Abstract
Background
Inhibition of interleukin (IL)-1 represents a promising treatment option in adult-onset Still's disease (AOSD).
Objective
To investigate the efficacy and safety of canakinumab in patients with AOSD and active joint involvement by means of a multicentre, double-blind, randomised, placebo-controlled trial.
Methods
Patients with AOSD and active joint involvement (tender and swollen joint counts of ≥4 each) were treated with canakinumab (4 mg/kg, maximum 300 mg subcutaneous every 4 weeks) or placebo. The primary endpoint was the proportion of patients with a clinically relevant reduction in disease activity at week 12 as determined by the change in disease activity score (ΔDAS28>1.2).
Results
At enrolment, patients had high active disease with a mean DAS28(ESR) of 5.4 in the canakinumab and 5.3 in the placebo group, respectively. In the intention-to-treat analysis, 12 patients (67%) in the canakinumab group and 7 patients (41%) in the placebo group fulfilled the primary outcome criterion (p=0.18). In the per-protocol analysis, significantly higher American College of Rheumatology (ACR) 30% (61% vs 20%, p=0.033), ACR 50% (50% vs 6.7%, p=0.009) and ACR 70% (28% vs 0%, p=0.049) response rates were observed in the canakinumab group compared with the placebo group. Two patients in the canakinumab group experienced a serious adverse event.
Conclusion
Although the study was terminated prematurely and the primary endpoint was not achieved, treatment with canakinumab led to an improvement of several outcome measures in AOSD. The overall safety findings were consistent with the known profile of canakinumab. Thus, our data support indication for IL-1 inhibition with canakinumab in AOSD.
Keywords: adult onset still's disease, arthritis, disease activity
Key messages.
What is already known about this subject?
During protocol development in 2011, and regularly through study trial premature termination in 2018, we searched PubMed with the terms adult-onset Still’s disease (AOSD) and a combination of AOSD and interleukin (IL)-1, canakinumab, anakinra, treatment, clinical trials, review and macrophage activating syndrome.
(In vivo) Studies show the central importance of innate immune cell activation and the overproduction of proinflammatory cytokines, such as IL-1, IL-6 and IL-18.
What does this study add?
This study was of important relevance for the approval of canakinumab for the treatment of patients with AOSD by the European Medicines Agency.
How might this impact on clinical practice or future developments?
AOSD is a rare systemic autoinflammatory disease with potentially severe disease manifestations and complications. In the beginning of this trial there were no approved drugs for the specific diagnosis AOSD. Physicians used to point to rheumatoid arthritis, (systemic) juvenile arthritis and Still’s disease to treat patients. This study supports that the use of canakinumab in patients with AOSD represents a valuable treatment approach.
Introduction
Targeted therapies have changed the course of disease and outcome in several autoimmune diseases. Recently, major progress has been achieved in the treatment of autoinflammatory conditions, especially with the approval of interleukin (IL)-1 and IL-6 inhibitors.1–5 These drugs have been mainly investigated in controlled clinical trials in children, including systemic juvenile idiopathic arthritis (sJIA).6–22 However, due to a lower prevalence of disease, a lack of standardised classification criteria and outcome measurements, only a few studies were have been performed in adults so far.23–36
Because of a similar pathogenesis, broadly overlapping symptoms and organ involvement, adult-onset Still's disease (AOSD) is believed to represent a disease continuum of sJIA.37 38 This hypothesis is supported by similar biomarker profiles, including cytokine and transcriptomic data, as well as by the disease manifestation.39 40 In addition to the classic traits of spiking fever, transient rash and arthritic joint involvement, both conditions can be complicated by potentially life-threatening manifestations such as serositis, vasculitis, pneumonitis and macrophage activating syndrome (MAS).41 42 Especially in MAS, the pathogenic relevance of dysregulated cytokine release is evident, leading to severe complications and a high mortality rate.41
In agreement with the postulation that sJIA and AOSD represent the same disease, it has been shown in numerous studies that similar approaches with IL-1 and IL-6 inhibiting drugs are sufficient to control disease activity in both conditions. In a retrospective analysis, the efficacy and safety of canakinumab are comparable between children and adolescent patients with sJIA.43 In particular, arthritic joint involvement was improved to a similar degree, irrespective of the age of the treated patients in these sJIA studies.43 However, these findings have still to be confirmed by controlled clinical studies in AOSD. In this context, it is remarkable to mention that the IL-6 receptor antagonist tocilizumab has failed to significantly improve primary as well as secondary outcome measures in a small phase III study in AOSD recently.28 Of note, in this study, the placebo response rates were clearly higher as in the sJIA study.7 This indicates that the obtained results from controlled studies in children may not at times be easily translated into adult patients.
Tumour necrosis factor inhibition can be considered as third-line treatment for patients with AOSD, preferentially with chronic arthritis, as shown in some uncontrolled trials involving small cohorts of patients.44–49 Tadekinig alfa, a recombinant human IL-18-binding protein, was investigated in an open-label study and showed promising results for efficacy in AOSD.50
Canakinumab is a specific IL-1β antagonist, which has been approved for the treatment of different autoinflammatory diseases, including children aged >2 years with sJIA, adults and children aged >2 years with cryopyrin associated periodic syndrome (CAPS), TNF receptor associated periodic syndrome (TRAPS) and familial mediterranean fever (FMF). Of note, the optimal dosing regimen was found to be different in the investigated conditions according to pharmacokinetic and dynamic results. In fact, patients with sJIA require a dosage of canakinumab at 4 mg/kg body weight and a short injection interval with monthly administration in contrast to CAPS with a bimonthly cycle. Since only a few small cohort studies have been published for the efficacy and safety of canakinumab in AOSD so far, we initiated a clinical study by using a similar dosing regimen as in sJIA.
