurrent reflux in treated incompetent veins documented by CDUS scanning [30].
Clinical success. The accomplishment of durable clinical success can be confirmed by significant improvement of postprocedural VCSS [13].
Statistical analysis. All statistical analyses were performed using IBM Statistical Package for the Social Science (SPSS®) program version 23, [IBM Corporation, Armonk, New York, USA]. Data expressed as mean ± standard deviation (SD). Categorical variables were presented as number and percentage. Continuous variables were presented as mean ± standard deviation (SD). These results interpreted in detail the characteristics of the study population. Comparisons between the 3 treated groups were analyzed using the Z-test for proportions. The Kaplan-Meier survival analysis was used to estimate survival free recanalization. P-value of < 0.05 was considered to have a statistical significance. Unadjusted hazard ratios with 95% confidence intervals (CI) were further used to evaluate the association between the risk factors of interest and their association with the development of lower limb varicosities.
RESULTS
Eighty female patients were enrolled in this prospective study. Patient's age ranged from 35-62 years with a mean of 47 ± 7.6. Patients' demographics, their clinical presentations, preoperative CDUS, as well as CEAP classification (clinical grades C2 or beyond) of the studied groups are listed in (Table 1). The predisposing factors associated to the development of varicose veins are illustrated in (Fig 1). Patients' age distribution among the treated groups is listed in (Table 2). In GI 35 patients (43.75%) underwent surgery in the form of SFJD and GSV stripping; 25 patients (31.25%) were treated by USGFS, and the remaining 20 patients (25%) underwent an EVLT. In the surgically treated group, the long-term follow-up after 6 years showed a complete ablation and absence of GSV in 91.5% (n = 32). The remaining 8.5% (n = 3) of patients developed recurrent varicosities after 18 months of follow-up. On the other hand, most of the patients who underwent USGFS, n = 15 of 25 (60%), showed a complete success of treatment, while 9 of 25 patients (36%) had recurrent varicosities within 12–18 months of follow-up, yet, the remaining patient 1 of 25 (4%) suffered from DVT as an early postoperative complication that was developed 1 week after the procedure. Furthermore, the majority of patients who were treated with EVLT have been reported to have completely occluded and ablated varicosities in 18 of 20 patients (90%) as verified by CDUS. Moreover, recurrence was observed in 2 patients after 18 months and 24 months, respectively. The anatomic success rate was statistically significantly higher in the surgically treated group compared to the group treated with USGFS (P = .003). In addition, there was a significantly high success rate of GSV ablation for the EVLT treated group over the USGFS treated patients (P = .023). On the other hand, there is no significant differences between the surgically treated group and those group treated with EVLT (P = .85), as depicted in (Table 3 and Fig 2). Analysis of VCSS using multivariate (Wilks’ Lambada) test revealed that there was a marked improvement of the post-interventional score, P = .0001 (Table 4). Moreover, by comparing the preoperative VCSS (level 1) with the postoperative VCSS after 1 year (level 2), 3 years (level 3), and after 6 years (level 4); we found that there was a statistically significant difference between the pre- and postoperative VCSS as the P value was, .0001, .0003, .0008, respectively (Table 5). Early postoperative complications were all of the mild types and recorded in 15% of patients (n = 11). They ranged from subcutaneous hematoma in 4 patients (5%), mild wound infection in 3 patients (3.75%), allergic reaction due to the bandage in 3 patients (3.75%), as well as DVT in 1.25% of patients (n = 1). Among 35 patients treated surgically, 3 patients (8.5%) developed recurrent varicosities. This recurrence might be due to the presence of multiple incompetent perforators in the anteromedial aspect of the leg as proved by CDUS (Fig 3). On the other hand, 9 out of 29 patients in GII who underwent USGFS developed recurrent varicosities. Partial recanalization was observed in the GSV by clinical examination and proved by the presence of a retrograde flow documented by CDUS which revealed that the GSV was dilated measuring about 6.2 mm in the upper-thigh, 5 mm in the mid-thigh, and 5.3 mm in the lower-thigh where it exits from its fascia and becomes more superficial in location (Fig 4 A and B). Furthermore, 2 (10%) out of 20 patients who treated with EVLT developed recurrent varicosities after 18 and 24 months, respectively. Patients with recurrent varicosities after surgery and EVLT were treated by compression sclerotherapy. This was taking place through further sessions of local injection (i.e. compression sclerotherapy) using (Chromium [III] Potassium Sulphate, 0.04 g and Glycerol 3.6 g/ampoule 5 ml — ScleremoTM). On the other hand, patients with recurrent varicosities that developed after USGFS were treated by additional sessions of foam sclerotherapy. Recurrent varicosities were observed in those previously reinjected patients (i.e. USGFS treated group), 18 months after follow-up and reinjected again. Forty-eight months after follow-up 2 of those patients who underwent reinjection developed venous leg ulcers at the ulcer bearing area (i.e. gaiter area) on the anteromedial part of the leg. This ulcer was developed because of leg perforator incompetence as documented by CDUS scanning (Fig 5). Conservative therapy was adopted from 6–10 months to allow for ulcer healing in the form of local ulcer dressing, leg elevation and the application of elastic compression stocking (Table 4). Unfortunately, the ulcers resist healing on conservative treatment and the operation of subfascial endoscopic perforator surgery (SEPS) took place after 48 months of the follow-up. This is followed by local ulcer dressing with the application of either graduated elastic compression stocking or a 4-layer dressing to decrease the venous pressure of the limb and allow the ulcer to heal. The ulcers gradually reduced in size and complete healing was achieved within 60–72 months of follow-up. The timing of recurrence of varicosities for all the procedures is illustrated in (Fig 6). Furthermore, the Kaplan Meier Survival method was done to stratify patients-free from recanalization and development of recurrent varicosities with 72 months follow-up period as depicted in (Fig 7). There was a marked improvement in HRQOLS after the intervention P < .001. Moreover, paired-samples t-test was used to compare the means of differences between HRQOLS before the interventions and at different periods of follow-up as displayed in (Table 6).
