Abstract
The COVID-19 pandemic has profoundly altered the daily lives of many people across the globe, both through the direct interpersonal cost of the disease, and the governmental restrictions imposed to mitigate its spread and impact. The UK has been particularly affected and has one of the highest mortality rates in Europe. In this paper, we examine the impact of COVID-19 on psychological health and well-being in the UK during a period of ‘lockdown’ (15th–21st May 2020) and the specific role of Psychological Flexibility as a potential mitigating process.
We observed clinically high levels of distress in our sample (N = 555). However, psychological flexibility was significantly and positively associated with greater wellbeing, and inversely related to anxiety, depression, and COVID-19-related distress. Avoidant coping behaviour was positively associated with all indices of distress and negatively associated with wellbeing, while engagement in approach coping only demonstrated weaker associations with outcomes of interest. No relationship between adherence to government guidelines and psychological flexibility was found.
In planned regression models, psychological flexibility demonstrated incremental predictive validity for all distress and wellbeing outcomes (over and above both demographic characteristics and COVID-19-specific coping responses). Furthermore, psychological flexibility and COVID-19 outcomes were only part-mediated by coping responses to COVID-19, supporting the position that psychological flexibility can be understood as an overarching response style that is distinct from established conceptualisations of coping. We conclude that psychological flexibility represents a promising candidate process for understanding and predicting how an individual may be affected by, and cope with, both the acute and longer-term challenges of the pandemic.
Keywords: COVID-19, Coronavirus, Psychological flexibility, Coping, Mental health, Wellbeing
Highlights
-
•
Our UK population sample report high levels of COVID-19 distress.
-
•
Psychological flexibility likely accounts for variance in wellbeing and distress.
-
•
Adherent social distancing was not related to psychological flexibility.
-
•
Psychological flexibility disposes adaptive COVID-19 coping responses.
-
•
Coping responses may part-mediate associations with psychological flexibility.
The COVID-19 pandemic has profoundly altered the daily lives of large swathes of the global population in ways that would have been perhaps unimaginable just months ago. With the virus having already claimed over 362,000 lives at the time of writing (May; Johns Hopkins University & Medicine, 2020), many national governments have imposed significant societal restrictions in an attempt to mitigate the spread and impact of the disease on their citizens and healthcare systems.
The UK has been particularly affected by the spread of COVID-19 and has one of the highest mortality rates in Europe (with over 38,500 reported deaths; Johns Hopkins University & Medicine, 2020). In March 2020, to reduce the exponential rate of COVID-19 infection, the UK government mandated that all UK citizens should leave their homes as infrequently as possible – termed ‘lockdown’ – and provided the police with new enforcement powers (fines) to encourage compliance (UK Government, 2020). Employees not designated as ‘critical workers’ were required to work from home if they could, others were furloughed or lost their jobs. Schools were closed for most students; shopping was for necessities only; and access to outside space was restricted to once per day for exercise. Family and social gatherings with others outside the home unit could no longer take place and conversations with loved ones living elsewhere became necessarily mediated by technology. Such rapid and significant change is largely unknown in the UK during modern peacetime. Table 1 provides an overview of UK restrictions across time.
Table 1.
UK COVID-19 restrictions.
| Date | Restriction summary |
|---|---|
| 23rd March – 12th May 2020 | Residents permitted to leave home:
All non-essential businesses closed (except food retailersa, hardware stores, and essential goods and services suppliers) All public gatherings of more than two people prohibited (except where the gathering consists of one household or for work purposes) |
| 13th May 2020 – ongoing (at time of study) | Residents permitted to leave home:
Some non-essential businesses allowed to open, but restaurantsb, cinemas, cafésb etc. remain closed. All public gatherings of more than two people prohibited (except where the gathering consists of one household or for work purposes) but some exceptions (e.g., funerals, house moves) and people also now able to meet with one person from another household at 2-m distance. |
Note: *Schools remain open where possible for children of critical workers and children considered vulnerable only.
Restaurants and café’s able to provide delivery only.
Restaurants and cafés able to provide delivery or physically distanced service (e.g., drive-thru; take-out).
The impact of these changes on the psychological health and wellbeing of the population is significant. Data from the UK Office of National Statistics (ONS) suggests that around 72% of people in the UK are currently worried about the effect of COVID-19 on their life, with many reporting high levels of anxiety (32%), diminished well-being (43%), and loneliness (23%) (ONS: 2020). These elevated distress indices (anxiety prevalence amongst the UK population is usually around 6%; McManus, Meltzer, Brugha, Bebbington, & Jenkins, 2009) cohere with findings from elsewhere. In a recent study from China, for example, half of respondents rated the psychological impact of COVID-19 as moderate to severe, and approximately one-third reported moderate to severe levels of anxiety during the first two weeks of the pandemic (Wang et al., 2020). Comparable reports have emerged from Italy, Spain, and other deeply affected countries (e.g., González-Sanguino et al., 2020; Odriozola-González, Planchuelo-Gómez, Irurtia-Muñiz, & de Luis-García, 2020; Orgilés, Morales, Delvecchio, Mazzeschi, & Espada, 2020; Ozamiz-Etxebarria, Dosil-Santamaria, Picaza-Gorrochategui, & Idoiaga-Mondragon, 2020; also see Rajkumar, 2020, for an early review).
Studies that have tracked the long-term sequelae of previous coronavirus pandemics (such as Severe Acute Respiratory Syndrome [SARS] in 2002) suggest that psychological difficulties – including PTSD, depression, anxiety, stress, and impaired quality of life – can sustain for months and even years post-outbreak, particularly for those who contract the virus or who are directly exposed to it through their occupational roles (e.g., Bonanno et al., 2008; Chan & Huak, 2004; Hui et al., 2005; Kwek et al., 2006; A. M.; Lee et al., 2007; Liu et al., 2012; Maunder et al., 2006; Wu, Chan, & Ma, 2005). There is additional evidence to suggest that the measures enforced to mitigate virus spread (such as quarantine and social isolation) can also contribute to lasting psychological distress, including elevated levels of depression, stress, irritability, and PTSD-type symptoms (see Brooks et al., 2020 for a review).
Identifying the psychological processes that can help to protect well-being and psychological health under such exceptional circumstances is therefore of utmost importance. Understanding these processes has implications for how individuals might be helped to manage the current pandemic, but also how we might best intervene in the coming months to prevent nascent psychological difficulties from developing into serious long-term mental health conditions. Understanding alone, however, is insufficient; these processes also need to be malleable and responsive to psychological intervention if they are to have functional utility (e.g., Holmes et al., 2020).
Psychological flexibility, the ability to recognise and adapt to situational demands in pursuit of personally meaningful longer-term outcomes, is one such process. Across a broad range of populations and presentations, greater psychological flexibility has consistently been associated with reduced stress, anxiety, depression, and increased well-being (e.g., Bluett, Homan, Morrison, Levin, & Twohig, 2014; Francis, Dawson, & Golijani-Moghaddam, 2016; Gloster; Klotsche; Chaker, Hummel, & Hoyer, 2011; Kashdan; Rottenberg, 2010; Masuda & Tully, 2012; McCracken & Morley, 2014; Tyndall et al., 2020). Conversely, psychological inflexibility, particularly in the form of experiential avoidance (an excessive tendency to avoid difficult experiences, thoughts, feelings, and situations; S. C. Hayes, Wilson, Gifford, Follette, & Strosahl, 1996), and/or a propensity to engage rigid and inflexible psychological, emotional, or behavioural strategies, has been found to relate to poorer coping and impaired psychological and emotional health across an array of psychological literature (e.g., Bardeen, Fergus, & Orcutt, 2013; Bonanno, Papa, Lalande; Westphal, & Coifman, 2004; Chawla; Ostafin, 2007; Cheng, 2001; Karekla; Panayiotou, 2011; Kashdan, Barrios, Forsyth, & Steger, 2006; Kashdan; Rottenberg, 2010; Nielsen, Sayal, & Townsend, 2016). Moreover, of particular pertinence to the current context, it has been found that psychological flexibility can buffer the adverse impact of recent life stressors on psychological health and wellbeing (Fonseca, Trindade, Mendes, & Ferreira, 2020; Gloster, Meyer, & Lieb, 2017).
