Abstract
Background
Caregivers of children with fetal alcohol spectrum disorders (FASD) have elevated levels of stress, which can negatively impact family functioning and caregivers’ mental and physical health. Self-care is a critical resource to address caregivers’ stress.
Aims
This study describes strategies and obstacles related to self-care reported by caregivers of children with FASD. It also examines how caregivers’ perceived confidence in and frequency of self-care is related to stress, parenting attitudes, and family needs.
Methods & Procedures
Forty-six caregivers of children with FASD identified self-care strategies and obstacles and rated their confidence and frequency of self-care. Additional measures of perceived parenting efficacy, stress, family needs, child behavior, and family demographics were administered. Correlation analyses examined associations between self-care and measures of child and family functioning.
Results
Self-care strategies and obstacles were varied. Greater reported confidence in self-care was associated with less parental distress and more satisfaction in the parenting role. Frequency of self-care was positively associated with confidence in self-care but not with any other measure of family functioning.
Conclusions
Caregivers use a variety of strategies and face significant obstacles in self-care. Confidence in self-care may be associated with lower stress and greater satisfaction in the parenting role.
Keywords: Fetal alcohol spectrum disorders, prenatal alcohol exposure, fetal alcohol syndrome, self-care, stress, parenting
1. Introduction
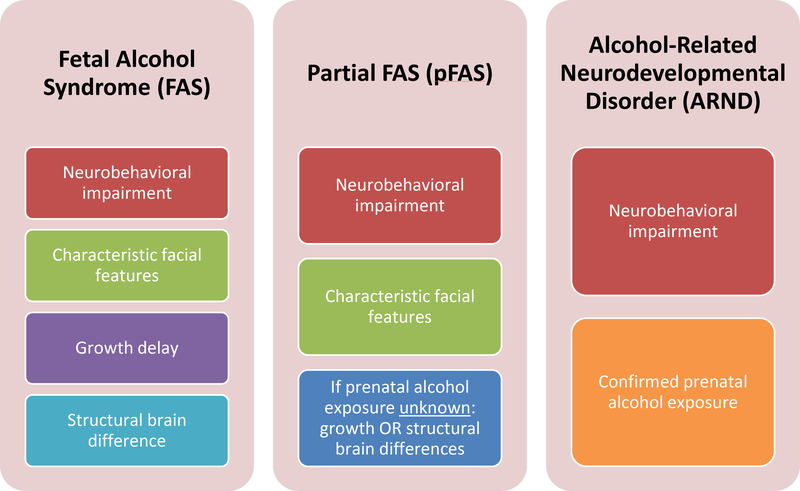
Fetal alcohol spectrum disorders (FASD) represent a range of neurological and physical symptoms associated with prenatal alcohol exposure (PAE) and affect approximately 2–5% of children in the US (May et al., 2018). An evaluation for FASD includes assessment of prenatal alcohol exposure, characteristic facial features, growth deficiency, deficient brain growth, and neurobehavioral impairment; the specific FASD diagnosis rendered depends on the constellation of symptoms present (see Figure 1; Hoyme et al., 2016). It is important to recognize that neurobehavioral impairment is the one consistent symptom across the primary FASD diagnoses and has the most significant impact on everyday functioning. Although the criteria for fetal alcohol syndrome (FAS) have largely remained consistent since it was first recognized in the US in 1973 (Jones & Smith, 1973), characterization of other conditions on the spectrum and refinement of criterion cutoffs continue to evolve to maximize sensitivity and specificity (Warren, Hewitt, & Thomas, 2011).
Figure 1.
Diagnostic categories under the classification of fetal alcohol spectrum disorders (FASD) according to Hoyme et al., 2016.
Children diagnosed with FASD have many diverse and unique strengths (Brown, Rodger, George, St Arnault, & Sintzel, 2008; Olson, Oti, Gelo, & Beck, 2009), but also can face lifelong cognitive and behavioral impairments, as well as high rates of mental health disorders and other life problems (Streissguth et al., 2004). Caregivers of children with FASD face numerous system barriers, lack of awareness and resources, and other obstacles in raising their children (Olson et al., 2009; Petrenko, Tahir, Mahoney, & Chin, 2014). These barriers contribute to high levels of stress in caregivers of children with FASD, despite the many protective actions these caregivers take to support their children (Petrenko, Alto, Hart, Freeze, & Cole, 2019).
Although caregivers report important rewards, research has documented high levels of stress related to parenting a child with a disability (Smith, Oliver, & Innocenti, 2001; Baker et al. 2003; Paley, O’Connor, Kogan, & Findlay, 2005; Webster, Majnemer, Platt, & Shevell, 2008; Bobbitt et al., 2016). Research suggests parenting children with FASD may be especially stressful. Olson et al. (2009) found that in a study of 52 primary caregivers of children with prenatal alcohol exposure, 92% reported clinically elevated child-related stress (Olson et al., 2009). Caregivers of children with FASD may even experience more stress than those of children with other developmental disorders, including autism spectrum disorder (ASD; Watson, Coons, & Hayes, 2011). This is especially notable as ASD has consistently been associated with high caregiver stress (Dumas, Wolf, Fisman, & Culligan, 2009; Estes et al., 2009). Specifically, one study found that caregivers of children with FASD reported significantly higher levels of stress than did caregivers of children with ASD (Watson, Coons, & Hayes, 2011). Although both groups identified stressors in qualitative interviews relating to the diagnostic process, dealing with behavioral issues, and the need for advocacy, the nature of these stressors was different between groups (Watson, Hayes, Coons, & Radford-Paz, 2013). Specifically, the ASD diagnostic process often involved doctors minimizing parents’ concerns and long waitlists to see multiple providers, whereas the FASD diagnostic process required traveling long distances to find a knowledgeable provider and challenges verifying maternal drinking and getting a diagnosis when facial features were absent. In terms of behavioral issues, parents of children with ASD emphasized stressful behavioral issues such as temper tantrums and rigidity. In contrast, parents of children with FASD were especially worried about how current behaviors might possibly lead to incarceration or other secondary conditions in the future. Although both groups described the need for advocacy, the FASD group reported having to educate teachers and providers about the condition, which was not the case for ASD (Watson et al., 2013). Finally, early family stress can lead to difficulty in children’s adjustment later in life (Abidin, 1992). Taken together, these studies underscore the importance of finding stress management techniques for this population, especially given the high level of stress in families of children with FASD (Olson et al., 2009) and the negative impact of stress on children’s adjustment and functioning (Abidin, 1992).