Table 1.
Clinical presentation of patients with VV and preoperative CDUS findings⁎
| Factor | n (%) |
|---|---|
| Patients’ number and age | |
| Total number of patients | 80 (100%) |
| Age in years (mean ± SD), (range) | 47 ± 7.6 (35-62) |
| Clinical presentation | |
| Swelling | 64 (80%) |
| Hyperpigmentation | 28 (35%) |
| Diffuse leg pain | 40 (50%) |
| Sensations of throbbing/heaviness | 56 (70%) |
| Cosmetic concern only | 20 (25%) |
| Preoperative CDUS | |
| SFJ incompetence and VV limited to the knee | 45 (56.25%) |
| SFJ incompetence and VV involving the whole GSV | 35 (43.75%) |
| CEAP (ACP) classification | Surgery | USGFS | EVLT |
|---|---|---|---|
| C2,S, Ep, As, Pr: Varicose veins | 35 (44%) | 25 (31%) | 20 (25%) |
| C3,S, Ep, As, Pr: Edema | 20 (25%) | 15 (19%) | 39(49%) |
| C4,S, Ep, As, Pr: Skin changes without ulceration | 8 (10%) | 9 (11%) | 11 (37%) |
Results are expressed as number (n) and percentage (%). CEAP, Clinical Etiologic Anatomic Pathophysiologic; ACP, American College of Phlebology; CDUS, color Doppler ultrasonography; SFJ, saphenofemoral junction; VV, varicose veins; GSV, great saphenous vein; USGFS, ultrasound-guided foam sclerotherapy; EVLT, endovenous laser therapy.
Fig 1.
Predisposing factors for the development of varicose veins.
Table 2.
Patient’s age distribution among the treated groups
| Mean age in years |
47.3 ± 06.2 |
Median (Min – Max) |
47 (35 – 62) |
|||
|---|---|---|---|---|---|---|
| Age group stratification | ||||||
| Groups | n | Mean | SD | SE | Minimum | Maximum |
| GI | 20 | 44.5000 | 5.91608 | 1.32288 | 35.00 | 54.00 |
| GII | 25 | 47.5200 | 8.67525 | 1.73505 | 35.00 | 62.00 |
| GIII | 35 | 48.8000 | 7.61114 | 1.28652 | 35.00 | 62.00 |
| Total | 80 | 47.3250 | 7.69477 | .86030 | 35.00 | 62.00 |
SD, Standard deviation; SE, standard error.
Table 3.
The success and failure rate of different therapeutic options
| Patients’ group | Success | Fail | Total | % | P-value |
|---|---|---|---|---|---|
| I - Surgery | 32 | 3 | 35 | 91.5 | .003⁎ I vs. II |
| II - USGF | 15 | 10 | 25 | 60 | .023⁎ II vs. III |
| III - ELVT | 18 | 2 | 20 | 90 | .850ň I vs. III |
Significant; ňNon-significant; USGFS, ultrasound-guided foam sclerotherapy; EVLT, endovenous laser therapy.
Fig 2.

The success and failure rate between different therapeutic options. USGF: Ultrasound-guided foam sclerotherapy, EVLT: Endovenous laser therapy
Table 4.
