Abstract
Introduction
COVID-19 emerged as a global pandemic in 2020 and has affected millions of lives. Surgical training has also been significantly affected by this pandemic, but the exact effect remains unknown. We sought to perform a national survey of general surgery residents in the United States to assess the effect of COVID-19 on surgical resident training, education, and burnout.
Methods
An anonymous online survey was created and distributed to general surgery residents across the United States. The survey aimed to assess changes to surgical residents’ clinical schedules, operative volume, and educational curricula as a result of the COVID-19 pandemic. Additionally, we sought to assess the impact of COVID-19 on resident burnout.
Results
One thousand one hundred and two general surgery residents completed the survey. Residents reported a significant decline in the number of cases performed during the pandemic. Educational curricula were largely shifted toward online didactics. The majority of residents reported spending more time on educational didactics than before the pandemic. The majority of residents feared contracting COVID-19 or transmitting it to their family during the pandemic.
Conclusions
COVID-19 has had significant impact on surgical training and education. One positive consequence of the pandemic is increased educational didactics. Online didactics should continue to be a part of surgical education in the post-COVID-19 era. Steps need to be taken to ensure that graduating surgical residents are adequately prepared for fellowship and independent practice despite the significantly decreased case volumes during this pandemic. Surgery training programs should focus on providing nontechnical clinical training and professional development during this time.
KEY WORDS: Surgical Education, COVID 19, online didactics, surgical residents, residency survey
COMPETENCIES: Patient Care, Medical Knowledge, Practice-Based Learning and Improvement
INTRODUCTION
The 2019 to 2020 coronavirus pandemic is an ongoing pandemic of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 The outbreak was first identified in Wuhan, China, in December 2019.2 The World Health Organization declared the outbreak a Public Health Emergency of International Concern on 30th January 2020, and a pandemic on the 11th of March 2020.3 As of May 1, 2020, more than 3.3 million cases of COVID-19 have been reported in 187 countries and territories, resulting in more than 235,000 deaths.4 COVID19 has severely affected United States as well. On January 20, 2020, the first U.S. case of COVID-19 was reported in the state of Washington; and as of May 15, 2020, 1.11 million Americans have been affected with the virus resulting in 86,744 deaths.5 , 6
Not only has COVID-19 affected millions of lives, but it has also had a significant impact on the healthcare system and the practice of medicine and surgery. Surgical providers have been forced to reconsider almost every facet of their daily practice. To ensure adequate hospital resources and to maintain social distancing, elective surgeries have been cancelled and clinics have scaled back drastically. Inpatient care teams have downsized to limit provider exposure. At teaching hospitals, resident schedules have changed substantially to provide a workforce where needed while preventing unnecessary resident exposure. Resident educational curricula have moved toward completely online platforms to avoid large gatherings.7
Surgical trainees have been uniquely impacted by these changes. While solutions have been implemented to make up for missing in-person educational didactics and conferences, there are no substitutes in place to compensate for the significant reduction of hands-on surgical training during this period. Further the restrictions of visitors as well as the number of people permitted into patient rooms have impacted the training of patient and family communications. Infected residents have required long absences from the hospitals which has resulted in reassignments of remaining residents. To learn more about how the COVID-19 pandemic is affecting the training and education of surgical residents, we conducted a brief anonymous survey of general surgery residents across the United States.
METHODS
An anonymous 23-question multiple choice survey was developed using Qualtrics, an online survey platform. All general surgery residency programs in the United States were invited to participate. The survey queried resident demographics, training program type and location, plans for fellowship training, operative and clinic duties before and during the COVID-19 pandemic, and effects of the pandemic on resident wellbeing and burnout.
Demographic and program information included clinical postgraduate year (PGY), training program state, and training program type (university or community). Changes to resident schedules, operating room protocols, duty hours, resident operative volume, number of clinic days before and during the pandemic and changes to educational curricula were assessed. Residents were asked if these changes will affect their graduation requirements and overall preparedness for their next career step. Finally, we assessed the effect of the pandemic on resident wellbeing and burnout.