An individual's level of psychological flexibility appears related to, but distinct from, their particular ways of coping. While psychological inflexibility (in the form of experiential avoidance) strongly relates to a tendency to deploy avoidant coping strategies, such as distraction, disengagement, or substance use, which can become dysfunctional, it has also been found to account for a greater proportion of psychological distress outcomes over and above a person's typical coping-style alone (e.g., Karekla; Panayiotou, 2011; Nielsen et al., 2016). This distinction is important as it implies that psychological flexibility (or lack thereof), rather than a specific coping style or proclivity, is likely to be more important for understanding (and influencing) how people successfully navigate the impact of the pandemic now and in the future (e.g., Cheng, 2001; Karekla; Panayiotou, 2011; Kashdan; Rottenberg, 2010; Nielsen et al., 2016). Conceptually, psychological flexibility can be understood as a generalised or higher-order ability to respond effectively to situational demands in the pursuit of longer-term goals, enabling selection of coping responses as apt to the situation. Thus, psychological flexibility may partly affect outcomes via its influence on selection of coping behaviours (including, but not limited to, facilitation of more open/less avoidant ways of responding). This notion has been supported by mediational modelling demonstrating indirect effects of psychological flexibility on wellbeing and distress outcomes, via coping strategies (Rueda & Valls, 2020). Notably, Rueda and Valls (2020) found direct effects of psychological flexibility in addition to indirect (mediated) effects: These direct effects may reflect unique aspects of psychological flexibility as a functional-contextual process (adapting responding according to situational demands/affordances and desired consequences) which may not be captured by traditional measures of coping.
Psychological flexibility is also the key process targeted by Acceptance and Commitment Therapy (ACT; S. C. Hayes, Strosahl, & Wilson, 2009) – the empirically established third-wave cognitive-behaviour therapy with demonstrated efficacy for improving psychological health and wellbeing outcomes across a multitude of clinical and non-clinical populations and presentations (e.g., Bluett et al., 2014; Brown, Glendenning, Hoon, & John, 2016; Hacker, Stone, & MacBeth, 2016; E. B.; Lee, An, Levin, & Twohig, 2015; Powers, Vörding, & Emmelkamp, 2009; Veehof; Oskam; Schreurs, & Bohlmeijer, 2011). Psychological flexibility thus represents a promising candidate process for both understanding and predicting how an individual may be affected by, and cope with, the significant challenges of the pandemic, while also offering a potential intervention target should theorised functional relationships be confirmed.
The aims of this study were to (1) provide a rapid snapshot of how psychological flexibility interacts with coping, psychological health, well-being, and government restriction-adherence during the COVID-19 pandemic in the UK1 ; and (2) investigate psychological flexibility – as conceptualised within ACT – as an overarching response style that may lead to improved psychological outcomes by facilitating flexible (rather than restrictive or stereotyped) coping behaviour during this period of acute global uncertainty.
1. Method
1.1. Participants
Participants were 555 adults living in the UK (72% female, M age = 39.2; Table 2 provides detailed sample characteristics), recruited to an online questionnaire-based study via snowball sampling and advertising on UK-directed forums (reddit), social media (Facebook and Twitter), and a research-recruitment site (callforparticipants.com). Participants were required to confirm that they were 18 years or over, were currently residing in the UK (England, Scotland Wales, or Northern Ireland), and consented to take part. No other inclusion or exclusion criteria were applied.
Table 2.
Characteristics of the sample.
| Characteristic | n | (%) |
|---|---|---|
| Age: Mean 39.2 (SD 13.2; range 18–76) | ||
| Gender | ||
| Female | 397 | 72 |
| Male | 143 | 26 |
| Not disclosed | 9 | 2 |
| Non-binary/third gender | 6 | 1 |
| Ethnic group | ||
| White | 510 | 92 |
| Mixed Ethnicity | 15 | 3 |
| Not disclosed | 14 | 3 |
| Asian or Asian British | 9 | 2 |
| Black or Black British | 4 | 1 |
| Other | 3 | 1 |
| Current work status | ||
| Working from home | 237 | 43 |
| Unemployed | 113 | 20 |
| Working outside home – key worker | 104 | 19 |
| Furloughed | 81 | 15 |
| Working outside home – not key worker | 13 | 2 |
| Not disclosed | 7 | 1 |
| Current living arrangementsa | ||
| With partner | 310 | 56 |
| With child | 147 | 27 |
| Alone | 93 | 17 |
| With parents | 68 | 12 |
| Other (friends, housemates, or relatives) | 56 | 10 |
| COVID-19 status | ||
| Not suspected or confirmed (e.g., no symptoms and/or negative test) | 450 | 81 |
| Suspected or confirmed (e.g., symptoms and/or positive test) | 98 | 18 |
| Not disclosed | 7 | 1 |
| COVID-19 worry | ||
| Not at all worried | 30 | 5 |
| Somewhat unworried | 80 | 15 |
| Neither worried nor unworried | 63 | 11 |
| Very or somewhat worried | 375 | 68 |
| Not disclosed | 7 | 1 |
Some categories not mutually exclusive.
Of 714 individuals who accessed the survey, 684 consented to participation and 610 provided basic demographic data. Of these, 555 completed all measures and formed the final study sample. Completers were compared to non-completers on available data (using t-tests or Fisher's exact tests as apt) – the only significant difference was in age (t [607] = −2.07, p = .039) with non-completers being younger (M = 35.5, SD = 13.4) than completers (M = 39.2, SD = 13.2) on average.
To be able to compare our sample to the wider UK population at this extraordinary time, we asked our participants a question that was being used in contemporaneous weekly representative polling of the UK general population (ONS, 2020): “How worried or unworried are you about the effect that Coronavirus (COVID-19) is having on your life right now?” Our sample (with 68% reporting that they are very or somewhat worried about COVID-19) appear similar to the broader UK population; the proportion of UK adults very or somewhat worried about the effect of COVID-19 on their life ranged from 72.4% to 66.7% during the study data collection period (ONS, 2020).
We aimed to recruit a minimum sample-size of 252, to obtain stable estimates of sample correlation coefficients (converging on population values; Schönbrodt & Perugini, 2013). Our analysis plan is predicated on multiple correlational analyses and ensuring the stability of estimated coefficients provides foundational confidence for contingent modelling. Specifically, we powered our study to achieve a corridor of stability of ±0.10 for any coefficients ≥ .102 (i.e., any associations of greater than negligible magnitude; Cohen, 1992) enabling (80%) confidence that our estimated coefficients would be within ±0.10 of the true population value (i.e., only fluctuations of small magnitude would be tolerated).
2. Measures
To maximise domain coverage while minimising participant burden, we utilised short-form versions of established measures where possible. In addition to the measures outlined below, demographic information including age, gender, ethnicity, and current living and working arrangements was also collected.
