Abstract
Background
There remains a great deal of controversy regarding the selection of long-segment fixation and short-segment fixation, especially for degenerative scoliosis (DS) patients with Cobb angle 20°~40°. The purpose of this study was to investigate the effects of different fixation levels in DS patients with Cobb angle 20°~40°.
Material/Methods
We enrolled 96 DS patients, divided into a long-segment fixation group (>3 segments) and a short-segment fixation group (≤3 segments). The visual analogue scale (VAS) and Oswestry disability index (ODI) were used to evaluate the clinical outcomes. The spinal-pelvic parameters and complications were also collected and analyzed.
Results
The short-segment fixation group had the advantages of less blood loss, shorter operation time and shorter fluoroscopy time (P<0.05). The 2 groups achieved similar effects in leg pain (VAS) and ODI after operation (P>0.05); however, there was a better relief of low back pain in the long-segment fixation group (P<0.05). The changes of Cobb angle, sagittal vertical axis (SVA), lumbar lordosis (LL), pelvic tilt (PT) and sacral slope (SS) in the long-segment fixation group were more obvious than that in the short-segment fixation group at the final follow-up (P<0.05). The prevalence of complications in the long-segment fixation group was significantly higher than in the short-segment fixation group (P<0.01).
Conclusions
Short-segment fixation has less surgical trauma and fewer complications, whereas long-segment fixation has more advantages in improving spine-pelvis parameters and relieving low back pain.
MeSH Keywords: Anastomosis, Surgical; Anatomy, Comparative; Scoliosis; Spine
Background
Degenerative scoliosis (DS) refers to primary spinal deformity with coronal Cobb angle above 10°, which may be caused by asymmetric degeneration of intervertebral discs and articular processes [1]. Several studies suggested that the average Cobb angle is 22.3°~32.5° and 4 segments are always involved [2–4]. Patients need surgery when their quality of life is seriously affected, and the common surgical methods include decompression alone, decompression with short-segment (limited) fixation, and long-segment fixation with full curve correction [5]. However, there is a serious controversy regarding the selection of long-segment fixation and short-segment fixation [6,7].
Bao et al. recommended short-segment fixation in patients with Cobb angle <20° because their vertebral rotation and lateral slip are small with no sagittal imbalance [8]. A positive correlation has been found between Cobb angle and sagittal imbalance in some studies [2,3,9]. Patients are often disturbed by severe sagittal imbalance when their Cobb angle >40° [10,11]. Accordingly, some researchers recommended long-segment fixation when Cobb angle >40° to correct 3-dimensional malformations of the spine, especially in patients with severe sagittal imbalance [5,12,13].
Thus, the main controversial point for the selection of long- and short-segment fixation is the DS patients with Cobb angle 20°~40°, because the degeneration of their spine is mild-to-moderate [1,6,14]. In addition, it includes a large proportion of clinical patients [11,15]. However, the effects of the 2 surgical methods in DS patients with Cobb angle 20°~40° has not been previously explored.
Therefore, the aim of this study was to explore and compare the effects of long-segment fixation and short-segment fixation on clinical outcomes and spinal-pelvic parameters in DS patients with Cobb angle 20°~40°, and try to provide a theoretical basis for the clinical treatment of DS.
Material and Methods
Study design
This study was a retrospective review of surgical, radiographic, and clinical parameters for the treatment of DS. All surgeons involved had significant experience within their respective patient cohorts, and all parameters were measured by 2 senior physicians. Patients were stratified into 2 groups: the long-segment fixation group (the fixation segments >3) and the short-segment fixation group (the fixation segments ≤3) [13].
Inclusion criteria: (1) coronal Cobb angle 20°~40°; (2) leg pain and numbness due to neurogenic claudication; (3) complete radiographic and clinical parameters. Exclusion criteria: (1) spinal deformity caused by infection, tumor or fracture; (2) history of spine surgery; (3) lower-limb deformity affecting balance; (4) patients younger than 40 years old. Follow-up was a minimum of 24 months for each included subject.
A total of 138 cases met the inclusion criteria in our hospital between January 2013 and September 2017; 37 patients were excluded based on exclusion criteria, and 8 patients were excluded based on lack of 24-month follow-up and/or lack of clinical data. Finally, a total of 51 patients were enrolled in the short-segment fixation group (average fixation segments were 2.12±0.82) and 45 were enrolled in the long-segment fixation group (average fixation segments were 5.31±1.34) (Figure 1). Of the 96 patients, 34 patients were male and 62 were female. The average age of the patients was 69.5±7.6 years at the time of surgery. The average follow-up period was 28.6±17.4 months. The distribution of end vertebrae was: 6 cases of T9, 7 cases of T10, 9 cases of T11, 11 cases of T12, 17 cases of L1, 25 cases of L2, and 21 cases of L3 for the upper vertebrae, while there were 21 cases of L3, 45 cases of L4, and 30 cases of L5 for the lower vertebrae.
Figure 1.