SURVERY DEVELOPMENT, AND DISTRIBUTION
The survey questions were developed after a comprehensive review of current literature and validated instruments. The questions were converted to an online format and beta tested to ensure brevity, clarity, relevance, and consistent interpretation. The survey was then refined, incorporating feedback from the beta test of the survey. The survey was preceded by a statement explaining that the purpose of the survey was research, that data would be deidentified before analysis, and that program directors and chairs would not have access to the responses. There were no incentives or disincentives to participate. This study was deemed exempt by the University of Southern California Institutional Review Board.
A link to the survey was e-mailed to all 260 general surgery program directors (PDs) and program coordinators (PCs) and requested to be forwarded to the residents in their program. The emails of PDs and PCs were obtained from the Association of Program Directors in Surgery website (www.apds.org). Reminder emails to encourage participation were distributed weekly for a period of 4 weeks. Responses were captured anonymously to maintain confidentiality. The survey is summarized in Appendix A1. Descriptive statistical analysis was performed to summarize the data.
OUTCOMES MEASURED
The primary outcome was the change in volume of surgical cases performed by residents during the COVID-19 pandemic compared to prior.
Secondary outcomes were changes in educational curricula as a result of COVID-19, resident perceptions of the overall effects of the pandemic on their preparedness for their next career step, and the effects of COVID-19 on resident wellness and burnout.
RESULTS
Resident Information
One thousand one hundred and two general surgery residents completed the survey. The majority of respondents (18.7%) were from the state of New York followed by California (12.9%). Of the respondents, 20% were surgical interns, 38.1% were senior residents (PGY 4 and PGY 5) while mid-level residents (PGY 2 and 3) composed 41% of the respondents. The majority of residents belonged to a university-affiliated program (66%). Eighty-three percent of residents planned to pursue fellowship after residency. 70.4% of residents had cared for COVID-19 positive and suspected patients. Table 1 highlights resident demographics and program structure.
TABLE 1.
Resident and Program Demographics
| Q1. State of Training | |
| New York | 18.70% |
| California | 12.90% |
| Massachusetts | 5.50% |
| Michigan | 3.80% |
| Illinois | 3.80% |
| Q2. Current year of clinical training | |
| PGY1 | 20% |
| PGY2 | 16% |
| PGY3 | 25.50% |
| PGY4 | 18.20% |
| PGY5 | 19% |
| Q3. Type of training institution | |
| University hospital | 66.50% |
| Community with university affiliation | 23.50% |
| Nonuniversity affiliated hospital | 9.90% |
| Q4. Plan for fellowship after residency | |
| Yes | 83.10% |
| Q5. Exposure to a COVID-19 positive patient | |
| Yes | 53.40% |
| No | 29% |
| Unsure | 17.50% |
Surgical Training
In terms of daily rounding and floor duties, 77% of respondents reported that more duties were delegated to physician extenders such as nurse practitioners and physician assistants. Regarding changes to operating room protocol, 40.6% of the respondents reported that they were not allowed in the operating room for cases considered high-risk for COVID-19 transmission, and 12.5% of respondents reported interns and junior residents were not allowed in to the operating room at all. 26.6% of the respondents reported working more than 80 hours per week during the pandemic.
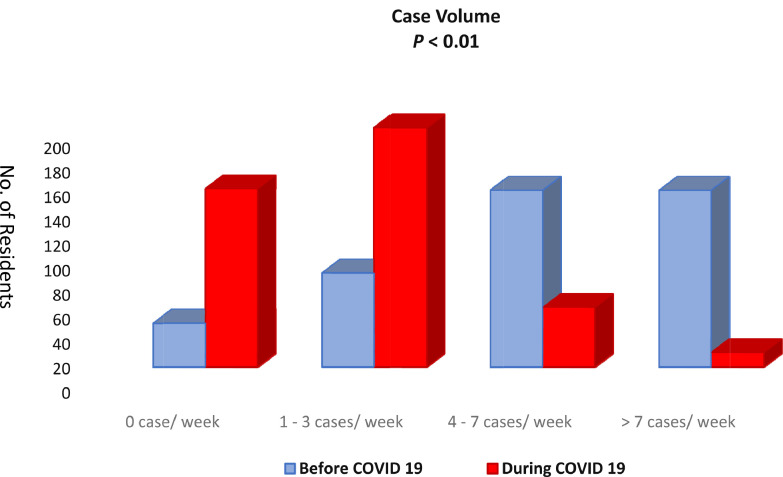
In terms of operative experience, we found a significant decline in the number of cases performed by residents per week. Figure 1 highlights the change in resident operative experience during the pandemic. In terms of clinic experience, while the majority of surgical residents attended some clinic prior to the pandemic, the overwhelming majority (80.67%) of residents attended no clinic during the pandemic.