Multivariate analysisb of VCSS before and after the interventions.
| Effect | Value | F | Hypothesis df | Error df | P |
|---|---|---|---|---|---|
| VCSS | a | ||||
| Wilks’ Lambada | .036 | 168.182a | 3.000 | 19.000 | .0001⁎ |
a. Exact Statistic
b. Design: Intercept, Within Subject Design: VCSS
Significant; VCSS, Venous Clinical Severity Score
Table 5.
Comparisons between VCSS before intervention and after 1, 3, and 6 years post intervention.
| Source | VCSS | Type III Sum of Square | df | Mean Square | F | P |
|---|---|---|---|---|---|---|
| VCSS | Level 2 vs. Level 1 | 3.633 | 1 | 3.633 | 379.350 | .001⁎ |
| Level 3 vs. Level 1 | 4.419 | 1 | 4.419 | 515.194 | .003⁎ | |
| Level 4 vs. Level 1 | 4.410 | 1 | 4.410 | 215.284 | .008⁎ |
Significant; VCSS, Venous Clinical Severity Score; Level 1, VCSS; Level 2, follow-up after 1 year; Level 3, follow-up after 3 years; level 4, follow-up after 6 years; df, degree of freedom.
Fig 3.
CDUS showing recurrent below knee varicosities after SFJD and GSV stripping. Dilated right great saphenous vein measuring 11 mm in the mid-thigh.
Fig 4.
CDUS show recurrent varicosities after ultrasound-guided foam sclerotherapy. The left great saphenous vein is dilated measuring as follow 12.2 mm in the upper thigh (A), incompetent left saphenofemoral junction grade 3, it measures about 12 mm (B).
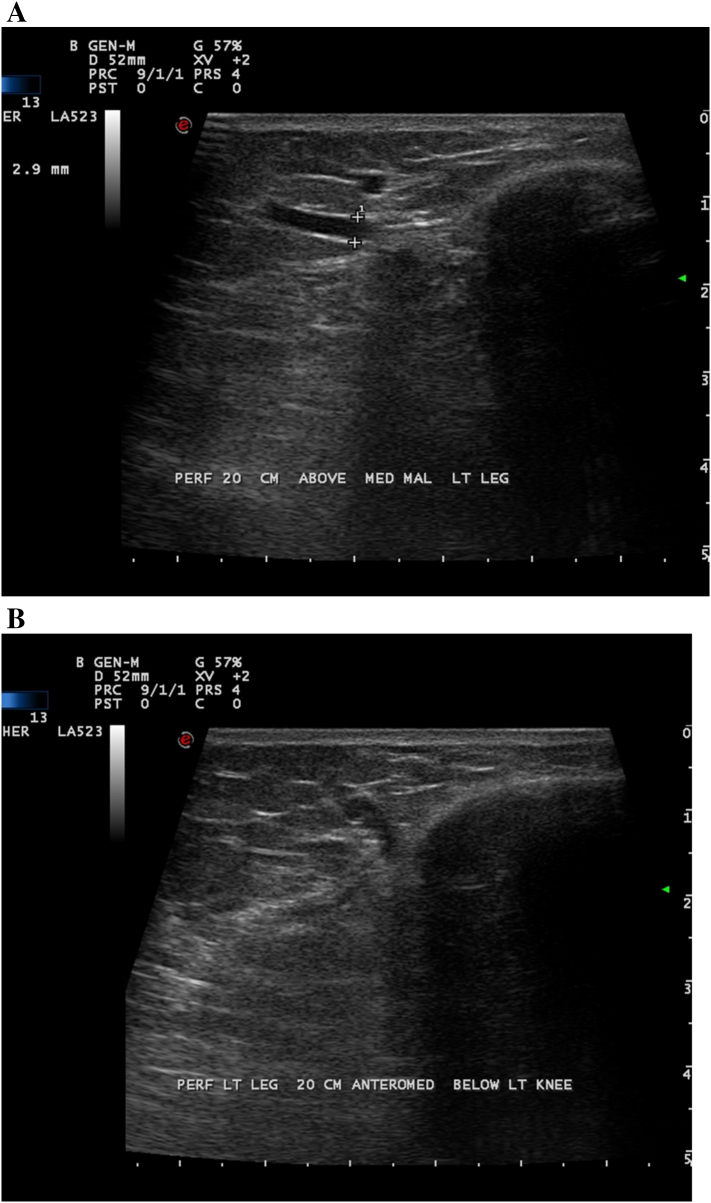
Fig 5.
Incompetent leg perforator 20 cm above the medial malleolus that developed within 48 months of follow-up. An incompetent perforator is seen in the anteromedial aspect of the left leg about 20 cm below the left knee measuring approximately 4 mm and seen supplying a 3.7 mm subcutaneous vein which is running upward along the medial aspect of the lower thigh (A). Another similar smaller incompetent perforator measuring about 3 mm is seen approximately 20 cm above the medial malleolus on the medial aspect of the left leg. Otherwise, few other leg perforators are seen in the posterior and medial aspects of the left leg (B).
