Abstract
As a pathogen spread primarily by the respiratory route COVID-19 infection not only poses significant risks to health care workers, but to dentists and dental health care workers, owing to the potential prolonged exposure and proximity to patients. This holds true for non-dentist health care workers who often in the setting of emergency departments and urgent care centers are tasked with addressing oral symptoms including abscesses, damaged teeth, jaw injuries and other dental urgencies. Infection control practice guidelines were evaluated for COVID-19 infection prevention in a dental setting. In this brief review, protective measures to reduce the risk of COVID-19 infection for dentists and non-dentist health care providers will be introduced. This includes patient evaluation, personal and patient protective equipment use, sterilization and disinfection protocols.
Keywords: COVID-19, SARS-COV-2, Dental, Infection control, Clinical decision making, Risk factor
One of the critical steps in preserving the safety and health of medical professionals, health care workers, including dentists, and non dental providers of oral care is the use of effective infection control measures, and consistent use of appropriate levels of personal protective equipment (PPE).
Towards that end, the following is a brief introduction of important concepts and guidelines for dental health care providers, and non-dental medical practitioners who may be faced with treating oral illness in the context of COVID-19, although the information can be considered for general preparedness.
The oral cavity is a natural reservoir of both opportunistic and pathogenic microorganisms. Due to the invasive nature of the dental procedures, dental staffs are directly exposed to potentially pathogenic microorganisms, posing an occupational risk. This makes treating oral problems of increased concern owing to exposure time and proximity to the respiratory tract that dental and non-dental health care workers will be faced with in the treatment of dental, and other medical/dental issues involving the oral cavity and upper respiratory tract that can afflict patients – whether as from trauma, infection, or neglect resulting in abscess or cavities.
Studies have confirmed this occupational risk, demonstrating bacterial and viral transmission in dental practice,1 , 2 which also includes respiratory viruses like influenza, despite the use of mask and spectacles.3 , 4 SARS-CoV-2 can be transmitted through respiratory droplets and bio-aerosols produced as a result of drilling. Saliva also has high load of viruses. This increases the risk for dental staff contracting COVID-19 within a dental setting. The mode of transmission involves face-face communication with the infected patient who might cough or sneeze, direct exposure to oral and upper respiratory fluids, along with blood, inhalation of these fluids that were aerosolized by the use of high speed rotatory and ultrasonic instruments in dental treatments, and contact transmission with contaminated instruments and fomites.
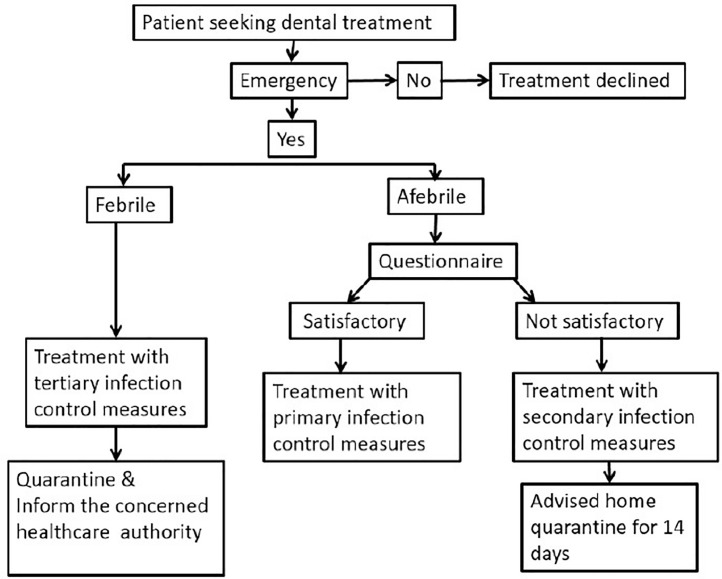
As of now questions remain in terms of how long SARS-CoV-2 can survive on various fomites. However, considering some preliminary information and the fact that it behaves similar to other coronaviruses, SARS-CoV-2 may have persistent survival, perhaps a few hours, or longer depending on the type of surface, temperature and humidity of the environment, adding to the continued risk of contact transmission, as specified above Fig. 1 .