FIGURE 1.
Surgical case volume before and during the COVID-19 pandemic.
42.3% of general surgery respondents felt they would not meet the traditional Accredited Council for Graduate Medical Education (ACGME) case requirements for graduation with the current changes made to their program as a result of COVID-19. When asked if they would be comfortable graduating with less than the traditional required number of cases, responses varied by training year. Junior residents were less comfortable with this (34%-42%), compared to senior residents (58%-65%).
COVID-19 appeared to have a positive effect on educational didactics, as the majority of the respondents (41.3%) reported receiving more didactics during the pandemic than before. 80.6% of respondents reported a transition to a completely online platform for didactics. Table 2 highlights the effect of COVID-19 on surgical education as reported by residents.
Table 2.
Effects of COVID-19 on Surgical Training
| Q6. Changes to resident schedules | |
| Residents completely removed from some services | 29% |
| More responsibility given to NPs and PAs | 77% |
| Smaller teams cover all the inhouse patients | 12.70% |
| No change made | 5.40% |
| Q7. Changes to operating room protocol | |
| No residents allowed | 1.40% |
| No interns or junior residents allowed | 12.30% |
| No residents allowed for high risk patients/case by case basis | 40.60% |
| No changes made | 31.60% |
| Q8. Changes in examining patients during rounds | |
| More frequently than before | 10.10% |
| Less frequently than before | 35.00% |
| My role did not change during rounds | 55.00% |
| Q9. Days off per month during the pandemic | |
| <4/month | 4.30% |
| 5-7/month | 23.50% |
| 8-10/month | 16.60% |
| Q10. Duty hour violations during the pandemic | |
| Yes | 26.60% |
| Q11. Surgical cases performed per week prior to the pandemic | |
| 0 case/week | 7.20% |
| 1-3 cases/week | 16.50% |
| 4-6 cases/week | 34.30% |
| More than 7 case/week | 37.10% |
| Q12. Surgical cases performed per week during the pandemic | |
| 0 case/week | 35.15% |
| 1-3 cases/week | 45.55% |
| 4-6 cases/week | 12% |
| More than 7 cases/week | 2.50% |
| Q13. Outpatient clinics attended per week prior to the pandemic | |
| 0 clinic/week | 15.54% |
| 1-4 clinic days/week | 76.74% |
| Q14. Outpatient clinics attended per week during the pandemic | |
| 0 clinic/week | 80.67% |
| 1-4 clinic days/week | 13.72% |
| Q15. How likely do you feel you will NOT meet the traditional ACGME minimum case requirements for your training year with the current schedule and operative volume changes? | |
| Likely | 42.20% |
| Not likely | 47.61% |
| Q16. Are you comfortable graduating with less than the traditional number of required cases? (Yes) | |
| PGY 1 | 34% |
| PGY 2 | 39.60% |
| PGY 3 | 42% |
| PGY 4 | 58% |
| PGY 5 | 65% |
| Q17. Effect of the pandemic on the amount of educational didactics provided | |
| More than prior | 41.30% |
| Less than prior | 34.60% |
| Q18. Educational curriculum now completely online | |
| Yes | 80.60% |
Resident Work Hours and Burnout
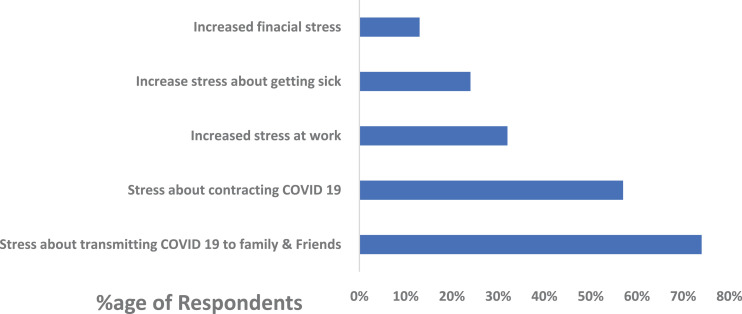
The average days off for surgery residents in the pre-COVID-19 era is 4 days per month. During the pandemic, 65.1% of respondents reported having 5 or more days off per month. Despite more time off overall, 33.1% of respondents reported more burnout than usual during the COVID-19 pandemic. 72.7% reported concern about potential transmission of COVID-19 to family members and friends, while 55% reported concern about contracting COVID-19 themselves. Table 3 highlights the effects of COVID-19 on resident wellbeing and burnout. Figure 2 highlights specific resident stressors during the COVID-19 pandemic.