Patients and methods
Study design
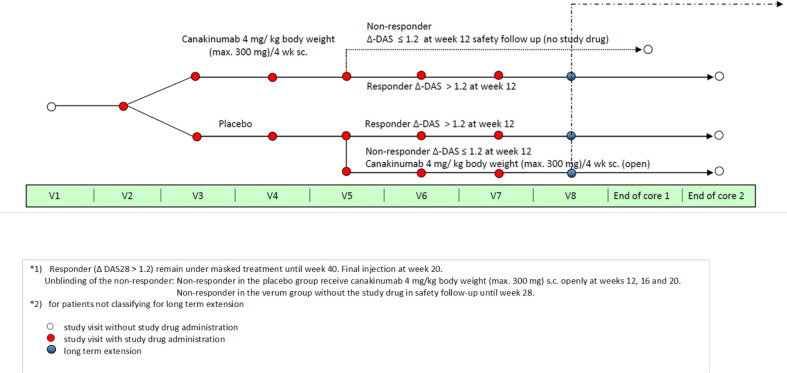
The phase II Canakinumab for Treatment of Adult-Onset Still’s Disease to Achieve Reduction of Arthritic Manifestation (CONSIDER) study was performed as a multicentre, double-blind, randomised, placebo-controlled trial in patients with AOSD and active joint involvement (figure 1). Randomisation stratified by pretreatment status with biological disease-modifying antirheumatic drug (bDMARDs) and study centre was performed in a 1:1 ratio to the canakinumab 4 mg/kg body weight or the placebo arm according to Atkinsons’s DA-optimal biassed coin algorithm.51 As justification for the selection of the higher canakinumab dose, reference is made to the similarity of the clinical pictures of Still's disease in juvenile and adult age groups. According to current knowledge gained from pharmacokinetic investigations, a higher dose of canakinumab (4 mg/kg monthly) is required in patients with sJIA compared, for example, with CAPS patients.52 53 Placebo non-responders at week 12 received canakinumab from weeks 12 to 24. Patients who responded to treatment at week 24 were able to enter the long-term extension (LTE) phase being treated with canakinumab (open label).
Figure 1.
Study design. ΔDAS, change in disease activity score.
Patients
All patients provided written informed consent before any assessment was performed. Patients were not involved in study design development.54 Patients with AOSD and active joint involvement were eligible for enrolment if they fulfilled the AOSD Yamaguchi classification criteria,55 were aged between 18 and 75 years, had a disease activity based on DAS28(ESR) of ≥3.2 at screening, and had ≥4 tender and swollen (28-joint count) joint counts at screening and baseline. In patients treated with non-steroidal anti-inflammatory drugs (NSAIDs), glucocorticoids or conventional DMARDs, a stable dose prior to randomisation and throughout study treatment was required (≥2 weeks (NSAIDs), ≥1 week (glucocorticoids with a dose of ≤10 mg/day prednisolone equivalent) and ≥6 weeks (conventional DMARDs)). For bDMARDs, a washout period between 1 week and 9 months was required, depending on the substance.28 35 53 56 After approval of canakinumab for the indication of AOSD by the European Medicines Agency (EMA), recruitment was stopped prematurely with enrolment of 36 out of 68 planned patients.
Efficacy outcomes
The primary outcome was defined as the proportion of patients with a clinically relevant reduction of the articular manifestation measured by change in disease activity score (ΔDAS28(ESR)>1.2) at week 12. Several additional secondary outcomes were investigated at weeks 4, 8 and 12 and at visits thereafter, including DAS28 (ESR and CRP), fever episodes, physician assessment of disease activity, limitation of motion (LOM), patient-reported outcomes: assessment of pain, Health Assessment Questionnaire (HAQ)–Disability Index quality of life 36-Item Short Form Survey (SF-36), American College of Rheumatology (ACR) and European League Against Rheumatism (EULAR) response criteria developed for rheumatoid arthritis and a modified adapted ACR variable (requiring ACR 30% response (ACR30) in addition no intermittent fever in the preceding week and no more than one out of seven variables worsening by more than 30%).
Safety evaluation
Safety events including relevant laboratory changes were captured at every visit. Furthermore, in the safety analysis, the two patients randomised to the placebo group who mistakenly received canakinumab at week 4 were considered to be exposed to canakinumab thereafter. According to these determinations, assignments of adverse events (AEs) and serious adverse events (SAEs) were made; the total placebo and canakinumab exposure times were calculated; and rates per 100 patient-years were estimated for each AE and SAE. Patients who contributed to placebo and canakinumab exposure added for that reason also to the denominator of both groups in the case that the percentage of patients with an AE was calculated.
Statistical analyses
The statistical evaluation of the efficacy of canakinumab was conducted according to the intention-to-treat (ITT) principle. The safety analyses were based on all patients randomised who received at least one dose of the study drug.
The two-sided Fisher’s exact test was applied to compare the primary endpoint at week 12. Patients with missing primary outcome data were considered to be non-responders. Furthermore, Fisher’s exact test was applied to compare binary and categorical (eg, EULAR response criteria) secondary outcome measures at weeks 4, 8 and 12 between the treatment groups. Additionally, mid-p 95% CIs of the response rates were calculated to describe the uncertainty in the estimates. The last observation carried forward (LOCF) method was used to impute a maximum of five missing parameters needed to calculate the ACR response criterion. Non-responder imputation was used in the other case, as well as in the case of other missing binary outcome data. No adjustments of p values for multiple testing were made. This is also true for the PP analyses.
Analysis of covariance (ANCOVA) was applied to compare the outcome of continuous parameters at week 12 between the treatment group (verum) and the placebo group after adjustment for the baseline status (covariable). For parameters assessed at screening and at the baseline visit, the average of both values was used as covariable. LOCF was used to impute missing values of the outcome at week 12. In addition, baseline (covariable) adjusted least square means (LSmeans) of the outcome parameter and their corresponding 95% CI were calculated. Since in the case of skewed parameters large individual values were able to bias the LSmean estimates and to increase the error variance clearly, the following specification was made: a non-parametric ANCOVA model was applied in case of the following parameters: laboratory parameters: erythrocyte sedimentation rate, C reactive protein, ferritin and joint counts. No adjustments of p values for multiple testing were made in any analysis of secondary outcomes. The online supplementary material includes details to the statistical analysis.
annrheumdis-2020-217155supp001.pdf (682.6KB, pdf)
Results
Description of patients included
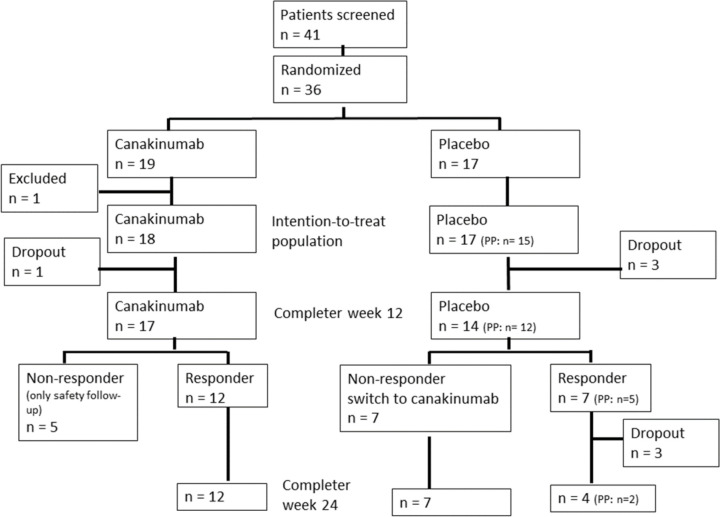
A total of 41 patients were screened and 36 of them were randomised (figure 2). In one of the patients randomised to canakinumab, the diagnosis was changed to Whipple’s disease leading to exclusion from the efficacy analysis. Baseline characteristics are summarised in table 1 and online supplementary table S1. Due to the limited sample sizes, some differences, for example, in the percentage of female patients or the percentage of patients with short disease duration, were observed, which did not achieve statistical significance.