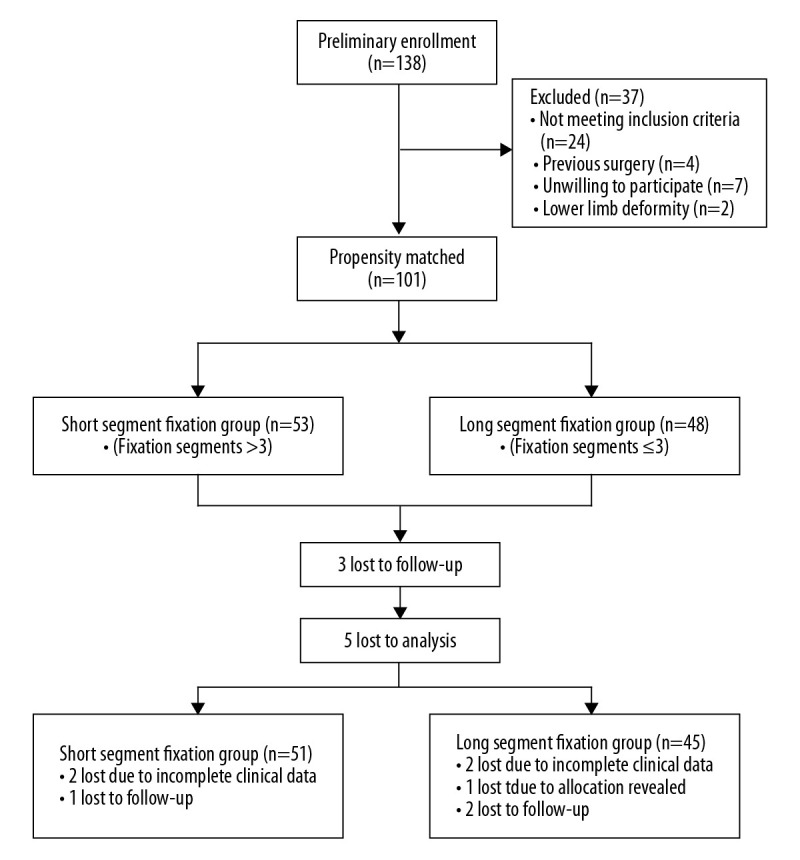
Diagram showing the process of patient selection.
Surgical procedure and postoperative management
All patients underwent general anesthesia with routine tracheal intubation in prone position and posterior median incision. The surgical process consisted of 3 steps: decompression, fixation with pedicle screw, and fusion. Decompression was performed for nerve roots and dural sac when there were sciatica and neurological claudication with evidence of compression at the imaging examination such as magnetic resonance image (MRI) or discography. Fusion was performed with a cage for unstable segments after decompression, segments with obvious lateral slip, and L5/S1 segments fixed to the sacrum. The hollow part of the cage was filled with autogenous bone fragments, and allogeneic bone was employed if necessary. The fixation was determined by the severity of imbalance in the sagittal plane and coronal plane of the spine before operation. Cefuroxime sodium was routinely administered during the first 3 days after operation. Back muscle function exercises started gradually from the second day, and patients could get out of bed using brace protection from the third day after operation.
Institutional Review Board: The First Affiliated Hospital of Chongqing Medical University. [2019, July 15th, Ethics of Scientific Research (2019-177)].
Outcome measurements
Clinical outcomes assessment
Health-related quality of life measures (ODI and VAS) were obtained from each patient. ODI is a measure of functional disability, with scores ranging from 0 to 100, while VAS is a measure of low back and leg pain, with scores based on a scale of 0 to 10. The higher the scores, the more obvious the functional disability. Data on other clinical characteristics were also collected: operation time, blood loss, fluoroscopic time, hospital stay, and complications of surgery.
Spino-pelvic parameters assessment
The spino-pelvic parameters were digitized and stored by PACS (Picture Archiving and Communication Systems; Shenzhen Annet Information System, China). The following radiographical parameters were measured through PACS: coronal Cobb angle (Cobb angle), sagittal vertical axis (SVA), thoracolumbar kyphosis (TK), thoracolumbar kyphosis (TLK), lumbar lordosis (LL), pelvic incidence (PI), pelvic title (PT) and sacral slope (SS). All parameters were measured by 2 senior physicians, and the evaluation procedure was finished by 1 tester acting as the independent observer in a blinded manner (Figure 2).
Figure 2.
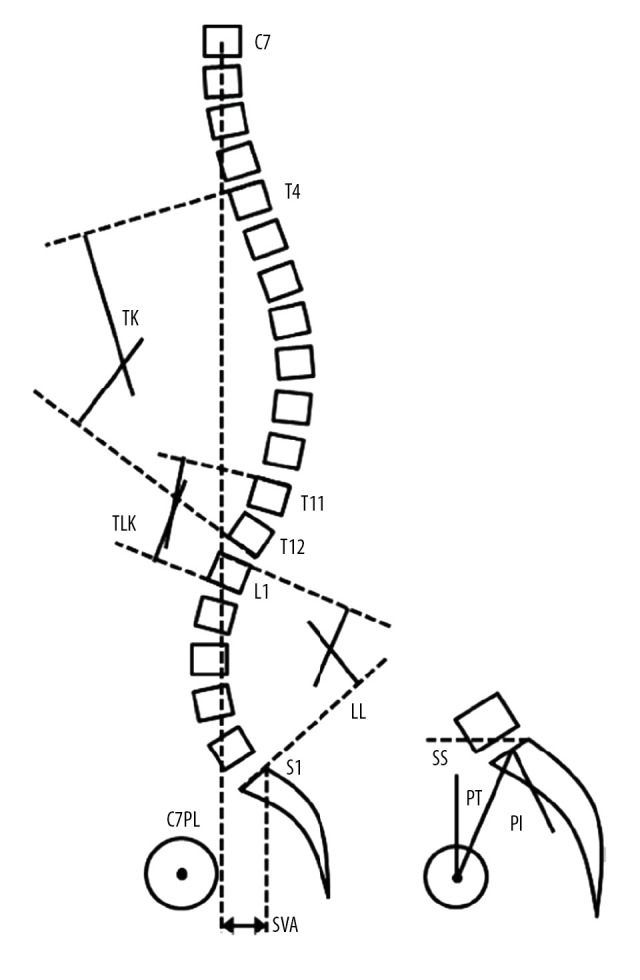
Schematic diagram of the spino-pelvic parameters measurements. TK – thoracic kyphosis; TLK – thoracolumbar kyphosis; SVA – sagittal vertical axis; LL – lumbar lordosis; SS – sacral slope; PT – pelvic tilt; PI – pelvic incidence; C7PL – C7 plumb line.