Research supports a transactional relationship between parent stress and child problem behavior; parental stress contributes to child behavior problems which in turn contribute to parental stress (Baker et al., 2003). Studies have shown a clear association between increased problem behavior in young children and high child-focused parental stress for both mothers and fathers (Creasey & Jarvis, 1994; Myers & Taylor, 1998; Smith et al., 2001; Paley et al., 2005; Paley, O’Connor, Frankel, & Marquardt, 2006; Jirikowic, Olson, & Astley, 2012). This relationship has been shown to be moderated by maternal social support and mediated by caregivers’ cognitive appraisal of the responsibilities of caregiving (Plant & Sanders, 2007). Additionally, parental stress can have ripple effects into adolescence, especially in adjustment and peer relations (Conger, Patterson, & Ge, 1995).
Parental stress has been shown to have an effect on attitudes around the parenting role. Parents who are more stressed tend to have feelings of decreased parental efficacy, decreased confidence in parenting, and lower satisfaction in the parenting role (McBride, 1989; Hassall, Rose, & McDonald, 2005; Ngai & Chan, 2012; Renner, Whitney, & Easton, 2015). Evidence is mixed on the association between parental satisfaction and child problem behavior. Some studies show that parental role satisfaction is not linked with increased child problem behavior (Hill & Rose, 2009). However, some other studies show that as children’s problem behaviors increase, parental role satisfaction decreases (Johnston & Mash, 1989; Gilmore & Cuskelly, 2012). In sum, stress affects how parents think about their role as a parent, especially how confident and satisfied they feel about parenting. Child problem behavior may also affect parental satisfaction.
Stress reduction is important for all parents. But stress reduction interventions may be especially critical in caregivers of children with special needs given their documented high stress levels. Some stress-reduction interventions, such as behavioral parent training and coping skills education, have shown promise in reducing stress in parents of children with developmental disabilities (Singer, Ethridge, & Aldana, 2007; Lindo, Kliemann, Combes, & Frank, 2016). Interventions that combine these two methods are highly effective in stress reduction (Singer et al., 2007), indicating these types of interventions may have an additive effect when conducted together. Recently, mindfulness interventions have also been shown to significantly reduce stress in parents of children with developmental delay (Neece, 2014; Bazzano et al., 2015). Though standard services such as respite care and case management may slightly reduce stress, targeted stress-reduction interventions have a larger effect on parental stress-reduction (see Hastings & Beck, 2004 for a review).
Although the caregiving burden of a child with a disability and the negative effects of stress on parental behavior and parental role satisfaction have been established, little research has been conducted on how caregivers care for themselves. Styles of coping used by parents of children with disabilities have been explored, including active-avoidance coping, problem-focused coping, positive coping, and religious/denial coping (Hastings et al., 2005). However, few studies have investigated what specific strategies parents use to cope. Social support has been commonly reported as a coping strategy for parents (Beresford, 1994; Heaman, 1995; Jones & Passey, 2005). Higher social support has been associated with higher satisfaction in parenting, higher family and parental well-being, and lower stress. Parent social support has been found to predict parent stress better than child functioning (Smith et al., 2001). Some have proposed a model in which social support mediates the effect of parent stress on parent well-being, family functioning, and even child outcomes (Armstrong, Birnie-Lefcovitch, & Ungar, 2005). Other coping strategies may include exercise or meditation (Hansmann, Hug, & Seeland, 2007; Neece, 2014; Bazzano et al., 2015), but have not been well studied in parents of children with developmental disabilities.
Self-care is a critical resource for not only caregivers’ own physical and mental health but also for the benefit of their children. As discussed above, limited research has been done on parents’ self-care strategies, and of that no research has examined specific self-care strategies in caregivers of children with FASD. The current study aimed to elucidate how caregivers of children with FASD feel about their own self-care, what they do for self-care, and obstacles they may face in doing so. An additional goal was to identify how measures of self-care were associated with indicators of family functioning, including caregiver stress, satisfaction in the parenting role, and child behavior. Results from this study could inform intervention development for stress reduction in families raising children with FASD.
2. Methods
2.1. Participants
Forty-six caregivers (ages 31–65) of children with FASD participated in this study. Participants were originally recruited as part of two separate intervention trials investigating family-focused interventions for FASD. Intervention trial 1 was a small-scale pilot randomized controlled trial of a multi-component intervention. Trial 2 was a community replication trial of a parent consultation program. For both trials, study information was shared with local providers and agencies serving children with FASD and within family support groups and conferences. Interested families then contacted the research team. At the time of screening, families reported they were primarily referred by local clinicians. To be included in analyses for the current study, participants had to have a child with a diagnosis of an FASD or confirmed prenatal alcohol exposure (PAE) between the ages of 3 and 12. Diagnosis was determined as part of the intervention trials and/or based on review of records from prior FASD evaluations. Further participant characteristics can be found in Table 1.
Table 1.
Participant demographics.
| Demographic Variable | Value |
|---|---|
| Caregiver Age Mean (SD) | 45.78 (8.00) |
| Caregiver Biological Sex Frequency (%) | |
| Female | 41 (89.1) |
| Caregiver Race/Ethnicity (non-exclusive categories) Frequency (%) | |
| Caucasian/White | 41 (89.1) |
| African American/Black | 5 (10.9) |
| Hispanic/Latino | 1 (2.2) |
| Native American | 3 (6.5) |
| Other | 1 (2.2) |
| Caregiver Type Frequency (%) | |
| Biological parent | 1 (2.2) |
| Relative of child | 7 (15.2) |
| Adoptive parent | 32 (69.5) |
| Non-relative foster care | 6 (13.0) |
| Caregiver Marital Status Frequency (%) | |
| Single, never married | 3 (6.5) |
| Separated/divorced | 8 (17.4) |
| Married or living with partner | 34 (73.9) |
| Not reported | 1 (2.2) |
| Caregiver Educational Attainment Frequency (%) | |
| High school diploma or less | 7 (15.2) |
| Some college or Associate’s degree | 13 (28.3) |
| Bachelor’s degree | 11 (23.9) |
| Master’s degree or higher | 13 (28.3) |
| Not reported | 2 (4.3) |
| Annual Family Income Frequency (%) | |
| Less than 35,000 | 4 (8.7) |
| 35,000–49,999 | 5 (10.9) |
| 50,000–74,999 | 9 (20.0) |
| 75,000–99,999 | 14 (30.4) |
| More than 100,000 | 12 (26.1) |
| Not reported | 2 (4.3) |
| Child Age Mean (SD) | 6.21 (1.59) |
| Child Age Range | 3.0–8.8 |
| Child Biological Sex Frequency (%) | |
| Female | 13 (28.3) |
| FAS/pFAS Diagnosis Frequency (%) | 20 (43.5) |
| ARND Frequency (%) | 26 (56.5) |
| Child Other Conditions Frequency (%) as reported by parents | |
| Attention Deficit Hyperactivity Disorder | 37 (80.4) |
| Behavioral or Emotional Problems | 40 (87.0) |
| Learning Problems | 30 (65.2) |
| Speech or Language Problems | 24 (52.2) |
| Mental Retardation/Developmental Delay | 20 (43.5) |
| Physical Disability, Orthopedic or Neurological Problem | 17 (37.0) |
2.2. Procedures
The University Institutional Review Board reviewed and approved all study procedures and informed consent was obtained from all participants. At baseline research visits (prior to intervention), participants completed interviews and questionnaires. Research visits for 31 participants (intervention trial 1) were completed in the laboratory. Participants from intervention trial 2 (n=15) completed questionnaires in their home.