Table 3.
Effects of COVID-19 on Resident Well-being and Burnout
| Q19. Do you feel more burnout now compared to before the pandemic? (Yes) | |
| PGY 1 | 38.80% |
| PGY 2 | 31.10% |
| PGY 3 | 34.90% |
| PGY 4 | 28.50% |
| PGY 5 | 28.50% |
| Q20. Compared to before, during the pandemic I spend more time on: | |
| Research | 49.50% |
| Hobbies | 44.20% |
| Reading/didactics | 49.40% |
| Family/significant others | 49.40% |
| Q21. During the pandemic I feel: | |
| Increased work-related stress | 31.80% |
| Increased financial stress | 13% |
| Increased stress about taking time off if I am sick | 23.10% |
| Stress about potentially transmitting COVID-19 to family/friends | 72.70% |
| Stress about contracting COVID-19 | 55.70% |
FIGURE 2.
Effect of COVID 19 on resident well-being.
DISCUSSION
We performed a survey to assess the effects of COVID-19 on surgical training, education, and burnout in surgical residents across the United States. By surveying trainees in all ACGME-accredited general surgical residency programs in the United States, we were able to comprehensively assess the overall effect of COVID-19 on surgical training. We saw a consistent decline in the number of surgical cases per week performed by residents during the pandemic compared to before, likely due to the elimination of elective cases nationwide. Other hospital policies to preserve personal protective equipment and decrease provider exposure, such as limiting residents in the operating room, has resulted in further reduction of surgical experience for residents. This is resulting in resident apprehension regarding their readiness for program completion and further studies are needed to determine what resident levels will be most impacted and what programmatic changes can be made to correct this deficit.
Another important finding of the study is that of resident wellness and burnout during the pandemic. The burn out rate was higher than the traditional rates reported in literature.8, 9, 10 Hewitt et al. in a national survey of general surgery residents reported a burnout rate of 22%.9. In our study 65.1% of respondents reported having 5 or more days off per month during the pandemic, compared to 4 days per month before. The increased time off is likely a result of schedule changes that remove residents from services with low clinical volume due to the elimination of elective cases, in addition to the strategy of keeping a healthy reserve of residents at home in the case of a surge. Despite more time off overall, 33.1% of respondents reported more burnout than usual during the COVID-19 pandemic. This suggests burnout is not just associated with long duty hours. Stress about contracting the virus and bringing it home to friends and family appears to be an important contributor to burnout during the pandemic. We found that the PGY 1 class experienced more burnout than the other classes.9 , 10 At this time, the immediate concerns pertaining to COVID-19 are on the forefront of research and planning. However, as time goes on, it can be anticipated that people will experience anxiety and depression. The data accumulated in this survey demonstrates that there are immediate emotional impacts and in order to manage these concerns and attempt to ameliorate future consequences, program should consider implementing aggressive and accessible wellness programs.