Statistical analysis
The data were analyzed using SPSS 21.0 (SPSS, Inc, Chicago, IL). Clinical outcomes and spine-pelvis parameters are reported as mean±standard deviations (SD). The paired-sample t test was used for intra-group comparison, and the independent-samples t test was used for inter-group comparison. Count data of complications are presented as numbers or ratios, and the chi-square test was used for comparisons. Statistical significance was indicated at P<0.05.
Results
Intraoperative data
The short-segment fixation group had relatively little surgical injury whose operation time, blood loss, and intraoperative fluoroscopy times were lower than in the long-segment fixation group (P<0.05), but the days of hospitalization between the 2 groups had no significantly difference (P>0.05) (Table 1).
Table 1.
Clinical information about the patients.
| Groups | Number (n) | Operation time (min) | Blood loss (ml) | Fluoroscopy time (times) | Hospital stay (d) |
|---|---|---|---|---|---|
| Long-group | 45 | 238±44 | 352±68 | 8.42±3.55 | 9.56±3.43 |
|
| |||||
| Short-group | 51 | 159±32 | 231±53 | 6.16±3.02 | 8.42±2.77 |
|
| |||||
| Statistic | – | t=10.140 | t=9.781 | t=3.801 | t=1.801 |
| P=0.000 | P=0.000 | P=0.003 | P=0.075 | ||
Long-group: long segment fixation group; Short-group: short segment fixation group.
Clinical outcomes
The health-related quality of life (VAS and ODI) of the 2 groups was significantly improved after operation (P<0.05), and further improved at the final follow-up compared with 3–6 months after operation (P<0.05). The improvement in ODI and leg pain (VAS) between the 2 groups was not significantly different at the final follow-up (t=1.937, p=0.060; t=1.159, p=0.249), but a better lower-back pain relief was observed in the long-segment fixation group compared with the short-segment fixation group (t=4.771, p=0.000) (Table 2).
Table 2.
Comparison of the health-related quality of life.
| Groups | ODI | Low leg pain(VAS) | Low back pain(VAS) | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Pre-op | 3-6 M after-op | Final follow-up | Pre-op | 3–6 M after-op | Final follow-up | Pre-op | 3–6 M after-op | Final follow-up | |
| Long-group | 72.32±18.64# | 35.82±17.17* | 26.54±8.36*# | 6.33±1.78# | 3.12±1.47* | 2.14±1.38*# | 4.27±1.24# | 2.71±0.87* | 1.42±0.56*# |
|
| |||||||||
| Short-group | 64.72±19.43# | 33.61±16.62* | 23.73±7.55*# | 6.06±1.36# | 2.86±1.56* | 1.68±0.98*# | 3.54±1.13# | 2.36±0.71* | 1.25±0.42*# |
|
| |||||||||
| Statistic | t=1.949 | t=0.640 | t=1.731 | t=0.841 | t=0.837 | t=1.899 | t=3.017 | t=2.169 | t=1.694 |
| P=0.054 | p=0.523 | p=0.086 | p=0.403 | p=0.405 | p=0.061 | p=0.003 | p=0.033 | p=0.093 | |
Compared with pre-op value, P<0.05;
compared with the value at 3–6 M after operation, P<0.05.
Pre-op – preoperative; 3–6 M after-op – 3–6 months after operation.
Spino-pelvic parameters
Compared with the preoperative values, the Cobb angle, SVA, and PT decreased significantly, TK, SS and LL increased significantly in the long-segment fixation group at 3–6 months after operation and at final follow-up (P<0.05). Similarly, the Cobb angle, SVA, and PT decreased and only SS increased in the short-segment fixation group (P<0.05). The changes in Cobb angle, SVA, LL, PT, and SS in the long-segment fixation group were greater than that in the short-segment fixation group at the final follow-up (P<0.05). Spine-pelvis parameters of the 2 groups remained stable at the final follow-up, but the SVA of the short-segment fixation group was slightly higher than that at 3–6 months (P<0.05) (Table 3).
Table 3.
Comparison of spinal-pelvic parameters.
| Parametes | Long-group | Short-group | ||||
|---|---|---|---|---|---|---|
| Pre-op | 3–6 M after-op | Final follow-up | Pre-op | 3–6 M after-op | Final follow-up | |
| Cobb’s (°) | 33.43±8.99# | 12.77±6.05* | 13.23±6.46* | 25.38±7.64#@ | 11.69±5.63* | 13.46±5.75* |
| SVA(mm) | 63.11±20.76# | 20.01±11.82* | 22.76±12.23* | 46.26±23.46#@ | 23.67±13.15* | 31.78±13.27*# |
| TK (°) | 20.36±15.68 | 25.58±9.81 | 27.43±8.96* | 23.45±12.43 | 25.63±11.42 | 26.47±10.72 |
| TLK (°) | 15.73±11.68# | 10.54±9.77* | 11.53±8.96 | 12.46±9.71 | 11.25±10.43 | 11.76±9.41 |
| LL (°) | 27.71±11.42# | 38.64±12.76* | 37.42±13.52* | 32.65±12.63@ | 36.47±11.98 | 35.86±12.72 |
| PI (°) | 47.01±8.56 | 48.23±8.73 | 47.76±7.48 | 46.46±8.38 | 46.44±8.26 | 45.93±7.48 |
| PT (°) | 23.26±8.69# | 16.73±6.34* | 15.21±6.74* | 21.92±8.27# | 17.81±6.82* | 17.84±6.15*@ |
| SS (°) | 24.72±7.63# | 31.31±6.21* | 32.45±5.86* | 26.56±7.21# | 29.61±6.02* | 30.11±5.52*@ |
Intra-group:
Compared with pre-op value, P<0.05;
compared with the value at 3–6 M after operation, P<0.05; Out-group:
Compared with Long-group at the same time point, P<0.05.