2.3. Measures
2.3.1. Self Care Assessment (SCA)
Caregivers completed a self-report measure of various aspects of engagement in self-care developed for this study. The measure consisted of 4 items assessing confidence in taking care of oneself, identification of self-care strategies, frequency of self-care, and identification of obstacles or barriers to utilizing self-care strategies. First, participants were asked to rate their ability/confidence in maintaining self-care on a 5-point scale ranging from “none” to “a great deal”, with higher scores indicating higher confidence in self-care abilities. Next, participants were asked to list the top 5 self-care strategies they engaged in the most often. Participants then reported on the frequency of their use of self-care strategies on an 8-point scale ranging from “rarely (less than once a month)” to “multiple times per day”, again with higher scores indicating a higher frequency of self-care. Finally, participants were asked to list the top 5 obstacles which got in the way of utilizing self-care strategies.
2.3.2. Family Needs Met Questionnaire (FNM)
The Family Needs Met Questionnaire (Olson et al., 2009) is based on a measure developed for traumatic brain injury (Kreutzer, Marwitz, & West, 1988). The measure includes items relating to common needs of parents and caregivers of children with alcohol-related disabilities and assesses the degree to which caregivers perceive these needs have been met. Each need is rated on a 4-point scale (1=not at all met, 4=a great deal met). The total score reflects the average response across items. Internal consistency in the current sample was high (α=.94).
2.3.3. Eyberg Child Behavior Inventory (ECBI)
The ECBI (Eyberg & Pincus, 1999) is a rating scale measuring conduct problems in children ages 2 through 16. The ECBI consists of 36 items that are each rated on a 7-point Intensity scale to indicate the frequency of the behavior, as well as a Yes-No Problem scale to indicate whether or not the behavior is problematic for the parent. The current study focuses on the intensity scale, which has demonstrated high internal consistency (α=.95) and construct validity for children and adolescents (Eyberg & Pincus, 1999). Scores are presented as T-scores (M=50, SD=10), with higher scores indicating higher frequency behavior problems. Internal consistency in the current sample was high (α=.93).
2.3.4. Parenting Sense of Competence (PSOC)
The PSOC (Johnston & Mash, 1989) is a 16-item self-report measure of the parent’s sense of parenting efficacy and satisfaction. The items in the PSOC are answered on a 6-point scale ranging from “strongly disagree” to “strongly agree”. The scale assesses two factors: Satisfaction, or extent to which the individual enjoys the parenting role and parenting frustration and anxiety; and Efficacy, or perceived competence, problem solving ability, and capability. Higher scores indicate higher feelings of satisfaction or efficacy. The measure has demonstrated adequate internal consistency scores for both the Efficacy (α=.76) and Satisfaction (α=.75) scales as well as adequate validity (Johnston & Mash, 1989). Internal consistency in the current sample was acceptable for both the Efficacy scale (α=.71) and the Satisfaction scale (α=.76).
2.3.5. Parenting Stress Index, fourth edition, short form (PSI-4-SF)
The PSI-4-SF (Abidin, 2012) is a 36-item, abbreviated inventory evaluating the magnitude of stress in the parent-child system. The PSI-4-SF is made up of three domains, including Parental Distress (PD), Parent-Child Dysfunctional Interaction (PCDI), and Difficult Child (DC). Scores are presented as T-scores (M=50, SD=10), with higher scores reflecting greater levels of stress. The PSI-4-SF has demonstrated adequate internal consistency for all three scales (PD α=.90; PCDI α=.89; DC α=.88) and validity (Abidin, 2012). Internal consistency in the current sample was high for all three scales (PD α=.90; PCDI α=.87; DC α=.83).
2.4. Data Analyses
Data were entered into SPSS and manually rechecked. The primary aim of the current study was to document the self-care experiences of families raising children with FASD and examine the inter-relations between self-care and indices of child and family functioning. As a result, analyses were descriptive in nature. Correlational analyses examined associations between self-care confidence and frequency and measures of child and family functioning. Self-care strategies and obstacles were examined and categories to provide additional description of common strategies and obstacles faced by families.
Self-care strategies and obstacles were categorized based on key words and themes that emerged throughout the process of coding. Two independent raters aggregated each participant’s responses based on similar or identical responses of key words together. Grouping of responses yielded independent categories for both self-care strategies and common obstacles.
3. Results
3.1. Descriptives of Sample
Descriptives are presented in Table 2. All variables approximated a normal distribution (skew values ranged from −0.84–0.99; kurtosis values ranged from −0.79–2.22). Parental distress, parent-child dysfunctional interaction, and difficult child-related stress are presented as T scores with a mean of 50 and SD of 10. Means and standard deviations for parental satisfaction and parental efficacy are generally in line with normative data (Johnston & Mash, 1989). A T score on the ECBI above 60 is considered clinically significant (Eyberg & Pincus, 1999), indicating the current sample showed elevated problem behavior scores on average. On the PSI, a T score from 60–62 indicates high stress and a score of 63 or above indicates clinically significant levels of stress. On average, the current sample showed high levels of stress on the difficult child-related stress subscale of the PSI.
Table 2.
