Screening for cancer is an important aspect of medical practice in this new millennium. It is well accepted that to decrease mortality due to oesophageal carcinoma, it is necessary to identify the malignancy at earlier, curable stages. In The Lancet, Rebecca Fitzgerald and colleagues1 report the results of a prospective, multicentre, pragmatic, randomised controlled trial, done at 109 sociodemographically diverse general practice clinics in England, which investigated whether offering the Cytosponge-trefoil factor 3 (TFF3) procedure to patients on medication for gastro-oesophageal reflux would increase the detection of Barrett's oesophagus compared with standard management. In this study,1 13 657 eligible patients were randomly assigned to either the usual care group (n=6531) or the intervention group (n=6983). Participants in the usual care group received standard management of gastro-oesophageal reflux, and participants in the intervention group were offered the Cytosponge-TFF3 procedure to collect cytological specimens, which were stained with an antibody against TFF3 to detect Barrett's oesophagus, and a subsequent endoscopy if TFF3-positive cells were identified. 1750 participants met all of the eligibility criteria on a telephone screening interview and underwent the procedure. Most of these participants (1654 [95%]; median age 69 years; 858 [52%] female) swallowed the Cytosponge successfully. The Cytosponge1, 2, 3 is an orally administered, single-use, gelatine-encapsulated sponge device. Approximately 5 min after swallowing the Cytosponge, the capsule dissolves in the stomach to release the sponge, which is then manually drawn through the oesophagus by an attached string to collect oesophageal cytological specimens.
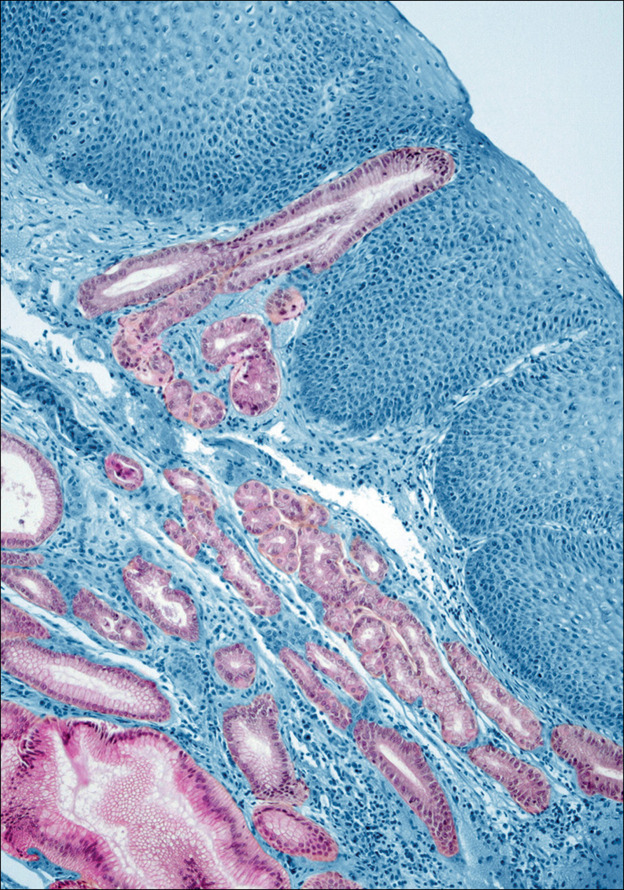
© 2020 ISM/Science Photo Library
The primary endpoint of the study was the diagnosis of Barrett's oesophagus at 12 months after enrolment, expressed as a rate per 1000 person-years, in all participants in the intervention group (regardless of whether they had accepted the offer of the Cytosponge-TFF3 procedure) compared with all participants in the usual care group. The aim was to establish whether the offer of the Cytosponge-TFF3 test in general practice results in an increase in Barrett's oesophagus diagnoses. Overall, 140 (2%) of 6834 participants in the intervention group and 13 (<1%) of 6388 participants in the usual care group were diagnosed with Barrett's oesophagus (absolute difference 18·3 per 1000 person-years [95% CI 14·8–21·8]; overall rate ratio [RR] 10·2 [5·8–18·1]; RR adjusted for cluster randomisation 10·6 [6·0–18·8], p<0·0001). The results showed that 131 (59%) of 221 participants who underwent endoscopy after testing positive for TFF3 had Barrett's oesophagus or early-stage oesophago-gastric cancer. Of those participants who underwent the Cytosponge-TFF3 procedure, only one serious adverse event associated with the device was reported (detachment of the sponge from the string, requiring endoscopic retrieval). 142 (9%) of 1654 participants who swallowed the Cytosponge successfully reported an adverse event, with a sore throat being the most commonly reported. The investigators are to be congratulated on completing a difficult prospective randomised trial in the primary care setting; a context that resembles one in which the device is anticipated to be clinically applied. These encouraging results prompt us to consider whether the Cytosponge-TFF3 procedure should now be accepted as a screening tool for oesophago-gastric cancer.