Cobb’s – coronal Cobb’s angle; SVA – sagittal vertical axis; TK – thoracic kyphosis; TLK – thoracolumbar kyphosis; LL – lumbar lordosis; PI – pelvic incidence; PT – pelvic tilt; SS – sacral slope.
Complications
The incidence of complications in the long-segment fixation group (15 of 45=33.33%) was significantly higher than that in the short-segment fixation group (10 of 51=19.61%) (P<0.001), and no perioperative deaths occurred in either group (Table 4). Six of 96 (6.25%) patients had pseudarthroses, and all patients with implant failure had pseudarthroses. Seven of 96 (7.29%) patients had a proximal problem. One patient (1.04%) had distal junctional kyphosis. A total of 6 patients developed cerebrospinal fluid leakage after operation, and, unfortunately, 1 patient developed secondary wound infection with Staphylococcus aureus.
Table 4.
Comparison of complications.
| Parametes | Long-group | Short-group |
|---|---|---|
| System diseases | 3 | 1 |
| Cerebrospinal fluid leakage | 4 | 2 |
| Infection | 1 | 0 |
| Proximal junctional problems | 2 | 5 |
| Pseudoarthrosis | 4 | 2 |
| Distal junctional kyphosis | 1 | 0 |
| Revision surgery | 5 | 5 |
| Prevalence of complications | 15/45 | 10/51 |
| Prevalence of revision | 5/45 | 5/51 |
Suffering from a serious systemic disease that requires re-admission in 1 month after operation, such as heart failure, pneumonia and urinary tract infection. Proximal junctional problem such as global sagittal imbalance, proximal junctional kyphosis (PJK), and fracture at the uppermost instrumented vertebra (UIV)
Ten of 96 (10.41%) patients had subsequent revision surgery performed at an average 3.5 years after operation. There were 5 revisions performed in the long-segment fixation group (11.11%). Four of 45 (8.89%) patients had pseudarthroses, and 2 of them had nail rod fracture with obvious displacement requiring revision surgery. The other 1 had distal junctional kyphosis with the lowest instrumented vertebra (LIV) at L5. Two patients had proximal junctional problems – 1 fracture at the uppermost instrumented vertebra (UIV) and 1 proximal junctional kyphosis associated with spinal stenosis. The short-segment fixation group also had 5 revisions (9.80%). Two of 51 (3.92%) patients had pseudarthroses and the other 3 patients had proximal junctional problems – 1 sagittal imbalance, 1 sagittal imbalance with spinal stenosis, and 1 proximal junctional kyphosis (PJK) with spinal stenosis. The prevalence of revision surgery was not significantly different between groups (5 of 45 in the long-segment group and 5 of 51 in the short-segment group) (χ2=0.044; P=0.834). A typical case is shown in Figures 3, 4.
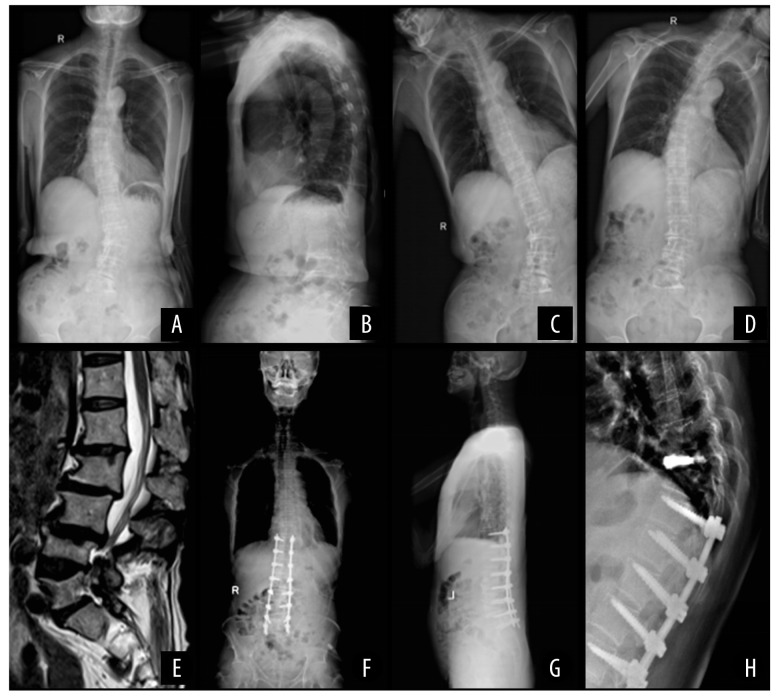
Figure 3.