Figure 2.
Flowchart of patients screened and randomised.
Table 1.
Baseline characteristics
| Parameter | Canakinumab | Placebo | |
| n=18 | n=17 | ||
| Female | n (%) | 10 (55.6) | 13 (76.5) |
| Age | Mean (SD) | 41.06 (13.2) | 40.53 (13.2) |
| Time since diagnosis (years) | Median (IQR) | 2.6 (0.3–4.7) | 1.6 (0.3–3.8) |
| Diagnosis since <1 year | n (%) | 6 (33.3) | 8 (47.1) |
| Diagnosis since ≥5 years | n (%) | 4 (22.2) | 4 (23.5) |
| Previous bDMARDs | n (%) | 13 (72.2) | 13 (76.5) |
| Previous anakinra | n (%) | 12 (66.7) | 13 (76.5) |
| Previous TNF inhibitors | n (%) | 6 (33.3) | 6 (35.3) |
| Previous tocilizumab | n (%) | 4 (22.2) | 2 (11.8) |
| 28-tender joint count | Mean (SD) | 6.94 (4.4) | 7.29 (5.2) |
| 28-swollen joint count | Mean (SD) | 5.22 (1.5) | 6.65 (4.7) |
| DAS28(ESR) | Mean (SD) | 5.4 (0.8) | 5.3 (1.2) |
| ESR (mm/hour) | Median (IQR) | 44 (28–70) | 50 (17.5–63) |
| CRP (mg/L) | Median (IQR) | 40.4 (20.5–85.8) | 38 (9.4–101.2) |
| Ferritin (ng/mL) | Median (IQR) | 448 (220–772) | 173.4 (60–664) |
| Fever | n (%) | 9 (50) | 8 (47.1) |
| Lymphadenopathy | n (%) | 2 (11.1) | 0 |
| Serositis | n (%) | 0 | 0 |
| Skin manifestation (rash) | n (%) | 4 (22.2) | 6 (35.3) |
| Sore throat | n (%) | 1 (5.6) | 0 |
| Myalgia | n (%) | 1 (5.6) | 0 |
bDMARD, biological disease-modifying antirheumatic drug; CRP, C-reactive protein; DAS28 (CRP), disease activity score 28 (using C-reactive protein value); DAS28 (ESR), disease activity score 28 (using erythrocyte sedimentation rate value); ESR, erythrocyte sedimentation rate; TNF, tumour necrosis factor.
Efficacy outcomes of the double-blind period (ITT population if not otherwise indicated)
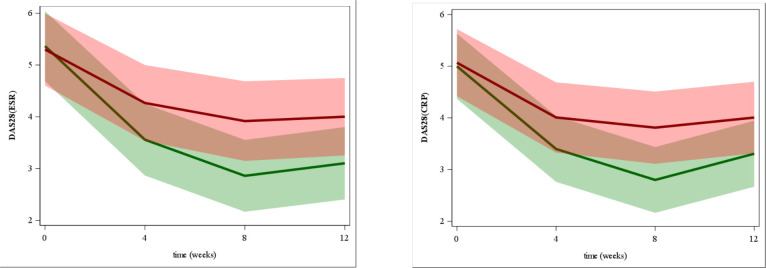
Twelve patients in the canakinumab and seven patients in the placebo group showed a reduction of the DAS28(ESR) of more than 1.2 at week 12 (66.7% vs 41.2%, respectively) (figure 3). The difference in the DAS28(ESR) response rate of 25.5% (95% CI −10.3% to 55.9%) was not statistically significant (p=0.18, Fisher’s test) and the primary outcome was not met.
Figure 3.
Intention-to-treat improvement in disease activity score 28 (using erythrocyte sedimentation rate value) DAS28(ESR) and disease activity score 28 (using C-reactive protein value) pDAS28(CRP). LSmeans estimates of DAS28(ESR) and DAS28(CRP) and their 95% CIs calculated by means of a linear mixed model: green line: LSmeans canakinumab group, green area: 95% CI of the LSmeans of the canakinumab group; red line: LSmeans of the placebo group, red area: 95% CI of the LSmeans of the placebo group, brown area: overlap of both 95% CI areas. LSmeans, least square means.
Although the response rates for several secondary outcome parameters were higher in the verum group, the differences compared with the placebo group did not achieve statistical significance (table 2 and online supplementary table S2).
Table 2.
Intention-to-treat number of patients fulfilling primary and secondary response criteria at week 12
| Outcome parameter | Canakinumab | Placebo | P value | OR (95% CI) | ||
| Responder n (%) | 95% CI | Responder n (%) | 95% CI | |||
| DAS28(ESR) response | 12 (66.7) | 43.1 to 85.2 | 7 (41.2) | 20.1 to 65 | 0.18 | 2.86 (0.72 to 11.31) |
| DAS28(CRP) response | 12 (66.7) | 43.1 to 85.2 | 7 (41.2) | 20.1 to 65 | 0.18 | 2.86 (0.72 to 11.31) |
| ACR20 | 11 (61.1) | 37.7 to 81.1 | 7 (41.2) | 20.1 to 65 | 0.32 | 2.86 (0.72 to 11.31) |
| ACR30 | 11 (61.1) | 37.7 to 81.1 | 5 (29.4) | 11.7 to 53.7 | 0.09 | 2.24 (0.58 to 8.69) |
| ACR30 mod | 10 (55.6) | 32.7 to 76.8 | 4 (23.5) | 8 to 47.5 | 0.09 | 3.77 (0.92 to 15.44) |
| ACR50 | 9 (50) | 27.8 to 72.2 | 3 (17.6) | 4.7 to 40.9 | 0.08 | 4.06 (0.95 to 17.42) |
| ACR70 | 5 (27.8) | 11 to 51.3 | 2 (11.8) | 2 to 33.7 | 0.40 | 4.67 (0.99 to 22.03) |
| ACR90 | 2 (11.1) | 1.9 to 32.1 | 1 (5.9) | 0.3 to 25.8 | 1.0 | 2.88 (0.48 to 17.45) |
| EULAR response | 14 (77.8) | 54.7 to 92.5 | 9 (52.9) | 29.7 to 75.2 | 0.16 | 1.88 (0.16 to 22.83) |
| EULAR DAS(CRP) Resp. | 13 (72.2) | 48.7 to 89 | 8 (47.1) | 24.8 to 70.3 | 0.18 | 3.11 (0.72 to 13.44) |
Diff. response in % indicates difference between the response rates (in per cent)
EULAR response indicates good or moderate response according to the EULAR criterion based on disease activity score 28 (using erythrocyte sedimentation rate value) DAS28(ESR) or if specified on disease activity score 28 (using C-reactive protein value) DAS28(CRP).
