Abstract
Studies of the effect of neighborhood poverty on health are dominated by research designs that measure neighborhood poverty at a single point in time, ignoring the potential influence of exposure to neighborhood poverty over the life course. Applying latent class analysis to restricted residential history data from the National Longitudinal Survey of Youth, 1979 Cohort, we identify four trajectories of life-course exposure to high-poverty neighborhoods between adolescence and midlife and then examine how these groups differ in their physical health conditions (SF-12 score) and self-rated health at around age 40. Linear and logistic regression analyses show that life-course exposure to high-poverty neighborhoods is a stronger predictor of midlife physical health than are point-in-time measures of neighborhood poverty observed during either adolescence or midlife. Our findings suggest that a life-course approach can enhance our understanding of how neighborhood poverty affects physical health.
Keywords: Neighborhood, Poverty, Physical health, SF-12 score, Self-rated health, Life course
Research shows that perceived physical health is a significant predictor of future morbidity and mortality, even after controlling for other individual characteristics [1–4]. Previous studies have investigated the determinants of physical health with an emphasis on either personal or family traits, such as employment status, education, and family structure [5–7]. For example, poor self-rated health is associated with being unemployed, working in informal job sectors [8], and living with a stepparent [7]. Moreover, in contrast to whites, blacks are more likely to report poor self-rated health while Latinos are less likely to do so [9]. Individuals with higher educational attainment and higher income report better physical health than those in a disadvantaged socioeconomic position [10, 11].
The impact of neighborhood poverty on health has also drawn research attention, but the literature has yielded somewhat inconsistent findings [12, 13]. A possible reason for this inconsistency is that these studies have been dominated by cross-sectional research designs that measure both neighborhood characteristics and health outcomes at the same point in time [14, 15]. By failing to consider individuals’ prior and cumulative exposure to neighborhood poverty, these studies may underestimate the effect of neighborhood poverty on health. Although some studies investigate how change in neighborhood poverty exposure affects health [16, 17], this approach typically fails to consider individuals’ exposure to high levels of neighborhood poverty over the entire life course. We suggest that it is important to investigate the effects of neighborhood poverty on health from a dynamic life-course perspective. Adopting a life-course approach responds to calls to explore the “temporal dimension” of neighborhood effects [18, 19].
Background and Hypotheses
A substantial literature has begun to address the effect of neighborhood poverty on individual health [12, 16, 17, 20, 21]. Living in a poor community is likely to be associated with unfavorable health conditions and behaviors for several reasons. First, socioeconomically disadvantaged neighborhoods are less likely than advantaged neighborhoods to provide residents with access to healthy foods, recreational opportunities, medical care, and quality housing units [22–25]. The lack of both tangible (e.g., access to healthy food) and intangible resources (e.g., social efficacy or support) in disadvantaged neighborhoods [26, 27] limits an individual’s life chances, which undermines individual health. Second, high-poverty neighborhoods are likely to exhibit low levels of social control among residents, creating an environment that hinders individual health via prevalence of crime or weak physical safety [28]. Finally, poor neighborhoods often suffer from environmental injustice as residents of such neighborhoods are more likely to be exposed to pollutants or toxins than their counterparts in socioeconomically advantaged neighborhoods [29].
High neighborhood poverty is experienced most acutely among racial and ethnic minorities. Two theoretical perspectives explain why minority groups are more likely to live in high poverty neighborhoods than the white non-Hispanic majority. First, spatial assimilation theory [30] posits that racial-ethnic differences in neighborhood conditions stem primarily from racial-ethnic differences in the resources required to attain residence in desirable neighborhoods. Thus, the spatial assimilation perspective implies that minority groups are more likely to live in high-poverty neighborhoods because they lack the financial and human capital required to purchase residence in lower-poverty neighborhoods. Second, place stratification theory [31] argues that minority groups, especially African Americans, are constrained to reside in high-poverty neighborhoods mainly because of the discriminatory practices of real estate agents, local governments, and mortgage lenders. White stereotyping of, and hostility towards, other ethno-racial groups may also impede minorities’ entrance into middle-class neighborhoods.
Although there are reasons to expect a detrimental impact of neighborhood poverty on health, evidence from previous research remains inconsistent [12] as some studies report an adverse impact but others find a null association. For example, data from the Alameda County Study show that residents of poor neighborhoods have a higher mortality rate and odds of reporting poor self-rated health than those residing in non-poor neighborhoods, even after adjusting for individual risk factors such as educational attainment and health behaviors (e.g., excessive alcohol consumption) [13, 20]. Do and Finch [32] control for unobserved heterogeneity across individuals and find that exposure to high neighborhood poverty is a risk factor for poor self-rated health. By contrast, Browning and Cagney [33] find that without adjusting for individual covariates, neighborhood poverty is positively associated with the odds of reporting poor self-rated health. However, this association is not robust to adjustment for individual risk factors. Some researchers argue that the often observed adverse impact of neighborhood poverty on individual health is spurious or conditional on other individual or neighborhood features (e.g., income levels or neighborhood affluence) [20, 34, 35].