Descriptive statistics for study variables.
| Measure | Mean | SD | Range |
|---|---|---|---|
| SCA: Confidence in Self-Care Abilities | 3.5 | .96 | 1–5 |
| SCA: Frequency of Self-Care | 5.0 | 2.0 | 1–8 |
| PSOC: Parenting Satisfaction | 35.37 | 6.74 | 22–51 |
| PSOC: Parental Efficacy | 20.74 | 5.27 | 9–33 |
| PSI-4: Parental Distress | 51.46 | 10.25 | 34–79 |
| PSI-4: Parent Child Dysfunctional Interaction | 55.59 | 12.04 | 18–76 |
| PSI-4: Difficult Child-R elated Stress | 62.17 | 11.61 | 35–84 |
| Family Needs Met | 2.80 | .71 | 1.15–4 |
| ECBI: Intensity Child Problem Behavior | 66.96 | 9.70 | 47–90 |
Abbreviation: SCA: Self Care Assessment; PSOC: Parenting Sense of Competence; PSI-4: Parenting Stress Index, Fourth Edition; ECBI: Eyberg Child Behavior Inventory
3.2. Correlational Analyses
Pearson’s correlation coefficients were computed to investigate the relationships between confidence in and frequency of self-care and measures of child and family functioning. Correlational results are shown in Table 3. Caregivers with greater confidence in self-care abilities were significantly more likely to report higher satisfaction in parenting, lower parental distress, and more family needs being met. They were also more likely to report lower difficult child-related stress, an association which approached significance (p=.07). Caregiver ratings of abilities and confidence were significantly correlated with caregiver report of how often they engaged in self-care; however, caregiver report of how often they engaged in self-care was not significantly correlated with any other measure. Caregiver ratings of abilities and confidence were not significantly correlated with caregiver ratings of child behavior, perceived parenting efficacy, or parent-child dysfunctional interaction. Neither caregiver ratings of abilities and confidence nor caregiver ratings of frequency of self-care were significantly correlated with child age or gross family household income. Additionally, parental role satisfaction was negatively correlated with all subscales on the PSI (parental distress, parent-child dysfunctional interaction, and difficult child-related stress), and child problem behavior. The association between parental distress approached significance criterion with child behavior problems (p=.07), with higher problem behaviors relating to higher parent stress.
Table 3.
Correlation table for relevant study variables.
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Confidence in Self-Care Abilities | .36** | .35** | −.18 | −.33* | −.21 | −.27 | .48** | −.20 | −.08 | −.16 |
| 2. Frequency of Self-Care | -- | .04 | −.29 | .01 | −.09 | .08 | .12 | −.04 | .06 | −.24 |
| 3. Parenting Satisfaction | -- | −.24 | −.63** | −.48** | −.58** | .45** | −.48** | −.31* | .10 | |
| 4. Parental Efficacy | -- | .23 | .08 | .06 | −.42** | −.08 | −.09 | .54** | ||
| 5. Parental Distress | -- | .53** | .58** | −.42** | .27 | .18 | −.09 | |||
| 6. Parent Child Dysfunctional Interaction | -- | .62** | −.45** | .60** | .24 | −.21 | ||||
| 7. Difficult Child-Related Stress | -- | −.37 | .74** | .30* | −.17 | |||||
| 8. Family Needs Met | -- | −.26 | −.18 | −.08 | ||||||
| 9. Child Problem Behavior | -- | .32* | −.18 | |||||||
| 10. Child Age | -- | .07 | ||||||||
| 11. Family Income | -- |
Note:
=.01
=.05
3.3. Self-Care Strategies and Obstacles
Self-care strategies fell into seven overarching categories which were: being present, seeking social support, maintaining physical health, engaging in hobbies, consuming media, treating oneself to small luxuries, and seeking information. These categories and example responses are presented in Table 4.
Table 4.
Categories and definitions for caregivers’ strategies for self-care. Caregivers could list up to five self-care strategies. The number of parents who reported using at least one strategy in the relevant category are listed below category names.
| Code | Description | Example |
|---|---|---|
| Being Present (34 caregivers, 73.9%) | Parent references an activity focused on quiet time, time alone, or time in nature. Included in this category was spirituality and religious activities. | • Meditation • Yoga • Spending time in nature • “Me time” • Prayer |
| Maintaining Physical Health (31 caregivers, 67.4%) | Parent references being active or healthy eating, or other method of maintaining health. | • Exercise • Take walk • Sleep • Eat healthier |
| Seeking Social Support (25 caregivers, 54.3%) | Parent references spending time with or talking to loved ones, or reaching out for professional or specialized support. | • Spend time with friends • Spend time with partner • Go to a support group • Talk to a counselor |
| Engaging in Hobbies (18 caregivers, 39.1%) | Parent references participating in a hobby or favored activity. | • Read quietly • Gardening • Cooking |
| Treating Oneself to Small Luxuries (13 caregivers, 28.3%) | Parent references a small luxury or indulgence. | • Get pedicures • Take a bath • Eat chocolate |
| Consuming Media (9 caregivers, 19.6%) | Parent references music, movies, or other media. | • Watch TV • Relax with movie • Music |
| Seeking Information (3 caregivers, 6.5%) | Parent references educating self or researching solutions. | • Research • Internet – seminars |
Common obstacles fell into eight categories, which were time restraints, lack of resources, family needs and challenges, exhaustion, health issues, mood, logistics, and pride. These are shown in Table 5.
Table 5.
Categories and definitions for caregivers’ perceived obstacles to self-care. Caregivers could list up to five obstacles. The number of parents who reported facing at least one obstacle in the relevant category are listed below category names.
| Code | Description | Example |
|---|---|---|
| Time Restraints (34 caregivers, 73.9%) | Parent references lack of time or busy schedule. | • Not enough time in a day • Running out of time • Too much housework |
| Lack of Resources (26 caregivers, 56.5%) | Parent references a lack of resources such as financial resources, support from family, or child care. | • Money and costs • Lack of support from family • Child care |
| Family Needs and Challenges (26 caregivers, 56.5%) | Parent references the idea that children’s or partner’s needs come first, or difficulties associated with behavior of children. | • Children and family needs come first • Behavior of children • Constant supervision |
| Exhaustion (14 caregivers, 30.4%) | Parent references fatigue or exhaustion. | • Too exhausted • Tired |
| Health Issues (6 caregivers, 13.0%) | Parent references medical issues. | • Medical problems • Physical health limitations |
| Mood (5 caregivers, 10.9%) | Parent references stress or a lack of motivation. | • Work stress • Mood |
| Logistics (4 caregivers, 8.7%) | Parent references logistics of strategies for self-care. | • Live far away • Friends not available |
| Pride (1 parent, 2.2%) | Parent mentions pride. | • Pride |
4. Discussion
4.1. Significance of Results
Caregivers of children with FASD face increased stress related to parenting (e.g., Paley et al., 2005; Webster et al., 2008); therefore, it is imperative that research focus on how caregiver self-care may be used as a method to alleviate parenting stress among this population. Self-care strategies have not been previously investigated in FASD. Results from the current study show that caregivers who reported higher confidence in their ability to use self-care also had higher family needs being met, higher satisfaction in the parenting role, and lower parental distress. These relationships were not seen with regard to frequency of self-care. Neither confidence in self-care abilities nor frequency of self-care was related to caregiver ratings of child problem behavior, parenting self-efficacy, child age, or gross family household income.