ACR, American College of Rheumatology; ACR20, ACR 20% response; ACR30, ACR 30% response; ACR90, ACR 90% response; ACR30 mod, modified ACR 30 response; EULAR, European League Against Rheumatism; Resp, response.
Information on systemic manifestations was collected at each visit; lymphadenopathy, serositis and other features were captured in physical examination. Laboratory abnormalities were captured in the AE form. At week 12, more canakinumab-treated patients reported to be free from fever for the past 7 days (77.8% and 64.7%) compared with placebo. A similar occurrence of skin manifestations was observed in the canakinumab and placebo groups (1/21 (4.8%) and 1/15 (6.7%)). There was no report of lymphadenopathy, pericarditis, pleuritis or laboratory abnormalities in both groups.
In the per-protocol (PP) population, two patients randomised to placebo who received canakinumab at week 4 were excluded. This led to a decrease in the response rate in the placebo group to 5 (33.3%) (p=0.08, Fisher’s test) (online supplementary table S3). There were significant differences between response rates in the PP analyses regarding ACR30, ACR 50% response and ACR 70% response (online supplementary figure S1).
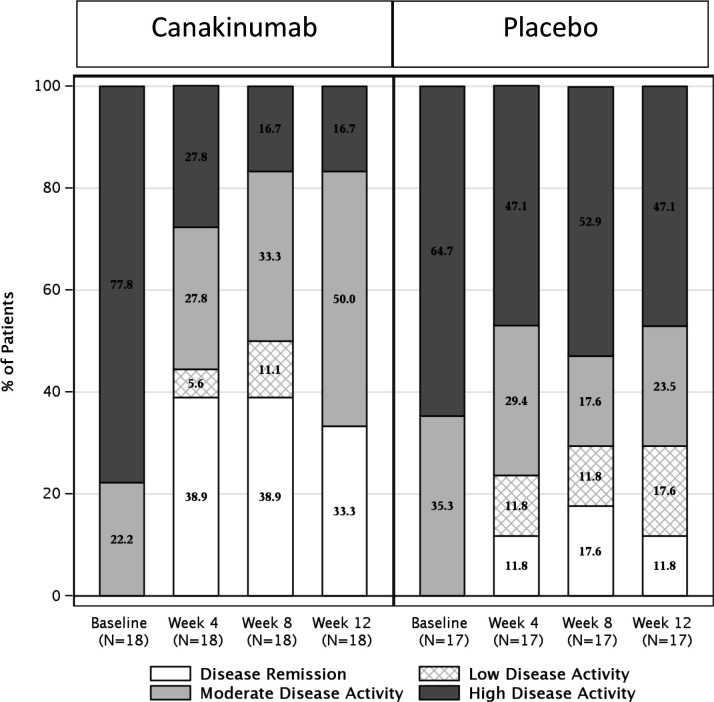
Five verum patients (33.3%) compared with two (11.8%) of the placebo patients achieved remission according to the DAS28(ESR) criterion (DAS28(ESR)<2.6) at week 12 (p=0.23, figure 4). Of note, in the PP analyses, none of the remaining placebo patients achieved DAS28(CRP) or extended remission with a significant difference in favour of canakinumab (DAS28(CRP) remission, n=7, p=0.01, and extended remission, n=5, p=0.05, respectively; online supplementary table S4).
Figure 4.
DAS28(ESR) disease activity by treatment groups and visits with imputation.
By using ANCOVA, a significantly higher improvement in disease activity score 28 (using erythrocyte sedimentation rate value) DAS28(ESR) and disease activity score 28 (using C-reactive protein value) DAS28(CRP) was observed in the canakinumab group at week 12 (online supplementary table S2). Further secondary outcome measures such as physician’s global assessment of disease activity, pain, ferritin levels, HAQ, SF-36 and LOM are shown for the PP analyses in online supplementary table S5.
Clinical outcomes from weeks 12 to 24
Placebo non-responders who switched to canakinumab according to the protocol had a similar outcome after 12 weeks of treatment with canakinumab (at week 24) than those randomised to verum at baseline (BL) (online supplementary table S6).
Ten out of 12 canakinumab DAS28(ESR) responders at week 12 remained DAS28(ESR) responders until week 24, while the other two remained responders until week 20.
Four placebo responders who were not withdrawn after week 12 remained DAS28(ESR) responders until week 24. Of note, two of them had received one dose of canakinumab at week 4 (mistakes by independent pharmacists).
LTE phase
In this phase, patients who responded to treatment with the study drug (canakinumab or placebo) were treated with open-label canakinumab to capture long-term safety events and efficacy. Four patients remained in DAS28(ESR) remission (<2.6), whereas the remaining three patients were in low-disease activity (<3.2) during the full LTE period.
Safety analysis
Within the first 12-week-period of this trial, two patients experienced an SAE, both of them under treatment with canakinumab (increased liver enzymes and patellofemoral pain syndrome leading to hospitalisation).
Further seven SAEs were observed in the second period of the study (between weeks 12 and 24): two in canakinumab-exposed patients (deep vein thrombosis and hypotonia) and the other five in one patient treated with placebo (fracture at MCP 5, hand fracture, removal of a medical device at MCP 5, upper abdominal pain and acute cholecystitis).
During the LTE period, there were two ongoing SAEs which began prior to week 24 (upper abdominal pain in previous hospitalisation for cholecystitis and chondromalacia due to patellofemoral syndrome).