Fig 6.
Line graph demonstrating the time of postoperative recurrent varicosities.
Fig 7.
Kaplan Meier survival curves for patients free from recurrent varicosities on long-term follow-up after 72 months.
Table 6.
Health-related quality of life scores (HRQOLS) before and after the interventions
| Variable | Paired differences |
t | P | ||
|---|---|---|---|---|---|
| Mean | ± SD | ||||
| Pair 1 | Bodily pain before/ | –.4064 | .09786 | –19.477 | .001⁎ |
| Bodily pain before/after 1 year | |||||
| Pair 2 | Social functioning before/ | –.4482 | .09261 | –22.698 | .001⁎ |
| Social functioning before/after 3 years | |||||
| Pair 3 | Physical and mental component before/ | –.4477 | .1431 | –14.673 | .001⁎ |
| Physical and mental components before/after 6 years | |||||
Significant; SD, Standard deviation.
DISCUSSION
Primary varicose veins of the lower limb are one of the major challenges, confronting the surgeons. Although many modalities have existed for their management, the one that may have a 100% cure rate does not exist yet. These modalities include conservative treatment such as compression, leg elevation, and avoidance of long standing. Traditional operations including surgical SFJD and stripping of the GSV, in addition to, sonographically-guided foam sclerotherapy, radiofrequency ablation as well as EVLT [29], [32], [33], [34]. Our patients’ age ranged between 35-62 years with a mean of 47 ± 7.6, this data coincides with that previously reported in the literature [4], [23], [35], [36], [37]. In our series, we have applied a surgical treatment of primary varicosities of the GSV in the form of SFJD and GSV stripping in 35/80 patients, EVLT using DL in 20/80 patients, and USGFS in 25/80 patients. Our results showed an anatomic success rate of 91.5% in the surgically treated group coincides with previously reported data in long-term prospective studies [5], [13], [38], [39]. Moreover, the recurrence rate post-surgical intervention was observed in 3.8% of patients contradicting that reported in some of the literature, where they described an incidence of 13–29% [40], [41]. In addition, the recurrence rate following long-term follows up of 5–20 years was observed clinically in the previous literature ranged from 20–80% [42]. The recurrence of varicosities after conventional surgery may be attributed to the improperly adopted primary surgical technique, neovascularization, accessory vein reflux/perforator incompetence [43], [44]. Furthermore, the anatomic success rate in the USGFS treated group was somewhat low reaching up to 60%. This can be compared to the previously published reports [38], [44], [45]. The reason for this relatively low success rate of USGFS compared to surgery and EVLT may be referred to the fact that its effectiveness is usually low in large diameter veins compared to a smaller one. In addition, recanalization following USGFS may be related to both SFJ incompetence and paratibial perforator incompetence [23], despite USGFS may be the sole treatment modality most of the patients who have strong contraindications to surgery or EVLT. It may also be very effective in small diameter saphenous vein varicosities [44]. Nevertheless, USGFS may be considered as an excellent alternative in treating patients with recurrent varicosities as it can be combined with other techniques [45], [46], [47]. In this study, only 1 patient complicated with DVT within 2 weeks after the first injection of USGFS that might be compared to the previously recorded reports following USGFS [48]. The reason for this coincidence may be explained by an accidental increase in the volume of the injected foam/increase in the production of endothelin-1 [49], [50]. Another patient suffered from leg ulceration 18 months after treatment with USGFS. The causative factor may be due to an increased concentration or extravasation of the sclerosing materials, as previously reported [51]. Despite the limitations and the low success rate of USGFS, it may still be considered as an effective and valuable option in treating some selected cases with varicose veins [4]. Long-term assorted follow-up prospective studies have been published [5], [13], and recording the following results for open surgery, EVLT, and USGFS of 94%, 90%, and 58%, respectively. Our data showed a high success rate of surgery and EVLT coinciding with previously published reports as regards the long-term follow-up [5], [15], [51], [52]. In the current study, the success rate after adopting surgery and EVLT were approaching 91% and 90%, respectively. These results coinciding with previously published reports [31], [52], [53], [54], although they appeared to be superior to other data reported in some literature [13], [34], [46], [53]. The reason for this discrepancy may be attributed to the difference in the definition of the success rate. Some defined it very strictly considering failure when the great saphenous varicosities presented as a segment above the knee level. To date, there are little reports that studied the long-term follow-up of primary non-complicated GSV varicosities underwent different surgical and non-surgical modalities. Therefore, our current study proposed to highlight the long-term follow-up of this condition. Although the study is having some limitations that are the relatively low number of cases, it may lead to explain that surgery still has the best long-term follow-up management modality compared to EVLT. However, despite the inferior results of USGFS in comparison to the other 2 techniques, it may still have a role in treating primary uncomplicated varicosities of the lower limb especially when the other 2 modalities are contraindicated due to anesthesia obstacles. Furthermore, VCSS and HRQOLS showed equal improvement among the treated groups. However, there were various limitations to the current study. The cohort sample size is relatively small as previously described, and larger series may be needed in future studies for a more accurate investigation of this notion. Moreover, the selected patients had primary non-complicated great saphenous vein varicosities with minimal chronic venous changes (CEAP 2-4); thus, they were patients who had early varicose veins. So, patients who had complicated varicosities with either chronic leg ulceration or leg perforator incompetence; in addition to patients with lesser saphenous vein should be involved in future studies.