One positive consequence of the pandemic is that of increased resident educational didactics. The majority of the residents reported a shift to online didactics and an increase in overall didactic time during the COVID-19 pandemic. The use of technology allows residents to connect at any time of the day, from any location, with any expert present anywhere in the country. Several questions have been raised about the benefits of telemedicine; we believe COVID 19 has highlighted the significance of telemedicine. From online didactics to virtual rounds to tele-clinic, the COVID-19 pandemic has brought telemedicine into a new light which will help us significantly in post COVID era.
We did not discuss the response rate of our survey. According to the Association of American Medical Colleges in 2018 there were 7378 residents in ACGME approved general surgery programs. So, if we were to use that number our response rate will be 14.6% (1102/7378). This however is subject to debate as the number of total residents as mentioned by Association of American Medical Colleges does include residents who are in active research year and also the other major factor being the survey was not equally distributed to all the residents in the United States. Hence, the true response rate of this study would be hard to gauge.
Our study has several limitations typical of survey-based studies. First, we had a low response rate. The survey was emailed to all program directors and coordinators in the United States. It was at their discretion if it was sent to the residents or not. Though the total response rate may be low, we had a higher response states from states with higher incidence of Coronavirus such as New York and California. Also, because of lower response, only descriptive analysis was used. Another limitation was that participation was voluntary, meaning it is possible that people who had strong opinions regarding surgical education and COVID 19 are more likely to complete the survey, resulting in selection bias.
Surgical education aims to provide resident physicians with a foundation of surgical knowledge, clinical judgment, and technical competency. In the course of their training, residents are confronted with increasing clinical complexity and take on graded responsibility.11 Even before the current global pandemic, surgical education has needed to respond to dynamic changes in knowledge of surgical disease, new technologies, new treatments, and new procedures. Simultaneously, the public demand for greater accountability, resident oversight, and patient safety has pushed programs to re-examine their training practices.10 Experience suggests that the usual slow-paced response to changing training models will prove ineffective in the face of a rapidly escalating global crisis that is forcing many trainees to stay home, and a greater number to shift their attention from the management of surgical patients to preparing to manage critically ill medical patients.12, 13, 14
While there may be no way to replace direct hands-on training in the operating room during this pandemic, programs can support trainees’ clinical development in other ways, taking advantage of the fact that many residents and faculty have more time off now than ever before. Programs should provide increased support for trainees’ clinical development in nontechnical skills, such as providing opportunities and courses related to teamwork development, crisis management, leadership, and residents as educators.15, 16, 17 Professional development can also be supported in the realms of research and academic productivity, career planning, and financial literacy. Residents approaching graduation can continue to prioritize completing case logs, preparing for board examinations, and career transitions (e.g., credentialing/licensing paperwork).18, 19, 20
Footnotes
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Appendix 1. COVID-19 and Surgical Training, Education, and Burnout
What is your residency year?
-
○
PGY1-2
-
○
PGY3-4
-
○
PGY5
Which of the following best describes your training institution?
-
○
University hospital
-
○
Community hospital with university affiliation
-
○
Nonuniversity affiliated hospital
In which state is your training program?
Do you plan to pursue a fellowship?
-
○
Yes
-
○
No
-
○
Unsure
Have you personally cared for a COVID-19 positive patient at your hospital, involving face-to-face interaction?
-
○
Yes
-
○
No
-
○
Unsure (tests were pending or not performed)
What scheduling changes, if any, has your program made in response to the COVID-19 pandemic? (select all that apply)
□ Residents have been completely removed from some services
□ A smaller team of in-house residents covers more patients
□ More work is delegated to advanced practice providers (i.e. nurse practitioners, physician assistants)
□ No changes have been made to my program
□ Other ________________________________________
What operating room changes, if any, have your hospital(s) made to limit the number of people in the operating room during a case? (select all that apply)
□ No residents are allowed in the operating room
□ Interns and/or junior residents are not allowed in the operating room
□ Residents are allowed into the operating room on a case-by-case basis (i.e. not allowed in high-risk cases)
□ No changes have been made at my hospital(s)
□ Other ________________________________________
How many surgical cases on average per week were you performing prior to the COVID-19 pandemic?
-
○0 cases/week
-
○1-3 cases/week
-
○4-6 cases/week
-
○More than 7 cases/week
-
○
How many surgical cases on average per week are you performing during the COVID-19 pandemic?