Further details to SAEs and all AEs are included in the online supplementary material.
First results of this study have been presented as posters in EULAR Congress and German Rheumatology Congress in 2019.57 58
Discussion
This study was of important relevance for approval of canakinumab for the treatment of patients with AOSD by the EMA. Due to the rarity and severity of the disease as well as the conditional approval of canakinumab for AOSD by the EMA, it was difficult to complete the recruitment of this placebo-controlled trial. For these reasons, the study was terminated prematurely and only 3635 out of the planned 68 patients could be included in the efficacy analysis. Of note, randomisation within strata of patients led to similar baseline characteristics with a highly active disease with a mean DAS28(ESR) score of 5.4 in the canakinumab (n=18) and 5.3 in the placebo group (n=17). Our prediction of the DAS28 (ESR and CRP) response rates in the active treatment group, as well as in the placebo group, was very close to the obtained results; however, due to a lower number of recruited patients, the difference in the primary outcome and several secondary outcomes was not statistically significant. The primary outcome, in addition to several secondary outcomes, was not met. Nevertheless, most of the observed results including, for example, DAS28 (ESR and CRP) but also ACR30, ACR50 and ACR70 rates were higher in the canakinumab group compared with the placebo group. The better results in the canakinumab arm were especially highlighted in the PP analysis, since the respective response rates as well as the change in the mean levels were higher in the verum group at week 12 and now significant. Furthermore, the efficacy of canakinumab was also supported by the fact that placebo non-responders who switched to canakinumab at week 12 reached a similar efficacy outcome after 12 weeks of treatment as those randomised to canakinumab during the first 12 weeks.
It is important to note that our study was also hampered by the fact that at the time of protocol design, no established outcome measures were available for evaluation of disease activity in AOSD in clinical trials. Therefore, our decision to use the active joint involvement in AOSD as a primary outcome measure may not be fully representative of the disease state, since this measure does not sufficiently take into account the systemic manifestations in AOSD. We used a modified adapted ACR variable as a secondary outcome parameter in order to estimate disease activity including systemic features. We would strongly encourage to establish a specific AOSD score, like the modified Pouchot or the 2016 published AIDAI score.59–62 Unfortunately, a Pouchot score post hoc analysis with our study data is not possible because there are simply too many baseline parameters missing to precisely describe the systemic disease activity. Furthermore, it is known that a significant proportion of patients with AOSD have a self-limited course of their disease. An additional limitation of this study was the lack of information about the reason for previous treatment discontinuation. Another unfortunate point to consider was the fact that two patients of the placebo group received mistakenly canakinumab at week 4. All of these might have contributed to a relatively high placebo response rate in our study. However, a higher response rate was observed in the canakinumab arm compared with placebo for most of the outcome measures. Thus, the results also indicate that inhibition of IL-1β signalling in AOSD represents a valuable treatment approach.
The discussion concerning an individualised treatment for specific manifestations of AOSD is ongoing. The main question is whether IL-6 blockade could be more effective in the control of arthritic manifestation, whereas lL-1 could be a better target in case of predominant systemic manifestation. However, the evidence for a dichotomous approach in AOSD is still limited, and several studies have shown a beneficial result for both targets in one or more AOSD manifestations simultaneously.10 14 17 27 30 39 43 63–68 In our study, we focused on articular manifestations of AOSD; therefore, our cohort is not representative for the full spectrum of disease, and further research investigating a stratified treatment approach is needed.
As in other previous canakinumab studies, no identical placebo for canakinumab was available in this study. The decision to use unblinded, independent drug dispensers led to mistakes. In fact, the pharmacokinetics (PK)/pharmacodynamics (PD) analysis of all patients revealed that two placebo patients were inadvertently treated with canakinumab. Since the primary endpoint was missed by a very close margin, the fact that these two placebo patients reached remission could be the reason that the primary endpoint was not met.
In a biomarker substudy of this CONSIDER randomised controlled trial, we were also able to show that the transcriptomic signature from patients with AOSD was similar to patients with sJIA.40 These results provide additional evidence for the role of the IL-1 signalling pathway and support the concept of a Still's disease continuum that includes both a paediatric/juvenile-onset (sJIA) and an adult-onset (AOSD) form.
Although the study was terminated prematurely and the primary endpoint did not achieve statistical significance, treatment of patients with AOSD and active joint involvement with canakinumab led to an improvement of several outcome measures. In addition, the safety profile was similar to that reported in sJIA, and no unexpected safety issues were observed. These data support the treatment of patients with AOSD with canakinumab using 4 mg/kg body weight every 4 weeks.39
Acknowledgments
We thank the study nurses and patients; without them, the study would not have been possible. We thank Novartis Pharma GmbH Deutschland for the financial support and for study drug provision.
Footnotes
Handling editor: Josef S Smolen
Contributors: CK did literature research, designed the study, recruited patients, collected data, advised on data analysis, interpreted the data, and wrote and revised the report. JL advised on study design, planned the randomisation, and analysed and interpreted the data. JZ designed the study, recruited patients, collected data and revised the report. AW performed the randomisation and revised the report. FB recruited patients, collected data, advised on data analysis, advised interpreting data, and revised the report. NB recruited patients, collected data, advised on data analysis, advised interpreting data and revised the report. JCH recruited patients, collected data, advised on data analysis, advised on interpreting data and revised the report. JK recruited patients, collected data, advised on data analysis, advised on interpreting data and revised the report. AR-R recruited patients, collected data and revised the report. HS-K recruited patients, collected data, advised on data analysis, advised on interpreting data and revised the report. ES recruited patients, collected data and revised the report. CS recruited patients, collected data, advised on data analysis, advised on interpreting data and revised the report. EF did literature research, designed the study, recruited patients, collected data, advised on data analysis, interpreted the data, and wrote and revised the report.
Funding: This was an investigator-initiated trial sponsored by Novartis Pharma GmbH.