In conclusion, long-term follow-up of different treatment modalities for primary non-complicated GSV varicosities among females is mandatory to elucidate the postoperative complications, especially those who underwent USGFS. Moreover, there was a lower incidence of postoperative recurrence rate and objective evaluation and assessment showed good ablation of the great saphenous vein varicosities within 6 years of interventions. Furthermore, our study showed that a recurrence with recanalization of the GSV was frequently encountered following USGFS. In addition, no difference was found in the technical efficacy between the other modalities during a 6-year follow-up period with marked improvement of both the venous clinical severity and the health-related quality of life scores.
DECLARATIONS
Author contributions. AM, ME, designed the study. AM, ME, MAE, performed the analysis and interpretation of data. AM, ME, MAE, revised it critically. AM, ME, MAE, final approval of the version to be published All authors reviewed and approved the manuscript for final publication.
Conflict of interest statement. The authors declare that there is no conflict of interests regarding the publication of this article.
Funding. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics approval and consent to participate. Ethical approval was taken from our institute’s research board (IRB) and ethical committee of Faculty of Medicine, Al-Azhar University, Cairo, Egypt. A waiver for approval by our institutional review board was achieved.
Disclosures. None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
Acknowledgments. The authors would like to thank Prof. Tarek D. Hussein, Professor of Zoology, Faculty of Science, Cairo University, Cairo, Egypt; for his effort in performing the statistical analysis for this article.
Footnotes
Acknowledgments: The authors would like to thank Prof. Tarek D. Hussein, Professor of Zoology, Faculty of Sciences, Cairo University, Cairo, Egypt; for his effort for performing the statistical analysis for this article.
Potential Conflict of Interest: All authors declare that no competing interests regarding the publication of this article.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Meissner MH, Gloviczki P, Gergan J, Kistner RL, Morrison N, Pannier F et al. Primary chronic venous disorders. J Vasc Surg 2007;(46 Suppl S):54S-67S. [DOI] [PubMed]
- 2.Cheng W.H., Patel H., Lee W.J., Lin F.J., Pickard A.S. Positive outcomes of varicose vein surgery: the patient perspective. Patient. 2015;8:329–337. doi: 10.1007/s40271-014-0092-x. [DOI] [PubMed] [Google Scholar]
- 3.Mosquera D. Historical overview of varicose vein surgery. Ann Vasc Surg. 2010;24:1159. doi: 10.1016/j.avsg.2010.03.038. [DOI] [PubMed] [Google Scholar]
- 4.van der Velden S.K., Biemans A.A., De Maeseneer M.G., Kockaert M.A., Cuypers P.W., Hollestein L.M. Five-year results of a randomized clinical trial of conventional surgery, endovenous laser ablation and ultrasound-guided foam sclerotherapy in patients with great saphenous varicose veins. Br J Surg. 2015;102:1184–1194. doi: 10.1002/bjs.9867. [DOI] [PubMed] [Google Scholar]
- 5.Blomgren L., Johansson G., Dahlberg-AKerman A., Norén A., Brundin C., Nordström E. Recurrent varicose veins: incidence, risk factors and groin anatomy. Eur J Vasc Endovasc Surg. 2004;27:269–274. doi: 10.1016/j.ejvs.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 6.Onida S., Shalhoub J., Moore H.M., Head K.S., Lane T.R., Davies A.H. Factors impacting on patient perception of procedural success and satisfaction following treatment for varicose veins. Br J Surg. 2016;103:382–390. doi: 10.1002/bjs.10117. [DOI] [PubMed] [Google Scholar]
- 7.Zamboni P., Gianesini S., Menegatti E., Tacconi G., Palazzo A., Liboni A. Great saphenous varicose vein surgery without saphenofemoral junction disconnection. Br J Surg. 2010;97:820–825. doi: 10.1002/bjs.7022. [DOI] [PubMed] [Google Scholar]
- 8.Mackay D.C., Summerton D.J., Walker A.J. The early morbidity of varicose vein surgery. J R Nav Med Serv. 1995;81:42–46. [PubMed] [Google Scholar]