Caregivers with higher confidence in self-care had higher family needs met, lower parental distress, and higher satisfaction in the parenting role. It is not surprising that higher family needs met correlated with higher confidence in self-care, as many parents cited lack of resources as an obstacle to self-care. Family needs, including respite and sufficient services, are essential to families’ well-being (Olson et al., 2009). Unfortunately, many caregivers raising children with FASD have difficulty accessing these types of services (Petrenko et al., 2014; Petrenko et al., 2019; Ryan, Bonnett, & Gass, 2006). Helping families find creative solutions to meet these needs may reduce caregiver burden and have important benefits on self-care confidence. Additionally, higher confidence in self-care was associated with decreased parental distress and increased parental satisfaction. This study was correlational in nature and can’t infer directionality. It is possible self-care use and confidence led to caregivers feeling less distress and more satisfaction; alternately, less distressed families may have fewer self-care needs. Future research investigating a directional relationship between these variables could have implications for intervention targets.
Several themes were repeated throughout the caregivers’ descriptions of their self-care strategies, including being present, seeking social support, maintaining physical health, engaging in hobbies, consuming media, treating oneself to small luxuries, and seeking information. These strategies line up with current literature on protective factors for caregiver stress and negative outcomes. For example, mothers of children with developmental disabilities reported poorer physical health than mothers of typically developing children (Eisenhower, Baker, & Blacher, 2009). Additionally, social support has been shown to be important for parents and caregivers of children with developmental disabilities, especially mothers (Jones & Passey, 2005; Plant & Sanders, 2007). Giallo, Rose, & Vittorino (2011) found mothers of children with ASD evidenced high need for social support, low sleep quality, and low physical health predictive of maternal fatigue. These factors were in turn predictive of stress, anxiety, and depression in these mothers. More research is needed to further illuminate the relationship between caregivers’ self-care strategies and their needs as parents.
Similarly, themes emerged among obstacles to self-care reported by caregivers, including time constraints, lack of resources, family needs and challenges, exhaustion, health issues, mood, logistics, and pride. Herman and Thompson (1995) found that families of children with developmental disabilities perceived their basic resources as adequate, but felt they lacked the time, financial resources, and child-care to fully care for their children. In fact, they found that parents’ perception of time resources was the strongest predictor of depression. Perception of time resources was associated with amount of care needed for the child, adequacy of financial resources, and child-care (Herman & Marcenko, 1995). Our findings replicate those perceived barriers and contribute more information on caregivers’ perceived obstacles. Lack of time was by far the most common obstacle reported, with lack of financial resources also frequent. Many parents also noted that not having child-care, especially child-care that is equipped to handle the needs of their children, was an obstacle to self-care. Low awareness of FASD and stigma often prevent these needs from being met (Petrenko et al., 2014). Other common obstacles included lack of support, with caregivers noting lack of social support broadly as well as lack of support from close family members and spouses. Olson and colleagues (2009) reported that an imperative need of caregivers of children with FASD was to be able to connect with others who understood their experience. Support and reassurance in difficult situations was also a common need for these caregivers (Olson et al., 2009).
The lack of relationship between the frequency of self-care and parental stress and role satisfaction may indicate that caregivers’ perceptions of their self-care abilities, and not necessarily actual self-care behavior, may be more important for their well-being. This is consistent with studies that have found that parents’ cognitive appraisal of the situation may be more relevant to their mental health than specific coping strategies (Higgins, Bailey, & Pearce, 2005; Hassall et al., 2005). This idea is important given the strain on resources, especially time, experienced by caregivers of children with disabilities (Herman & Thompson, 1995; Herman & Marcenko, 1997), which was also seen in caregivers’ perceived obstacles to self-care in this study. Therefore, targeting caregivers’ perceptions and attitudes about self-care may be more important than frequency per se. This finding has important implications for effective stress interventions, discussed below.
It is notable in the current study that child problem behavior did not correlate with indices of self-care. Given the current literature on the transactional relationship between child problem behavior and parent stress (Baker et al., 2003), this finding suggests that although stress may be affected by child problem behavior, confidence in caring for oneself is not. However, it is important to note that the majority of children in the current sample evidenced clinically elevated behavior problems, and also that the sample size of the study was relatively small. Perhaps this pattern of findings would be different in a sample with more variable behavior and a larger sample size.
This study also replicated additional relationships documented in the literature on parent wellbeing. For example, parents of children with intellectual disabilities who were more stressed, especially as related to their caregiving responsibilities, tended to have lower parental role satisfaction (Hassall et al., 2005). We found a negative association between satisfaction and child problem behavior, also reflected in the literature on parents of typical children (Johnston & Mash, 1989; Gilmore & Cuskelly, 2012). Current research suggests a transactional relationship between parent stress and child problem behavior, in which parental stress contributes to child behavior problems, which in turn increases parental stress (Baker et al., 2003; Jirikowic, Olson, & Astley, 2012; Paley et al., 2005). We found a marginally significant positive relationship between stress and child problem behavior in this sample.
4.2. Implications for Intervention
Self-care strategies reported give insight into existing stress-reduction interventions that may be particularly effective in parents and caregivers of children with FASD. Themes found in the current study, especially being present, reflect principles of mindfulness such as spending time alone and reflection. Mindfulness-based interventions for parent stress reduction have recently shown promise (Neece, 2014; Bazzano et al., 2015), and could be reasonable approaches to test with this population. Notably, a recent feasibility study in parents of children with FASD found positive results for the Parents under Pressure program, an intervention aimed at increasing self-regulation and improving the parent-child relationship through mindfulness-based strategies (Reid et al., 2017). This lends further support to the promise of mindfulness-based intervention in this population, not just for stress-reduction but also self-regulation and the parent-child relationship. Caregivers who seek individual psychotherapy may also consider pursuing providers who use mindfulness-based approaches in their practice.
Results of the current study support the use of existing psychological interventions in caregivers of children with FASD. For example, Acceptance and Commitment Therapy (ACT) may be especially effective in this population given findings regarding caregivers’ self-care strategies and obstacles. ACT emphasizes acceptance of difficult or unpleasant emotions and a focus on personal values and goals (Hayes, Strosahl, & Wilson, 1999). Promising results for ACT have been found in parents of children with autism and cerebral palsy (Blackledge & Hayes, 2006; Whittingham, Sanders, McKinlay, & Boyd, 2013). Interventions to decrease caregivers’ stress and increase their mental health have important implications for their quality of life. Results from the current study suggest that parental distress plays an vital role in caregiver self-care and wellbeing. Poorer caregiver mental health has also been associated with lower caregiver and family quality of life (Reid & Moritz, 2019).
