Abstract
The practice of community pharmacy in low and middle-income countries, including in Indonesia, is often described as in the state of infancy with several intractable barriers that have been substantially and continuously hampering the practice. Such description might be valid in highlighting how pharmacy is practiced and the conditions within and beyond community pharmacy organizations. Therefore, it is not surprising that the concept of integrating community pharmacy into the primary care system may not be considered in the contemporary discourse despite the fact that community pharmacy has been operating within communities for years. However, in the case of Indonesia, we argue that changes in the health care system within the past decade particularly with the introduction of the universal health coverage (UHC) in 2014, may have significantly amplified the role of pharmacists. There is good evidence which highlights the contribution of pharmacist as a substantial health care element in primary care practice. The initiative for employing pharmacist, identified in this article as primary care pharmacist, in the setting of community health center [puskesmas] and the introduction of affiliated or contracted community pharmacy under the UHC have enabled pharmacist to work together with other primary care providers. Moreover, government agenda under the “Smart Use of Medicines” program [Gema Cermat] recognizes pharmacists as the agent of change for improving the rational use of medicines in the community. Community pharmacy is developing, albeit slowly, and is able to grasp a novel position to deliver pharmacy-related primary care services to the general public through new services, for example drug monitoring and home care. Nevertheless, integrating community pharmacy into primary care is relatively a new notion in the Indonesian setting, and is a challenging process given the presence of barriers in the macro, meso- and micro-level of practice.
Keywords: Pharmacies; Primary Health Care; Delivery of Health Care, Integrated; ; Ambulatory Care; Community Health Services; Pharmacists; Community Pharmacy Services; Professional Practice; Indonesia
INTRODUCTION
The Indonesian health care and primary care system
Indonesia is one of the largest archipelagic countries in the world comprising 17,504 islands stretching in an area between two oceans (the Pacific and Indian oceans) with three different time zones and connecting two continents (Asia and Australia).1 It has a population of approximately 267 million people representing more than 300 ethnicities with 700 local languages and dialects blending in with expatriates from numerous nationalities making it the fourth most populous country in the world.2,3 The geographic and demographic size of Indonesia presents major barriers, including to health care delivery.
Indonesia remains saddled with a huge burden of a number of communicable tropical diseases – some of which are classified by the World Health Organization (WHO) as neglected tropical diseases – such as dengue, malaria, filariasis, leprosy, schistosomiasis, soil-transmitted helminths and yaws.4 The list is not exhaustive with the inclusion of tuberculosis, lower respiratory infections and diarrheal diseases which often sits in the top ten causes of mortalities.3 Although the overall trend is a steadily decreasing number, the persistent presence of communicable diseases has been an ongoing challenge for any government ruling the country.
Within the past two decades, major noncommunicable diseases related to several risk factors such as tobacco smoking, obesity, unhealthy diet, physical inactivity and high blood pressure have shifted the trend of disease burden in Indonesia.5 For instance, a study in 2015 estimated that the morbidity of smoking-related diseases accounted for almost one million cases, about 21.6% of total cases of chronic diseases in Indonesia, with the treatment cost was estimated at least US$2,177 million, approximately 2.5% of the 2015 gross domestic product (GDP).6 Chronic diseases such as ischemic heart disease, stroke, diabetes, hypertension and cancer remain the top cause of health loss and disabilities among Indonesians.7
The prominent “double burden” of persistent communicable diseases and increasing noncommunicable diseases has resulted in a huge cost for the country to maintain the health care sector. It was reported that nominal health spending had been steadily increasing within the past decade by 222% overall.8 This has created a pressure on Indonesia’s health expenditure which remains on the level of 3% of the GDP despite the mandate of Health Law 2009 stating that 5% of the national budget must be attributed to the health sector.9 Health expenditure was reported at USD 125 per capita in 2018, which was the lowest among Low Middle-Income Countries (LMICs) and particularly within the developing Southeast Asian countries.1,3,10
The country also faces a critical shortage of health care workers and facilities. As of 2019, Indonesia only had 0.4 physicians and 1.3 nurses per 1,000 people.11 This is exacerbated by the uneven distribution of these workers, with the majority (67%) being located in Java Island – the most heavily populated island in the country.11 Whilst the number of health facilities has nearly doubled within the past two decades, reaching 2,877 hospitals and 10,134 government-financed community health center [Puskesmas] in 2019, maldistribution and underperformance of these facilities have been evident, leading to a serious problem of accessing health care in the rural and suburban areas.11
Puskesmas and their auxiliary network in the district level are among the frontline primary care providers along with the private sector which is dominated by individual practice such as general practitioners, nurses, midwives and a range of private clinics.8 Although puskesmas has been playing a vital role in providing promotive, preventive, curative services in a range of areas including maternal and child health, family planning, communicable disease, community nutrition and environmental health, their role has been underutilized. Its role remains marginalized with some fractions of the community still perceive that “puskesmas is for the poor and private practice is for the rich”.12
The performance of puskesmas arguably has improved after an accreditation system was implemented in 2015.13 Nevertheless, their functioning has been highly variable, and huge disparities have been noted among districts. Some puskesmas perform well, but the remaining facilities face various issues, including inadequate staffing, inability to provide basic care and poor relationships with the communities.8,14 The decentralization system partly contributes to this disparity.15 With the greater authority of the local head of the government at the district level, the functioning of puskesmas heavily relies on the district funding and commitment from the local leaders, leading to puskesmas in several districts suffering from poor functioning due to insufficient district funding, or shifted agendas and priorities from the district leaders.16-18
The introduction of Universal Health Coverage
Despite the intractable and persistent problems in the health care system and its delivery, the Indonesian government has made a significant investment over the years, aiming to improve the health care environment and funding. An ambitious program was set, i.e. Universal health coverage (UHC) for all Indonesians by 2019 in light of the United Nations (UN) Sustainable Development Goals (SDGs) 2030.19 The UHC program was firstly designed in 2004, yet, hampered by the political and financial circumstances of the nation, it took ten years for the program to be finally introduced in 2014.20 The UHC, on the one hand, has been viewed as a promising initiative to finance the health care sector, improve health equity and accessibility of health services.1 It has been claimed to having features of protecting Indonesians from catastrophic payments for health care.21 On the other hand, concern was raised over how the country would be able to continuously fund the scheme, given the complexity and diversity of resources and conditions in Indonesia.22 Despite this discourse, the UHC program continues to grow and becomes a large single-payer scheme as it has covered roughly 90% of the population by the end of March 2020.
UHC is a game-changer for Indonesian health care. The program has changed the landscape of health care which was originally fragmented with private health insurance – provided only for those who could afford – and government insurance for a small portion of the population – mainly government workers, police and military, and very poor or vulnerable people – into a single national health insurance system.23 The universal coverage system provides major benefits for Indonesians, particularly for covering the cost of medical bills for most diseases and health problems. As predicted, however, the program has a severe funding deficit every year. It is estimated that there will be a USD 2 billion (IDR 26 trillion) cash shortfall by the end of 2020, which may grow double by the end of 2025.1 One of the contributing factors for this deficit is the low compliance in paying for the monthly insurance payment, particularly among the informal sector workers, which constituted 37% of the UHC members.24 As a consequence, the government increased the payment package on May 2020 leading to a heated debate given that such initiative was previously annulled by the Supreme Court roughly two months before the policy was revoked.25,26
The UHC has transformed the referral system of health care. Previously any patient was able to go directly to hospitals or specialists when seeking medical help without referral even for minor cases. Staged referral mechanism has now been put in place between the three tiers of care: primary, secondary and tertiary care, with puskesmas as the gatekeeper for higher levels of care.8 What might be relevant to pharmacy practice is that the UHC has opened up new opportunities for pharmacist involvement in primary care, which will be explained in the subsequent section.