- 9.Miller G.V., Lewis W.G., Sainsbury J.R., Macdonald R.C. Morbidity of varicose vein surgery: auditing the benefit of changing clinical practice. Ann R Coll Surg Engl. 1996;78:345–349. [PMC free article] [PubMed] [Google Scholar]
- 10.Baker D.M., Turnbull N.B., Pearson J.C., Makin G.S. How successful is varicose vein surgery? A patient outcome study following varicose vein surgery using the SF-36 Health Assessment Questionnaire. Eur J Vasc Endovasc Surg. 1995;9:299–304. doi: 10.1016/s1078-5884(05)80134-0. [DOI] [PubMed] [Google Scholar]
- 11.MacKenzie R.K., Allan P.L., Rukley C.V., Bradbury A.W. The effect of long saphenous vein stripping on deep venous reflux. Eur J Vasc Endovasc Surg. 2004;28:104–107. doi: 10.1016/j.ejvs.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 12.Neglen P. Long saphenous vein stripping is favored in treating varicose veins. Dermatol Surg. 2001;27:901–902. doi: 10.1046/j.1524-4725.2001.01999.x. [DOI] [PubMed] [Google Scholar]
- 13.Proebstle T.M., Alm B.J., Gockeritz O., Wenzel C., Noppeney T., Lebard C. Five-year results from the prospective European multicentre cohort study on radiofrequency segmental thermal ablation for incompetent great saphenous veins. Br J Surg. 2015;102:212–218. doi: 10.1002/bjs.9679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lurie F., Creton D., Eklof B., Kabnick L.S., Kistner R.L., Pichot O. Prospective randomized study of endovenous radiofrequency obliteration (closure procedure) versus ligation and stripping in a selected patient population (EVOLVeS Study) J Vasc Surg. 2003;38:207–214. doi: 10.1016/s0741-5214(03)00228-3. [DOI] [PubMed] [Google Scholar]
- 15.Rautio T., Ohinmaa A., Perala J., Ohtonen P., Heikkinen T., Wiik H. Endovenous obliteration versus conventional stripping operation in the treatment of primary varicose veins: a randomized controlled trial with comparison of the costs. J Vasc Surg. 2002;35:958–965. doi: 10.1067/mva.2002.123096. [DOI] [PubMed] [Google Scholar]
- 16.Nicolaides A., Kakkos S., Eklof B., Perrin M., Nelzen O., Neglen P. Management of chronic venous disorders of the lower limbs-guidelines according to scientific evidence. Int Angiol. 2014;33:87–208. [PubMed] [Google Scholar]
- 17.Hill D., Hamilton R., Fung T. Assessment of techniques to reduce sclerosant foam migration during ultrasound-guided sclerotherapy of the great saphenous vein. J Vasc Surg. 2008;48:934–939. doi: 10.1016/j.jvs.2008.05.077. [DOI] [PubMed] [Google Scholar]
- 18.Centre National Clinical Guideline. Commissioned by the National Institute for Health and Care Excellence (NICE) Varicose Veins in the Legs: The Diagnosis and Management of Varicose Veins. 2013:1–250. [PubMed] [Google Scholar]
- 19.Gloviczki P., Comerota A.J., Dalsing B.G., Gillespie D.L., Gloviczki M.L., Lohr J.M. Society for vascular Surgery; American Venous Forum. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5 Suppl):2S–48S. doi: 10.1016/j.jvs.2011.01.079. [DOI] [PubMed] [Google Scholar]
- 20.Eklof B., Rutherford R.B., Bergan J.J., Carpentier P.H., Gloviczki P., Kistner R.L. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40:1248–1252. doi: 10.1016/j.jvs.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 21.Beebe H.G., Bergan J.J., Berggvist D., Eklof B., Eriksson I., Goldman M.P. Classification and grading of chronic venous disease in the lower limbs. A consensus statement Eur J Vasc Endovasc Surg. 1996;12:487–491. doi: 10.1016/s1078-5884(96)80019-0. [DOI] [PubMed] [Google Scholar]
- 22.Labropoulos N., Delis K., Nicolaides A.N., Leon M., Ramaswami G. The role of the distribution and anatomic extent of reflux in the development of signs and symptoms in chronic venous insufficiency. J Vasc Surg. 1996;23:504–510. doi: 10.1016/s0741-5214(96)80018-8. [DOI] [PubMed] [Google Scholar]
- 23.Baeshko A., Shestak N., Korytko S. Results of Ultrasound-Guided Foam Sclerotherapy of the Great Saphenous Vein with New Parameters of the Technique. Vasc Endovasc Surg. 2016;50:528–533. doi: 10.1177/1538574416675482. [DOI] [PubMed] [Google Scholar]
