Abstract
PURPOSE
Medicaid expansion was designed to increase access to health care. Evidence is mixed, but theory and empirical data suggest that lower cost of care through greater access to insurance increases health care utilization and possibly improves the health of poor and sick populations. However, this major health policy has yet to be thoroughly investigated for its effect on health disparities. The current study is motivated by one of today’s most stark inequalities: the disparity in breast cancer mortality rates between Black and White women.
METHODS
This analysis used a difference-in-difference fixed effects regression model to evaluate the impact of Medicaid expansion on the disparity between Black and White breast cancer mortality rates. State-level breast cancer mortality data were obtained from the Centers for Disease Control and Prevention. Each state’s Medicaid expansion status was provided by a Kaiser Family Foundation white paper. Two tests were conducted, one compared all expanding states with all nonexpanding states, and the second compared all expanding states with nonexpanding states that voted to expand—but did not by 2014. The difference-in-difference regression models considered the year 2014 a washout period and compared 2012 and 2013 (pretreatment) with 2015 and 2016 (posttreatment).
RESULTS
Medicaid expansion did not lower the disparity in breast cancer mortality. In contrast to expectations, the Black/White mortality ratio increased in states expanding Medicaid for all Medicaid-eligible age groups, with significant effects in younger age groups (P = .01 to .15).
CONCLUSION
These results suggest that states cannot solely rely on access to insurance to alleviate disparities in cancer or other chronic conditions. More exploration of the impacts of low-quality health systems is warranted.
INTRODUCTION
Medicaid expansion, at its core, was designed as a policy to improve health equity. This policy allowed men and women to enroll in state-sponsored, free health insurance if their income fell between 100% and 138% of the federal poverty level. The program’s goal was to ultimately improve not just the coverage of insured, but also health outcomes for vulnerable populations.1 Being poor and sick increases the risk of mortality or morbidity, but theory and empirical evidence suggest that a lower cost of care will lead to greater health care use, and eventually better health2; however, improved health outcomes do not necessarily result from new insurance coverage or greater health care use in the general public.3 Still, Medicaid expansion was expected to improve the health of low-income individuals, specifically minority populations, given that men and women of color are disproportionately living near the federal poverty line.4 Health care providers therefore anticipated that lower-income African Americans, with chronic health conditions, such as breast cancer, would benefit from Medicaid expansion relative to White counterparts, ultimately decreasing racial health disparities in the long term.
Motivated by the stark racial disparity in breast cancer mortality, this study estimates the average treatment effect (ATE) of Medicaid expansion on the Black/White breast cancer mortality ratio. ATE can be calculated using a DID fixed-effects regression model, which mitigates the potential exogenous differences between states that did and did not expand Medicaid.5 DID exploits this variation in expansion status to evaluate the effect of a major policy. Although quasiexperimental analyses are widely used to evaluate public policy, few studies have used such methods to estimate the effect of health insurance access on health disparity ratios.