CONTEMPORARY COMMUNITY PHARMACY PRACTICE IN INDONESIA
Overview
Community pharmacy services in Indonesia exist in public and private health sectors. Pharmacists in the public sector work in puskesmas are employed by the government, in this article they are referred to as primary care pharmacist. Unlike the public sector, pharmacists in the community pharmacy are generally private practitioners, in this article referred to as community pharmacist. The income of private community pharmacy is largely derived from the sales of medicines and other products. Additional services, such as consultation and prescription review, are often not remunerated. Also, the pharmacy owner determines the income of individual pharmacists if the pharmacists do not own the pharmacy. Ownership of pharmacy is open to anyone leading to a significant portion of pharmacies (roughly 70%) being owned by non-pharmacist.27,28 However, a pharmacy cannot be opened without the pharmacist. Each pharmacy must, therefore, employ a minimum of one pharmacist to be in charge of the operation of the pharmacy.
In 2019, there were approximately 30,000 community pharmacies employing approximately 62,000 pharmacy personnel, including pharmacist and pharmacy support workforce, which represents one of the largest health care settings in the country.11 In addition, community pharmacy is among the most accessible and frequently used health care facilities. It operates within the heart of the communities, with more than 90% of the population having visited community pharmacy.29 Moreover, clients do not need to spend a long time queuing, and most pharmacies open seven days in a week with nearly 15 hours of operation per day.30
Community pharmacists in Indonesia contribute to health care through the delivery of medicines and health-related products and services either independently or in collaboration with other primary care members, particularly General Practitioners (GPs).31-33 Dispensing has been the predominant activities in community pharmacy.34-36 However, the sale of over the counter medications and practice consultations are also common with pharmacist plays a role in providing advice and assistance for self-medication. These features might imply that community pharmacies are strategically placed and can offer a unique role to relieve strains on the health care system and reduce the over-reliance on the major primary care providers, e.g. GPs and the hospital admissions by operating at their full scope of practice.
There are two main legislations underpin pharmacy practice in Indonesia: the President Regulation number 51 of 2009 (Pharmacy Practice Act of 2009) and the Minister of Health (MoH) Regulation number 9 of 2017 (Community Pharmacy Decree of 2017).37,38 The Pharmacy Practice Act provides the main policy framework ensuring that pharmacists have the solely responsibility for conducting pharmacy practice, including in puskesmas and community pharmacy. More importantly, the Act defines the scope of practice of pharmacist from the planning and procurement of pharmaceutical products to activities ensuring the use of quality medicines for the patients and communities. The Community Pharmacy Decree, on the other hands, regulates specific features of community pharmacy operation such as premise, ownership, pharmacy location, workforce and provision of services which align with the standards governing pharmacy services.
The MoH has issued standards for pharmacy services at the community pharmacy (under the MoH Regulation Number 73 of 2016) and puskesmas level (under the MoH Regulation Number 74 of 2016), respectively.39,40 These standards are intended to serve as a basic guide for the provision of pharmacy services; outlining the minimum level of services that should be consistently delivered by the pharmacist in each setting. In these standards, pharmacists are encouraged to provide two elements of services namely (1) the supply and management of pharmaceuticals, health devices and other medical products and (2) clinical pharmacy services (Table 1). While the implementation might vary across sites, these standards have set the baseline for any pharmacist - related activities.
Table 1. The difference in pharmacy practice standard across sites.
| Pharmacy Practice Standard | Community Pharmacy39 | Community health center [puskesmas]40 | Hospital41 |
|---|---|---|---|
| Supply and management of pharmaceuticals, health devices and other medical products | |||
| Selection | √ | ||
| Planning process | √ | √ | √ |
| Procurement | √ | √ | √ |
| Receiving process | √ | √ | √ |
| Storage | √ | √ | √ |
| Distribution | √ | √ | |
| Recall | √ | ||
| Disposal | √ | √ | |
| Controlling | √ | √ | √ |
| Documentation | √ | ||
| Administration | √ | √ | √ |
| Report | √ | √ | |
| Monitoring and evaluation | √ | ||
| Clinical pharmacy services | |||
| Prescription assessment | √ | √ | √ |
| Medication reconciliation | √ | ||
| Drug information center | √ | √ | √ |
| Dispensing | √ | √ | √ |
| Counselling | √ | √ | √ |
| Independent ward round or collaboration ward round | √ (specific for inpatient care) | √ | |
| Drug therapeutic assessment | √ | √ | √ |
| Monitoring of medication side effect | √ | √ | √ |
| Drug use evaluation | √ | √ | |
| Aseptic dispensing | √ | ||
| Therapeutic drug monitoring (TDM) | √ | ||
| Home pharmacy care | √ | √ | |
| √ available in this setting | |||
Integration of community pharmacy into the primary care system
Recognizing the potential of pharmacist in primary care particularly in the era of UHC, the government has introduced three scenarios for pharmacist integration within the primary care system. First, community pharmacy has now had the opportunity to become part of a network of primary care providers under the contractual agreement with the prescribers or the UHC insurance agency.23 Second, as aforementioned, the allocation of pharmacists at puskesmas which was virtually nonexistent prior to UHC.23 Third, the “Gema Cermat” program – a national campaign aimed at improving awareness and rational use of medicines – has been launched with pharmacist holds the key player for delivery of the program.42
Under the UHC, community pharmacy can opt for any of the three models: as a pharmacy affiliated with a network of primary care provider (affiliated pharmacy), as a pharmacy commissioned for providing back referral program (contracted pharmacy), or both.23 An affiliated pharmacy works in partnership with other primary care providers, particularly GPs, dentists and clinics. These community pharmacies are responsible for supplying pharmaceuticals and providing services for patients taken care of by the network. The pharmacy is reimbursed for pharmaceuticals based on the electronic catalogue (e-catalogue) pricing system. In addition, the pharmacy fee for dispensing the medicine is negotiated with the network based on the proportion of capitation payment for treating each individual patient. Each network receives capitation payment ranges from IDR 8,000 to 10,000 (less than USD 1) per patient, and ideally, this should be distributed within the network, including pharmacy.43
A contracted pharmacy is only responsible for providing services and pharmaceuticals for patients following hospital discharge. At the time of discharge, the patient can collect their discharge prescription either at puskesmas or at the contracted pharmacy. In this manner, the patient can continue to receive their medication for up to 30 days and consultation from the pharmacist for any medication problems. However, this service is only available for patients with certain chronic diseases, including hypertension, diabetes mellitus, heart failure, chronic obstructive pulmonary disease, stroke, asthma, epilepsy, schizophrenia, and systemic lupus erythematosus.44 Community pharmacy under this scheme is reimbursed for the pharmaceuticals based on the e-catalogue pricing and the dispensing fee is paid using the formula on Table 2. For example, if a pharmacy dispensed a medicine which costs IDR 50,000, they would receive IDR 13,000 for the dispensing fee. Please note that this fee is paid for the pharmacy and not the pharmacist.