The CompACT-8 (Morris, Golijani-Moghaddam, & Dawson, 2019) is an 8-item abbreviated version of the Comprehensive Assessment of Acceptance and Commitment Therapy Processes (CompACT; Francis et al., 2016) and measures psychological flexibility as conceptualised within ACT. The CompACT-8 (formerly termed CompACT-SF [short-form]) retains the same three-factor structure as the original measure, providing indices of ‘openness to experience’, ‘valued action’, and ‘behavioural awareness’ (key dyadic processes of psychological flexibility as conceptualised within ACT; Francis et al., 2016; S. C. Hayes, Villatte, Levin, & Hildebrandt, 2011), and an overall summed psychological flexibility score (which forms the focus of analyses in the present study). Items are scored on a 7-point Likert scale, ranging from 0 = “strongly disagree” to 6 = “strongly agree”; total scores range from 0 to 48, with higher scores indicating greater psychological flexibility. The scale has been validated in an independent community sample (N = 571), has acceptable internal reliability (psychological flexibility α = 0.73), and good convergent and divergent validity with measures of wellbeing, experiential avoidance, and distress, respectively.
The Short Warwick-Edinburgh Mental Well-Being Scale (SWEMWBS; Stewart-Brown et al., 2009) is a seven-item measure frequently used to assesses the emotional, cognitive, functional, and social components of mental wellbeing. Items are rated on a five-point scale (1 = “none of the time” to 5 = “all of the time”), with a higher total score (range 7–35) indicating greater mental wellbeing. The measure is frequently used in epidemiological studies, has been normed on a large, nationally representative sample in England (UK), and has good internal reliability (α = 0.84) and external criterion validity (Fat, Scholes, Boniface, Mindell, & Stewart-Brown, 2017).
The Patient Health Questionnaire-9 (PHQ-9) is a 9-item self-report measure assessing symptoms of depressed mood (Kroenke, Spitzer, & Williams, 2001). Frequency of symptoms is assessed on a 4-point scale, ranging from 0 = “not at all” to 3 = “nearly every day”; the summed score ranges from 0 to 27, with higher scores indicating greater severity. In the current study, respondents were asked to report symptom frequency over the last week. The PHQ-9 performs as well as clinician-administered assessments for detecting depression in primary care (Gilbody, Richards, & Barkham, 2007) and has been found to be valid for assessing depression severity in research and practice (Kroenke et al., 2001). Scores ≥10 indicate clinical levels of depression (Levis, Benedetti, & Thombs, 2019).
The Generalised Anxiety Disorder Scale-7 (GAD-7) is a 7-item self-report measure assessing symptoms of generalised anxiety (Spitzer, Kroenke, Williams, & Löwe, 2006). Frequency of symptoms is assessed on a 4-point scale, ranging from 0 = “not at all” to 3 = “nearly every day”; the summed score ranges from 0 to 21, with higher scores indicating greater severity. In the current study, respondents were asked to report frequency over the last week. The GAD-7 has been found to be valid for detecting generalised anxiety in primary care settings (scores ≥10 indicate clinical levels of anxiety) and for assessing severity in research and practice (Löwe et al., 2008, Spitzer et al., 2006).
The Impact of Event Scale-6 (IES-6; Thoresen et al., 2010) is a 6-item abbreviated version of the Impact of Event Scale-Revised (IES-R; Weiss, 2007, pp. 219–238) and measures the principal components of PTSD (intrusion, avoidance, and hyperarousal; Giorgi et al., 2015). Items are rated on a 5-point scale, ranging from 0 = “not at all” to 4 = “extremely”; the summed score ranges from 0 to 24, with higher scores indicating greater PTSD symptomology. In the current study, respondents were asked to complete the measure in relation to the COVID-19 pandemic and its impact on them during the previous week. The scale has good internal consistency (α = 0.80), and good construct and convergent validity with the IES-R (Giorgi et al., 2015; Thoresen et al., 2010).
The Brief COPE (Carver, 1997) is a 28-item self-report measure of coping styles in response to a stressful experience. Different coping responses are rated on a 4-point scale, ranging from 1 = “I haven't been doing this at all” to 4 = “I've been doing this a lot”. Instructions were adapted to focus on coping in the context of COVID-19 (“Please indicate how much you have engaged in the following during the past week in relation to the COVID-19 pandemic”). Factor analysis indicates that the various coping styles reflect two core factors (Eisenberg, Shen, Schwarz, & Mallon, 2012): (1) avoidant coping (comprising self-distraction, denial, substance use, behavioural disengagement, venting, and self-blaming); and (2) approach coping (comprising active coping, use of emotional and instrumental support, positive reframing, planning, and [passive, resigned] acceptance [distinct from the active, willing acceptance underpinning psychological flexibility]). In the current study, the Brief COPE was scored accordingly, deriving summary scores for both avoidant and approach coping, with higher scores reflecting greater use of the respective class of coping responses. The Brief COPE has been used to assess coping amongst a community sample following the SARS pandemic (Sim, Chan, Chong, Chua, & Soon, 2010) and has adequate validity and reliability (Carver, 1997).
We asked participants additional questions related to COVID-19. To gauge worry about the personal impact of COVID-19, we asked participants: “How worried or unworried are you about the effect that Coronavirus (COVID-19) is having on your life right now?” (ONC, 2020). Participants respond on a 5-point scale ranging from “not at all worried” to “very worried”. We also asked respondents to confirm their COVID-19 status (e.g., whether they have been tested or confirmed to have contracted the virus). Finally, participants were presented with an outline of current government restrictions (tailored according to location within the UK) and asked how closely they were adhering to the guidance, ranging from: “Not closely (I don't follow the above)” to “Very closely (I follow all of the above at all times)”.
3. Procedure
Institutional ethical approval was obtained for all aspects of the study. Potential participants were directed to study information via a weblink; those who wished to take part (after being reminded about their right to withdraw) were required to confirm that they met eligibility criteria and consented to take part. Participants then proceeded to complete the above-described measures online. We used the survey platform Qualtrics for study hosting and data collection. All data collection for the current report took place between 15th–21st May 2020 (see Table 1 for an overview of restrictions in place at the time of data collection).
4. Data analyses
Preliminary analyses allowed for data exploration and assumption-checking, using IBM SPSS Statistics (version 25). Assumptions were met for all parametric tests conducted. Correlational analyses (Pearson's r) were carried out to examine any zero-order relations among psychological flexibility, COVID-19 coping behaviours, and focal outcome variables. To correct for multiple testing of focal relations, we applied a Benjamini-Hochberg adjustment to p-values using a false discovery rate of 0.05. We additionally tested whether predictor and outcome variables of interest were associated with demographic characteristics (applying ANOVAs for nominal demographic variables and correlational analyses for continuous or binary variables) to inform selection of control variables for subsequent regression analyses. To more inclusively identify potential control variables, these exploratory analyses were not adjusted for multiple testing.
Research aims were met using hierarchical multiple regression analyses. Five models were run, one for each outcome/dependent variable of interest: (1) wellbeing (SWEMWBS); (2) depression (PHQ-9); (3) anxiety (GAD-7) (4) event-specific (i.e., COVID-19); distress (IES-6); (5) COVID-19 worry; and (6) adherence (to applicable government guidance on social distancing). Psychological flexibility (CompACT-8) and COVID-19 coping behaviours (avoidance and approach coping; Brief COPE) were included as a priori predictors of interest in all regression models. We controlled for any demographic variables (e.g., gender, age, and work status) demonstrating significant associations with one or more of the identified predictor and outcome variables of interest; control variable selection was thus data-driven, based on preliminary analyses of association (described above). Variables were entered into the model in three blocks: Block one entered control demographic variables; block two entered the Brief COPE scales (avoidance and approach coping behaviours); and block three entered the CompACT-8. This allowed R2 change scores to be calculated for the incremental contribution of psychological flexibility (CompACT-8) to each model. In consideration of multiple testing and likely error inflation (across 6 regression models) we first applied an omnibus multivariate test (of whether regression coefficients equal zero across all dependent variables) and only proceeded to examine separate models (for each dependent variable) if this F test was significant (Dattalo, 2013).