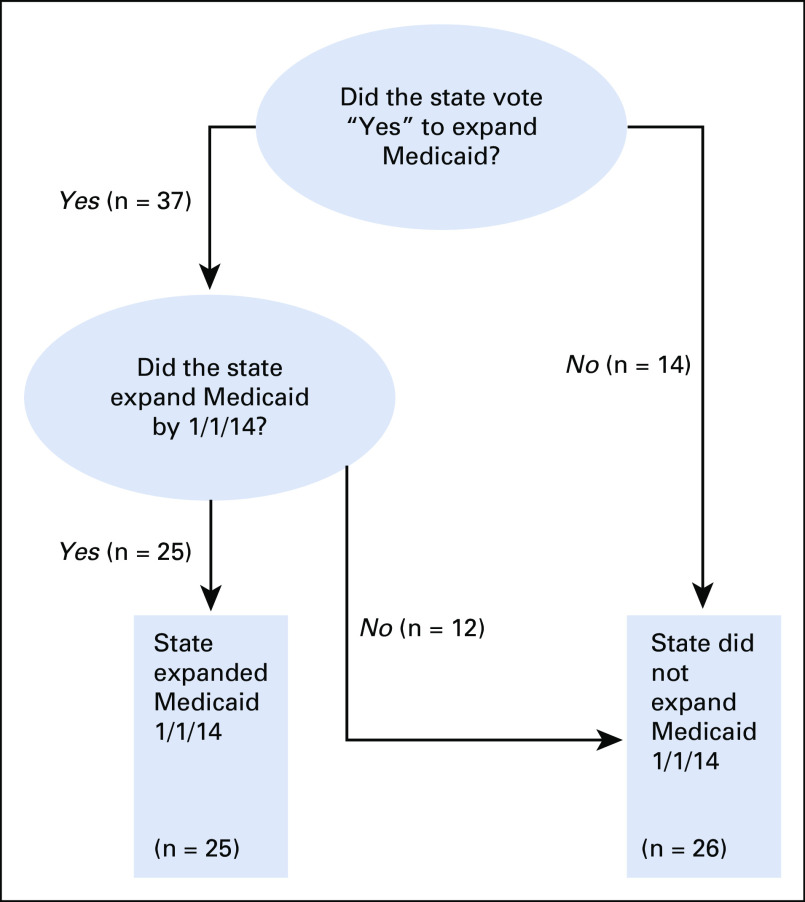
Health care reform has always been politically volatile, and Medicaid expansion was no exception. Originally, the Affordable Care Act mandated that all states expand public insurance coverage or forgo all federal Medicaid funds6; however, the Supreme Court declared this punitive measure unconstitutional in 2012.7 States were then allowed to freely decide whether to expand. Fourteen states outright voted against expansion, but even among the states voting to expand, there was significant heterogeneity in start dates, with some states yet to expand insurance coverage to this day.8 On January 1, 2014, 25 states expanded Medicaid. Along with the 14 dissenting states, 12 states that had voted to expand coverage were among the states not expanding on January 1, 2014 (Table 1 and Fig 1). This state-level variation provided an excellent opportunity for quasiexperimental analyses.
TABLE 1.
States Expanding Medicaid
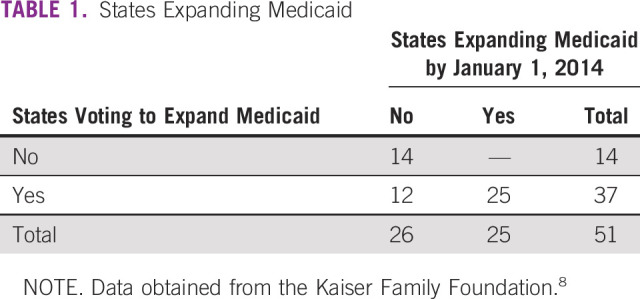
FIG 1.
Flowchart used to create the treatment and control groups for this analysis. As of August 2018, 37 states eventually chose to expand Medicaid. Among these states, the 25 that expanded Medicaid on January 1, 2014, are considered the treatment group. The 12 states expanding at a later date and the 14 states that never expanded Medicaid were considered the control group. In the second analysis, only states that eventually expanded, but did not expand by January 1, 2014, were included in the control group.