Table 2. Dispensing fee for pharmacy under the contracted scheme43.
| Drug price on e-catalogue system (IDR) | Coefficient for dispensing fee |
|---|---|
| < 50,000 | 0.28 |
| 50,000 – 250,000 | 0.26 |
| 250,000 – 500,000 | 0.16 |
| 1,000,000 – 5,000,000 | 0.11 |
| 5,000,000 – 10,000,000 | 0.09 |
| > 10,000,000 | 0.07 |
| (USD1 equals to IDR 14,000 as of June 2020) | |
It was reported that only less than 9% of community pharmacies have participated in the UHC scheme, with the large portion of the remaining is independent of it.45 The number was even smaller for contracted pharmacy as there are only 469 contracted pharmacies across the country in 2020, representing less than 2% of the total community pharmacy population.45 Factors contributing to the low participation of pharmacy has been mixed and anecdotal. On the one hand, the BPJS Health – the insurance agency responsible for organizing UHC – claimed that the low participation had been associated with the uneven distribution of pharmacy, making it difficult to recruit more pharmacies in an area in which ratio between pharmacy and population has not been met. On the other hand, pharmacies, which were not willing to participate or those who already discontinued their affiliation, complained about the late payments which may take several months after submitting the claims.46,47
The allocation of primary care pharmacist in puskesmas cannot be separated from the MoH Regulation number 46 of 2015 concerning puskesmas accreditation which states pharmacy service as an essential part of puskesmas operation.13,40 Such allocation is critical because prior to 2014, pharmacy practice in puskesmas was mainly provided by non-pharmacists i.e. other health care professionals. The regulation mandates that every puskesmas needs to have at least one pharmacist as the pharmacist in charge. The pharmacist in charge is responsible for the operation of the pharmacy unit and the provision of pharmacy services. The regulation also specifies a ratio for pharmacists to patients of 1:50 for outpatient services and 1:30 for inpatient services. This regulation has enabled puskesmas to have more flexibility in recruiting pharmacists, either on a contractual basis or in a permanent position as a government official. The pharmacist receives a fixed monthly salary from the government and other incentives to top up their income. The incentives may include dispensing fee following to the formula on Table 2, an income from the portion of capitation payment which ranges from IDR 3,000 to IDR 6,000 (less than USD 0.5) per patient paid to puskesmas and other sources of income funded by the district government such as merit reward and incentive for delivering health campaign which may vary between Puskesmas.43
The involvement of pharmacists in puskesmas allows for collaboration with other primary care providers within puskesmas. For example, pharmacists can assess medication appropriateness, ensure the safety, efficacy and adherence to medication, as well as provide recommendations to the other providers (Table 1). In addition, pharmacists’ role in puskesmas can also include the delivery of home care pharmacy programs and public health campaigns to the general public. The degree of pharmacist’s involvement and collaboration, however, may vary across puskesmas, depending on their workload, given that most puskesmas have only one pharmacist in charge of providing a service to roughly 300 patients per day.48,49
Another scenario for pharmacist involvement in primary care both for community and primary care pharmacist is through the “Gema Cermat” (smart use of medicines campaign) program. However, unlike the other two scenarios, “Gema Cermat” which was launched in 2015, in principle is a campaign program to improve the community awareness in using medicines.50 The campaign has been recruiting pharmacist as the trainer of the program conveying public educational message regarding self-management and rational use of medicines. The program uses the jargon of “DAGUSIBU”, an acronym from words of DApatkan (to obtain), GUnakan (to use), SImpan (to keep) and BUang (to dispose of) medication properly. The pharmacist has been participating in the program actively, conducting several public education activities within and beyond the community pharmacy settings including at the schools, community gatherings and other public spots.51
The funding for “Gema Cermat” program is shared between the MoH and the provincial or district health offices. There is limited information about the amount and proportion of each party on financing the program. This also implies a lack of information regarding remuneration received by individual community pharmacy joining the program. Nevertheless, there is evidence on the positive impact of the program on improving public knowledge and attitude in using medicines as well as increased recognition towards pharmacist existence.35,52 However, whether the program has been successfully translated into sustainable practice and eventually changed the way the public properly use the medicines remains unknown. The fact that most of the activities of the program are one-off campaign, knowledge-based rather than practice-focused, and do not necessarily correlate with the pharmacy services may highlight challenges for its effectiveness in daily practice.42,53,54 Additionally, due to the decentralization system, the evaluation of the “Gema Cermat’ implementation has been heavily relied on the commitment of the provincial or district health offices, with few attention has been put towards systematic nationwide evaluation efforts.
STAKEHOLDERS IN INDONESIAN COMMUNITY PHARMACY SECTOR
Many different actors form the community pharmacy sector in Indonesia (Figure 1). Community pharmacy operates in a highly regulated environment with regulatory function is formally set up by the Ministry of Health (MoH). One of the current initiatives by the MoH to leverage community pharmacy practice is to promote the use of electronic pharmacy (e-pharmacy) system.55 This will allow a licensed community pharmacy to go digital and online with medicines can be delivered to the patient via a courier. Another influential institution is the National Agency of Drug and Food Control (BPOM) with its auxiliary network at the provincial level. The BPOM plays a regulatory and supervisory role for drugs and food products marketed in Indonesia. This includes conducting inspection and monitoring to pharmacy outlets and their facilities.
Figure 1. Stakeholders in Indonesian Community Pharmacy Sector.
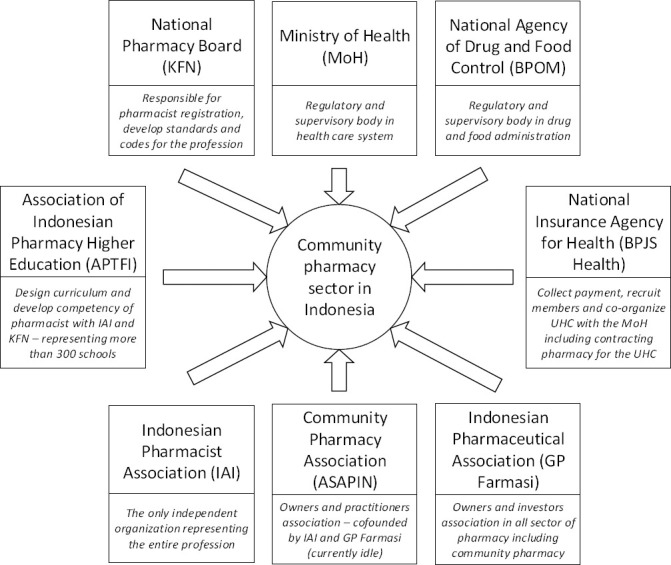
In the context of professional practice, the Indonesian Pharmacist Association (IAI) is the largest association of pharmacists in Indonesia. It is the solely responsible organization representing and advancing the profession of pharmacist. The IAI sets the standard of practice for pharmacist and continuously strengthen the profession through five pillars of action (Table 3).56
Table 3. Summary of the five pillars of action for strengthening the profession.
