Dear editor,
We have read with interest the short communication published by Segovia-Juarez et al., 2020 in Respiratory Physiology & Neurobiology establishing that high altitude reduces the infection rate of COVID-19 but not the case fatality rate in the Peruvian setting. We support this hypothesis, however there could be an important number of under registered deaths on account of a low rate of diagnostic tests performed per inhabitant and mostly in symptomatic patients (Pasquariello and Stranges, 2020). It has been estimated that in Peru, 4 tests are performed per 1000 inhabitants; a fairly low figure compared to other countries in the region such as Chile and the United States, who perform 30 and 51 tests per 1000 inhabitants, respectively (Our World in Data, 2020). Furthermore, in Peru, only patients that tested positive for SARS-CoV-2 are labeled as COVID-19 deaths. Following this consideration, we would like to add the importance to evaluate the excess mortality (EM). In Peru, EM registered between March to May was 13,000 more deaths than expected for that period, of which, only 3000 were positive for SARS-CoV-2. This represents an EM of 54 %, which was the highest reported compared to 20 countries (Mundo, 2020). We would like to highlight the relation between EM rate and altitude per district in Peru during COVID-19 pandemic.
We conducted an ecological study in order to assess the relation between EM rate and altitude of the 1874 Peruvian districts during COVID-19 pandemic. Our population included all subjects who died between April and June from 2017 to 2020 in Peru and were registered in the National Death Computer System (SINADEF). Based on this, we included 1829 districts in our analysis. EM is a numerical variable, created by subtracting the number of deaths from April to June 2020 minus the average deaths each month in the 2017–2019 period per district, respectively. In order to obtain the EM rate, the following equation was used:
X = Excess mortality rate
Y = Number of deaths recorded from April to June 2020
Z = Average of deaths recorded from April to June 2017–2019
M = Population 2020
N = Average population 2017–2019
Districts population was obtained from the 2017 national census, and 2018–2020 population growth projections; which was collected from National Institute of Statistics and Informatics (INEI). Furthermore, altitude was used as a numerical variable which was gathered from INEI. In our statistical analysis, firstly we tested normality assumption through Shapiro Wilk test, and we obtained an abnormal distribution. Then, we performed a Spearman’s correlation between EM rate and altitude. We used RStudio version 3.5.2. (RStudio Team (2020). RStudio: Integrated Development for R. RStudio, PBC, Boston, MA URL http://www.rstudio.com/)
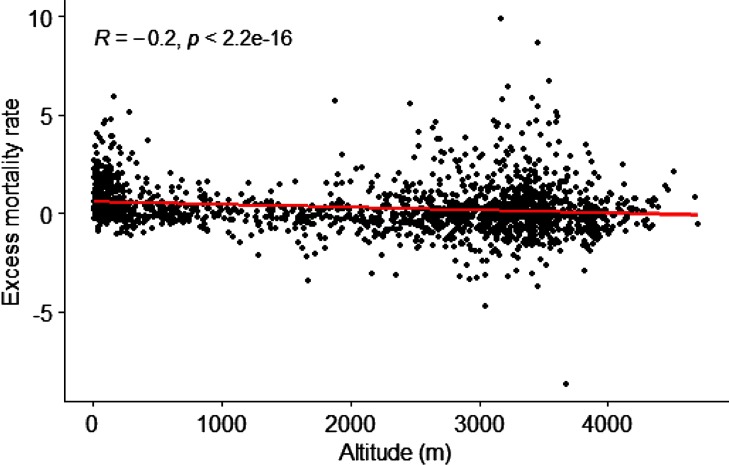
Nationwide, we found an EM of 36,322 (139.8 %) and an EM rate of 1.1 death per 1000 inhabitants. Meanwhile, there were only 9860 officially COVID-19 deaths (Stand June 30, 2020). This EM could be explained by two plausible reasons: a high rate of officially and non-officially reported COVID-19 deaths; and an increase in non−COVID-19 related deaths as a result of non-seeking medical attention, lockdown-related deaths and hospitals collapse (Vandoros, 2020; Watkins and Wulaningsih, 2020). We found that as altitude increases, the EM rate decreases (R = -0.2, p < 0.001) (Fig. 1 ). SARS-CoV-2's virulence seems to decrease at high altitude as mentioned by Arias-Reyes et al., 2020 Furthermore, it has been suggested that Peruvian districts located at high altitude may behave this way due to smaller populations and a lower population density (Huamaní et al., 2020). Therefore, our analysis included districts’ population to reduce this bias. Moreover, we used district altitudes in our analysis because Peruvian geography is greatly variable, and within a single province there may be a great difference between the altitude of different cities and towns. Hence, we believe a district altitude-based approach reduces the bias that may arise by altitude variability, which characterizes the province altitude-based approach used by Segovia-Juarez et al., 2020
Fig. 1.
Correlation between excess mortality rate and altitude.
In conclusion, we support Segovia-Juarez et al., 2020 findings which are consistent with ours. However, we believe that the assessment of EM during a pandemic is a more trustworthy way to assess the COVID-19 public health impact. Our results may explain a decrease in COVID-19 deaths as altitude increases as well as a lower impact of COVID-19 among other deaths at higher altitudes.
Funding sources
The authors received no financial support for the research, authorship, and/or publication of this article.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
References
- Arias-Reyes C., Zubieta-DeUrioste N., Poma-Machicao L. Does the pathogenesis of SARS-CoV-2 virus decrease at high-altitude? Respir. Physiol. Neurobiol. 2020 doi: 10.1016/j.resp.2020.103443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huamaní C., Velásquez L., Montes S. Propagation by COVID-19 at high altitude: cusco case. Respir. Physiol. Neurobiol. 2020 doi: 10.1016/j.resp.2020.103448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundo L.R. La República; 2020. Perú es el país con más exceso de muertes durante la pandemia de COVID-19.https://larepublica.pe Retrieved from: [Google Scholar]
- Our World in Data . 2020. Coronavirus (COVID-19) Testing - Statistics and Research - Our World in Data.https://ourworldindata.org/coronavirus-testing Access 20 July 2020. [Google Scholar]
- Pasquariello P., Stranges S. Excess mortality from COVID-19: a commentary on the Italian experience. Int. J. Public Health. 2020 doi: 10.1007/s00038-020-01399-y. [DOI] [PubMed] [Google Scholar]
- Segovia-Juarez J., Castagnetto J.M., Gonzales G.F. High altitude reduces infection rate of COVID-19 but not-case fatality rate. Respir. Physiol. Neurobiol. 2020 doi: 10.1016/j.resp.2020.103494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandoros S. Excess mortality during the Covid-19 pandemic: early evidence from England and Wales. Soc. Sci. Med. 2020 doi: 10.1016/j.socscimed.2020.113101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins J., Wulaningsih W. Three further ways that the COVID-19 pandemic will affect health outcomes. Int. J. Public Health. 2020 doi: 10.1007/s00038-020-01383-6. [DOI] [PMC free article] [PubMed] [Google Scholar]