METHODS
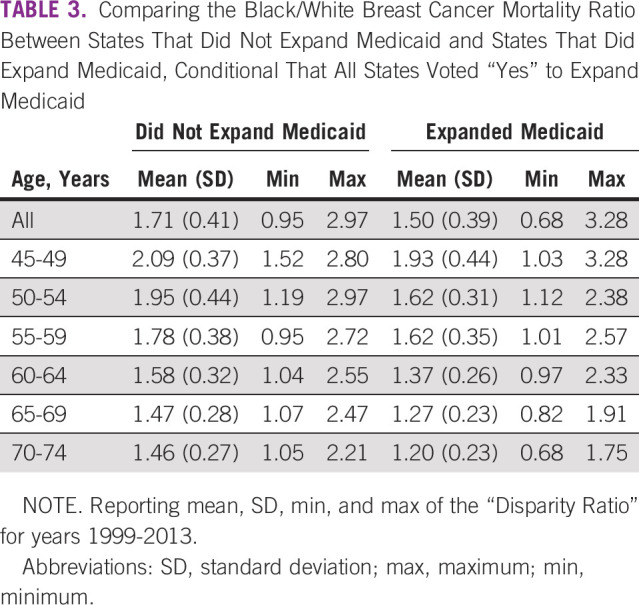
State-level breast cancer mortality data were obtained from the Centers for Disease Control and Prevention (CDC) All-Cause Mortality Database.9 Each states’ Medicaid expansion status was provided by a Kaiser Family Foundation white paper.8 States were coded as “Voted ‘yes’ to Expand Medicaid” and “Expanded Medicaid 1/1/14”. Statistical analyses were conducted using R software with the following packages: ggplot, tidyr, psych, plm, and Rmisc.10-16 First, mortality data were cleaned to recode states with suppressed values to “NA” (the CDC suppresses values less than 15). These observations were eventually dropped. Second, a “Disparity Ratio” was calculated by dividing the African American mortality rate by the White mortality rate. States with a zero disparity ratio were eliminated, as were outlier observations with a disparity ratio greater than 10. Two regression models were constructed. The first compares all expanding states with all nonexpanding states, and the second compares all expanding states with nonexpanding states that voted to expand but did not by January 2014. Fixed-effects and random-effects regression models were constructed for each specific age group. The DID regression model used the year 2014 as a washout period and compared 2012 to 2013 (pretreatment) with 2015 to 2016 (post-treatment). We used a Hausmann test to determine which model was most appropriate. A graph of expanding and nonexpanding states from 1999 to 2013 was presented to test the necessary common trend assumption (Data Supplement). Basic summary statistics were reported (Tables 2 and 3). DID estimators (ATE) and respective P values were reported for each age group. Non–Medicaid-eligible age groups were included as a pseudocontrol.
TABLE 2.
Comparing the Black/White Breast Cancer Mortality Ratio Between States That Did Not Expand Medicaid and States That Did Expand Medicaid
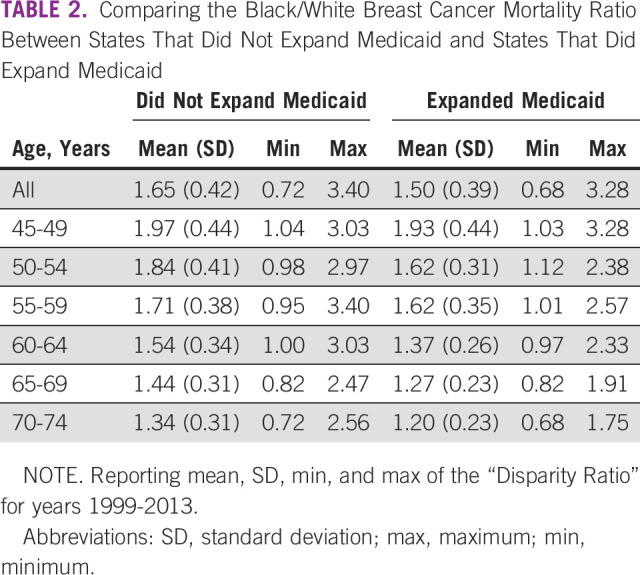
TABLE 3.