| Pillar 1. Advocating the philosophy of the responsible and professional practice of pharmacist |
| The strategic position of pharmacist for public health must be preserved by delivering practice that is not only professional but also responsible. The responsible practice reflects pharmacist integrity, including moral and ethical value and becomes sensible to public health issues. The IAI ensures this approach by investing on a certification program for pharmacists, initiating credit system for licensure and re-certification, creating pharmacist group of interest – including the group of community pharmacist and the Young Pharmacist Group (YPG), and series of activities focusing on the mentoring, coaching and advocacy program for pharmacists. |
| Pillar 2. Improving the good governance of the organization |
| As the solely responsible organization representing the pharmacist profession, the IAI strives to provide benefits for the member and maintain good governance of the organization, including the management of financials, assets and human resources. With respect to this strategy, IAI introduces leadership training for the member, sets up accountability measures for the good management of the organization including audit for the financials, builds an expert group as advisor to the organization, and assigns three main area coordinators following to the geographical division of the country (western, central and eastern coordinator) for handling issues in the management of IAI at the local level. |
| Pillar 3. Enhancing pharmacist recognition and acceptance |
| The profession of the pharmacist has been known for its role in the supply of medicine. However, there is a lack of awareness from the public and other health professionals regarding pharmacist potentials beyond dispensing medication, particularly on the public health and clinical related issues. The IAI enhances pharmacist recognition through partnership and networking with other stakeholders within and beyond health care sector, rebranding the image of the profession by introducing a policy on pharmacist wearing a coat and name badge during practice, signboard for pharmacist name and practice hours and invites members to involve in the IAI and MoH campaign events such as Gema Cermat and disaster responses. |
| Pillar 4. Contributing to pharmacy education development and practice transformation |
| The IAI understands that education is an essential element to change practice and therefore, strategic action towards improving the quality of education and transforming practice must be prioritized. IAI facilitates continuing professional education for pharmacist, promotes research-based evidence and the use of digital and information technology in practice by developing a division for research and digitalization of practice, sets up a new platform for facilitating pharmacist continuing education, activity management, membership administration and documentation, called as “SIAP [Sistem Informasi Apoteker] (Pharmacist Information System)”.57 |
| Pillar 5. Actively involved in the policymaking and legislation |
| Pharmacists are an established profession in the health sector. The scope of practice of pharmacists and the legal position of pharmacists have been acknowledged in the Indonesian regulation and legislation. Nevertheless, challenges regarding pharmacist role and authority, including ethical dilemma and lawsuits involving pharmacist often occurs. The IAI implements this pillar by actively involved in the legislation making at the national and local level. One of the regulations that was promoted by the IAI and is currently being drafted at the national parliament level is the Omnibus Law on Pharmacy, which will become the overarching law governing pharmacy sector in Indonesia, including community pharmacy practice.58 In addition, IAI protects and supports the member through advocacy, providing legal assistance and mediation for those who need it. |
The pillars are short-term action introduced by the National Committee of the IAI serving period of 2018-2022. It was formed in 2018 in response to the changing landscape of pharmacy and health care sector after the introduction of the UHC, which at the same time has presented both opportunities and challenges for the profession. The pillars are implemented at all level of the organization focusing on the commitment of pharmacist member to change and to work at their full capacity with integrity for the public health.
CHALLENGES OF PHARMACY SERVICES DELIVERY
Several challenges are hampering the sustainability of pharmacy services delivery in the primary care setting in Indonesia, which should be considered and addressed in the future. These challenges range from macro-level, meso-level, and micro-level.59,60
The macro-level challenges include the legal, regulatory and economic barriers of pharmacy services as part of the health care system. In the Indonesian context, the health system constraints include lack of recognition and decisive supports from the health authorities, absence of funding supporting pharmacy viability, and lack of investment in the pharmaceutical supply chain leading to some events of pharmaceutical shortages.61-63 Apart from the health system constraints, the poor coverage of pharmacy participation in the UHC scheme is another challenge in this level. This, in turn, has limited client’s access to services covered by their JKN insurance scheme. Also, poor law enforcement mechanisms happen at the root level. For example, there is a regulation that antibiotics can only be dispensed by pharmacists with a prescription.37 However, several studies have noted that a significant percentage of pharmacies in the country dispensed antibiotics without prescription.64-66 Lack of monitoring mechanism and poor law enforcement from the district government, due to the insufficient human resources or financial constraints have exacerbated this situation.8 The absence of community pharmacy accreditation and poor remuneration system for pharmacy services are also among the factors hindering the sustainability of pharmacy service delivery.51
The meso-level challenges include the organizational and cultural barriers of pharmacy services and the determination of the level and quality of services provided by community pharmacies.67 Community pharmacies operate in a dynamic environment. To remain competitive, they should be able to adapt to service implementation. However, the traditional culture of community pharmacy which has predominantly been focused on dispensing has, in some way, resulted in unpreparedness and inability of community pharmacy to, for example, adopt and adapt new technology and informational system.68
The UHC arguably has improved the access of the public to health care. However, it may also bring consequence to overcrowding in puskesmas due to an increased number of daily visits by patients. The excessive workload for all health professionals is inevitable with a pharmacist is arguably worst affected by this situation.69 Only less than half of puskesmas (4,986 puskesmas) are equipped with pharmacist reflecting that there are still major imbalances and gaps in the availability and distribution of pharmacist across puskesmas.11 The high workload experienced by primary care pharmacists has been evident, often due to understaffing, and the need to deal with many administrative and technical tasks.23,61,70 Lack of performance indicators to assess the quality of services provided is also among the challenges.71 Despite the health reform in the Indonesian health systems, which regulates pharmacy’s roles in the primary care network, few formal performance indicators are available to monitor the implementation of these roles. This situation challenges the comparison of pharmacy performance across districts and poses difficulties in evaluating the implementation of health reform.
The micro-level challenge includes the capacity of individual pharmacists themselves. Community pharmacists typically work in a silo within the walls of pharmacy. The problem arises when there is a need for interprofessional collaboration which requires communication and teamwork skills. In addition to the lack of interprofessional skills, individual pharmacists have often had a lack of knowledge in particular topics and lack of individual confidence, which affects the variety of service provision to the patients.61,72 A shortcoming in the graduate’s competence themselves could also be one of the causes of the lack of pharmacists’ competency.23 Other obstacles from the individual pharmacists relate to the poor motivation from the pharmacist to be more involved in patient care, to adopt new roles and to participate in Continuing Professional Development (CPD) program.30,62,73
WAY FORWARD
Health inequalities and inequitable access to health care have been a concern in many parts of Indonesia, affecting a significant portion of the populations, particularly those living in rural and remote areas. Decentralization policy has been introduced to address this issue; however, its implementation varies across districts, challenging its ability to address health care inequality at the local level. We argue that increasing access to community pharmacy and pharmacist network might assist in addressing this challenge.
Community pharmacy has been a stronghold for the general public to obtain medication.74-76 Besides, the current policy under the UHC has been a steppingstone for the pharmacist to involve in the primary care system. There is a nexus between pharmacy services and other health services; therefore, an expansion of pharmacist’s roles in partnership with the GPs and other health professionals might be promoted as a new model of comprehensive care, in the prevention, service integration and continuity of care within the system.
There has been a lack of attention to the role of the community pharmacist in the prevention and early intervention. There is only a small portion of pharmacies providing health screening services, such as blood pressure monitoring, blood glucose level measurement, cholesterol and uric acid check as an adjunct to dispensing services, may highlight the potential venue for early intervention.29 Particularly in Indonesia, this is not yet the norm of contemporary pharmacy practice and might be introduced in the future once the public trust to the role of pharmacists in providing health and medicine information is high.77
Service integration can be implemented in various activities, including medication reviews and pharmacovigilance. Community pharmacist can be appropriately positioned to review and monitor the use of medicines. In fact, pharmacovigilance has been an emerging role for primary care pharmacist to tackle misuse and abuse of medicines, including the opportunity for antimicrobial resistance surveillance.78,79 Also, due to the unique position of community pharmacies as the first point of contact to the health care system, they can help in providing information on the trend of medicine purchased or dispensed at the community level over time, thus providing us with critical early warning system in the event of a disease outbreak.80
Whilst the UHC offers a promising pathway for community pharmacy to provide continuity of care for patients at hospital discharge under the contracted pharmacy scheme, the small number of community pharmacies involved in the program has limited the program effectiveness. The role of pharmacists in providing care on discharged medication can be improved by strategically recruiting more contracted pharmacies. Additionally, continuity of care can be effectively delivered using Information and Communication Technology (ICT) system, one of which through developing patient Electronic Health Record (EHR) and shared databases.81 Although the implementation of EHR is common in most hospitals and puskesmas, it has not facilitated data sharing between organizations and across the three tiers of care. A strategy to facilitate this data sharing would be a way to move forward to ensure all patients EHR are safe and kept sustainably.