Competing interests: CK has received personal advisory board and congress fees from Novartis, Pfizer, Roche and Sobi. FB has received grants from Abbvie, Pfizer, Roche, Chugai and Janssen, and consultant, speaker or advisory board fees from Abbvie, Pfizer, Roche, Chugai, UCB, BMS, Celgene, MSD, Novartis, Biotest, Janssen, Genzyme and Lilly; Boehringer; and Sandoz. NB has received grants from Novartis and Sobi, and personal fees from Novartis, Sobi, Lilly, Pfizer, Abbvie, BMS, MSD, Actelion, UCB, Boehringer-Ingelheim and Roche. JCH has received grants from Novartis, Roche and Celgene, and advisory board and speaker fees from Novartis, Roche, Pfizer, Abbvie, Sanofi, Boehringer-Ingelheim and Celgene. AR-R has received speaker fees from UCB, and advisory board and speaker fees from Novartis, Roche, Lilly, Pfizer, Abbvie, BMS, Janssen, Sanofi and Celgene. CS has received personal fees from Abbvie, Boehringer-Ingelheim, Chugai, Lilly, Novartis, Sobi, UCB, Celgene, Janssen-Cilag, MSD, Pfizer, Roche, UCB and Toshiba. EF has received advisory board and speaker fees from Novartis, Roche, Sobi, Lilly, Pfizer, Abbvie, BMS, MSD and Sanofi.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Patient consent for publication: Not required.
Ethics approval: The study was conducted according to the ethical principles of the Declaration of Helsinki. The study protocol and all amendments were reviewed by the Independent Ethics Commission of the State of Berlin (Ethik-Kommission des Landes Berlin) and independent ethics committees for each centre (EudraCT number 2011-001027-20, protocol number CACZ885GDE01T, ethics number 11/0561–ZS EK 11).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the manuscript or available in supplemental
material. Complete data and raw data/datasets are saved in the Institution Server and are available upon request.
References
- 1. Aksentijevich I, McDermott MF. Lessons from characterization and treatment of the autoinflammatory syndromes. Curr Opin Rheumatol 2017;29:187–94. 10.1097/BOR.0000000000000362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hausmann JS. Targeting cytokines to treat autoinflammatory diseases. Clin Immunol 2019;206:23–32. 10.1016/j.clim.2018.10.016 [DOI] [PubMed] [Google Scholar]
- 3. Neven B, Prieur A-M, Quartier dit Maire P. Cryopyrinopathies: update on pathogenesis and treatment. Nat Clin Pract Rheumatol 2008;4:481–9. 10.1038/ncprheum0874 [DOI] [PubMed] [Google Scholar]
- 4. Tanaka T, Kishimoto T. Targeting interleukin-6: all the way to treat autoimmune and inflammatory diseases. Int J Biol Sci 2012;8:1227–36. 10.7150/ijbs.4666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yu JR, Leslie KS. Cryopyrin-associated periodic syndrome: an update on diagnosis and treatment response. Curr Allergy Asthma Rep 2011;11:12–20. 10.1007/s11882-010-0160-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bielak M, Husmann E, Weyandt N, et al. IL-6 blockade in systemic juvenile idiopathic arthritis - achievement of inactive disease and remission (data from the German AID-registry). Pediatr Rheumatol Online J 2018;16:22. 10.1186/s12969-018-0236-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. De Benedetti F, Brunner HI, Ruperto N, et al. Randomized trial of tocilizumab in systemic juvenile idiopathic arthritis. N Engl J Med 2012;367:2385–95. 10.1056/NEJMoa1112802 [DOI] [PubMed] [Google Scholar]
- 8. Giancane G, Minoia F, Davì S, et al. Il-1 inhibition in systemic juvenile idiopathic arthritis. Front Pharmacol 2016;7:467. 10.3389/fphar.2016.00467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Grevich S, Shenoi S. Update on the management of systemic juvenile idiopathic arthritis and role of IL-1 and IL-6 inhibition. Adolesc Health Med Ther 2017;8:125–35. 10.2147/AHMT.S109495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kearsley-Fleet L, Beresford MW, Davies R, et al. Short-term outcomes in patients with systemic juvenile idiopathic arthritis treated with either tocilizumab or anakinra. Rheumatology 2019;58:94–102. 10.1093/rheumatology/key262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lai JM, Wu FQ, Zhou ZX, et al. [Tocilizumab for refractory systemic juvenile idiopathic arthritis]. Zhonghua Er Ke Za Zhi 2017;55:830–4. 10.3760/cma.j.issn.0578-1310.2017.11.008 [DOI] [PubMed] [Google Scholar]
- 12. Nigrovic PA, Beukelman T, Tomlinson G, et al. Bayesian comparative effectiveness study of four consensus treatment plans for initial management of systemic juvenile idiopathic arthritis: first-line options for systemic juvenile idiopathic arthritis treatment (FROST). Clin Trials 2018;15:268–77. 10.1177/1740774518761367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ruperto N, Brunner HI, Quartier P, et al. Two randomized trials of canakinumab in systemic juvenile idiopathic arthritis. N Engl J Med 2012;367:2396–406. 10.1056/NEJMoa1205099 [DOI] [PubMed] [Google Scholar]
- 14. Ruperto N, Brunner HI, Quartier P, et al. Canakinumab in patients with systemic juvenile idiopathic arthritis and active systemic features: results from the 5-year long-term extension of the phase III pivotal trials. Ann Rheum Dis 2018;77:1710–9. 10.1136/annrheumdis-2018-213150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Saccomanno B, Tibaldi J, Minoia F, et al. Predictors of effectiveness of Anakinra in systemic juvenile idiopathic arthritis. J Rheumatol 2019;46:416–21. 10.3899/jrheum.180331 [DOI] [PubMed] [Google Scholar]
- 16. Tarp S, Amarilyo G, Foeldvari I, et al. Efficacy and safety of biological agents for systemic juvenile idiopathic arthritis: a systematic review and meta-analysis of randomized trials. Rheumatology 2016;55:669–79. 10.1093/rheumatology/kev382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Toplak N, Blazina Štefan, Avčin T. The role of IL-1 inhibition in systemic juvenile idiopathic arthritis: current status and future perspectives. Drug Des Devel Ther 2018;12:1633–43. 10.2147/DDDT.S114532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vastert SJ, Nigrovic PA. Editorial: toward personalized treatment for systemic juvenile idiopathic arthritis. Arthritis Rheumatol 2018;70:1172–4. 10.1002/art.40501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Woo P. Anakinra treatment for systemic juvenile idiopathic arthritis and adult onset still disease. Ann Rheum Dis 2008;67:281–2. 10.1136/ard.2007.082859 [DOI] [PubMed] [Google Scholar]