Comparing the Black/White Breast Cancer Mortality Ratio Between States That Did Not Expand Medicaid and States That Did Expand Medicaid, Conditional That All States Voted “Yes” to Expand Medicaid
RESULTS
There was no evidence that Medicaid expansion lowered the disparity in breast cancer mortality. This finding held true for both tests. The first regression model estimated the effect of Medicaid expansion by comparing the disparity in mortality between all expanding states and all nonexpanding states. This test showed that, in contrast to the expectation, the Black/White mortality ratio increased in states expanding Medicaid for all Medicaid-eligible age groups (Table 4 and Data Supplement). Disparity ratios in younger age groups demonstrated a significant increase. The Hausmann test result indicates the appropriateness of using a fixed-effects model. Still, the differences between the 2 models are negligible. Whereas the DID regression controls for exogenous effects between states, the second regression model more accurately estimates the effect of Medicaid expansion by eliminating some of the inherent political differences between expanding and nonexpanding states (Table 5 and Data Supplement). The second model included only states voting to expand Medicaid. Here, states that did in fact expand Medicaid on January 1, 2014, were compared with states that did not expand by that date. While obvious political differences remain between states that were able to expand in a timely manner or not, the results of this test seem to be less biased by partisan effects.
TABLE 4.
Effect of Medicaid Expansion on the Black/White Breast Cancer Mortality Ratio
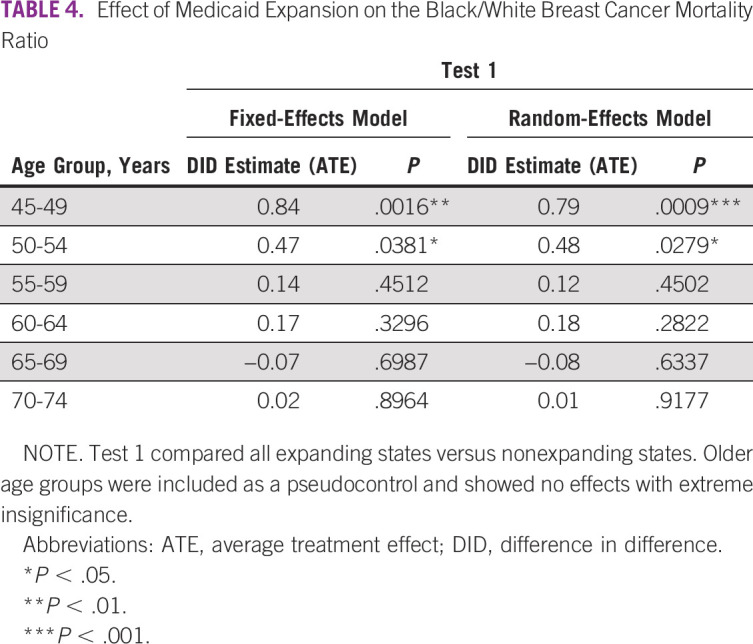
TABLE 5.
Effect of Medicaid Expansion on the Black/White Breast Cancer Mortality Ratio
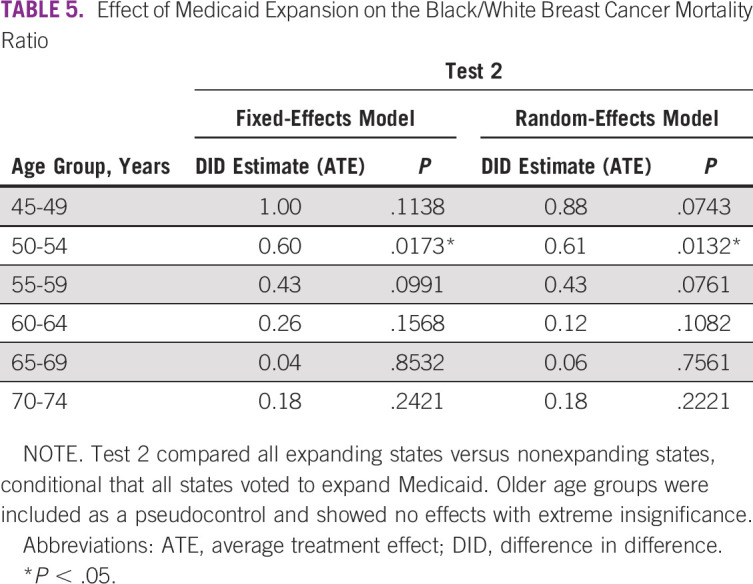
These results indicate that Medicaid expansion did not address the racial disparity in breast cancer mortality. Of most interest, Medicaid expansion led to greater inequality in younger age groups. In the age 50 to 54 years group, the disparity significantly increased after Medicaid expansion (estimate, 0.6; P = .017). The disparity in the age 45 to 49 years group also increased after expansion (estimate, 0.8; P = .001). Given the result of increasing disparities in younger age groups, these findings discouragingly suggest that spillover effects from Medicaid expansion may have further contributed to the detrimental inequality facing African American women with early-onset breast cancer.