Since the integration of pharmacists and their services into primary care is essential, community pharmacist must be equipped and trained to keep up with the expanded services. Indeed, expanding clinical skills and expertise of pharmacist can contribute to the significant impact on the health of Indonesians. New roles and services of pharmacists, including therapeutic outcome monitoring and primary disease prevention as aforementioned, suggest that pharmacists are important stakeholders to contribute to the provision of care through encouraging a healthy lifestyle, preventing disease, and contribute to better therapeutic outcomes to the population.32 This opportunity means that pharmacists need to advance their practice and maintain a high standard of practice throughout careers to assure the quality of health service delivery.
Pharmacy education in Indonesia has reacted to adapt their curricula to prepare pharmacy students entering their practice. Changes to the curricula were firstly brought into discussion through the Health Professional Education Quality (HPEQ) Project initiated by the Ministry of Education in 2010.82 The aim was to transform the curricula which was predominantly pharmaceutical science based into problem-based curricula which promotes skill development and clinical knowledge. However, the most significant change in the education is the introduction of competency examination.
The exam was firstly designed in 2013, pilotted in 2015, but it was finally implemented in 2017. The exam consists of of two types of test: the Computer Based Test (CBT) with an emphasis on knowledge test and Observed Structured Clinical Examination (OSCE) on skill test.83 Passing the exam is a requirement for prospective pharmacist to obtain competency certificate prior to registration. The number of students undertaking the exam has been fluctuative every year with the portion of students passed the exam at the first trial tended to decrease.84 On the one hand, this indicates an improvement on the difficulty and quality of the assessment. However, on the other hand, this also highlights a gap in the quality of education across fifty schools of pharmacy which are eligible to deliver pharmacist program - these are the accredited A and B schools which conduct four years bachelor program and one year pre-pharmacist program.
The failure to pass the exam would also affect to students’ motivation and financials as they have to wait longer to get their first job as pharmacist. In addition, the negative result has worsened the bottleneck issue in the contemporary education system as there are fewer eligible schools (50 schools accredited A and B) as compared to schools offering only four year bachelor of pharmacy program (265 schools with lower accreditation level).85 As a result, waiting time is even longer for students from these schools to start practicing as pharmacist as they have to enroll in one of the eligible schools to start pre-pharmacist education program.
It is fair to say that the pharmacy education system in Indonesia has significantly changed over a decade. However, the challenge as aforementioned is to prepare graduates that can collaborate and communicate with other professionals and the patients. It is indeed an explicit call from the Association of Indonesian Pharmacy Higher Education (APTFI) for the integration of curriculum content and practice experience i.e. period of workplace learning in form of interprofessional education. There is evidence that interprofessional education can contextualize learning, develop skills, knowledge and values to become professional pharmacist.86 Whilst there is a small portion of pharmacy schools strive to pursue such integration, the majority might need to be stimulated.87
Apart from the efforts in updating pharmacy curriculum to prepare future generation, there is also an effort to support the pharmacy profession after graduated, i.e. pharmacists. The Indonesian Pharmacists Association (IAI) is working collaboratively with the International Pharmaceutical Federation (FIP), on a Workforce Transformation Program (WTP), which aims to advance pharmacy practice in Indonesia by developing a professional recognition system to signpost pharmacists advancement.88,89 The professional recognition system is a quality assured process, which aimed to be independent, credible, fair, transparent and robust, to recognize an individual’s achievement of defined levels of performance. The principles of professional recognition system can be explained within three themes: in the context of the “profession as a whole”, in the context of the “individual practitioner”, and in the context of “the practice of pharmacy”.90 In the context of the profession as a whole, a professional recognition system aims to provide credible evidence of the pharmacist role in medicines expertise, patient safety and in enhancing the quality and impact of pharmaceutical care provision. The idea of professional recognition is based on the needs of quality assured professional development of health professionals. In the context of individual practitioners, a credentialing system should support pharmacists’ professional development and career progression principally by identifying and providing evidence on their performance at defined stages of practice. A credentialing system should motivate and inspire pharmacists to develop them to the next professional stage of development. In terms of the practice, through professional recognition, patients have the right to receive the highest level of care depending on their need.
In order to develop a professional recognition system, an establishment of a set of criteria - framework – can be a starting point to support this advancement. The Indonesian Pharmacists Association (IAI) has addressed this, by developing an Indonesian Advanced Development Framework (IADF), which serves as a tool to identify pharmacists’ learning gaps and skills to advance their careers and practice.33 The IADF will be used as a tool to map useful and relevant education and training provisions as well as a tool for credentialing or professional recognition. The professional recognition model could be linked to a clear career pathway, and staff remuneration in the workplace. Career pathway and remuneration availability could affect the motivation of pharmacists which also linked to the performance of the pharmacy workforce in delivering the service.51,61,91,92 There is evidence suggesting that credentialed practitioners deliver improved therapeutic outcomes, quality of care, and better patient safety compared with non-credentialed practitioners.90 This, therefore, will assure the quality of practitioner services for the public. Recognition of practitioners will also address patient safety issues and provide the trust about the role of pharmacists in the delivery of universal health care.
CONCLUSION
Community pharmacists are highly trained professionals, have been central to the delivery of medicines, and are located within the heart of the communities. Community pharmacy is also a highly regulated industry which operates under dynamic health sector landscape allowing for innovation and changes in the contemporary practice. These features are the key drivers in leveraging the full potential of community pharmacy and pharmacist to meet the changing societal needs and to expand their roles within the primary care system in Indonesia.
This article promulgates the notion that the integration of community pharmacy into primary care in Indonesia is an incremental process and often requires policy initiatives to drive such changes. Community pharmacy in Indonesia can be a great example to untap the tremendous opportunity to deliver greater health outcomes. The conditions under which pharmacists are able to play a role in primary care services either via puskesmas or the network of primary care providers may suggest that pharmacist is an essential part of allied health services and integrated care. Arguably, the “Gema Cermat” program has improved pharmacist engagement with the communities which is vital for any practitioners working in the primary care sector.
Despite the presence of persistent barriers which are often exacerbated by a range of system constraints, we argue that there has been some progress in the integration process. Major reforms are needed to reduce the barriers, improve the quality of pharmacy services and enable pharmacists to establish their ground within the primary care system strategically.
Footnotes
CONFLICT OF INTEREST
None declared.
FUNDING
None.
Contributor Information
Andi Hermansyah, Faculty of Pharmacy, Airlangga University. Surabaya (Indonesia). andi-h@ff.unair.ac.id.
Luh Wulandari, Faculty of Medicine, Udayana University. Bali (Indonesia). lwulandari@unud.ac.id.
Susi A. Kristina, Faculty of Pharmacy, University Gadjah Mada. Yogyakarta (Indonesia). susiari_k@ugm.ac.id
Sherly Meilianti., Department of practice and policy, School of Pharmacy, University College London. London (United Kingdom). sherly.meilianti.15@ucl.ac.uk.