Fig. 1.
Process of managing a COVID-19 Patient in a dental setting.
Advice for dental professionals for patient evaluation during and post-COVID time period
Upon initial presentation of the patient to the practice or facility it is recommended to record the temperature of the patient, and the staff, using a contact free thermometer. If found febrile, the patient should be immediately quarantined and the same should be informed to the concerned health authorities.
If without fever, then the patient and the attender, if any, should be screened with a questionnaire, if possible, in an isolated triage, with medical masks on. The questions can be framed primarily to elucidate the possibilities of a recent SARS-CoV-2 transmission, which could make the unaware patient an active spreader. Peng X et al., have recommended some reasonable question5, which we list here with slight modification: (i) nature of the patient's work to help to assess the high risk of contracting COVID-19. Important question is in the past 14 days has the patient: (a) Experienced fever/respiratory issues/diarrhea/vomiting, (b) traveled to COVID-19 active zone, (c) has been in contact with a person who has traveled to COVID-19 active zone, (d) has been in contact with a COVID-19 positive patient, (e) has been in contact with a person who had fever &/or cough, (f) been using public transport or have attended a public gathering. The patients who answer “No” to 2nd question with a satisfying answer to 1st question are considered for treatment. Otherwise, the patient should be educated on the importance of, and asked to, self-quarantine and reporting to health authorities of any fever or respiratory issues that may develop during the period. The dentist can defer the treatment to such patients, up until the quarantine period, unless it is a dental emergency, in which case the patient has to be treated with proper precautions.
Infection control in dental settings
Personal hygiene - Staff
With a known risk of contact transmission, it is extremely important for the dental staff to maintain personal hygiene. Hand hygiene is a well-known critical measure to reduce cross-contamination in healthcare settings (6), which is routinely followed in dental practice as well. The best way to maintain hand hygiene is to clean the hands with clean water and soap before and after treatment, after touching the contaminated devices/instruments and the surroundings, and after any contact with biological tissues/fluids. A thorough cleaning with alcohol based rubs is also recommended by centers for disease control and prevention (CDC), USA (7). It is advised against touching one's eyes, nose and mouth, and is recommended to clean the hands again if done. Further, the dental staffs are advised to equip with personal protective gears before handling any dental patients. With the known knowledge of simple masks unable to prevent respiratory viral transmission in dentists (4), the dental staff are advised to fortify their primary protective gears like disposable surgical mask, cap, gloves and scrubs with protective eye/face shield and impermeable shoe cover, or upgrade to secondary or tertiary protective gears as necessary. If a need arise to treat a COVID-19 positive patient, it is highly recommended to use the special protective wear, which are used in general healthcare settings to treat such patients.
Procedural hygiene
Considering the low number of patient inflow in this pandemic era, it is advisable to treat the patients in isolated and well-ventilated rooms or even better in a negatively pressurized room, if available. A preoperative mouth rinse with 0.2% povidone iodine is advised before the oral examination of the patients, which is known to reduce the number of microorganisms in oral cavity, including SARS-CoV-2.8 The procedures that may induce cough/gag reflex and saliva secretion, like dental impressions and other prosthodontic procedures and intraoral X-rays, should be avoided. Following a four-handed dentistry increases the efficiency of the procedure and thus reduces the chances of cross contamination. With the fact that SARS-CoV-2 is found in saliva, it is recommended to get rid of the contaminant using a high-volume saliva ejector. In case where a high-speed hand piece or ultrasonic device needs to be used, it is safer to isolate the operating area with rubber dams, which can reduce the saliva or blood contaminants in the resultant aerosol. Using high-speed hand piece with anti-retraction valves will prevent the aspiration of biological fluids/microbes into dental air and water tubes, thus preventing the cross-contamination of the dental unit (9). In case of extraction or other minor surgeries, absorbable sutures are preferred to prevent the need for the patient's short-term follow-up visit for suture removal.