Long-segment fixation. A 65-year-old male patient. (A, B) X-ray films of the whole spine in standard standing position before operation: Cobb angle: 36.35°, SVA: 63.35 mm, TK: 19.63°, TLK: 9.35°, LL: 19.28°, PI: 43.03°, PT: 20.37°, SS: 23.99°; (C, D) The X-ray film of left and right bending position before operation; (E) Sagittal MRI before operation; (F, G) Four months after operation, X-ray films of the whole spine in standard standing position: Cobb angle: 17.41°, SVA: 19.34 mm, TK: 17.53°, TLK: 6.79°, LL: 36.28°, PI: 41.42°, PT: 14.66°, SS: 26.02°; (H) At the eighth month after operation, patients with vertebral compression fractures, and percutaneous vertebroplasty (PVP) was performed.
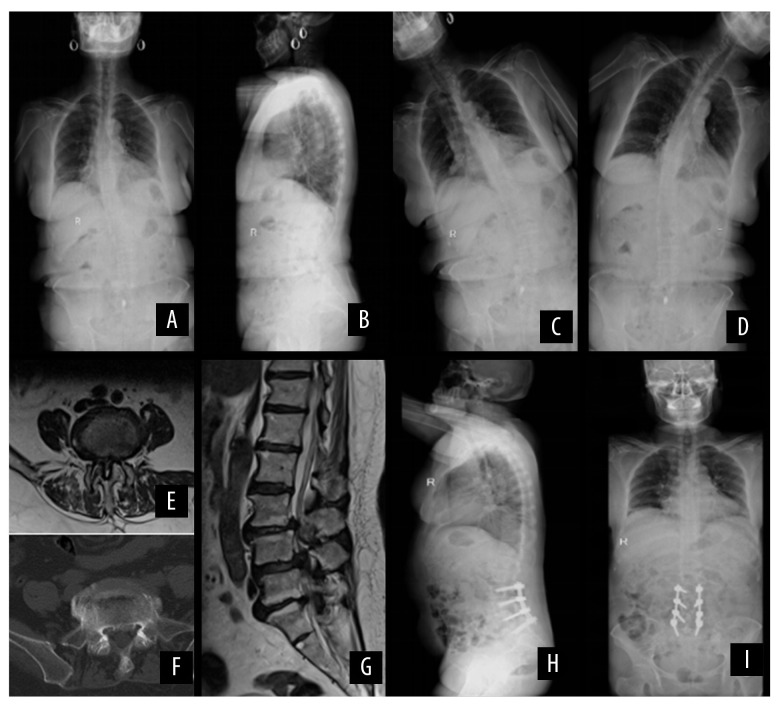
Figure 4.
Short-segment fixation. A 63-year-old female patient. (A, B) X-ray films of the whole spine in standard standing position before operation: Cobb’s: 30.13°, SVA: 10.06mm, TK: 12.36°, LL: 28.57°, PI: 44.45°, PT: 21.43°, SS: 24.14°; (C, D) The X-ray film of left and right bending position before operation; (E) Preoperative transaxial plane of MRI showed spinal stenosis; (F) Preoperative transaxial plane of CT scans showed hyperosteogeny at the edge of vertebral body; (G) Sagittal MRI shows disc herniation with dural sac compression; (H, I) One year after operation, X-ray films of the whole spine in standard standing position: Cobb’s: 10.41°, SVA: 34.34mm, TK: 24.53°, TLK: 13.79°, LL: 28.28°, PI: 45.42°, PT: 17.68°, SS: 27.43°.
Discussion
DS patients often have intractable low back and leg pain, and most of them are middle-aged and elderly [12,15]. The Cobb angle of most patients is less than 40°, and the curve progresses by about 3° per year [3,16]. Our research showed that the average Cobb angle was 29.41°, with a mild-to-moderate sagittal imbalance. At present, there is no definitive surgical strategy for DS patients with Cobb angle 20°~40° because the circumstances surrounding each patient are highly complex [3,5,12,13]. Therefore, it is necessary to compare the outcomes of long- and short-segment fixation on DS.
In our research, satisfactory clinical outcomes were obtained in both groups after surgery. The ODI improved from 68.3 to 34.7 and leg pain (VAS score) improved by 4.25 points (the improvement rate was 68%), but there was no significant difference between the 2 groups, which was similar to the results of a meta-analysis reported by Lee [16]. However, Sun et al. showed that the improvement rate of ODI in the long-segment fixation group (83.1%) was significantly higher than in the short-segment fixation group (60.8%), and they believed long-segment fixation was more beneficial to reconstruction of the 3-dimensional deformity and better dispersed the stress of the nail rod [17]. The reasons for the same improvement in quality of life in both groups are still unclear, and the mild-to-moderate sagittal imbalance may be one of the reasons [18]. Compared with coronal imbalance, sagittal imbalance had a greater impact on the quality of life of patients; and when SVA was >6 cm, the ODI was significantly higher [19,20]. However, the average preoperative SVA was 54.18 mm in patients with Cobb angle 20°~40°, and then decreased to 27.27 mm at the final follow-up. The quality of life was not significantly affected for patients with mild-to-moderate sagittal imbalance.
Additionally, the compensation for stenosis also should be considered. A forward-bending posture was observed in patients with DS, which is an effective way to relieve neural compression by increasing the volume of the central vertebral canal and the intervertebral foramina [21]. Clinically, patients with a forward-bending posture may resemble a patient with sagittal imbalance. On one hand, we found that the imbalance of some patients was significantly reduced by the release of muscle spasm after anesthesia, thus we reduced the fixation of 1 to 2 segments during the operation. However, the patient’s quality of life was not as bad as we expected at the final follow-up. On other hand, for some patients who received treatment of lumbosacral deformity by short-segment fixation, the upper segment bending was obviously corrected by self-repair, and they also achieved good clinical outcomes with stable spine-pelvis parameters at the final follow-up [22]. Therefore, the sagittal imbalance needs to be carefully evaluated before surgery, and selection of mild-to-moderate sagittal imbalance patients with short-segment fixation can achieve no worse clinical outcomes than long-segment fixation.