Caregivers also reported using physical activity for self-care. Observational studies have shown a strong link between physical activity and reduced stress (Aldana, Sutton, Jacobson, & Quirk, 1996; Hansmann et al., 2007). While some interventions have used yoga or other forms of movement for stress reduction in the general population (Michalsen et al., 2005; Granath, Ingvarsson, von Thiele, & Lundberg, 2006; Smith et al., 2008; Berger & Owen, 1988), these interventions could also be studied in parents of children with disabilities. Social support was also a common strategy for self-care in caregivers, and lack of social and family support was reported as an obstacle to self-care. While a strong social network has been associated with reduced stress (Jones & Passey, 2005; Plant & Sanders, 2007), caregivers raising children with FASD often report feeling isolated and have difficulty finding support (Petrenko et al., 2019). Future interventions could work to strengthen social networks of parents and caregivers in this population.
Results of this study suggest that targeting perceived confidence in self-care abilities may be more helpful than emphasizing frequency of activities. The cognitive nature of the associations found in this study may suggest the relevance of cognitive behavioral methods to target attitudes around self-care. This has been reflected in current research on parents of children with developmental disabilities (Singer et al., 2007; Lindo et al., 2016) and should continue to be utilized in and tailored to this population. In addition, as reflected in the identified obstacles, participants reported the idea that family needs were more important than their own needs. This suggests that motivational interviewing (Millner & Rollnick, 1991) may be important to consider for this population. Caregivers may need assistance to consider how self-care aligns with their family goals and values as well as support in behavior change.
This descriptive study also provides documentation of self-care practices and obstacles that may be useful for clinicians developing and implementing interventions with families. Strategies for self-care vary widely from person to person; what works well for one person may not work well at all for another. Clinicians should keep in mind the variability of methods of self-care when working with parents and caregivers of children with developmental disabilities. Additionally, the obstacles detailed in this study should inform intervention work with this population. FASD is a lifelong condition and many parents will have extended caregiving roles throughout the child’s life. Thus, it is imperative that stress reduction intervention be sustainable, which means being able to address the difficulties families face in being able to use self-care in the long-term. Clinicians should consider obstacles families may encounter in self-care and work with them to address these issues in a realistic manner.
4.3. Strengths and Limitations
Self-care is often emphasized by clinicians working with families and in self-help materials, but almost no formal research has been conducted on the self-care practices of caregivers raising children with FASD and how this relates to child and family functioning. This descriptive study documents important information about self-care in this population that can help guide subsequent research and intervention development.
This study is limited by its cross-sectional design; thus, no conclusions on causality or longitudinal transactions between constructs of interest can be made. Future studies using longitudinal designs could assess whether self-care can lead to a significant reduction in stress. Further, a randomized controlled trial (RCT) of an intervention targeting self-care could add additional advantages. Because these designs can more effectively assess causality than can cross-sectional designs, clearer conclusions could be made with regard to the relationship of self-care and stress in caregivers (Toth, Petrenko, Gravener-Davis, & Handley, 2016). Specifically, future research should assess whether a transactional relationship exists between self-care and stress. To get an even more clear assessment of the relationship between self-care and stress, ecological momentary assessment diary analysis would be useful in pinpointing the exact causes, effects, and fluctuations of these constructs.
The findings of this study should be considered in the context of the sample recruited. Findings should be cautiously considered as the sample size was relatively small. The sample was made up of caregivers of preschool and school-aged children, and their experiences may differ substantially from caregivers of infants or adolescents. The sample was also drawn from an intervention study, meaning the participants may differ from non-treatment seeking populations. Additionally, biological parents of children with FASD are underrepresented in this sample, as are fathers; these populations may approach self-care differently. Although a wide range was included, our sample consisted mostly of middle-class participants with some college education or greater, which may further limit the generalizability of the results.
Finally, the possibility of an unknown variable driving the associations found in this study should be considered. Confidence in self-care, satisfaction in parenting, and parental stress could all be affected by a variable not measured in this study, such as global cognitive style. Further research should investigate the possibility of a more general factor affecting these constructs. It is also possible that the self-care frequency variable was not sensitive to caregivers’ self-care behavior.
5. Conclusions
This study provides important information about self-care in caregivers and its associations with other family functioning variables including stress and parental satisfaction. Although stress-reduction in caregivers of children with developmental disabilities has been discussed in the literature, little research has been done on how these caregivers engage in self-care. This study investigated strategies and obstacles relating to self-care, as well as how confident caregivers felt in self-care and how frequently they engaged in it. The findings of this descriptive study hold important implications for clinicians working with families of children with FASD. Interventions targeting stress reduction in this population should keep in mind the obstacles faced by caregivers as well as the highly varied strategies they utilize. Future research should investigate a causal or transactional relationship between caregiver self-care, parental stress, and parental satisfaction.
Highlights.
Caregivers of children with FASD reported varied self-care strategies.
Self-care confidence related to parenting satisfaction, distress, and needs met.
Self-care frequency related to perceived confidence, but not other outcomes.
Limited time, resources, and social support were common obstacles to self-care.
What this paper adds.
This paper is the first to describe caregivers’ strategies for self-care and the obstacles they face in this area. Caregivers’ strategies, while varied, were grouped into categories which can inform clinical work with parents of children with FASD. Additionally, this paper contributes to our understanding of the obstacles and barriers these caregivers face in raising their children and caring for themselves. This paper emphasizes the importance of confidence in self-care, especially with regard to stress and parenting satisfaction.
Acknowledgements
This study was funded by a grant (K01AA020486) from the National Institute on Alcohol Abuse and Alcoholism. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health. We gratefully acknowledge the undergraduate, post-bachelor, and graduate student research assistants who were involved in participant recruitment and data collection for this study. Most importantly, we thank the courageous and dedicated caregivers, and their children, who participated in this study and without whom these research advances would not be possible.
Funding: This work was supported by the National Institutes of Health [grant number K01 AA020486, 2011–2016].