General hygiene
Where possible, disposable instruments must be used in the treatment procedures. The reusable instruments should be pretreated with spirit, washed well to get rid of any adhering debris and autoclaved before storing, as per the applicable standards. Similarly, the dental clinics/settings should be cleaned and disinfected as per the applicable regulatory standards. Considering the contact mode of transmission of SARS-CoV-2, a frequent disinfection of every part of the clinics should be followed without any reservations. All the instruments/equipment's and tissues disposed after the treatment of COVID-19 patient are considered infectious medical waste. They should be marked and properly/responsibly disposed into the respective containers, as per the requirements of the applicable standards.
Conclusion
A single possible animal-to-human transmission of SARS-CoV-2 in Wuhan, China has profusely turned into a pandemic across the globe, threatening >160 countries. Unlike SARS-CoV (2003) and MERS-CoV (2012), Novel SARS-CoV-2 is more aggressive in its spread, given its ability to transmit rapidly during its incubation period. This turns an asymptomatic person into a COVID-19-spreader, making it a challenge to locate and quarantine such people. With its ability for both direct and contact transmission, healthcare workers are at a great risk of contracting the disease. Despite the strict infection control and preventive measures followed, several healthcare workers are reportedly infected with SARS-CoV-2, while some of them died as well.10 The reasons for this failure need to be assessed and addressed in future to lower such issues in future. As per the recent analysis dentists are at the highest possible risk of contracting COVID-19. Although, dental treatments have been called off, several emergency conditions continue to be treated across many dental settings.
Dental staff, including non-dental health care workers who may treat dental emergencies, needs to follow several steps, from patient evaluation to infection control at personal, procedural and clinical levels, to prevent any possible COVID-19 cross-contamination in dental clinics.
References
- 1.McCarthy G.M. Risk of transmission of viruses in the dental office. J Can Dent Assoc. 2000;66:554–555. 557. [PubMed] [Google Scholar]
- 2.Volgenant C., de Soet J. Cross-transmission in the dental office: does this make you ill? Curr Oral Health Rep. 2018;5:221–228. doi: 10.1007/s40496-018-0201-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Q., Guan X., Wu P., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus – infected pneumonia. NE J Med2020 [DOI] [PMC free article] [PubMed]
- 4.Davies K., Herbert A., Westmoreland D., et al. Seroepidemiological study of respiratory virus infections among dental surgeons. Br Dent J. 1994;176:262–265. doi: 10.1038/sj.bdj.4808430. [DOI] [PubMed] [Google Scholar]
- 5.Peng X., Xu X., Li Y., et al. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:1–6. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Larson E.L., Early E., Cloonan P., et al. An organizational climate intervention associated with increased handwashing and decreased nosocomial infections. Behav Med. 2000;26:14–22. doi: 10.1080/08964280009595749. [DOI] [PubMed] [Google Scholar]
- 7.Prevention CfDCa. Frequently Asked Questions about Hand Hygiene for Healthcare Personnel Responding to COVID-2019, https://www.cdc.gov/coronavirus/2019-ncov/hcp/hand-hygiene-faq.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Finfection-control%2Fhcp-hand-hygiene-faq.html (2020).
- 8.AAE . American Association of Endodontists; 2020. Coronavirus Disease 19 (COVID-19): Implications for Clinical Dental Care. [Google Scholar]
- 9.Ji X.Y., Fei C.N., Zhang Y., et al. Three key factors influencing the bacterial contamination of dental unit waterlines: a 6‐year survey from 2012 to 2017. Int Dent J. 2019;69:192–199. doi: 10.1111/idj.12456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang J., Zhou M., Liu F. Exploring the reasons for healthcare workers infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020;105(1):100–101. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]