Low back pain (axial pain) is often the main symptom at onset and the chief complaint at the first visit to the clinic for DS. Recent studies have shown that paraspinal muscle spasm caused by sagittal and coronal imbalance is the main mechanism of low back pain [23]. Unfortunately, dramatic pain relief is not established in some patients, and 15–30% continue to experience chronic pain in the months and years after surgery [24]. In our research, better low back pain relief was observed in the long-segment fixation group compared with the short-segment fixation group, which may be related to the improvement of spinal-pelvic parameters [25]. The improvement of SVA, PT, PI-LL, SS and LL in the long-segment fixation group was greater than that in the short-segment fixation group after operation. Some studies have shown that long-segment fixation is more conducive to return of the gravity center line to the economic cone, and it relieves low back pain by reducing muscle work needed to maintain balance [26,27]. Although long-segment fixation has more advantages in relieving low back pain, low leg pain is the key factor in health-related quality of life [1]; residual mild low back pain is acceptable for many patients after surgery [26]. Thus, the key point of the operation is to decompress the nerve roots and dural sac, as performed for sciatica and neurological claudication [16]. We prefer to use short-segment fixation, especially in elderly patients with DS, because it reduces surgical trauma and allows more activity.
The operation of DS is often accompanied by a high risk of complications due to older age, osteoporosis, and other organ diseases [28]. The prevalence of revision is an important index to test the complications. Pichelmann et al. reported the prevalence of revision was 9% for adult scoliosis through a 22-year follow-up study of 643 patients [29]. Yongjung et al. found the revision prevalence was 24.6% after degenerative lumbar scoliosis (DLS) instrumented fusion from the distal thoracic/upper lumbar spine (T9–L2) to L5 or S1 [30]. In our research, the revision prevalence was 10.41%, and was performed at an average 3.5 years after the first surgery. Pseudarthrosis and proximal junctional problems were the major causes of revision. A growing number of studies show that pseudarthrosis is related to the mismatch of spinal-pelvic parameters, fusion to thoracolumbar junction, and sagittal imbalance [31]. Fortunately, anterior or transforaminal lumbar interbody fusion (TLIF) of L5/S1, fixation into the ilium, and attention to the matching of PI-LL can reduce the incidence of pseudarthrosis [5,32].
The proximal junctional area of the patient is prone to stress concentration on the intervertebral disc, leading to PJK during postoperative follow-up, and the overall incidence of PJK was reported to be 12~43% [33]. In our research, there were 4 patients with PJK, and 3 of them underwent revision surgery. As we know, the incidence of PJK differs between the proximal thoracic vertebrae and the distal thoracic vertebrae. Shufflebarger et al. found the incidence of PJK was the lowest when UIV chose T9–T10, and recommended T9 or T10 as the UIV [34]. The risk factors for PJK have been shown in a growing body of research, including age > 55 years old, obesity, low bone mass, paraspinal muscle fat infiltration (weakening of posterior tension band), excessive LL and SVA correction, and PI-LL mismatch [35]. In our experience, the reconstruction of the LL is the key, and it should be based on the patient’s PI in order to avoid overcorrection (control PI-LL within 20°). Moreover, it is important to pay attention to the ratio between the upper and lower lumbar vertebrae, and to control the ratio at around 1: 2 when bending the bar.
The purpose of DS surgery is to improve the quality of life, not to correct deformities. Accordingly, considering the outcomes and complications, our treatment policy for DS patients with Cobb angle 20~40° is: “neural decompression is the key; deformity correction is the auxiliary; using the long-segment fixation as little as possible”. It represents a smaller operation and theoretically less likelihood of complications if fewer segments are being fused. In general, short-segment fixation is considered for patients with small Cobb angle, low risk of deformity progression, and no severe sagittal imbalance. However, long-segment fixation can be used cautiously when the following situations occur: 1) patients with repeated treatment of unrelieved low back and leg pain, and low back pain (VAS) ≥3 points; 2) severe sagittal imbalance, SVA >9.5 cm [36]; 3) loss of lumbar physiological kyphosis or lumbar kyphosis; 4) atrophy of back muscles, or with obvious fat infiltration [37]; and 5) no serious underlying disease and can able to withstand major orthopedic surgery.
There are several limitations of our study. First, the preoperative spine-pelvic parameters of the 2 groups were not propensity-matched. It is unrealistic to match each parameter exactly because DS is a complex disease with a variety of clinical manifestations and spine-pelvic parameters. The purpose of our study was to observe the effects of different fixation levels in patients with Cobb angle 20°~40°. Therefore, even if the spine-pelvic parameters were not propensity-matched, it does not contradict the purpose of our study. Second, we evaluated only the spine-pelvic parameters and clinical outcomes for the DS patients without analyzing the correlations. The correlations and other potential factors such as postoperative functional exercise, life style, bone mineral density, and atrophy of back muscles should be assessed in further research. Third, our sample size was limited in this single-center study and the follow-up time was relatively short, which causes unavoidable selection bias. Thus, large-scale and long-term follow-up studies are urgently needed.