Footnotes
Declarations of interest: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abidin RR (1992). The determinants of parenting behavior. Journal of clinical child psychology, 21(4), 407–412. [Google Scholar]
- Abidin RR (2012). Parenting stress index, (PSI-4). Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Aldana SG, Sutton LD, Jacobson BH, & Quirk MG (1996). Relationships between leisure time physical activity and perceived stress. Perceptual and Motor skills, 82(1), 315–321. [DOI] [PubMed] [Google Scholar]
- Armstrong MI, Birnie-Lefcovitch S, & Ungar MT (2005). Pathways between social support, family well being, quality of parenting, and child resilience: What we know. Journal of child and family studies, 14(2), 269–281. [Google Scholar]
- Baker BL, McIntyre LL, Blacher J, Crnic K, Edelbrock C, & Low C (2003). Pre-school children with and without developmental delay: behaviour problems and parenting stress over time. Journal of Intellectual Disability Research, 47(4 5), 217–230. [DOI] [PubMed] [Google Scholar]
- Bazzano A, Wolfe C, Zylowska L, Wang S, Schuster E, Barrett C, & Lehrer D (2015). Mindfulness based stress reduction (MBSR) for parents and caregivers of individuals with developmental disabilities: A community-based approach. Journal of Child and Family Studies, 24(2), 298–308. [Google Scholar]
- Beresford BA (1994). Resources and strategies: How parents cope with the care of a disabled child. Journal of child psychology and psychiatry, 35(1), 171–209. [DOI] [PubMed] [Google Scholar]
- Berger BG, & Owen DR (1988). Stress reduction and mood enhancement in four exercise modes: Swimming, body conditioning, hatha yoga, and fencing. Research quarterly for exercise and sport, 59(2), 148–159. [Google Scholar]
- Blackledge JT, & Hayes SC (2006). Using acceptance and commitment training in the support of parents of children diagnosed with autism. Child & Family Behavior Therapy, 28(1), 1–18. [Google Scholar]
- Bobbitt SA, Baugh LA, Andrew GH, Cook JL, Green CR, Pei JR, & Rasmussen CR (2016). Caregiver needs and stress in caring for individuals with fetal alcohol spectrum disorder. Research in developmental disabilities, 55, 100–113. [DOI] [PubMed] [Google Scholar]
- Brown JD, Rodger S, George N, St Arnault D, & Sintzel J (2008). Rewards of parenting a child with a fetal alcohol spectrum disorder. The Open Family Studies Journal, 1, 23–30. [Google Scholar]
- Conger RD, Patterson GR, & Ge X (1995). It takes two to replicate: A mediational model for the impact of parents’ stress on adolescent adjustment. Child development, 66(1), 80–97. [DOI] [PubMed] [Google Scholar]
- Creasey GL, & Jarvis PA (1994). Relationships between parenting stress and developmental functioning among 2-year-olds. Infant Behavior and Development, 17(4), 423–429. [Google Scholar]
- Dumas JE, Wolf LC, Fisman SN, & Culligan A (1991). Parenting stress, child behavior problems, and dysphoria in parents of children with autism, Down syndrome, behavior disorders, and normal development. Exceptionality: A Special Education Journal, 2(2), 97–110. [Google Scholar]
- Eisenhower AS, Baker BL, & Blacher J (2009). Children’s delayed development and behavior problems: Impact on mothers’ perceived physical health across early childhood. Social Science & Medicine, 68(1), 89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes A, Munson J, Dawson G, Koehler E, Zhou XH, & Abbott R (2009). Parenting stress and psychological functioning among mothers of preschool children with autism and developmental delay. Autism, 13(4), 375–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyberg SM, & Pincus D (1999). Eyberg child behaviour inventory and sutter-eyberg student behaviour inventory–Revised: professional manual. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Giallo R, Rose N, & Vittorino R (2011). Fatigue, wellbeing and parenting in mothers of infants and toddlers with sleep problems. Journal of Reproductive and Infant Psychology, 29(3), 236–249. [Google Scholar]
- Gilmore L, & Cuskelly M (2012). Parenting satisfaction and self-efficacy: A longitudinal study of mothers of children with Down syndrome. Journal of Family Studies, 18(1), 28–35. [Google Scholar]
- Granath J, Ingvarsson S, von Thiele U, & Lundberg U (2006). Stress management: a randomized study of cognitive behavioural therapy and yoga. Cognitive behaviour therapy, 35(1), 3–10. [DOI] [PubMed] [Google Scholar]
- Hansmann R, Hug SM, & Seeland K (2007). Restoration and stress relief through physical activities in forests and parks. Urban forestry & urban greening, 6(4), 213225. [Google Scholar]
- Hassall R, Rose J, & McDonald J (2005). Parenting stress in mothers of children with an intellectual disability: The effects of parental cognitions in relation to child characteristics and family support. Journal of intellectual disability research, 49(6), 405–418. [DOI] [PubMed] [Google Scholar]
- Hastings RP, & Beck A (2004). Practitioner review: Stress intervention for parents of children with intellectual disabilities. Journal of child psychology and psychiatry, 45(8), 1338–1349. [DOI] [PubMed] [Google Scholar]
- Hastings RP, Kovshoff H, Brown T, Ward NJ, Espinosa FD, & Remington B (2005). Coping strategies in mothers and fathers of preschool and school-age children with autism. Autism, 9(4), 377–391. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl K, & Wilson KG (1999). Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change. New York: Guilford Press. [Google Scholar]
- Heaman DJ (1995). Perceived stressors and coping strategies of parents who have children with developmental disabilities: a comparison of mothers with fathers. Journal of Pediatric Nursing, 10(5), 311–320. [DOI] [PubMed] [Google Scholar]
- Herman SE, & Marcenko MO (1997). Perceptions of services and resources as mediators of depression among parents of children with developmental disabilities. Mental Retardation, 35(6), 458. [DOI] [PubMed] [Google Scholar]
- Herman SE, & Thompson L (1995). Families’ perceptions of their resources for caring for children with developmental disabilities. Mental retardation, 33(2), 73. [PubMed] [Google Scholar]
- Higgins DJ, Bailey SR, & Pearce JC (2005). Factors associated with functioning style and coping strategies of families with a child with an autism spectrum disorder. Autism, 9(2), 125–137. [DOI] [PubMed] [Google Scholar]
- Hill C, & Rose J (2009). Parenting stress in mothers of adults with an intellectual disability: Parental cognitions in relation to child characteristics and family support. Journal of Intellectual Disability Research, 53(12), 969–980. [DOI] [PubMed] [Google Scholar]
- Hoyme HE, Kalberg WO, Elliott AJ, Blankenship J, Buckley D, Marais AS, … & Jewett T (2016). Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics, 138(2), e20154256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jirikowic T, Olson HC, & Astley S (2012). Parenting stress and sensory processing: Children with fetal alcohol spectrum disorders. OTJR: Occupation, Participation and Health, 32(4), 160–168. [Google Scholar]
- Johnston C, & Mash EJ (1989). A measure of parenting satisfaction and efficacy. Journal of clinical child psychology, 18(2), 167–175. [Google Scholar]
- Jones K, & Smith D (1973). Recognition of the fetal alcohol syndrome in early infancy. The Lancet, 302(7836), 999–1001. [DOI] [PubMed] [Google Scholar]
- Kreutzer JS, Marwitz J, & West D (1988). Family needs questionnaire. Richmond, VA: Rehabilitation Research and Training Center on Severe Traumatic Brain Injury, Medical College of Virginia. [Google Scholar]
- Lindo EJ, Kliemann KR, Combes BH, & Frank J (2016). Managing stress levels of parents of children with developmental disabilities: A meta analytic review of interventions. Family Relations, 65(1), 207–224. [Google Scholar]
- May PA, Chambers CD, Kalberg WO, Zellner J, Feldman H, Buckley D, … & Taras H (2018). Prevalence of fetal alcohol spectrum disorders in 4 US communities. Jama, 319(5), 474–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride BA (1989). Stress and fathers’ parental competence: Implications for family life and parent educators. Family Relations, 385–389. [Google Scholar]
- Michalsen A, Grossman P, Acil A, Langhorst J, Lüdtke R, Esch T, … & Dobos G (2005). Rapid stress reduction and anxiolysis among distressed women as a consequence of a three-month intensive yoga program. Medical Science Monitor, 11(12), CR555–CR561. [PubMed] [Google Scholar]
- Millner WR, & Rollnick S (1991). Motivational interviewing: Preparing people to change addictive behaviors.