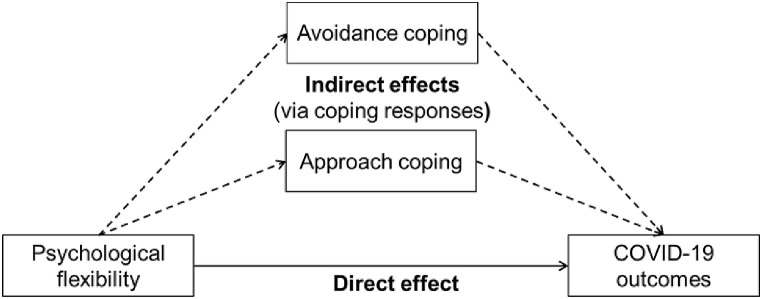
To examine whether relationships between psychological flexibility and COVID-19 outcomes could be accounted for in terms of COVID-19-specific coping responses (i.e., engagement in avoidance and/or approach behaviours) we conducted mediational analyses using the PROCESS macro (A. F. Hayes, 2017). Applying Model 4 (parallel multiple mediation), robust standard errors and 99% percentile confidence intervals (chosen to conservatively account for multiple testing and likely error inflation) were computed for all parameters, based on 5000 bootstrap samples. General psychological flexibility (as measured by the CompACT-8) is logically operating prior to the deployment of context-specific (COVID-19) coping responses (as measured by the Brief COPE) and outcomes. Based on this, and theory outlined in the background, we posited and tested the general mediational model depicted in Fig. 1 – mirroring mediation modelling applied by Rueda and Valls (2020).
Fig. 1.
General mediation model depicting putative and testable pathways between psychological flexibility and COVID-19 outcomes.
5. Results
5.1. Distress in the COVID-19 context
At the time of responding, 206 participants (37%) met criterion for clinical depression and 145 (27%) met criterion for clinical anxiety (scores ≥10 on the PHQ-9 and GAD-7 respectively); overall, 41% of participants met criteria for anxiety and/or depression, with 22% meeting criteria for both. These findings reflect broader UK trends, with 32–33% of the population reporting high levels of anxiety in ONS surveys over the study period (ONS, 2020).
5.2. Correlational analyses
Table 3 presents correlations among the focal (predictor and outcome) variables, descriptive statistics, and internal consistency (Cronbach's ɑ) coefficients. All statistically significant inter-correlations between a priori focal variables of interest survived correction for multiple testing (Benjamini-Hochberg adjustment to preserve a 5% false discovery rate among 36 correlations). Table 3 additionally presents demographic variables that were found, in unadjusted exploratory analysis, to be significantly associated with one or more focal variables.
Table 3.
Pearson product–moment correlations, descriptive statistics, and ɑ coefficients (N = 555).
| Focal variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Measure | Range | Mean | SD | ɑ |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Psychological flexibility (1) | -.52** | .10* | .68** | -.60** | -.63** | -.51** | -.35** | .07 | CompACT-8 | 4–48 | 27.42 | 7.89 | .77 | |
| Avoidance coping (2) | .24** | -.48** | .55** | .61** | .61** | .37** | -.10* | Brief COPE | 12–48 | 21.91 | 5.58 | .76 | ||
| Approach coping (3) | .15** | .02 | -.08 | .17** | .12** | .05 | Brief COPE | 12–46 | 28.89 | 6.16 | .81 | |||
| Wellbeing (4) | -.67** | -.68** | -.52** | -.47** | .07 | SWEMWBS | 7–35 | 20.21 | 3.97 | .87 | ||||
| Anxiety (5) | .75** | .70** | .47** | -.02 | GAD-7 | 0–21 | 6.79 | 5.75 | .92 | |||||
| Depression (6) | .56** | .35** | -.06 | PHQ-9 | 0–27 | 8.74 | 6.71 | .90 | ||||||
| COVID-19 distress (7) | .51** | -.00 | IES-6 | 0–24 | 8.22 | 5.60 | .86 | |||||||
| COVID-19 worry (8) | -.02 | 0–4 | 2.61 | 1.10 | ||||||||||
| Adherence (9) |
0–3 |
2.60 |
0.56 |
|||||||||||
| Demographic correlates | ||||||||||||||
| Age | .34** | -.32** | .03 | .33** | -.31** | -.36** | -.21** | -.09* | .02 | |||||
| Male | .10* | -.10* | -.14** | .04 | -.10* | -.07 | -.13** | -.09* | -.01 | |||||
| L w/partner | .17** | -.14** | .02 | .19** | -.14** | -.22** | -.08* | -.02 | .09* | |||||
| L w/child | .06 | -.10* | .01 | .10* | -.05 | -.12** | -.09* | -.04 | .05 | |||||
| L w/parents | -.13** | .12** | -.03 | -.14** | .16** | .18** | .18** | .06 | .06 | |||||
Note. SWEMWBS = Short Warwick-Edinburgh Mental Well-Being Scale. GAD-7 = Generalised Anxiety Disorder Scale-7. PHQ-9 = Personal Health Questionnaire-9. IES-6 = Impact of Event Scale-6. L w/ = Living with. Male is coded such that male = 1 and other genders = 0. L w/variables are coded such that 1 = yes and 0 = no. ɑ = Cronbach's alpha (internal consistency in the present sample). *p < .05, **p < .01.
As expected, psychological flexibility was significantly and positively associated with wellbeing; negative relationships were found between psychological flexibility and distress (anxiety, depression, and COVID-19-related distress and worry). Psychological flexibility was not associated with adherence to government social distancing guidance.
Engaging in avoidant coping behaviours was positively associated with all indices of distress and negatively associated with wellbeing. Moreover, avoidance coping was inversely associated with adherence to current social distancing guidance – albeit that this association (whilst statistically significant) was of small magnitude. Engagement in approach coping demonstrated weaker associations with outcomes of interest. The only significant relationships were with wellbeing, COVID-19 distress, and COVID-19 worry; all were positive and of small magnitude (suggesting that approach coping had both adaptive and maladaptive functions).
In terms of inter-relationships between psychological flexibility and COVID-19 coping behaviours, psychological flexibility demonstrated a large, inverse relationship with avoidant responses to COVID-19 – and a small, positive relationship with approach coping behaviours (including use of external supports).
When examining the focal predictor and outcome variables in relation to sample demographic characteristics, there were no significant associations with work status or ethnic group (ps = .09 - 0.98). However, predictor and outcome variables varied by age, gender (specifically, male versus other gender identities), and living arrangements (specifically, living with a partner, a child, or with parents versus other arrangements). Consequently, consistent with planned analyses, these demographic variables were entered as control variables in subsequent regression models (and relevant relationships to outcome are reported therein).
5.3. Regression analyses
Hierarchical regression results are displayed in Table 4 . The multivariate multiple regression omnibus test was significant (Pillai's Trace, F = 12.31, p < .001), permitting progression to examine regression models for each outcome. The addition of psychological flexibility (CompACT-8, in block three) produced statistically significant increases in R 2 for five of the six outcome models. In these five models, psychological flexibility explained an additional 5–18% of outcome variance – over and above demographic characteristics and COVID-19-specific coping responses (as measured by the Brief COPE). Whilst associations generally (inversely) paralleled those observed for avoidant coping, psychological flexibility accounted for unique variance in both distress and wellbeing – including COVID-19-specific distress (IES-6) and worry. Based on absolute values of standardised coefficients, psychological flexibility demonstrated a particularly strong relationship with wellbeing in the context of lockdown (other significant associations were of moderate magnitude).