- 20. Yokota S, Itoh Y, Morio T, et al. Tocilizumab in systemic juvenile idiopathic arthritis in a real-world clinical setting: results from 1 year of postmarketing surveillance follow-up of 417 patients in Japan. Ann Rheum Dis 2016;75:1654–60. 10.1136/annrheumdis-2015-207818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yokota S, Tanaka T, Kishimoto T. Efficacy, safety and tolerability of tocilizumab in patients with systemic juvenile idiopathic arthritis. Ther Adv Musculoskelet Dis 2012;4:387–97. 10.1177/1759720X12455960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zou L, Lu M, Guo L, et al. [Efficacy and safety of humanized interleukin-6 receptor antibody in treatment of systemic juvenile idiopathic arthritis]. Zhejiang Da Xue Xue Bao Yi Xue Ban 2017;46:421–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cipriani P, Ruscitti P, Carubbi F, et al. Tocilizumab for the treatment of adult-onset still's disease: results from a case series. Clin Rheumatol 2014;33:49–55. 10.1007/s10067-013-2381-5 [DOI] [PubMed] [Google Scholar]
- 24. de Boysson H, Février J, Nicolle A, et al. Tocilizumab in the treatment of the adult-onset still's disease: current clinical evidence. Clin Rheumatol 2013;32:141–7. 10.1007/s10067-012-2105-2 [DOI] [PubMed] [Google Scholar]
- 25. Elkayam O, Jiries N, Dranitzki Z, et al. Tocilizumab in adult-onset still's disease: the Israeli experience. J Rheumatol 2014;41:244–7. 10.3899/jrheum.130881 [DOI] [PubMed] [Google Scholar]
- 26. Fitzgerald AA, Leclercq SA, Yan A, et al. Rapid responses to anakinra in patients with refractory adult-onset still's disease. Arthritis Rheum 2005;52:1794–803. 10.1002/art.21061 [DOI] [PubMed] [Google Scholar]
- 27. Jamilloux Y, Gerfaud-Valentin M, Henry T, et al. Treatment of adult-onset still's disease: a review. Ther Clin Risk Manag 2015;11:33–43. 10.2147/TCRM.S64951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kaneko Y, Kameda H, Ikeda K, et al. Tocilizumab in patients with adult-onset still's disease refractory to glucocorticoid treatment: a randomised, double-blind, placebo-controlled phase III trial. Ann Rheum Dis 2018;77:1720–9. 10.1136/annrheumdis-2018-213920 [DOI] [PubMed] [Google Scholar]
- 29. Kontzias A, Efthimiou P. The use of canakinumab, a novel IL-1β long-acting inhibitor, in refractory adult-onset still's disease. Semin Arthritis Rheum 2012;42:201–5. 10.1016/j.semarthrit.2012.03.004 [DOI] [PubMed] [Google Scholar]
- 30. Li T, Gu L, Wang X, et al. A pilot study on tocilizumab for treating refractory adult-onset still's disease. Sci Rep 2017;7:13477. 10.1038/s41598-017-13639-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ma Y, Wu M, Zhang X, et al. Efficacy and safety of tocilizumab with inhibition of interleukin-6 in adult-onset still's disease: a meta-analysis. Mod Rheumatol 2018;28:849–57. 10.1080/14397595.2017.1416924 [DOI] [PubMed] [Google Scholar]
- 32. Naumann L, Feist E, Natusch A, et al. IL1-receptor antagonist anakinra provides long-lasting efficacy in the treatment of refractory adult-onset still's disease. Ann Rheum Dis 2010;69:466–7. 10.1136/ard.2009.108068 [DOI] [PubMed] [Google Scholar]
- 33. Ortiz-Sanjuán F, Blanco R, Calvo-Rio V, et al. Efficacy of tocilizumab in conventional treatment-refractory adult-onset still's disease: multicenter retrospective open-label study of thirty-four patients. Arthritis Rheumatol 2014;66:1659–65. 10.1002/art.38398 [DOI] [PubMed] [Google Scholar]
- 34. Pouchot J, Arlet J-B. Biological treatment in adult-onset still's disease. Best Pract Res Clin Rheumatol 2012;26:477–87. 10.1016/j.berh.2012.07.002 [DOI] [PubMed] [Google Scholar]
- 35. Puéchal X, DeBandt M, Berthelot J-M, et al. Tocilizumab in refractory adult still's disease. Arthritis Care Res 2011;63:155–9. 10.1002/acr.20319 [DOI] [PubMed] [Google Scholar]
- 36. Vitale A, Cavalli G, Colafrancesco S, et al. Long-term Retention Rate of Anakinra in Adult Onset Still’s Disease and Predictive Factors for Treatment Response. Front Pharmacol 2019;10 10.3389/fphar.2019.00296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bywaters EG. Still's disease in the adult. Ann Rheum Dis 1971;30:121–33. 10.1136/ard.30.2.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jamilloux Y, Gerfaud-Valentin M, Martinon F, et al. Pathogenesis of adult-onset still's disease: new insights from the juvenile counterpart. Immunol Res 2015;61:53–62. 10.1007/s12026-014-8561-9 [DOI] [PubMed] [Google Scholar]
- 39. Feist E, Mitrovic S, Fautrel B. Mechanisms, biomarkers and targets for adult-onset still's disease. Nat Rev Rheumatol 2018;14:603–18. 10.1038/s41584-018-0081-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nirmala N, Brachat A, Feist E, et al. Gene-expression analysis of adult-onset still's disease and systemic juvenile idiopathic arthritis is consistent with a continuum of a single disease entity. Pediatr Rheumatol Online J 2015;13:50. 10.1186/s12969-015-0047-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Efthimiou P, Kadavath S, Mehta B. Life-threatening complications of adult-onset still's disease. Clin Rheumatol 2014;33:305–14. 10.1007/s10067-014-2487-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kádár J, Petrovicz E. Adult-onset still's disease. Best Pract Res Clin Rheumatol 2004;18:663–76. 10.1016/j.berh.2004.05.004 [DOI] [PubMed] [Google Scholar]
- 43. Feist E, Quartier P, Fautrel B, et al. Efficacy and safety of canakinumab in patients with still's disease: exposure-response analysis of pooled systemic juvenile idiopathic arthritis data by age groups. Clin Exp Rheumatol 2018;36:668–75. [PubMed] [Google Scholar]
- 44. Cavagna L, Caporali R, Epis O, et al. Infliximab in the treatment of adult still's disease refractory to conventional therapy. Clin Exp Rheumatol 2001;19:329–32. [PubMed] [Google Scholar]