- Myers HF, & Taylor S (1998). Family contributions to risk and resilience in African American children. Journal of Comparative Family Studies, 215–229. [Google Scholar]
- Neece CL (2014). Mindfulness based stress reduction for parents of young children with developmental delays: Implications for parental mental health and child behavior problems. Journal of Applied Research in Intellectual Disabilities, 27(2), 174–186. [DOI] [PubMed] [Google Scholar]
- Ngai FW, & Chan SWC (2012). Stress, maternal role competence, and satisfaction among Chinese women in the perinatal period. Research in Nursing & Health, 35(1), 30–39. [DOI] [PubMed] [Google Scholar]
- Olson HC, Oti R, Gelo J, & Beck S (2009). “Family matters:” fetal alcohol spectrum disorders and the family. Developmental Disabilities Research Reviews, 15(3), 235249. [DOI] [PubMed] [Google Scholar]
- Paley B, O’Connor MJ, Frankel F, & Marquardt R (2006). Predictors of stress in parents of children with fetal alcohol spectrum disorders. Journal of Developmental & Behavioral Pediatrics, 27(5), 396–404. [DOI] [PubMed] [Google Scholar]
- Paley B, O’Connor MJ, Kogan N, & Findlay R (2005). Prenatal alcohol exposure, child externalizing behavior, and maternal stress. Parenting: Science and Practice, 5(1), 2956. [Google Scholar]
- Petrenko CL, Alto ME, Hart AR, Freeze SM, & Cole LL (2019). “I’m Doing My Part, I Just Need Help From the Community”: Intervention Implications of Foster and Adoptive Parents’ Experiences Raising Children and Young Adults With FASD. Journal of Family Nursing. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrenko CL, Tahir N, Mahoney EC, & Chin NP (2014). Prevention of secondary conditions in fetal alcohol spectrum disorders: identification of systems-level barriers. Maternal and child health journal, 18(6), 1496–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plant KM, & Sanders MR (2007). Predictors of care giver stress in families of preschool-aged children with developmental disabilities. Journal of intellectual disability research, 51(2), 109–124. [DOI] [PubMed] [Google Scholar]
- Reid N, Dawe S, Harnett P, Shelton D, Hutton L, & O’Callaghan F (2017). Feasibility study of a family-focused intervention to improve outcomes for children with FASD. Research in developmental disabilities, 67, 34–46. [DOI] [PubMed] [Google Scholar]
- Reid N, & Moritz KM (2019). Caregiver and family quality of life for children with fetal alcohol spectrum disorder. Research in developmental disabilities, 94, 103478. [DOI] [PubMed] [Google Scholar]
- Renner LM, Whitney SD, & Easton SD (2015). Profiles of self-reported parenting competence and stress among women with/without histories of childhood sexual abuse. Journal of Child and Family Studies, 24(3), 749–761. [Google Scholar]
- Ryan DM, Bonnett DM, & Gass CB (2006). Sobering thoughts: Town hall meetings on fetal alcohol spectrum disorders. American Journal of Public Health, 96(12), 20982101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer GH, Ethridge BL, & Aldana SI (2007). Primary and secondary effects of parenting and stress management interventions for parents of children with developmental disabilities: A meta analysis. Mental retardation and developmental disabilities research reviews, 13(4), 357–369. [DOI] [PubMed] [Google Scholar]
- Smith BW, Shelley BM, Dalen J, Wiggins K, Tooley E, & Bernard J (2008). A pilot study comparing the effects of mindfulness-based and cognitive-behavioral stress reduction. The Journal of Alternative and Complementary Medicine, 14(3), 251–258. [DOI] [PubMed] [Google Scholar]
- Smith TB, Oliver MN, & Innocenti MS (2001). Parenting stress in families of children with disabilities. American journal of orthopsychiatry, 71(2), 257–261. [DOI] [PubMed] [Google Scholar]
- Streissguth AP, Bookstein FL, Barr HM, Sampson PD, O’Malley K, & Young JK (2004). Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. Journal of Developmental & Behavioral Pediatrics, 25(4), 228–238. [DOI] [PubMed] [Google Scholar]
- Toth SL, Petrenko CL, Gravener Davis JA, & Handley ED (2016). Advances in prevention science: A developmental psychopathology perspective. Developmental psychopathology, 1–59. [Google Scholar]
- Warren KR, Hewitt BG, & Thomas JD (2011). Fetal alcohol spectrum disorders: research challenges and opportunities. Alcohol Research & Health, 34(1), 4. [PMC free article] [PubMed] [Google Scholar]
- Watson SL, Coons KD, & Hayes SA (2013). Autism spectrum disorder and fetal alcohol spectrum disorder. Part I: A comparison of parenting stress. Journal of Intellectual and Developmental Disability, 38(2), 95–104. [DOI] [PubMed] [Google Scholar]
- Watson SL, Hayes SA, Coons KD, & Radford-Paz E (2013). Autism spectrum disorder and fetal alcohol spectrum disorder. Part II: A qualitative comparison of parenting stress. Journal of Intellectual and Developmental Disability, 38(2), 105–113. [DOI] [PubMed] [Google Scholar]
- Webster RI, Majnemer A, Platt RW, & Shevell MI (2008). Child health and parental stress in school-age children with a preschool diagnosis of developmental delay. Journal of child neurology, 23(1), 32–38. [DOI] [PubMed] [Google Scholar]
- Whittingham K, Sanders M, McKinlay L, & Boyd RN (2013). Stepping Stones Triple P and Acceptance and Commitment Therapy for parents of children with cerebral palsy: trial protocol. Brain Impairment, 14(2), 270–280. [Google Scholar]