Table 4.
Three-block hierarchical multiple regression results for focal outcome variables.
| Outcome |
Wellbeing |
Anxiety |
Depression |
COVID-19 distress |
COVID-19 worry |
Adherence |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Block | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 |
| Age | .31** | .16** | .07* | -.28** | -.12** | -.05 | -.33** | -.15** | -.09** | -.16** | .01 | .06 | -.07 | .04 | .08 | .04 | .01 | .01 |
| Male | .05 | .02 | -.02 | -.10* | -.05 | -.02 | -.08* | -.04 | -.01 | -.15** | -.08* | -.05 | -.09* | -.04 | -.03 | -.01 | -.01 | -.00 |
| L w/partner | .12** | .09* | .05 | -.06 | -.03 | .00 | -.13** | -.09** | -.07* | .01 | .04 | .06 | .02 | .04 | .06 | .11 | .11* | .11* |
| L w/child | .07 | .03 | .03 | -.03 | .02 | .02 | -.09* | -.04 | -.04 | -.09* | -.04 | -.04 | -.05 | -.01 | -.01 | .05 | .04 | .04 |
| L w/parents | .03 | .02 | .01 | .04 | .05 | .06 | .01 | .02 | .03 | .11* | .12** | .13** | .03 | .03 | .04 | .13 | .13 | .13* |
| Avoidant | -.48** | -.22** | .52** | .31** | .59** | .41** | .58** | .42** | .36** | .23** | -.11* | -.12* | ||||||
| Approach | .27** | .15** | -.11** | -.02 | -.22** | -.14** | .01 | .08* | .02 | .08 | .07 | .08 | ||||||
| PF | .53** | -.42** | -.36** | -.30** | -.26** | -.01 | ||||||||||||
| R2 | .13 | .34 | .52 | .11 | .34 | .45 | .17 | .46 | .55 | .08 | .37 | .43 | .02 | .14 | .18 | .02 | .03 | .03 |
| R2 change | .13** | .21** | .18** | .11** | .23** | .11** | .17** | .30** | .09** | .08** | .29** | .06** | .02 | .12** | .05** | .02* | .01* | .00 |
Note. Standardised beta coefficients are reported for comparability. PF = Psychological flexibility (CompACT-8). L w/ = Living with. Avoidant = Avoidant coping (Brief COPE). Approach = Approach coping (Brief COPE). Male is coded such that male = 1 and other genders = 0. L w/variables are coded such that 1 = yes and 0 = no. *p < .05, **p < .01.
Avoidant coping was an independent predictor of outcome in all final models (with all variables entered); avoidant responses to the COVID-19 context were associated with poorer wellbeing and distress outcomes – and lower restriction adherence – consistent with correlational results. Unique associations were of small-to-moderate magnitude. Approach coping demonstrated small unique associations with depression, wellbeing, and COVID-19 distress.
Some of the unique outcome variance in final models was explained by demographic characteristics (although all coefficients were of small magnitude). Specifically, age remained positively associated with wellbeing and negatively associated with depression; living with a partner was negatively associated with depression and positively associated with restriction adherence; and living with parents was positively associated with both COVID-19 distress (IES-6) and adherence. Living with others (a partner and/or parents) therefore appeared to support adherence to restrictions.
5.4. Mediation analyses
As outlined above, mediation analyses were conducted to determine whether relationships between psychological flexibility and COVID-19 outcomes were (to some extent) mediated by coping responses to COVID-19. Table 5 illustrates that, for all outcomes except adherence, there were significant indirect effects (of small magnitude) alongside significant direct effects (of moderate-to-large magnitude) for psychological flexibility. Thus, consistent with regression analyses, psychological flexibility retained direct (unique) relationships with outcomes of interest when modelled alongside coping responses. However, these models also extend the regression analyses by clearly outlining (theory- and logic-based) indirect pathways to outcome via coping responses to COVID-19; specifically, through a lower propensity to respond avoidantly. With respect to adherent social distancing, mediation modelling demonstrated no significant direct or indirect effect of psychological flexibility.
Table 5.
Mediation models of pathways between psychological flexibility and COVID-19 outcomes – including indirect pathways via coping responses to COVID-19.
| DV | Wellbeing |
Anxiety |
Depression |
COVID-19 distress |
COVID-19 worry |
Adherence |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p value | p value | p value | p value | p value | p value | |||||||
| PF → Avoidant | -.51* | <.001 | -.51* | <.001 | -.51* | <.001 | -.51* | <.001 | -.51* | <.001 | -.51* | <.001 |
| PF → Approach | .10 | .022 | .10 | .022 | .10 | .022 | .10 | .022 | .10 | .022 | .10 | .022 |
| PF → DV | .55* | <.001 | -.43* | <.001 | -.38* | <.001 | -.30* | <.001 | -.25* | <.001 | .00 | .987 |
| Avoidant → DV | -.24* | <.001 | .33* | <.001 | .46* | <.001 | .42* | <.001 | .21* | <.001 | -.11 | .033 |
| Approach → DV | .16* | <.001 | -.02 | .654 | -.15* | <.001 | .08 | .024 | .08 | .035 | .07 | .108 |
| Total PF effect | .686* | <.001 | -.604* | <.001 | -.628* | <.001 | -.509* | <.001 | -.351* | <.001 | .066 | .123 |
| Direct PF effect |
.548* |
<.001 |
-.432* |
<.001 |
-.381* |
<.001 |
-.299* |
<.001 |
-.251* |
<.001 |
.001 |
.987 |
| 99% CI |
99% CI |
99% CI |
99% CI |
99% CI |
99% CI |
|||||||
| Indirect PF effect | .138* | [.084,.192] | -.172* | [-.249,-.104] | -.247* | [-.307.-.185] | -.210* | [-.289,-.135] | -.101* | [-.178,-.023] | .065 | [-.015,.141] |
| via Avoidant | .123* | [.071,.177] | -.170* | [-.245,-.106] | -.233* | [-.293,-.170] | -.217* | [-.292,-.148] | -.109* | [-.180,-.037] | .058 | [-.017,.129] |
| via Approach | .015 | [-.004,.040] | -.002 | [-.015,.009] | -.015 | [-.036,.003] | .008 | [-.002,.028] | .009 | [-.003,.029] | .007 | [-.005,.027] |
Note. Standardised beta coefficients are reported for comparability. DV = Dependent Variable in each outcome model. PF = Psychological flexibility (CompACT-8). Avoidant = Avoidant coping (Brief COPE). Approach = Approach coping (Brief COPE). *p < .01 (adjusted significance level applied to mediational analyses). Indirect effect-sizes are significant when 99% CIs do not include 0.
6. Discussion
In this study, we examined psychological flexibility in the proximal UK context of the COVID-19 pandemic. Specifically, we assessed how psychological flexibility relates to psychological health and wellbeing outcomes within this context – and whether individual differences in psychological flexibility account for differences in coping behaviours and adherence to government restrictions. Moreover, we explored a potential mediational model of psychological flexibility as an overarching ability that may facilitate improved outcomes via more adaptive use of coping strategies.
The elevated prevalence of clinical distress in our general population sample (e.g., 27% meeting criterion for generalised anxiety – versus typical estimates of 6%; McManus et al., 2009) evinces the detrimental psychological impact of the pandemic and highlights the importance of identifying (malleable) factors that may contribute to outcomes in this context.