References
- 1.Agustina R, Dartanto T, Sitompul R, Susiloretni KA, Suparmi Achadi EL, Taher A, Wirawan F, Sungkar S, Sudarmono P, Shankar AH, Thabrany H Indonesian Health Systems Group. Universal health coverage in Indonesia:concept, progress, and challenges. Lancet. 2019;393(10166):75–102. doi: 10.1016/s0140-6736(18)31647-7. [DOI] [PubMed] [Google Scholar]
- 2.Central Intelligence Agency. The World Factbook:Indonesia Vol 2020. Washington DC: Central Intelligence Agency; 2020. [Google Scholar]
- 3.Ministry of Health Indonesia. Indonesia Health Profile 2018 (Profil Kesehatan Indonesia 2018) Jakarta: Ministry of Health Indonesia; 2018. [Google Scholar]
- 4.Tan M, Kusriastuti R, Savioli L, Hotez PJ. Indonesia:an emerging market economy beset by neglected tropical diseases (NTDs) PLoS Negl Trop Dis. 2014;8(2):e2449. doi: 10.1371/journal.pntd.0002449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schröders J, Wall S, Hakimi M, Dewi FST, Weinehall L, Nichter M, Nilsson M, Kusnanto H, Rahajeng E, Ng N. How is Indonesia coping with its epidemic of chronic noncommunicable diseases?A systematic review with meta-analysis. PLoS One. 2017 Jun 20;12(6):e0179186. doi: 10.1371/journal.pone.0179186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kristina SA, Endarti D, Wiedyaningsih C, Fahamsya A, Faizah N. Health Care Cost of Noncommunicable Diseases Related to Smoking in Indonesia 2015. Asia Pac J Public Health. 2018;30(1):29–35. doi: 10.1177/1010539517751311. [DOI] [PubMed] [Google Scholar]
- 7.Christiani Y, Dugdale P, Tavener M, Byles JE. The dynamic of non-communicable disease control policy in Indonesia. Aust Health Rev. 2017;41(2):207–213. doi: 10.1071/ah15196. [DOI] [PubMed] [Google Scholar]
- 8.Mahendradhata Y, Trisnantoro L, Listyadewi S, Soewondo P, Marthias T, Harimurti P, Prawira P The Republic of Indonesia Health System Review. Health Systems in Transition. New Delhi: WHO; 2017. [(accessed (Jul 15 2020)]. Available at: https://apps.who.int/iris/bitstream/handle/10665/254716/9789290225164-eng.pdf?sequence=1&isAllowed=y . [Google Scholar]
- 9.Government of Indonesia. [The National Health Law Number 36 of 2009] Indonesia Go Vol 36/2009. Jakarta: Government of Indonesia; 2009. [Google Scholar]
- 10.Suryanto S, Plummer V, Boyle M. Financing healthcare in Indonesia. Asia Pacific J Health Manag. 2016;11(2):33–38. doi: 10.24083/apjhm.v11i2.185. [DOI] [Google Scholar]
- 11.Ministry of Health Indonesia. [Data and Information:Indonesian Health Profile 2019] Jakarta: Ministry of Health Indonesia; 2020. [Google Scholar]
- 12.World Health Organization. Primary health care systems (PRIMASYS):comprehensive case study from Indonesia. Geneva: World Health Organization; 2017. [Google Scholar]
- 13.Ministry of Health Indonesia. [The Minister of Health Regulation Number 46 of 2015 on Puskesmas Accreditation] Indonesia MoH Vol 46/2015. Jakarta: Ministry of Health Indonesia; 2015. [Google Scholar]
- 14.Limato R, Tumbelaka P, Ahmed R, Nasir S, Syafruddin D, Ormel H, Kumar MB, Taegtmeyer M, Kok M. What factors do make quality improvement work in primary health care?Experiences of maternal health quality improvement teams in three Puskesmas in Indonesia. PLoS One. 2019;14(12):e0226804. doi: 10.1371/journal.pone.0226804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holzhacker RL, Wittek R, Woltjer J. Decentralization and Governance in Indonesia. Cham: Springer 2016 ISBN; 978-3-319-22433-6. [Google Scholar]
- 16.Heywood P, Choi Y. Health system performance at the district level in Indonesia after decentralization. [Published 2010 Mar 5];BMC Int Health Hum Rights. 2010 10:3. doi: 10.1186/1472-698x-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aspinall E. Health care and democratization in Indonesia. Democratization. 2014;21(5):803–823. doi: 10.1080/13510347.2013.873791. [DOI] [Google Scholar]
- 18.Fossati D. Beyond “Good Governance”:The multi-level politics of health insurance for the poor in Indonesia. World Development. 2016;87:291–306. doi: 10.1016/j.worlddev.2016.06.020. [DOI] [Google Scholar]
- 19.Mboi N. Indonesia:On the Way to Universal Health Care. Health Systems &Reform. 2015;1(2):91–97. doi: 10.1080/23288604.2015.1020642. [DOI] [PubMed] [Google Scholar]
- 20.Government of Indonesia. [The National Social Security System Law Number 40 of 2004] Indonesia Go Vol 40/2004. Jakarta: Government of Indonesia; 2004. [Google Scholar]
- 21.Suryahadi A, Febriany V, Yumna A. Expanding social security in Indonesia. In: Ilcheong Yi., editor. Towards universal health care in emerging economies. London: Palgrave Macmillan 2017. ISBN; 978-1-137-53376-0. [Google Scholar]
- 22.Pisani E, Olivier Kok M, Nugroho K. Indonesia's road to universal health coverage:a political journey. Health Policy Plan. 2017;32(2):267–276. doi: 10.1093/heapol/czw120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hermansyah A, Sainsbury E, Krass I. Investigating the impact of the universal healthcare coverage programme on community pharmacy practice. Health Soc Care Community. 2018;26(2):e249–e260. doi: 10.1111/hsc.12506. [DOI] [PubMed] [Google Scholar]
- 24.Dartanto T, Halimatussadiah A, Rezki JF, Nurhasana R, Siregar CH, Bintara H, Usman Pramono W, Sholihah NK, Yuan EZW, Soeharno R. Why Do Informal Sector Workers Not Pay the Premium Regularly?Evidence from the National Health Insurance System in Indonesia. Appl Health Econ Health Policy. 2020;18(1):81–96. doi: 10.1007/s40258-019-00518-y. [DOI] [PubMed] [Google Scholar]
- 25.Reuters. [(accessed Jul 15 2020)];Indonesia to raise health insurance premiums amid coronavirus outbreak. Available at: https://es.reuters.com/article/asia/idUSL4N2CV2H5 .