-
○0 cases/week
-
○1-3 cases/week
-
○4-6 cases/week
-
○More than 7 cases/week
-
○
How many clinic days on average per week were you attending prior to the COVID-19 pandemic?
-
○0 clinic days/week
-
○1-3 clinic days/week
-
○More than 4 clinic days/week
-
○
How many clinic days (not including telemedicine visits) on average per week are you attending during the COVID-19 pandemic?
-
○0 clinic days/week
-
○1-3 clinic days/week
-
○More than 4 clinic days/week
-
○
Compared to before, during the COVID-19 pandemic, how has your role examining patients on rounds changed?
-
○I examine patients less frequently on rounds now
-
○I examine patients more frequently on rounds now
-
○My role examining patients on rounds has not changed
-
○
How many days off per month on average do you have during the COVID-19 pandemic?
-
○Less than 4 days off per month
-
○4 days off per month
-
○5-7 days off per month
-
○8-10 days off per month
-
○More than 10 days off per month
-
○
Have you violated the 80-hour per week duty requirement during the COVID-19 pandemic?
-
○Yes
-
○No
-
○Unsure
-
○
If the COVID-19 pandemic persists until June, how likely do you feel you will not meet the traditional ACGME case minimum requirements for your training year or program (not including the new accommodated requirements)?
-
○Very likely
-
○Likely
-
○Somewhat likely
-
○Not likely
-
○Unsure
-
○
Q16 Would you feel comfortable graduating with less cases than the traditional number required by the ACGME, even if you met new accommodated requirements?
-
○Yes
-
○No
-
○
How concerned are you that the changes in your surgical training during the COVID-19 pandemic will make you less prepared in your next career step (fellowship or as a new attending)?
-
○Very concerned
-
○Concerned
-
○Somewhat concerned
-
○Not concerned
-
○
What effect, if any, has the COVID-19 pandemic had on the amount of educational didactics provided by your program (including lectures, conferences, etc.)?
-
○More didactics than before the pandemic
-
○Less didactics than before the pandemic
-
○No change in didactics
-
○Unsure
-
○
Has your educational curriculum been moved to a completely online format?
-
○Yes
-
○No
-
○Unsure
-
○
What changes, if any, have been made to your educational curriculum during the COVID-19 pandemic? (select all that apply)
□ Some didactics have been moved online, but others remain in-person
□ In-person didactics now fulfill social distancing requirements (i.e. smaller groups, distancing between group members, etc.)
□ No changes have been made to my educational curriculum
□ Other ________________________________________
Compared to before, during the COVID-19 pandemic I feel:
-
○Less burned out
-
○More burned out
-
○No differently in terms of burnout
-
○
Compared to before, during the COVID-19 pandemic I spend (select all that apply):
□ More time with family/significant others/friends
□ More time on hobbies
□ More time on educational activities (i.e. reading, didactics, etc.)
□ More time on research activities
□ More time on: _________________________________
□ None of the above
Compared to before, during the COVID-19 pandemic I have felt (select all that apply):
□ Increased stress at work (i.e. longer patient lists, sicker patients, greater responsibility, etc.)
□ Increased stress about missing work if I am sick
□ Increased financial stress
□ Stress about contracting COVID-19
□ Stress about potentially transmitting COVID-19 to others in my family, community, etc.
□ Other: ________________________________________
□ None of the above
References
- 1.“Naming the coronavirus disease (COVID-19) and the virus that causes it”. who.int. Retrieved 24 April 2020.
- 2.“Coronavirus very likely of animal origin, no sign of lab manipulation: WHO”. Reuters. 21 April 2020. Retrieved 1st May 2020.
- 3.WHO Coronavirus disease (COVID-2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed May 1, 2020.
- 4.Lau S.K., Luk H.K., Wong A.C. Possible bat origin of severe acute respiratory syndrome Coronavirus 2. Emerging Infectious Diseases. 2020;26(7) doi: 10.3201/eid2607.200092. PMID 32315281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.“WHO | Novel Coronavirus—China”. WHO. Retrieved 9 May 2020.