Results showed that, barring restriction adherence, psychological flexibility was directly related to all focal outcomes of interest – demonstrating a positive relationship with wellbeing and negative relationships with distress (depression, anxiety, and COVID-19 distress and worry). These relationships were somewhat unique, providing incremental explanatory power over and above the contributions of demographic and coping-style variables. Thus, generalised psychological flexibility (as measured by the deceptively brief but theoretically coherent CompACT-8) accounted for meaningful situational outcomes in the context of the COVID-19 pandemic. The valence and relative magnitude of these associations (e.g., the fact that the strongest [positive] relationship was with wellbeing) were congruent with theoretical expectations, and consistent with the strong body of evidence highlighting the critical role of psychological flexibility in facilitating psychological health and adjustment (Kashdan & Rottenberg, 2010). Thus, although the current study was cross-sectional, and unable to determine the directionality of associations, observations are compatible with broader theoretical assumptions and empirical evidence. The unique contribution of this study is in the situational specificity of our assessments of coping behaviours and outcomes, allowing us to make contextualised inferences about responses to the pandemic in particular, versus in participants’ lives more broadly. Examining focal variables at this time of acute stress arguably provides a more critical test of the relevance of psychological flexibility than when assessing in a global way under general conditions.
Psychological flexibility demonstrated substantive associations with coping variables (a large negative association with avoidant coping and a small positive association with approach coping) and mediational analyses identified significant indirect pathways to outcomes of interest through reduced avoidance. Where identified, for distress and wellbeing outcomes, these indirect pathways were present alongside significant direct effects. This finding of both unique and mediated effects of psychological flexibility is consistent with previous work demonstrating that psychological flexibility is independent of, but overlapping with, coping response (Karekla & Panayiotou, 2011). Our findings also mirror mediational analyses by Rueda and Valls (2020), who demonstrated indirect effects of psychological inflexibility on distress and wellbeing via coping strategies – with psychological inflexibility disposing greater use of avoidant coping strategies and poorer outcomes. So, although psychological flexibility is related to coping, it does not appear to be a form of coping.
Psychological flexibility is partly defined as an ability to respond effectively to situational demands in the pursuit of longer-term goals and can thus be conceptualised as a higher-order response style (e.g., Nielsen et al., 2016) that may facilitate the selection of coping responses (and other behaviours) as apt to the situation. Accordingly, while effective action might be harder to take when we are driven primarily by efforts to avoid unwanted experiences, psychological flexibility is not simply the inverse of avoidant coping. Effective, situational responding requires an extensive repertoire of behaviours, including avoidance behaviours, which can be functional and adaptive in various contexts (e.g., taking breaks from emotionally burdensome COVID-19 news stories may improve short-term wellbeing without any significant longer-term cost). Complete eschewal of avoidance strategies is a further manifestation of inflexibility. The ability to respond successfully is therefore dynamic and situated, requiring an openness (to experience difficult situations without habitually deploying avoidance strategies) and an awareness (sensitivity to context) that discriminates when behaviour change may be necessary to achieve a valued outcome. This coheres with theoretical and empirical coping literature that highlights the need to gauge overarching coping flexibility (capacity to select from a broad repertoire of coping strategies as apt to each situation), and the observation made by others that traditional coping measures are limited in their sensitivity to such flexibility (Zimmer-Gembeck et al., 2018).
It is notable that the magnitude of association between psychological flexibility and avoidant coping was greater in the current study than has been identified in previous studies. We observed a large zero-order association (−0.52) whereas previous studies have reported small-to-moderate associations (with comparable rs ranging from −0.25 to −0.34) across both community and clinical samples (Hulbert-Williams, Storey & Wilson, 2015; Karekla & Panayiotou, 2011; Kashdan et al., 2006). This contrast may reflect differences in study measures or populations but may also reflect something more particular about the current context. We directed participants to focus on coping behaviours used specifically in relation to the COVID-19 pandemic. Thus, the observed strength of association here may reflect a contextual strengthening of the inverse relationship; where, under the unfamiliar and challenging conditions of lockdown, those lacking in flexibility are tending towards more extensive avoidance. The isolative and restrictive pandemic context may mean that many individuals are unable to successfully draw on their usual repertoire of responses/ways of coping and default to behaviours that attenuate stress in the short-term; those with greater psychological flexibility may be relatively able to adapt and orient to alternative, personally-effective ways of responding. It is also possible that the strengthened association arises from the more situated assessment of coping used in the current study, which may have helped to delineate individual differences that are less apparent in global assessments. However, we would generally expect stronger correlations in studies where both measures of psychological flexibility and coping are at the same global/trait-like level (Hudson, Anusic, Lucas, & Donnellan, 2020).
There are important limitations that must be considered when interpreting the findings of this study. Our ability to draw robust conclusions about directionality was restricted by the cross-sectional, correlational nature of the data. When constructing and testing mediational models of indirect effects, we have relied on logical and theoretical bases for selecting and interpreting variables as predictor, mediator, or outcome variables. In practice, any observed concurrent relationship between psychological flexibility and outcomes of interest (e.g., wellbeing) could reflect multiple possibilities (e.g., psychological flexibility influences wellbeing, wellbeing influences psychological flexibility, bidirectional influence, a third variable [such as common method variance] influences both wellbeing and psychological flexibility, or a spurious correlation). Going forward, we aim to collect data longitudinally to enable further testing of these relationships over time, more apt to establish temporal precedence (and to reflect the dynamic nature of psychological flexibility; Kashdan & Rottenberg, 2010).
Notwithstanding the anonymous nature of data collection, the dependability of self-report data on ‘adherence’ to social distancing guidelines was likely subject to social desirability and demand artefacts. More broadly, the self-report nature of the study limits our ability to infer relationships between ways of coping or psychological flexibility and subjective outcomes of interest, because respondents may struggle to accurately report on their coping behaviours or propensity to respond with flexibility. Again, the strength of observed relationships between variables of interest is likely inflated by similarities in applied self-report formats (common method bias) particularly given their spatial and temporal contiguity in cross-sectional survey designs. The subjective nature of the explanatory and outcome variables of interest would make it difficult to meaningfully apply alternative methods, but longitudinal measurement may help to reduce the additional proximity bias (Pieters, 2017).
Whilst our selection of focal variables and measures was informed by theoretical interests, relatability to extant literature, and consideration of response burden, we have doubtlessly excluded variables and measures that may have enabled additional insight into our outcomes of interest. The majority of variance in our focal outcomes remains unexplained by the measures used in this study, and it is likely that we are missing important explanatory information in terms of individual historical and situational contexts. Moreover, expanded examination of coping and self-regulatory repertoires may have helped to account for relationships between psychological flexibility and health and wellbeing outcomes. Whilst we can say that those higher in psychological flexibility are tending to make less use of avoidant coping, we know less about the form and frequency of any alternative behaviours that they are using – again, we would expect that contextual responsiveness is key here, and this is unlikely to be reflected in unconditional measures of coping ‘styles’.
Whilst the applied chain-referral approach to recruitment is susceptible to bias, and might limit confidence in the broader representativeness of our sample, it was notable that responses from our participants converged with those from representative national surveys over the same timeframe (ONS, 2020; e.g., proportion reporting that they are very or somewhat worried about COVID-19). Direct and systematic replications (across different contexts, populations, and measurement strategies) would enable appreciation of whether/to what extent our findings apply more broadly.
Strengths of the study include its focus on explanatory variables (psychological flexibility and coping styles) that are amenable to interventional change. Whilst we found that some demographic variables (age, gender, and living arrangements) accounted for variance in outcomes of interest, the incremental explanatory power of (malleable) behavioural variables has clear implications for further research – indicating the potential value of examining whether interventions targeting psychological flexibility may be useful for promoting better psychological outcomes in the context of a pandemic.