- 26.The Jakarta Post. Jokowi raises BPJS Kesehatan premiums, again. Jakarta: The Jakarta Post; 2020. [Google Scholar]
- 27.Athiyah U, Setiawan CD, Nugraheni G, Zairina E, Utami W, Hermansyah A. Assessment of pharmacists'knowledge, attitude and practice in chain community pharmacies towards their current function and performance in Indonesia. Pharm Pract (Granada) 2019;17(3):1518. doi: 10.18549/pharmpract.2019.3.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hermansyah A, Rahem A, Sukorini AI. Survey of Pharmacy Contribution and Excellence:Nationwide Survey Report. Surabaya: Faculty of Pharmacy Universitas Airlangga. Indonesian Pharmacist Association; 2019. [Google Scholar]
- 29.Hermansyah A, Athiyah U, Setiawan CD. Are patients willing to ask for generic drug substitutions? Int J Pharm Teach Pract. 2013. 4(4):1–7. [Google Scholar]
- 30.Hermansyah A, Sukorini AI, Setiawan CD, Priyandani Y. The conflicts between professional and non professional work of community pharmacists in Indonesia. Pharm Pract (Granada) 2012;10(1):33–39. doi: 10.4321/s1886-36552012000100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith F. Private local pharmacies in low- and middle-income countries:a review of interventions to enhance their role in public health. Trop Med Int Health. 2009;14(3):362–372. doi: 10.1111/j.1365-3156.2009.02232.x. [DOI] [PubMed] [Google Scholar]
- 32.Hermansyah A, Sainsbury E, Krass I. Community pharmacy and emerging public health initiatives in developing Southeast Asian countries:a systematic review. Health Soc Care Community. 2016;24(5):e11–e22. doi: 10.1111/hsc.12289. [DOI] [PubMed] [Google Scholar]
- 33.Wibowo Y, Parsons R, Sunderland B, Hughes J. Evaluation of community pharmacy-based services for type-2 diabetes in an Indonesian setting:pharmacist survey. Int J Clin Pharm. 2015;37(5):873–882. doi: 10.1007/s11096-015-0135-y. [DOI] [PubMed] [Google Scholar]
- 34.Tri Murti Andayani, Satibi Satibi. Pharmacy Practice in Indonesia. In: Fathelrahman A, Ibrahim MI, Wertheimer AI, eds, editors. Pharmacy practice in Developing Countries:achievements and challenges. London: Academic Press; 2020. ISBN:9780128198377. [Google Scholar]
- 35.Setiadi AP, Wibowo Y, Brata C, Halim SV, Wardhani SA, Sunderland B. The role of pharmacists in community education to promote responsible self-medication in Indonesia:an application of the spiral educational model. Int J Clin Pharm. 2020 doi: 10.1007/s11096-020-01055-8. [Ahead of Print] [DOI] [PubMed] [Google Scholar]
- 36.Kimura S, Nakamura Y. Poor quality pharmaceuticals in global public health. Singapore: Springer; 2020. A case study in Indonesia:self-medication and limited access; pp. 119–147. ISBN 978-981-15-y2088-4. [Google Scholar]
- 37.President Regulation. [The pharmacy practice Act of 2009] Jakarta: Government of Indonesia; 2009. [Google Scholar]
- 38.Ministry of Health Indonesia. [The community pharmacy Decree of 2017] Indonesia MoH. Jakarta: Ministry of Health Indonesia; 2017. [Google Scholar]
- 39.Ministry of Health Indonesia. [The standard of pharmacy services in community pharmacy] Indonesia MoH. Jakarta: Ministry of Health Indonesia; 2016. [Google Scholar]
- 40.Ministry of Health Indonesia. [The standard of pharmacy services in Puskesmas] Indonesia MoH. Jakarta: Ministry of Health Indonesia; 2016. [Google Scholar]
- 41.Ministry of Health Indonesia. [The standard of pharmacy services in hospital] Indonesia MoH. Jakarta: Ministry of Health; 2016. [Google Scholar]
- 42.Hermansyah A, Sainsbury E, Krass I. Multiple policy approaches in improving community pharmacy practice:the case in Indonesia. BMC Health Serv Res. 2018;18(1):449. doi: 10.1186/s12913-018-3258-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Indonesia Ministry of Health. [The Standard of Tariff for Health Services in the Universal Health Coverage] Jakarta: Ministry of Health; 2016. [Google Scholar]
- 44.Ng JYS, Ramadani RV, Hendrawan D, Duc DT, Kiet PHT. National Health Insurance Databases in Indonesia, Vietnam and the Philippines. Pharmacoecon Open. 2019;3(4):517–526. doi: 10.1007/s41669-019-0127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Social Health Insurance Agency. [Health facilities under universal health coverage] Jakarta: Social Health Insurance Agency; 2020. [Google Scholar]
- 46.Dewi DAPS, Satibi S, Puspandari DA. [Cost Analysis of Medicines at the Supporting Facilities and Factors associated with it in Yogyakarta during the National Health Insurance Era] Jurnal Manajemen dan Pelayanan Farmasi. 2015;5:291–300. [Google Scholar]
- 47.Kaswindarti N, Satibi S, Puspandari DA. [Analysis of pharmacists'perceptions on the implementation of payment system at the pharmacy level in the National Health Insurance Era in Yogyakarta] Jurnal Manajemen dan Pelayanan Farmasi. 2015;5:275–282. [Google Scholar]
- 48.Wijaya IN, Athiyah U, Fasich Hermansyah A. Knowledge, attitude, and practice of pharmacists towards management of hypertension in primary care centers. J Basic Clin Physiol Pharmacol. 2020 doi: 10.1515/jbcpp-2019-0319. [Ahead of Print] [DOI] [PubMed] [Google Scholar]
- 49.Susyanty AL, Yuniar Y, Herman MJ, Prihartini N. [The Suitability of Pharmaceutical Services Standard Implementation in Public Health Centre] Media Penelitian dan Pengembangan Kesehatan. 2020;30:65–74. [Google Scholar]
- 50.Ministry of Health Indonesia. [The Minister of Health Decree on Gema Cermat] Jakarta: Ministry of Health; 2015. [Google Scholar]
- 51.Hermansyah A, Pitaloka D, Sainsbury E, Krass I. Prioritising recommendations to advance community pharmacy practice. Res Social Adm Pharm. 2018;14(12):1147–1156. doi: 10.1016/j.sapharm.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 52.Setiadi AP, Wibowo YI, Setiawan E, Mulyono I, Wardhani SA, Sunderland B. Strategies to implement community training to promote responsible self-medication in Indonesia:a qualitative study of trainers. Int Health. 2020 doi: 10.1093/inthealth/ihz115. [Ahead of Print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Simbara A, Primananda AZ, Tetuko A, Savitri CN. [The educational method for improving knowledge on self-medication practice under Gema Cermat] Indonesia Jurnal Farmasi. 2020;4:1–5. [Google Scholar]
- 54.Nining N, Yeni Y. [The education and campaign of Gema Cermat)] Jurnal Pengabdian kepada Masyarakat. 2019;5:36–48. [Google Scholar]
- 55.Ministry of Health Indonesia. [The Ministerial Decree on Integrated Permit Administration for Electronic System in Health Care 2018] Jakarta: Ministry of Health; 2018. [Google Scholar]
- 56.Indonesian Pharmacists Association. [The Decree of the Congress on General Program of the National Committee of Indonesian Pharmacist Association 2018-2022] Pekanbaru: Indonesian Pharmacist Association; 2018. [Google Scholar]
- 57.Indonesian Pharmacists Association. The User Manual for SIAP Apps. Jakarta: Indonesian Pharmacist Association; 2020. [Google Scholar]
- 58.The Parliament of Indonesia - House of Representative. The Draft of the Pharmacy Law (Omnibus Law) 2020. Jakarta: The Parliament of Indonesia - House of Representative; 2020. [Google Scholar]