Conclusions
DS patients with Cobb angle 20°~40° can achieve satisfactory clinical outcomes and improve the spine-pelvic parameters by choosing appropriate fixation levels. Short-segment fixation has less surgical trauma and fewer complications, whereas long-segment fixation has more advantages in improving spine-pelvis parameters and relieving low back pain.
Acknowledgments
The authors would like to thank the staff members of the 18th Ward at The First Affiliated Hospital of Chongqing Medical Iniversity for data collection, Zenghui Zhao for help with the operation, and Zhongyu Xiong for her assistance with Statistical analysis. We also thank the patients who participated in this study and the staff involved in this work.
Footnotes
Conflict of interest
None.
Source of support: This study was funded by the National Natural Science Foundation of China (81572634)
References
- 1.York PJ, Kim HJ. Degenerative scoliosis. Curr Rev Musculoskelet Med. 2017;10(3):1–12. doi: 10.1007/s12178-017-9445-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baghdadi YM, Larson AN, Dekutoski MB, et al. Sagittal balance and spinopelvic parameters after lateral lumbar interbody fusion for degenerative scoliosis: A case-control study. Spine. 2014;39(3):166–73. doi: 10.1097/BRS.0000000000000073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmid SL, Buck FM, Böni T, Farshad M. Radiographic measurement error of the scoliotic curve angle depending on positioning of the patient and the side of scoliotic curve. Eur Spine J. 2016;25(2):379–84. doi: 10.1007/s00586-015-4259-5. [DOI] [PubMed] [Google Scholar]
- 4.Yang C, Yang M, Chen Y, et al. Radiographic parameters in adult degenerative scoliosis and different parameters between sagittal balanced and imbalanced ADS patients. Medicine. 2015;94(29):e1198. doi: 10.1097/MD.0000000000001198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palmisani M, Dema E, Cervellati S. Surgical treatment of adult degenerative scoliosis. Eur Spine J. 2013;8(3):371–81. doi: 10.1007/s00586-013-3012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faldini C, Di MA, Borghi R, et al. Long vs. short fusions for adult lumbar degenerative scoliosis: Does balance matters? Eur Spine J. 2015;24(7 Suppl):887–92. doi: 10.1007/s00586-015-4266-6. [DOI] [PubMed] [Google Scholar]
- 7.Phan K, Xu J, Maharaj MM, et al. Outcomes of short fusion versus long fusion for adult degenerative scoliosis: A systematic review and meta-analysis. Orthop Surg. 2017;9(4):342–49. doi: 10.1111/os.12357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bao H, Yan P, Qiu Y, et al. Coronal imbalance in degenerative lumbar scoliosis: Prevalence and influence on surgical decision-making for spinal osteotomy. Bone Joint J. 2016;98-B(9):1227–33. doi: 10.1302/0301-620X.98B9.37273. [DOI] [PubMed] [Google Scholar]
- 9.Changwei Y, Mingyuan Y, Yuanyuan C, et al. Radiographic parameters in adult degenerative scoliosis and different parameters between sagittal balanced and imbalanced ADS patients. Medicine. 2015;94(29):e1198. doi: 10.1097/MD.0000000000001198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ploumis A, Hong L, Mehbod A, Transfeldt E. Can radiographic measurements of degenerative lumbar scoliosis predict clinical symptoms? Scoliosis. 2009;4(S1):O54. [Google Scholar]
- 11.Ploumis A, Liu HA. A correlation of radiographic and functional measurements in adult degenerative scoliosis. Spine. 2009;34(15):1581–84. doi: 10.1097/BRS.0b013e31819c94cc. [DOI] [PubMed] [Google Scholar]
- 12.Silva FE, Lenke LG. Adult degenerative scoliosis: Evaluation and management. Neurosurg Focus. 2010;28(3):E1. doi: 10.3171/2010.1.FOCUS09271. [DOI] [PubMed] [Google Scholar]
- 13.Phan K, Xu J, Maharaj MM, et al. Outcomes of short fusion versus long fusion for adult degenerative scoliosis: A systematic review and meta-analysis. Orthop Surg. 2017;9(4):342–49. doi: 10.1111/os.12357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jin DU, Song K, Shi XG, et al. [Effect of long and short segment fixation for degenerative scoliosis on spinal three-dimensional imbalance]. Academic Journal of Chinese PLA Medical School. 2013 [in Chinese] [Google Scholar]
- 15.Kotwal S, Pumberger M, Hughes A, Girardi F. Degenerative scoliosis: A review. HSS J. 2011;7(3):257–64. doi: 10.1007/s11420-011-9204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee CH, Chung CK, Sohn MJ, Kim CH. Short limited fusion versus long fusion with deformity correction for spinal stenosis with balanced de novo degenerative lumbar scoliosis: A meta-analysis of direct comparative studies. Spine (Phila Pa 1976) 2017;42(19):E1126–32. doi: 10.1097/BRS.0000000000002306. [DOI] [PubMed] [Google Scholar]
- 17.Sun Y, Shen Y, Ding W, et al. Comparison in clinical outcome of two surgical treatments in degenerative scoliosis. Cell Biochem Biophys. 2014;70(1):189–93. doi: 10.1007/s12013-014-9879-6. [DOI] [PubMed] [Google Scholar]