Through explicit exploration of inter-relationships between explanatory variables of interest (psychological flexibility and coping styles) and their combined role in relation to important individual outcomes, another strength of the study is its empirical contribution to conceptual understanding. It is important to explore these relationships in the context of a naturalistic stressor, to understand whether theory- and logic-based assumptions hold under critical real-world conditions (i.e., the situations where our models become practically meaningful and potentially useful).
7. Conclusion
The current COVID-19 pandemic presents multiple potential stressors – including fears for the health and welfare of self and others, social isolation, loss of routine and contact with usual sources of positive reinforcement, and rapidly changing behavioural demands – in a context of indeterminate uncertainty. Taken together, our findings demonstrate the value of psychological flexibility for understanding and predicting individual differences in how people proximally respond to – and are impacted by – these stressors. Moreover, understanding these differences in terms of psychological flexibility has clear research implications: Supporting testing of scalable contemporary cognitive-behavioural approaches that target psychological flexibility – whether in addressing individual support needs as they arise, equipping groups (e.g., key workers) with skills that may foster resilience, or promoting psychological health in the broader population. Such approaches warrant further investigation and may hold promise for managing the current and longer-term psychological impact of the COVID-19 pandemic.
Declaration of competing interest
The authors have no competing interests to declare.
Acknowledgements
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
This study is part of a broader longitudinal cohort study that will examine these processes as the nature and impact of the pandemic unfolds over time.
Informed by Cohen (1992) we characterised the absolute magnitude of correlation coefficients as 0.10 = “small”, 30 = “moderate”, and 0.50 = “large”; with coefficients < 0.10 = “negligible”.
Contributor Information
David L. Dawson, Email: ddawson@lincoln.ac.uk.
Nima Golijani-Moghaddam, Email: nmoghaddam@lincoln.ac.uk.
References
- Bardeen J.R., Fergus T.A., Orcutt H.K. Experiential avoidance as a moderator of the relationship between anxiety sensitivity and perceived stress. Behavior Therapy. 2013;44(3):459–469. doi: 10.1016/j.beth.2013.04.001. [DOI] [PubMed] [Google Scholar]
- Bluett E.J., Homan K.J., Morrison K.L., Levin M.E., Twohig M.P. Acceptance and commitment therapy for anxiety and OCD spectrum disorders: An empirical review. Journal of Anxiety Disorders. 2014;28(6):612–624. doi: 10.1016/j.janxdis.2014.06.008. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A., Ho S.M., Chan J.C., Kwong R.S., Cheung C.K., Wong C.P. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: A latent class approach. Health Psychology. 2008;27(5):659. doi: 10.1037/0278-6133.27.5.659. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A., Papa A., Lalande K., Westphal M., Coifman K. The importance of being flexible: The ability to both enhance and suppress emotional expression predicts long-term adjustment. Psychological Science. 2004;15(7):482–487. doi: 10.1111/j.0956-7976.2004.00705.x. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020 doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown M., Glendenning A.C., Hoon A.E., John A. Effectiveness of web-delivered acceptance and commitment therapy in relation to mental health and well-being: A systematic review and meta-analysis. Journal of Medical Internet Research. 2016;18(8):e221. doi: 10.2196/jmir.6200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver C.S. You want to measure coping but your protocol’too long: Consider the brief cope. International Journal of Behavioral Medicine. 1997;4(1):92. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Chan A.O., Huak C.Y. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occupational Medicine. 2004;54(3):190–196. doi: 10.1093/occmed/kqh027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chawla N., Ostafin B. Experiential avoidance as a functional dimensional approach to psychopathology: An empirical review. Journal of Clinical Psychology. 2007;63(9):871–890. doi: 10.1002/jclp.20400. [DOI] [PubMed] [Google Scholar]
- Cheng C. Assessing coping flexibility in real-life and laboratory settings: A multimethod approach. Journal of Personality and Social Psychology. 2001;80(5):814. doi: 10.1037//0022-3514.80.5.814. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112(1):155. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Dattalo P. Oxford University Press; 2013. Analysis of multiple dependent variables. [Google Scholar]
- Eisenberg S.A., Shen B.-J., Schwarz E.R., Mallon S. Avoidant coping moderates the association between anxiety and patient-rated physical functioning in heart failure patients. Journal of Behavioral Medicine. 2012;35(3):253–261. doi: 10.1007/s10865-011-9358-0. [DOI] [PubMed] [Google Scholar]
- Fat L.N., Scholes S., Boniface S., Mindell J., Stewart-Brown S. Evaluating and establishing national norms for mental wellbeing using the short Warwick–Edinburgh mental well-being scale (SWEMWBS): Findings from the health survey for England. Quality of Life Research. 2017;26(5):1129–1144. doi: 10.1007/s11136-016-1454-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonseca S., Trindade I.A., Mendes A.L., Ferreira C. The buffer role of psychological flexibility against the impact of major life events on depression symptoms. Clinical Psychologist. 2020;24(1):82–90. [Google Scholar]
- Francis A.W., Dawson D.L., Golijani-Moghaddam N. The development and validation of the comprehensive assessment of acceptance and commitment therapy processes (CompACT) Journal of Contextual Behavioral Science. 2016;5(3):134–145. [Google Scholar]
- Gilbody S., Richards D., Barkham M. Diagnosing depression in primary care using self-completed instruments: UK validation of PHQ–9 and CORE–OM. British Journal of General Practice. 2007;57(541):650–652. [PMC free article] [PubMed] [Google Scholar]
- Giorgi G., Perez F.S.F., D'Antonio A.C., Mucci N., Ferrero C., Cupelli V. Psychometric properties of the Impact of Event Scale-6 in a sample of victims of bank robbery. Psychology Research and Behavior Management. 2015;8:99. doi: 10.2147/PRBM.S73901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gloster A.T., Klotsche J., Chaker S., Hummel K.V., Hoyer J. Assessing psychological flexibility: What does it add above and beyond existing constructs? Psychological Assessment. 2011;23(4):970. doi: 10.1037/a0024135. [DOI] [PubMed] [Google Scholar]
- Gloster A.T., Meyer A.H., Lieb R. Psychological flexibility as a malleable public health target: Evidence from a representative sample. Journal of Contextual Behavioral Science. 2017;6(2):166–171. [Google Scholar]
- González-Sanguino C., Ausín B., ÁngelCastellanos M., Saiz J., López-Gómez A., Ugidos C. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacker T., Stone P., MacBeth A. Acceptance and commitment therapy–do we know enough? Cumulative and sequential meta-analyses of randomized controlled trials. Journal of Affective Disorders. 2016;190:551–565. doi: 10.1016/j.jad.2015.10.053. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. Guilford publications; 2017. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Hayes S.C., Strosahl K.D., Wilson K.G. American Psychological Association; Washington, DC: 2009. Acceptance and commitment therapy. [Google Scholar]
- Hayes S.C., Villatte M., Levin M., Hildebrandt M. Open, aware, and active: Contextual approaches as an emerging trend in the behavioral and cognitive therapies. Annual Review of Clinical Psychology. 2011;7 doi: 10.1146/annurev-clinpsy-032210-104449. [DOI] [PubMed] [Google Scholar]