DISCUSSION
Despite a lower incidence, African American women have higher breast cancer mortality than White women.17 This disparity is most stark among younger women, who not only face higher death rates, but more frequent diagnoses of triple-negative breast cancer.18,19 Whereas the overall disparity in breast cancer mortality has historically been attributed to a variety of genetic, behavioral, and social factors, the breast cancer disparity between young Black and White women has proven to be driven by systemic social and epigenetic differences.20 Given the persistent structural racism and the evidence that these epigenetic differences influence tumor biology, it would be naïve to assume that Medicaid expansion would completely eliminate cancer disparities. Still, 3 years after a major health policy that drastically increased access to care, at minimum we expected to observe a significant trend toward greater equity.
This study suggests, however, that Medicaid expansion may not have addressed the breast cancer mortality gap between Black and White women. The two leading explanations for this result center on assumptions of unequal access and quality: a lower proportion of African American women enrolled in Medicaid after expansion than did White women, and even though African American women were given access to free health insurance, the quality of the care available to this group was poor relative to the care available to White women. However, the purpose of this discussion is to dispute the two previous assumptions and introduce a third likely explanation—that the arrival of new Medicaid patients overloaded the capacity of health care providers, which disproportionately impeded breast cancer care for African American women in an already constrained, low-resource health system.
The likelihood of the first explanation hinges on the assumption that the cost of obtaining free health insurance differed between the two groups. Simply put, if enrolling in Medicaid required a higher cost than a woman expected to gain, those women would choose not to enroll. Furthermore, women of a traditionally underserved, minority group would in fact face higher nonmonetary costs as a result of such factors as housing segregation (a higher time cost to travel to the administrative agency), technology barriers (low access to online resources), or low system integration (a greater effort required to connect with enrollment services). Fortunately, these disparities in access were predicted by policymakers. The intrinsic design of the Affordable Care Act mitigated these potential barriers to enrollment. Substantial resources were spent on patient navigation, education, and outreach to prepare lower-resource communities for Medicaid expansion. And these efforts seem to have been effective, given the evidence showing that insurance coverage increased at nearly identical rates for both groups after Medicaid expansion.21 Whereas gaps in coverage could exist for individual states, in the aggregate there seems to be no difference in Medicaid expansion enrollment between Black and White women.
If insurance coverage did not differ between the two racial groups, the rise in disparity may have been affected by differences in the quality of cancer care. Care quality varies significantly throughout the US health system and at multiple levels: by geography (between states, counties, and municipalities) or type of health facility (private, public, or academic), and even between physicians within a single health care organization.22-28 This variation in quality especially affects racial minorities.29,30 No matter what country, health system, or disease metric, low-quality care significantly drives preventable deaths31; however, whereas the literature on quality-of-care variation is robust, the effect of this variation is less well understood. Are people better off receiving no care if that care is deemed to be of low quality? What are the most important quality measures to prevent cancer mortality? These kinds of questions remain unanswered. More so, to cause the significant change in disparity reported in breast cancer mortality after Medicaid expansion, there would need to be a decidedly observable variation in the quality of care between races for all newly enrolled Medicaid recipients. Even if every newly insured woman received high- or low-quality cancer care that corresponded with their respective race, the number of potential cases simply cannot explain observable, population-level disparity change.