- 59.Smith T, McNeil K, Mitchell R, Boyle B, Ries N. A study of macro-, meso- and micro-barriers and enablers affecting extended scopes of practice:the case of rural nurse practitioners in Australia. BMC Nurs. 2019;18:14. doi: 10.1186/s12912-019-0337-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hermansyah A, Sainsbury E, Krass I. Investigating influences on current community pharmacy practice at micro, meso, and macro levels. Res Social Adm Pharm. 2017;13(4):727–737. doi: 10.1016/j.sapharm.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 61.Puspitasari HP, Aslani P, Krass I. Challenges in the management of chronic noncommunicable diseases by Indonesian community pharmacists. Pharm Pract (Granada) 2015;13(3):578. doi: 10.18549/pharmpract.2015.03.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Widayati A, Virginia DM, Setiawan CH, Fenty F, Donowati MW, Christasani PD, Hartayu TS, Suhadi R, Saini B, Armour C. Pharmacists'views on the development of asthma pharmaceutical care model in Indonesia:A needs analysis study. Res Social Adm Pharm. 2018;14(12):1172–1179. doi: 10.1016/j.sapharm.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 63.Anggriani Y, Ramadaniati HU, Sarnianto P, Pontoan J, Suryawati S. The Impact of Pharmaceutical Policies on Medicine Procurement Pricing in Indonesia Under the Implementation of Indonesia's Social Health Insurance System. Value Health Reg Issues. 2020;21:1–8. doi: 10.1016/j.vhri.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 64.Hadi U, van den Broek P, Kolopaking EP, Zairina N, Gardjito W, Gyssens IC Study Group Antimicrobial Resistance in Indonesia:Prevalence and Prevention AMRIN. Cross-sectional study of availability and pharmaceutical quality of antibiotics requested with or without prescription (Over The Counter) in Surabaya, Indonesia. [Published 2010 Jul 9];BMC Infect Dis. 2010 10:203. doi: 10.1186/1471-2334-10-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Puspitasari HP, Faturrohmah A, Hermansyah A. Do Indonesian community pharmacy workers respond to antibiotics requests appropriately? Trop Med Int Health. 2011;16(7):840–846. doi: 10.1111/j.1365-3156.2011.02782.x. [DOI] [PubMed] [Google Scholar]
- 66.Wulandari L, Mashuri Y, Ferdiana A, Probandari A, Wibawa T, Wiseman V. Inside the black box of antibiotic dispensing by private drug sellers in Indonesia (PINTAR study) International Society to Improve the Use of Medicine (ISIUM) Conference. Bangkok. 2020 [Google Scholar]
- 67.Babar ZU, Scahill S. Barriers to effective pharmacy practice in low-and middle-income countries. Integr Pharm Res Pract. 2014;3:25–27. doi: 10.2147/IPRP.S35379. [DOI] [Google Scholar]
- 68.Herman MJ, Handayani RS. The Preparedness of Pharmacist in Community Setting to Cope with Globalization Impact. Indonesia Pharm J. 2015;5(1):57–66. [Google Scholar]
- 69.Sugiyatmi TA, Hadi U, Chalidyanto D, Hafidz F, Miftahussurur M. Does the implementation of national health insurance affect the workload of a doctor and have an impact on service quality?A systematic literature review. J Public Health Afr. 2019;10(1s):101–105. doi: 10.4081/jphia.2019.1198. [DOI] [Google Scholar]
- 70.Meilianti S, Bunyamin IM. How Indonesia's pharmacists are developing their primary healthcare workforce. Int Pharm J. 2019;37:30–32. [Google Scholar]
- 71.Satibi S, Rokhman MR, Aditama H. Developing Consensus Indicators to Assess Pharmacy Service Quality at Primary Health Centres in Yogyakarta, Indonesia. Malays J Med Sci. 2019;26(4):110–121. doi: 10.21315/mjms2019.26.4.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Brata C, Fisher C, Marjadi B, Schneider CR, Clifford RM. Factors influencing the current practice of self-medication consultations in Eastern Indonesian community pharmacies:a qualitative study. [Published 2016 May 13];BMC Health Serv Res. 2016 16:179. doi: 10.1186/s12913-016-1425-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Herman MJ, Susyanty AL. Analysis of pharmacy services by pharmacists in community pharmacy. Buletin Penelitian Sistem Kesehatan. 2012;15:271–281. [Google Scholar]
- 74.Hallit S, Selwan CA, Salameh P. Primary health care policy and vision for community pharmacy and pharmacists in Lebanon. Pharm Pract (Granada) 2020;18(2):2003. doi: 10.18549/pharmpract.2020.2.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Anderson C, Sharma R. Primary health care policy and vision for community pharmacy and pharmacists in England. Pharm Pract (Granada) 2020;18(1):1870. doi: 10.18549/pharmpract.2020.1.1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dineen-Griffin S, Benrimoj SI, Garcia-Cardenas V. Primary health care policy and vision for community pharmacy and pharmacists in Australia. Pharm Pract (Granada) 2020;18(2):1967. doi: 10.18549/pharmpract.2020.2.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kristina SA, Ekasari MP, Wati MR. Internet use for searching information on Health and Medicine:An Exploratory study among Indonesian customers. Res J Pharm Technol. 2019;12(12):5927–5931. doi: 10.5958/0974-360X.2019.01028.X. [DOI] [Google Scholar]
- 78.Al-Worafi YM. Drug safety in Indonesia. In: Al-Worafi Y, editor. Drug Safety in Developing Countries:Achievements and Challenges. London: Academic Press; 2020. ISBN:9780128198377. [Google Scholar]
- 79.Parathon H, Kuntaman K, Widiastoety TH, Muliawan BT, Karuniawati A, Qibtiyah M, Djanun Z, Tawilah JF, Aditama T, Thamlikitkul V, Vong S. Progress towards antimicrobial resistance containment and control in Indonesia. [Published 2017 Sep 5];BMJ. 2017 358:3808. doi: 10.1136/bmj.j3808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ung COL. Community pharmacist in public health emergencies:Quick to action against the coronavirus 2019-nCoV outbreak. Res Social Adm Pharm. 2020;16(4):583–586. doi: 10.1016/j.sapharm.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mooranian A, Emmerton L, Hattingh L. The introduction of the national e-health record into Australian community pharmacy practice:pharmacists'perceptions. Int J Pharm Pract. 2013;21(6):405–412. doi: 10.1111/ijpp12034. [DOI] [PubMed] [Google Scholar]
- 82.Kusumawati W, Orbayinah S. Interprofessional education from pilot to formal curriculum. In: Forman D, Jones M, Thistlethwaite J, editors. Leadership and Collaboration. London: Palgrave Macmillan; 2015. [Google Scholar]
- 83.Lin HW, Yang LC, Mafruhah OR, Nguyen HT, Cao TT, Yam FK. Evolution of Clinical Pharmacy Practice and Pharmacy Education in Taiwan, Vietnam, and Indonesia:A Narrative Review. J Am College Clin Pharm. 2020 doi: 10.1002/jac5.1258. [Ahead of Print]. [DOI] [Google Scholar]
- 84.Kristina SA, Gustriawanto N, Rokhman MR, Aditama H, Sari IP. Students'first experience with Objective Structured Clinical Examination in a pharmacy school in Indonesia. J Appl Pharm Sci. 2018;8(9):102–106. doi: 10.7324/JAPS.2018.8915. [DOI] [Google Scholar]
- 85.Ministry of Research TaHEoI. Database of Higher Education:Pharmacy 2020. Jakarta: Ministry of Research, Technology and Higher Education of Indonesia; 2020. [Google Scholar]
- 86.Remington TL, Foulk MA, Williams BC. Evaluation of evidence for interprofessional education. Am J Pharm Educ. 2006;70(3):66. doi: 10.5688/aj700366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Syahrizal D, Renaldi T, Dianti SW, Jannah N, Rachmah R, Firdausa S, Vonna A. The Differences in Perceptions of Interprofessional Education Among Health Profession Students:The Indonesian Experience [published correction appears in J Multidiscip Healthc 2020 Jun 25;13:557] J Multidiscip Healthc. 2020;13:403–410. doi: 10.2147/jmdh.s240195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wang Lin-Nam. Workforce transformation, endorsed by Ministry of Health, is brought to Indonesia's pharmacists by FIP 2019. Congress of FIP; Abu Dhabi: 2019. [Google Scholar]
- 89.Indonesian Pharmacists Association. [Press release:the signing of Memorandum of Understanding between IAI and FIP on advanced pharmacist program] Jakarta: Indonesian Pharmacist Association; 2019. [Google Scholar]
- 90.Indonesian Pharmacists Association. Advanced Pharmacy Practice Survey of Indonesia. Jakarta: Indonesian Pharmacist Association; 2019. [Google Scholar]
- 91.Rijaluddin MK, Utami W, Othman Z, Puspitasari HP, Rahem A, Sukorini AI, Hermansyah A. Exploration of barriers affecting job satisfaction among community pharmacists. J Basic Clin Physiol Pharmacol. 2020 doi: 10.1515/jbcpp-2019-0325. [Ahead of Print] [DOI] [PubMed] [Google Scholar]
- 92.Joint Partners Credentialing Task Group. Professional recognition and professional advancement:For our practitioners, for our profession and for our patients. London: Royal Pharmaceutical Society; 2013. [Google Scholar]