- 45. Fautrel B, Sibilia J, Mariette X, et al. Tumour necrosis factor alpha blocking agents in refractory adult still's disease: an observational study of 20 cases. Ann Rheum Dis 2005;64:262–6. 10.1136/ard.2004.024026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Husni ME, Maier AL, Mease PJ, et al. Etanercept in the treatment of adult patients with still's disease. Arthritis Rheum 2002;46:1171–6. 10.1002/art.10231 [DOI] [PubMed] [Google Scholar]
- 47. Kaneko K, Kaburaki M, Muraoka S, et al. Exacerbation of adult-onset still's disease, possibly related to elevation of serum tumor necrosis factor-alpha after etanercept administration. Int J Rheum Dis 2010;13:e67–9. 10.1111/j.1756-185X.2010.01544.x [DOI] [PubMed] [Google Scholar]
- 48. Kiyonaga Y, Maeshima K, Imada C, et al. Steroid-sparing effects of etanercept in a patient with steroid-dependent adult-onset still's disease. Intern Med 2014;53:1209–13. 10.2169/internalmedicine.53.1488 [DOI] [PubMed] [Google Scholar]
- 49. Kraetsch HG, Rascu A, Kalden JR, et al. [Clinical course and prognostic parameters in adult-onset Still's syndrome. Own experience and review of the literature]. Med Klin 1997;92:705–11. 10.1007/bf03044666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gabay C, Fautrel B, Rech J, et al. Open-label, multicentre, dose-escalating phase II clinical trial on the safety and efficacy of tadekinig alfa (IL-18BP) in adult-onset still's disease. Ann Rheum Dis 2018;77:840–7. 10.1136/annrheumdis-2017-212608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Atkinson AC. Optimum biased coin designs for sequential clinical trials with prognostic factors. Biometrika 1982;69:61–7. 10.1093/biomet/69.1.61 [DOI] [Google Scholar]
- 52. Ruperto N, Quartier P, Wulffraat N, et al. 2.2 a phase II trial with canakinumab, a new IL-1beta blocking monoclonal antibody (ACZ885), to evaluate preliminary dosing, safety and efficacy profile in children with systemic juvenile idiopathic arthritis (sJIA). Pediatric Rheumatology 2008;6:S2–S. 10.1186/1546-0096-6-S1-S2 [DOI] [Google Scholar]
- 53. Ruperto N, Quartier P, Wulffraat N, et al. A phase II, multicenter, open-label study evaluating dosing and preliminary safety and efficacy of canakinumab in systemic juvenile idiopathic arthritis with active systemic features. Arthritis Rheum 2012;64:557–67. 10.1002/art.33342 [DOI] [PubMed] [Google Scholar]
- 54. World Medical Association Declaration of Helsinki Ethical principles for medical research involving human subjects. JAMA 2013;310:2191–4. [DOI] [PubMed] [Google Scholar]
- 55. Yamaguchi M, Ohta A, Tsunematsu T, et al. Preliminary criteria for classification of adult still's disease. J Rheumatol 1992;19:424–30. [PubMed] [Google Scholar]
- 56. Lovell DJ, Giannini EH, Reiff AO, et al. Long-term safety and efficacy of rilonacept in patients with systemic juvenile idiopathic arthritis. Arthritis Rheum 2013;65:2486–96. 10.1002/art.38042 [DOI] [PubMed] [Google Scholar]
- 57. Kedor C. YVS.01 Canakinumab for treatment of adult onset Still‘s disease to achieve reduction of arthritic manifestation at week 12: a Multi-Centre, Placebo-Controlled Study (CONSIDER). 47 Kongress der Deutschen Gesellschaft für Rheumatologie; 2019.
- 58. Kedor C, Listing J, Zernicke J, et al. THU0561 Canakinumab for the treatment of adult onset still's disease to achieve reduction of arthritic manifestation at week 12: an investigator-initiated mu;ti-centre placebo-controlled study (CONSIDER). Ann Rheum Dis 2019;78:570–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Pouchot J, Sampalis JS, Beaudet F, et al. Adult Still's disease: manifestations, disease course, and outcome in 62 patients. Medicine 1991;70:118–36. [PubMed] [Google Scholar]
- 60. Rau M, Schiller M, Krienke S, et al. Clinical manifestations but not cytokine profiles differentiate adult-onset still's disease and sepsis. J Rheumatol 2010;37:2369–76. 10.3899/jrheum.100247 [DOI] [PubMed] [Google Scholar]
- 61. Ruscitti P, Cipriani P, Masedu F, et al. Adult-onset still's disease: evaluation of prognostic tools and validation of the systemic score by analysis of 100 cases from three centers. BMC Med 2016;14:194. 10.1186/s12916-016-0738-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Piram M, Koné-Paut I, Lachmann HJ, et al. Validation of the auto-inflammatory diseases activity index (AIDAI) for hereditary recurrent fever syndromes. Ann Rheum Dis 2014;73:2168–73. 10.1136/annrheumdis-2013-203666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Castañeda S, Atienza-Mateo B, Martín-Varillas JL, et al. Anakinra for the treatment of adult-onset still's disease. Expert Rev Clin Immunol 2018;14:979–92. 10.1080/1744666X.2018.1536548 [DOI] [PubMed] [Google Scholar]
- 64. Castañeda S, Blanco R, González-Gay MA. Adult-onset still's disease: advances in the treatment. Best Pract Res Clin Rheumatol 2016;30:222–38. 10.1016/j.berh.2016.08.003 [DOI] [PubMed] [Google Scholar]
- 65. Kadavath S, Efthimiou P. Adult-onset Still's disease-pathogenesis, clinical manifestations, and new treatment options. Ann Med 2015;47:6–14. 10.3109/07853890.2014.971052 [DOI] [PubMed] [Google Scholar]
- 66. Maria ATJ, Le Quellec A, Jorgensen C, et al. Adult onset still's disease (AOSD) in the era of biologic therapies: dichotomous view for cytokine and clinical expressions. Autoimmun Rev 2014;13:1149–59. 10.1016/j.autrev.2014.08.032 [DOI] [PubMed] [Google Scholar]
- 67. Nordström D, Knight A, Luukkainen R, et al. Beneficial effect of interleukin 1 inhibition with anakinra in adult-onset still's disease. an open, randomized, multicenter study. J Rheumatol 2012;39:2008–11. 10.3899/jrheum.111549 [DOI] [PubMed] [Google Scholar]
- 68. Wang C-Y, Guo S-H, Wang L-P, et al. Refractory adult-onset still disease treated by tocilizumab combined with methotrexate: a STROBE-compliant article. Medicine 2019;98:e16682. 10.1097/MD.0000000000016682 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
annrheumdis-2020-217155supp001.pdf (682.6KB, pdf)