The first two explanations explored the effect of Medicaid expansion for new enrollees. The shortsightedness of these approaches becomes apparent when considering the effect of Medicaid expansion on the entire US health care system. Thirteen million previously uninsured people legitimately entered the American health care system, essentially overnight; however, enrollment was not evenly distributed throughout each expanding state. Instead, given the income requirements of expansion enrollment, historic segregation policies, and the propensity for similar people to live in close proximity, these newly insured patients were heavily concentrated in low-resources areas, which are home to low-resource health systems. This drastic influx strained the capacity of health care providers, with the magnitude of the effect increasing with higher proportions of low-income, minority populations.32,33 Longer wait times, scheduling difficulties, and loss of physician continuity dramatically affect patient outcomes, especially for patients with chronic diseases. Because the current study included all breast cancer deaths, not just those of Medicaid patients, so too should the exploration of potential causes. Rather than unequal access or low-quality breast cancer treatment, the higher disparity after Medicaid expansion should be attributed to low-quality health systems—and so should the attention for reform.
This analysis is not without limitations. The primary critique rests on the data used to conduct this analysis. Three years of mortality data may not be enough to precisely measure any true impact of a policy. Moreover, a stronger dependent variable would be to calculate the Black/White mortality-incidence ratio.34 The mortality-incidence ratio divides the mortality rate by the incidence rate. This measure would more accurately identify states with a higher mortality burden in the current study; however, while these data would be more precise, they are simply not available. SEER data lags by 4 years, and whereas some statisticians estimate present-day mortality and incidence rates, those estimates serve to influence surveillance efforts, not policy evaluation. Given the data constraints, this specific limitation is less critical to interpreting the reported results and should instead motivate continued analysis as more data become available.17
Also with regard to the data, the low number of mortality cases in younger age groups decreases the power of each regression model. The CDC policy to suppress values less than 15, along with the removal of outliers, creates a smaller pool of states to analyze in these younger age groups. This limitation is especially present in the second regression model for the age 45 to 49 years group, hindering our ability to confidently infer the increased disparity after Medicaid expansion. The second model attempts to eliminate the bias introduced from political differences between expanding and nonexpanding states, but this results in fewer data points. To overcome this potential limitation, both regression models 1 and 2 were reported, from which no drastic differences in interpretation occur.
There was no attempt to control for other state-wide variables that may contribute to breast cancer mortality or racial inequality. This is less a limitation and more a function of the DID methodology. DID methodology controls for exogenous, time-in-variant effects between states; therefore, even if states have significantly different health care systems or income distributions, those variables are controlled for in a DID analysis. Although time-variant variables could yield a more precise estimate of the policies’ effect, the addition of a post-treatment variable would bias the results of the model. For example, state government spending or mammography rates may change over time and seem like reasonable contributors to a state’s breast cancer mortality; however, these two variables are likely to be affected by Medicaid expansion, along with the dependent variable. Adding these two confounders would simply bias the model. That said, future analyses could attempt to control for time-variant, nontreatment effects, but this was outside the scope of the current study.
In conclusion, investigators should use proven quasiexperimental methods to analyze the effect of policy variation on health disparities. Policymakers must consider institutional factors that may limit minority groups from benefiting from macrochanges in health policy. As SEER data become available in the coming years, research should investigate the effect of Medicaid expansion on breast cancer disparities in mortality, incidence, and screening for specific age groups, as well as stage and type of breast cancer diagnosis and family history. Robust analysis of specific states or health care systems could stratify outcomes by Medicaid status before and after expansion. Investigators should continue to use health system variation to identify macromechanisms that influence health disparities. Future research on cancer disparities must consider factors that limit a group’s ability to benefit from changes in health policy. Researchers and policymakers must give greater attention to improving the quality of local health systems.