- Hayes S.C., Wilson K.G., Gifford E.V., Follette V.M., Strosahl K. Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology. 1996;64(6):1152. doi: 10.1037//0022-006x.64.6.1152. [DOI] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L.…Everall I. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson N.W., Anusic I., Lucas R.E., Donnellan M.B. Comparing the reliability and validity of global self-report measures of subjective well-being with experiential day reconstruction measures. Assessment. 2020;27(1):102–116. doi: 10.1177/1073191117744660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui D.S., Wong K.T., Ko F.W., Tam L.S., Chan D.P., Woo J. The 1-year impact of severe acute respiratory syndrome on pulmonary function, exercise capacity, and quality of life in a cohort of survivors. Chest. 2005;128(4):2247–2261. doi: 10.1378/chest.128.4.2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulbert‐Williams N.J., Storey L., Wilson K.G. Psychological interventions for patients with cancer: Psychological flexibility and the potential utility of acceptance and commitment therapy. European Journal of Cancer Care. 2015;24(1):15–27. doi: 10.1111/ecc.12223. [DOI] [PubMed] [Google Scholar]
- Johns Hopkins University & Medicine (Producer) 2020. Coronavirus Resource Center.https://coronavirus.jhu.edu 24/05/2020. [Google Scholar]
- Karekla M., Panayiotou G. Coping and experiential avoidance: Unique or overlapping constructs? Journal of Behavior Therapy and Experimental Psychiatry. 2011;42(2):163–170. doi: 10.1016/j.jbtep.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Kashdan T.B., Barrios V., Forsyth J.P., Steger M.F. Experiential avoidance as a generalized psychological vulnerability: Comparisons with coping and emotion regulation strategies. Behaviour Research and Therapy. 2006;44(9):1301–1320. doi: 10.1016/j.brat.2005.10.003. [DOI] [PubMed] [Google Scholar]
- Kashdan T.B., Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review. 2010;30(7):865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwek S.-K., Chew W.-M., Ong K.-C., Ng A.W.-K., Lee L.S.-U., Kaw G. Quality of life and psychological status in survivors of severe acute respiratory syndrome at 3 months postdischarge. Journal of Psychosomatic Research. 2006;60(5):513–519. doi: 10.1016/j.jpsychores.2005.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee E.B., An W., Levin M.E., Twohig M.P. An initial meta-analysis of Acceptance and Commitment Therapy for treating substance use disorders. Drug and Alcohol Dependence. 2015;155:1–7. doi: 10.1016/j.drugalcdep.2015.08.004. [DOI] [PubMed] [Google Scholar]
- Lee A.M., Wong J.G., McAlonan G.M., Cheung V., Cheung C., Sham P.C.…Chua S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Canadian Journal of Psychiatry. 2007;52(4):233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- Levis B., Benedetti A., Thombs B.D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: Individual participant data meta-analysis. BMJ. 2019;365 doi: 10.1136/bmj.l1476. l1476-l1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Kakade M., Fuller C.J., Fan B., Fang Y., Kong J.…Wu P. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive Psychiatry. 2012;53(1):15–23. doi: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Masuda A., Tully E.C. The role of mindfulness and psychological flexibility in somatization, depression, anxiety, and general psychological distress in a nonclinical college sample. Journal of Evidence-Based Complementary & Alternative Medicine. 2012;17(1):66–71. [Google Scholar]
- Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S.…Hunter J.J. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infectious Diseases. 2006;12(12):1924. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken L.M., Morley S. The psychological flexibility model: A basis for integration and progress in psychological approaches to chronic pain management. The Journal of Pain. 2014;15(3):221–234. doi: 10.1016/j.jpain.2013.10.014. [DOI] [PubMed] [Google Scholar]
- McManus S., Meltzer H., Brugha T., Bebbington P., Jenkins R. 2009. Adult psychiatric morbidity in England: Results of a household survey. [DOI] [PubMed] [Google Scholar]
- Morris J., Golijani-Moghaddam N., Dawson D.L. University of Nottingham; 2019. Development and validation of a short form of the comprehensive assessment of acceptance and commitment therapy processes (CompACT-SF) (Doctorate in Clinical Psychology) [Google Scholar]
- Nielsen E., Sayal K., Townsend E. Exploring the relationship between experiential avoidance, coping functions and the recency and frequency of self-harm. PloS One. 2016;11(7) doi: 10.1371/journal.pone.0159854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odriozola-González P., Planchuelo-Gómez Á., Irurtia-Muñiz M.J., de Luis-García R. 2020. Psychological symptoms of the outbreak of the COVID-19 crisis and confinement in the population of Spain. [Google Scholar]
- Office for National Statistics [ONS] 2020. Coronavirus and the social impacts on Great Britain data.https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/datasets/coronavirusandthesocialimpactsongreatbritaindata Retrieved from. [Google Scholar]
- Orgilés M., Morales A., Delvecchio E., Mazzeschi C., Espada J.P. 2020. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cadernos de Saúde Pública. 2020;36 doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- Pieters R. Meaningful mediation analysis: Plausible causal inference and informative communication. Journal of Consumer Research. 2017;44(3):692–716. [Google Scholar]
- Powers M.B., Vörding M.B.Z.V.S., Emmelkamp P.M. Acceptance and commitment therapy: A meta-analytic review. Psychotherapy and Psychosomatics. 2009;78(2):73–80. doi: 10.1159/000190790. [DOI] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry. 2020 doi: 10.1016/j.ajp.2020.102066. 102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rueda B., Valls E. Is the effect of psychological inflexibility on symptoms and quality of life mediated by coping strategies in patients with mental disorders? International Journal of Cognitive Therapy. 2020:1–15. [Google Scholar]
- Schönbrodt F.D., Perugini M. At what sample size do correlations stabilize? Journal of Research in Personality. 2013;47(5):609–612. [Google Scholar]
- Sim K., Chan Y.H., Chong P.N., Chua H.C., Soon S.W. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. Journal of Psychosomatic Research. 2010;68(2):195–202. doi: 10.1016/j.jpsychores.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stewart-Brown S., Tennant A., Tennant R., Platt S., Parkinson J., Weich S. Internal construct validity of the Warwick-Edinburgh mental well-being scale (WEMWBS): A Rasch analysis using data from the Scottish health education population survey. Health and Quality of Life Outcomes. 2009;7(1):15. doi: 10.1186/1477-7525-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoresen S., Tambs K., Hussain A., Heir T., Johansen V.A., Bisson J.I. Brief measure of posttraumatic stress reactions: Impact of Event Scale-6. Social Psychiatry and Psychiatric Epidemiology. 2010;45(3):405–412. doi: 10.1007/s00127-009-0073-x. [DOI] [PubMed] [Google Scholar]
- Tyndall I., Waldeck D., Pancani L., Whelan R., Roche B., Pereira A. Profiles of psychological flexibility: A latent class analysis of the acceptance and commitment therapy model. Behavior Modification. 2020;44(3):365–393. doi: 10.1177/0145445518820036. [DOI] [PubMed] [Google Scholar]
- UK Government. (2020). Retrieved from https://www.gov.uk/government/news/police-given-new-powers-and-support-to-respond-to-coronavirus.
- Veehof M.M., Oskam M.-J., Schreurs K.M., Bohlmeijer E.T. Acceptance-based interventions for the treatment of chronic pain: A systematic review and meta-analysis. PAIN®. 2011;152(3):533–542. doi: 10.1016/j.pain.2010.11.002. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss D.S. Springer; 2007. The impact of event scale: Revised cross-cultural assessment of psychological trauma and PTSD. [Google Scholar]
- Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies. 2005;18(1):39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmer-Gembeck M.J., Skinner E.A., Modecki K.L., Webb H.J., Gardner A.A., Hawes T. The self-perception of flexible coping with stress: A new measure and relations with emotional adjustment. Cogent Psychology. 2018;5(1):1537908. [Google Scholar]