- 6.“COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU)”. ArcGIS. Johns Hopkins University. Accessed May 15, 2020.
- 7.Accreditation Council for Graduate Medical Education. “ACGME Response to Coronavirus (COVID19)”. Last Updated, March 18, 2020. Available at: https://acgme.org/Newsroom/NewsroomDetails/ArticleID/10111/ACGME-Response-to-the-Coronavirus-COVID-19. Accessed March 20, 2020.
- 8.Yuce T.K., Turner P.L., Glass C. National evaluation of racial/ethnic discrimination in US surgical residency programs [published online ahead of print, 2020 Apr 15] JAMA Surg. 2020 doi: 10.1001/jamasurg.2020.0260. e200260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hewitt D.B., Ellis R.J., Chung J.W. Association of surgical resident wellness with medical errors and patient outcomes [published online ahead of print, 2020 Apr 8] Ann Surg. 2020 doi: 10.1097/SLA.0000000000003909. [DOI] [PubMed] [Google Scholar]
- 10.Bilimoria KY, Chung JW, Hedges LV, et al. National cluster-randomized trial of duty-hour flexibility in surgical. [DOI] [PubMed]
- 11.Kogan M., Klein S.E., Hannon C.P., Nolte M.T. Orthopaedic education during the COVID-19 pandemic [published online ahead of print, 2020 Apr 8] J Am Acad Orthop Surg. 2020 doi: 10.5435/JAAOS-D-20-00292. 10.5435/JAAOS-D-20-00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daodu O., Panda N., Lopushinsky S., Varghese T.K., Jr, Brindle M. COVID-19 - considerations and implications for surgical learners [published online ahead of print, 2020 Apr 16] Ann Surg. 2020 doi: 10.1097/SLA.0000000000003927. 10.1097/S—LA.0000000000003927. [DOI] [PubMed] [Google Scholar]
- 13.García-Lozano J.A., Cuellar-Barboza A., Garza-Rodríguez V., Vázquez-Martínez O., Ocampo-Candiani J. Dermatologic surgery training during the COVID-19 era [published online ahead of print, 2020 May 9] J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16621. 10.1111/jdv.16621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Givi B., Moore M.G., Bewley A.F. Advanced head and neck surgery training during the COVID-19 pandemic [published online ahead of print, 2020 May 8] Head Neck. 2020 doi: 10.1002/hed.26252. 10.1002/hed.26252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yuce T.K., Turner P.L., Glass C. National evaluation of racial/ethnic discrimination in US surgical residency programs [published online ahead of print, 2020 Apr 15] JAMA Surg. 2020 doi: 10.1001/jamasurg.2020.0260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Wolf M., Birch E. A simple solution to improve surgical teaching amongst medical students: Comments on: Daily medical education for confined students during COVID-19 pandemic: a simple videoconference solution [published online ahead of print, 2020 May 5] Clin Anat. 2020 doi: 10.1002/ca.23618. 10.1002/ca.23618. [DOI] [Google Scholar]
- 17.Singh K., Srivastav S., Bhardwaj A., Dixit A., Misra S. Medical education during the COVID-19 pandemic: a single institution experience [published online ahead of print, 2020 May 4] Indian Pediatr. 2020 doi: 10.1007/s13312-020-1899-2. S097475591600174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roy S.F., Cecchini M.J. Implementing a structured digital-based online pathology curriculum for trainees at the time of COVID-19 [published online ahead of print, 2020 May 4] J Clin Pathol. 2020 doi: 10.1136/jclinpath-2020-206682. jclinpath-2020-206682. [DOI] [PubMed] [Google Scholar]
- 19.Sheikh M.R., Osman H., Butt M.U., Jeyarajah D.R. Perception of training in hepatopancreatobiliary surgery among general surgery residents in the Americas. HPB (Oxford) 2016;18:1039‐1045. doi: 10.1016/j.hpb.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aziz H., Filkins A., Kwon Y.K. Review of COVID 19 outcomes in surgical patients. Am Surg. 2020 doi: 10.1177/0003134820934395. [published online ahead of print, 2020 Jul 15] [DOI] [PubMed] [Google Scholar]