PRIOR PRESENTATION
Presented at the 7th Annual Cancer Symposium, Chicago, IL, March 7, 2019.
SUPPORT
Funded by Susan G. Komen Grant No. GTDR16376189 and National Cancer Institute SPORE Grant No. 1P20CA233307.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Financial support: Olufunmilayo Olopade
Administrative support: Olufunmilayo Olopade
Collection and assembly of data: Jason Semprini
Data analysis and interpretation: Jason Semprini
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/site/misc/authors.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Olufunmilayo Olopade
Employment: CancerIQ (I)
Leadership: CancerIQ
Stock and Other Ownership Interests: CancerIQ, Tempus
Research Funding: Novartis (Inst), Genentech (Inst)
Other Relationship: Tempus, Color Genomics, Genentech, Bio Ventures for Global Health
Uncompensated Relationships: Healthy Life for All Foundation
Open Payments Link: https://openpaymentsdata.cms.gov/physician/olopade
No other potential conflicts of interest were reported.
REFERENCES
- 1.Hahn JA, Sheingold BH. Medicaid expansion: The dynamic health care policy landscape. Nurs Econ. 2013;31:267–272, 297. [PubMed] [Google Scholar]
- 2.Aron-Dine A, Einav L, Finkelstein A. The RAND health insurance experiment, three decades later. J Econ Perspect. 2013;27:197–222. doi: 10.1257/jep.27.1.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment: Effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368:1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Census Bureau Poverty by race. https://www.census.gov/library/publications/2013/acs/acsbr11-17.html
- 5.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: The difference-in-differences approach. JAMA. 2014;312:2401–2402. doi: 10.1001/jama.2014.16153. [DOI] [PubMed] [Google Scholar]
- 6.Rosenbaum S, Westmoreland TM. The Supreme Court’s surprising decision on the Medicaid expansion: How will the federal government and states proceed? Health Aff (Millwood) 2012;31:1663–1672. doi: 10.1377/hlthaff.2012.0766. [DOI] [PubMed] [Google Scholar]
- 7.US Supreme Court National Federation of Independent Business et al v. Sebelius. https://www.supremecourt.gov/opinions/11pdf/11-393c3a2.pdf
- 8.Kaiser Family Foundation Status of State Action on the Medicaid Expansion Decision. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/
- 9.Centers for Disease Control and Prevention CDC WONDER: 1999-2016 mortality. http://wonder.cdc.gov/cancer-v2014.html [PubMed]
- 10.R Foundation for Statistical Computing R: A language and environment for statistical computing. http://www.r-project.org/
- 11.Wickham H. tidyr: Easily tidy data. https://CRAN.R-project.org/package=tidyr
- 12.Wickham H. ggplot2: Elegant Graphics for Data Analysis. New York, NY: Springer-Verlag; 2016. [Google Scholar]
- 13.Revelle W. psych: Procedures for Personality and Psychological Research. Evanston, IL: Northwestern University; 2018. https://CRAN.R-project.org/package=psych [Google Scholar]
- 14.Millo G. Robust standard error estimators for panel models: A unifying approach. J Stat Soft. 2017;82:1–27. [Google Scholar]
- 15.Croissant Y, Millo G. Panel data econometrics in R: The plm package. J Stat Soft. 2008;27:1–43. [Google Scholar]
- 16.Hope RM. Rmisc: Ryan miscellaneous. R package version 1.5. https://CRAN.R-project.org/package=Rmisc
- 17.DeSantis CE, Ma J, Goding Sauer A, et al. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin. 2017;67:439–448. doi: 10.3322/caac.21412. [DOI] [PubMed] [Google Scholar]