- 24.Pendy V.A., Davies A.S. Endoluminal treatments for varicose veins. Surgery (Oxford) 2010;28:263–267. [Google Scholar]
- 25.Marston W.A., Crowner J., Kouri A., Kalbaugh C.A. Incidence of venous leg ulcer healing and recurrence after treatment with endovenous laser ablation. J Vasc Surg Venous Lymphat Disord. 2017;5:525–532. doi: 10.1016/j.jvsv.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 26.Dunst K.M., Huemer G.M., Wayand W., Shamiyeh A. Diffuse phlegmonous phlebitis after endovascular laser treatment of the greater saphenous vein. J Vasc Surg. 2006;43:1056–1058. doi: 10.1016/j.jvs.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 27.Patel P.A., Barnacle A.M., Stuart S., Amaral J.G., John P.R. Endovenous laser ablation therapy in children: applications and outcomes. Pediatr Radiol. 2017;47:1353–1363. doi: 10.1007/s00247-017-3863-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meissner M.H. Venous duplex scanning. In: Rutherford R.D., editor. Vascular surgery 5Th. W.B. Saunders; Philadelphia: 2000. pp. 2014–2029. [Google Scholar]
- 29.Ruckley C.V. Socioeconomic impact of chronic venous insufficiency and leg ulcers. Angiology. 1997;48:67–69. doi: 10.1177/000331979704800111. [DOI] [PubMed] [Google Scholar]
- 30.Kundu S., Lurie F., Millward S.F., Padberg F., Jr., Vedantham S., Elias S. Recommended reporting standards for endovenous ablation for the treatment of venous insufficiency: joint statement of the American Venous Forum and the Society of Interventional Radiology. J Vasc Surg. 2007;46:582–589. doi: 10.1016/j.jvs.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 31.Pittaluga P., Chastanet S., Rea B., Barbe R. Midterm results of the surgical treatment of varices by phlebectomy with conservation of a refluxing saphenous vein. J Vasc Surg. 2009;50:107–118. doi: 10.1016/j.jvs.2008.12.067. [DOI] [PubMed] [Google Scholar]
- 32.Fletcher A., Cullum N., Sheldon T.A. A systemic review of compression treatment for venous leg ulcers. BMJ. 1997;315:576–580. doi: 10.1136/bmj.315.7108.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prandoni P., Lensing A.W., Prins M.H., Frulla M., Marchiori A., Bernardi E. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004;141:249–256. doi: 10.7326/0003-4819-141-4-200408170-00004. [DOI] [PubMed] [Google Scholar]
- 34.Negus D., Moffatt C.J., Franks P.J. Venous surgery in ulcer management: a review. In: Negus D., Smith P.D., Bergan J.J., editors. Textbook of Leg ulcer-diagnosis and management. 3rd ed. Hodder Arnold; London, UK: 2005. pp. 213–217. [Google Scholar]
- 35.Carradice D., Mekako A.I., Mazari F.A., Samuel N., Hatfield J., Chetter I.C. Randomized clinical trial of endovenous laser ablation compared with conventional surgery for great saphenous varicose veins. Br J Surg. 2011;98:501–510. doi: 10.1002/bjs.7394. [DOI] [PubMed] [Google Scholar]
- 36.Allegra C., Antignani P.L., Carlizza A. Recurrent varicose veins following surgical treatment: our experience with five years follow-up. Eur J Vasc Endovasc Surg. 2007;33:751–756. doi: 10.1016/j.ejvs.2006.12.020. [DOI] [PubMed] [Google Scholar]
- 37.Barandiaran J.V., Hall T.C., Lim M., El-Barghouti N., Perry E.P. Saphenofemoral junction ligation and disconnection for varicose veins-a longitudinal study of cosmesis and function. Ann Vasc Surg. 2011;25:662–668. doi: 10.1016/j.avsg.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 38.Kalodiki E., Lattimer C.R., Azzam M., Shawish E., Bountouroglou D., Geroukalso G. Long-term results of a randomized controlled trial on ultrasound-guided foam sclerotherapy combined with saphenofemoral ligation vs standard surgery for varicose veins. J Vasc Surg. 2012;55:451–457. doi: 10.1016/j.jvs.2011.08.040. [DOI] [PubMed] [Google Scholar]
- 39.Disselhoff B.C., der Kinderen D.J., Kelder J.C., Moll F.L. Five-year results of a randomized clinical trial comparing endovenous laser ablation with cryostripping for great saphenous veins. Br J Surg. 2011;98:1107–1111. doi: 10.1002/bjs.7542. [DOI] [PubMed] [Google Scholar]