- 18.Daubs MD, Brara HS, Raaen LB, et al. How does sagittal imbalance affect the appropriateness of surgical indications and selection of procedure in the treatment of degenerative scoliosis? findings from the RAND auc study. Spine J. 2018;18:900–11. doi: 10.1016/j.spinee.2018.01.027. [DOI] [PubMed] [Google Scholar]
- 19.Lee BH, Park JO, Kim HS, et al. Spinal sagittal balance status affects postoperative actual falls and quality of life after decompression and fusion in-situ surgery in patients with lumbar spinal stenosis. Clin Neurol Neurosurg. 2016;148:52–59. doi: 10.1016/j.clineuro.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 20.Hui L, Sibei L, Jiranru W, et al. An analysis of spinopelvic sagittal alignment after lumbar lordosis reconstruction for degenerative spinal diseases: How much balance can be obtained? Spine. 2014;39(26 Spec No):52–59. doi: 10.1097/BRS.0000000000000500. [DOI] [PubMed] [Google Scholar]
- 21.Buckland AJ, Vira S, Oren JH, et al. When is compensation for lumbar spinal stenosis a clinical sagittal plane deformity? Spine J. 2016;16(8):971–81. doi: 10.1016/j.spinee.2016.03.047. [DOI] [PubMed] [Google Scholar]
- 22.Cédric B, Pierre R, Gilles P, et al. Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J. 2011;5(5):626–33. doi: 10.1007/s00586-011-1930-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yamada K, Nakamae T, Shimbo T, et al. Targeted therapy for low back pain in elderly degenerative lumbar scoliosis: A cohort study. Spine. 2016;41(10):872–79. doi: 10.1097/BRS.0000000000001524. [DOI] [PubMed] [Google Scholar]
- 24.Houten JK, Nasser R. Symptomatic progression of degenerative scoliosis after decompression and limited fusion surgery for lumbar spinal stenosis. J Clin Neurosci. 2013;20(4):613–15. doi: 10.1016/j.jocn.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 25.Pinheiro-Franco JL, Roussouly P. The importance of sagittal balance for the treatment of lumbar degenerative disk disease. In: Pinheiro-Franco J, Vaccaro A, Benzel E, Mayer H, editors. Advanced concepts in lumbar degenerative disk disease. Springer; Berlin, Heidelberg: 2016. [Google Scholar]
- 26.Lin CWC, Qiang L, Williams CM, et al. The economic burden of guideline-recommended first line care for acute low back pain. Eur Spine J. 2016;27(1):109–16. doi: 10.1007/s00586-016-4781-0. [DOI] [PubMed] [Google Scholar]
- 27.Maki S, Aramomi M, Matsuura Y, et al. Paravertebral foramen screw fxation for posterior cervical spine fusion: Biomechanical study and description of a novel technique. J Neurosurg Spine. 2017;27(4):415–20. doi: 10.3171/2016.12.SPINE16803. [DOI] [PubMed] [Google Scholar]
- 28.Zhang XN, Sun XY, Meng XL, Yong H. Risk factors for medical complications after long-level internal fixation in the treatment of adult degenerative scoliosis. Int Orthop. 2018;42(9):2603–12. doi: 10.1007/s00264-018-3927-6. [DOI] [PubMed] [Google Scholar]
- 29.Pichelmann MA, Lenke LG, Bridwell KH, et al. Revision rates following primary adult spinal deformity surgery: Six hundred forty-three consecutive patients followed-up to twenty-two years postoperative. Spine. 2010;35(2):219–26. doi: 10.1097/BRS.0b013e3181c91180. [DOI] [PubMed] [Google Scholar]
- 30.Kim YJ, Bridwell KH, Lenke LG, et al. Is the T9, T11, or L1 the more reliable proximal level after adult lumbar or lumbosacral instrumented fusion to L5 or S1? Spine. 2007;32(24):2653–61. doi: 10.1097/BRS.0b013e31815a5a9d. [DOI] [PubMed] [Google Scholar]
- 31.Kim YJ, Bridwell KH, Lenke LG, et al. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: Prevalence and risk factor analysis of 144 cases. Spine. 2006;31(20):2329–36. doi: 10.1097/01.brs.0000238968.82799.d9. [DOI] [PubMed] [Google Scholar]
- 32.How NE, Street JT, Dvorak MF, et al. Pseudarthrosis in adult and pediatric spinal deformity surgery: A systematic review of the literature and meta-analysis of incidence, characteristics, and risk factors. Neurosurg Rev. 2018;319(2):319–36. doi: 10.1007/s10143-018-0951-3. [DOI] [PubMed] [Google Scholar]
- 33.Cho KJ, Suk SI, Park SR, et al. Selection of proximal fusion level for adult degenerative lumbar scoliosis. Eur Spine J. 2013;22(2):394–401. doi: 10.1007/s00586-012-2527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shufflebarger H, Suk SI, Mardjetko S. Debate: Determining the upper instrumented vertebra in the management of adult degenerative scoliosis: stopping at T10 versus L1. Spine. 2006;31(31):185–94. doi: 10.1097/01.brs.0000232811.08673.03. [DOI] [PubMed] [Google Scholar]
- 35.Kim HJ, Bridwell KH, Lenke LG, et al. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine. 2014;39(9):E576. doi: 10.1097/BRS.0000000000000246. [DOI] [PubMed] [Google Scholar]
- 36.Schwab F, Ungar B, Blondel B, et al. Scoliosis research society – Schwab adult spinal deformity classification: A validation study. Spine. 2012;37(12):1077–82. doi: 10.1097/BRS.0b013e31823e15e2. [DOI] [PubMed] [Google Scholar]
- 37.Shahidi B, Hubbard JC, Gibbons MC, et al. Lumbar multifidus muscle degenerates in individuals with chronic degenerative lumbar spine pathology. J Orthop Res. 2017;35(12):2700–6. doi: 10.1002/jor.23597. [DOI] [PMC free article] [PubMed] [Google Scholar]