- 18.Chollet-Hinton L, Olshan AF, Nichols HB, et al. Biology and etiology of young-onset breast cancers among premenopausal African American women: Results from the AMBER Consortium. Cancer Epidemiol Biomarkers Prev. 2017;26:1722–1729. doi: 10.1158/1055-9965.EPI-17-0450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sturtz LA, Melley J, Mamula K, et al. Outcome disparities in African American women with triple negative breast cancer: A comparison of epidemiological and molecular factors between African American and Caucasian women with triple negative breast cancer. BMC Cancer. 2014;14:62. doi: 10.1186/1471-2407-14-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daly B, Olopade OI. A perfect storm: How tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J Clin. 2015;65:221–238. doi: 10.3322/caac.21271. [DOI] [PubMed] [Google Scholar]
- 21.Artiga S, Foutz J, Published AD. Health coverage by race and ethnicity: Changes under the ACA—Issue brief. The Henry J. Kaiser Family Foundation; https://www.kff.org/report-section/health-coverage-by-race-and-ethnicity-changes-under-the-aca-issue-brief/ [Google Scholar]
- 22.Fisher ES, Wennberg DE, Stukel TA, et al. The implications of regional variations in Medicare spending. Part 1: The content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 23.Fisher ES, Wennberg JE. Health care quality, geographic variations, and the challenge of supply-sensitive care. Perspect Biol Med. 2003;46:69–79. doi: 10.1353/pbm.2003.0004. [DOI] [PubMed] [Google Scholar]
- 24.Wennberg JE, Peters PG., Jr Unwarranted variations in the quality of health care: Can the law help medicine provide a remedy/remedies? Spec Law Dig Health Care Law. 2002;37:9–25. [PubMed] [Google Scholar]
- 25.Skinner J, Chandra A, Goodman D, et al. The elusive connection between health care spending and quality. Health Aff (Millwood) 2009;28:w119–w123. doi: 10.1377/hlthaff.28.1.w119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weeks WB, Gottlieb DJ, Nyweide DE, et al. Higher health care quality and bigger savings found at large multispecialty medical groups. Health Aff (Millwood) 2010;29:991–997. doi: 10.1377/hlthaff.2009.0388. [DOI] [PubMed] [Google Scholar]
- 27.Birkmeyer JD, Gust C, Dimick JB, et al. Hospital quality and the cost of inpatient surgery in the United States. Ann Surg. 2012;255:1–5. doi: 10.1097/SLA.0b013e3182402c17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hines S, Joshi MS. Variation in quality of care within health systems. Jt Comm J Qual Patient Saf. 2008;34:326–332. doi: 10.1016/s1553-7250(08)34041-0. [DOI] [PubMed] [Google Scholar]
- 29.Bynum JPW, Fisher ES, Song Y, et al. Measuring racial disparities in the quality of ambulatory diabetes care. Med Care. 2010;48:1057–1063. doi: 10.1097/MLR.0b013e3181f37fcf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lewis VA, Fraze T, Fisher ES, et al. ACOs serving high proportions of racial and ethnic minorities lag in quality performance. Health Aff (Millwood) 2017;36:57–66. doi: 10.1377/hlthaff.2016.0626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kruk ME, Gage AD, Joseph NT, et al. Mortality due to low-quality health systems in the universal health coverage era: A systematic analysis of amenable deaths in 137 countries. Lancet. 2018;392:2203–2212. doi: 10.1016/S0140-6736(18)31668-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Polsky D, Candon M, Saloner B, et al. Changes in primary care access between 2012 and 2016 for new patients with Medicaid and private coverage. JAMA Intern Med. 2017;177:588–590. doi: 10.1001/jamainternmed.2016.9662. [DOI] [PubMed] [Google Scholar]
- 33.Miller S, Wherry LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376:947–956. doi: 10.1056/NEJMsa1612890. [DOI] [PubMed] [Google Scholar]
- 34.Choi E, Lee S, Nhung BC, et al. Cancer mortality-to-incidence ratio as an indicator of cancer management outcomes in Organization for Economic Cooperation and Development countries. Epidemiol Health. 2017;39:e2017006. doi: 10.4178/epih.e2017006. [DOI] [PMC free article] [PubMed] [Google Scholar]