National Health Service (NHS) screening recommendations for certain cancers are largely based on the age-specific prevalence of the disease.4, 5 Notably, in this study by Fitzgerald and colleagues,1 the screening population was restricted to patients who had been taking acid-suppressant medication for at least 6 months, which was used as a surrogate marker for gastro-oesophageal reflux disease (GORD). This strategy avoided the need to use GORD screening questionnaires, which might have been difficult to implement in the primary care setting. However, being male, which is one of the strongest risk factors for the development of oesophago-gastric cancer, was not incorporated in the screening criteria.6
The Cytosponge-TFF3 procedure is a promising non-endoscopic screening tool and will represent a component in the screening for Barrett's oesophagus and oesophago-gastric cancer. As with colorectal cancer, this procedure is unlikely to be the sole screening tool, as multiple tests will be needed to enhance participation in a screening programme. For instance, although intended for routine use in primary care, in the current environment of an infectious disease (COVID-19) pandemic, the Cytosponge-TFF3 procedure might be difficult to implement, given its potential to generate aerosolised particles during sponge withdrawal. It might also be necessary to enrich disease prevalence in the screened population by limiting this population to males and people with other risk factors, in order to make this test more cost-effective than previously shown. As the study1 authors comment, determining the ideal enrichment criteria will be crucial to ensuring the success of a Barrett's oesophagus screening method.
Acknowledgments
KKW reports receiving research funding from eNose (Zupten, Netherlands) for research on a device used in a screening study of Barrett's oesophagus, and declares no financial interests in the device. YH declares no competing interests.
References
- 1.Fitzgerald RC, di Pietro M, O'Donovan M. Cytosponge-trefoil factor 3 versus usual care to identify Barrett's oesophagus in a primary care setting: a multicentre, pragmatic, randomised controlled trial. Lancet. 2020;396:333–344. doi: 10.1016/S0140-6736(20)31099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kadri SR, Lao-Sirieix P, O'Donovan M. Acceptability and accuracy of a non-endoscopic screening test for Barrett's oesophagus in primary care: cohort study. BMJ. 2010;341 doi: 10.1136/bmj.c4372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ross-Innes CS, Debiram-Beecham I, O'Donovan M. Evaluation of a minimally invasive cell sampling device coupled with assessment of trefoil factor 3 expression for diagnosing Barrett's esophagus: a multi-center case-control study. PLoS Med. 2015;12 doi: 10.1371/journal.pmed.1001780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sikora K. Cancer screening. Medicine. 2020;48:132–137. [Google Scholar]
- 5.Calman K. Developing screening in the NHS. J Med Screen. 1994;1:101–105. doi: 10.1177/096914139400100208. [DOI] [PubMed] [Google Scholar]
- 6.Fitzgerald RC, di Pietro M, Ragunath K. British Society of Gastroenterology guidelines on the diagnosis and management of Barrett's oesophagus. Gut. 2014;63:7–42. doi: 10.1136/gutjnl-2013-305372. [DOI] [PubMed] [Google Scholar]