- 40.Dwerryhouse S., Davies B., Harradine K., Earnshaw J.J. Stripping the long saphenous vein reduces the rate of reoperation for recurrent varicose veins: five-year results of a randomized trial. J Vasc Surg. 1999;29:589–592. doi: 10.1016/s0741-5214(99)70302-2. [DOI] [PubMed] [Google Scholar]
- 41.Jones L., Braithwaite B.D., Selwyn D., Cooke S., Earnshaw J.J. Reprinted article “Neovascularisation is the principal cause of varicose vein recurrence: results of a randomised trial of stripping the long saphenous vein”. Eur J Vasc Endovasc Surg. 2011;42(Suppl. 1):S57–S60. doi: 10.1016/j.ejvs.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 42.Eklof B., Juhan C. Recurrences of primary varicose veins. In: EKLOF B., GORES E., THULESIUS O., BERQVIST O., editors. Controversies in the management of venous disorders. London, Bitterworths. 1989. pp. 220–233. [Google Scholar]
- 43.Zimmet S.E. Endovenous laser ablation. Phlebolymphology. 2007;14:49–96. [Google Scholar]
- 44.Myers K.A., Jolley D. Outcome of endovenous laser therapy for saphenous reflux and varicose veins: medium-term results assessed by ultrasound. Eur J Vasc Endovasc Surg. 2009;37:742. doi: 10.1016/j.ejvs.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 45.Shadid N., Nelemans P., Lawson J., Sommer A. Predictors of recurrence of great saphenous vein reflux following treatment with ultrasound-guided foam sclerotherapy. Phlebology. 2015;30:194–199. doi: 10.1177/0268355514521183. [DOI] [PubMed] [Google Scholar]
- 46.Darvall K.A., Bate G.R., Adm D.J., Silverman S.H., Bradbury A.W. Duplex ultrasound outcomes following ultrasound-guided foam sclerotherapy of symptomatic recurrent great saphenous varicose veins. E J Vasc Endovasc Surg. 2011;42:107–114. doi: 10.1016/j.ejvs.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 47.De Maeseneer M. Surgery for recurrent varicose veins: towards a less-invasive approach? Perspect Vasc Surg Endovasc Ther. 2011;23:244–249. doi: 10.1177/1531003511408338. [DOI] [PubMed] [Google Scholar]
- 48.Bradbury A.W., Bata G., Pang K., Darvall K.A., Adam D.J. Ultrasound-guided foam sclerotherapy is a safe and clinically effective treatment for superficial venous reflux. J Vasc Surg. 2010;52:939–945. doi: 10.1016/j.jvs.2010.04.077. [DOI] [PubMed] [Google Scholar]
- 49.Myers K.A., Jolley D. Factors affecting the risk of deep venous occlusion after ultrasound-guided sclerotherapy for varicose veins. Eur J Vasc Endovasc Surg. 2008;36:602–605. doi: 10.1016/j.ejvs.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 50.Frullini A., Felice F., Burchielli S., Di Stefano R. High production of endothelin after foam sclerotherapy: A new pathogenetic hypothesis for neurological and visual disturbances after sclerotherapy. Phlebology. 2011;26:203–208. doi: 10.1258/phleb.2010.010029. [DOI] [PubMed] [Google Scholar]
- 51.Mwipatayi B.P., Western C.E., Wong J., Angel D. Atypical leg ulcers after sclerotherapy for treatment of varicose veins: Case reports and literature review. Int J Surg Case Rep. 2016;25:161–164. doi: 10.1016/j.ijscr.2016.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rasmussen L., Lawaetz M., Bjoern L., Blemings A., Eklof B. Randomized clinical trial comparing endovenous laser ablation and stripping of the great saphenous vein with clinical and duplex outcome after 5 years. J Vasc Surg. 2013;58:421–426. doi: 10.1016/j.jvs.2012.12.048. [DOI] [PubMed] [Google Scholar]
- 53.Ravi R., Trayler E.A., Barrett D.A., Diethrich E.B. Endovenous thermal ablation of superficial venous insufficiency of the lower extremity: single-center experience with 3000 limbs treated in a 7-year period. J Endovasc Ther. 2009;16:500–505. doi: 10.1583/09-2750.1. [DOI] [PubMed] [Google Scholar]
- 54.Van den Bos R., Arends L., Kockaert M., Neumann M., Nijsten T. Endovascular therapies of lower extremity varicosities: a meta-analysis. J Vasc Surg. 2009;49:230–239. doi: 10.1016/j.jvs.2008.06.030. [DOI] [PubMed] [Google Scholar]