While the empirical support for the adverse impact of neighborhood poverty on health is mixed, the theoretical explanations for why neighborhood poverty matters lead us to propose the first hypothesis:
(H1): Exposure to high levels of neighborhood poverty is negatively associated with individual physical health, net of other covariates.
Life-Course Exposure to Neighborhood Poverty and Health
Despite a strong interest in the influence of neighborhood poverty on physical health, our knowledge in this area remains underdeveloped in at least one critical way. The typical research design for studying the health effect of neighborhood poverty uses cross-sectional data and estimates statistical models that regress some indicator of physical health measured at the time of a survey on the neighborhood poverty rate of the respondent’s residential neighborhood also as of the survey date [36, 37]. This approach aims to capture the contemporaneous relationship between neighborhood poverty and health. A few studies also examine the association between the level of neighborhood poverty experienced during childhood or early adulthood on health outcomes later in life [38, 39], potentially capturing long-lasting effects of neighborhood poverty on health. Although these commonly used approaches offer some insight into the relationship between neighborhood poverty and health, they fail to recognize the possible influence of an individual’s complete residential history, that is, their cumulative exposure to neighborhood poverty over the life course [14, 40].
Several recent studies have examined the effect of cumulative exposure to neighborhood poverty on health over the life course [41, 42]. These studies show that individuals who are consistently exposed to high neighborhood poverty are more likely to be obese than those who never experience high neighborhood poverty [16, 21]. Women who move from high-poverty to low-poverty neighborhoods have fewer depressive symptoms than their counterparts who do not experience significant changes in neighborhood poverty [17]. Although these studies link individual health to life-course change in exposure to neighborhood poverty, they mainly focus on short-term residential change and health outcomes during early adulthood (i.e., around late 20s/early 30s). Few studies trace individuals’ exposure to neighborhood poverty from youth to middle adulthood or later [42].
According to Elder [43], the life-course perspective includes five basic principles: life span development, human agency, historic time and place, timing, and linked lives. Among them, the life span development and timing are critical to this study. The former suggests that all life stages are intricately related with one another and past experience is likely to shape future outcomes [44]. The latter indicates that the impact of certain experiences on future outcomes is contingent on when the experience occurs [44]. Drawing from these principles, we propose two reasons why attending to life-course exposure to neighborhood poverty can enhance our understanding of the effect of neighborhood poverty on health at midlife.
First, the influence of neighborhood poverty on most health outcomes likely depends on how long individuals have been exposed to disadvantaged neighborhood conditions [45]. Regardless of the mechanisms linking neighborhood poverty and health outcomes, for most health measures persistent exposure to high-poverty neighborhoods is presumably more impactful than fleeting exposures. Yet, the conventional research designs in this area employ a single point-in-time measure of poverty, which cannot distinguish persistent from temporary exposures to high neighborhood poverty. Moreover, exposure to low neighborhood poverty during some life stages could counterbalance exposure to high neighborhood poverty during other periods. The impact of the duration of exposure to high neighborhood poverty on later-life health may also depend on when in the life course individuals are exposed to neighborhood disadvantage.
Second, concurrent point-in-time measures of exposure to neighborhood poverty fail to reflect the fact that many physical health problems develop over time and that the latency period may differ across individuals. In absence of longitudinal data, it can be difficult to confidently infer a causal effect of neighborhood poverty measured at the time of a survey on health conditions measured at the same time point. While by no means fully resolving problems of causal inference, measuring exposure to neighborhood poverty over the life-course stages prior to the measurement of health outcomes maintains the proper temporal alignment of independent and dependent variables.
We propose the following hypotheses regarding the effect of life-course exposure to neighborhood poverty on physical health in midlife:
(H2): Life-course exposure to neighborhood poverty is adversely associated with midlife physical health even net of point-in-time exposures to neighborhood poverty during adolescence or middle adulthood.
(H3): Continuous exposure to high neighborhood poverty over the life-course has a stronger effect on midlife health outcomes than exposure to high neighborhood poverty only during adolescence/young adulthood or only during middle adulthood.
(H4) Controlling for life-course exposure to neighborhood poverty alters the observed associations between point-in-time measures of neighborhood poverty and midlife physical health.
The overarching goal of this study is to determine the impact of exposure to neighborhood poverty over the life course on physical health at midlife.
Data and Methods
To explore the impact of life-course exposure to neighborhood poverty on health, it is essential to access individual residential neighborhood histories. The National Longitudinal Survey of Youth, 1979 Cohort (NLSY79), provides restricted access to such information and serves as the source of our individual-level variables. First administered in 1979, the NLSY79 interviewed respondents annually through 1994 and biennially since that time. Respondents’ census tract of residence, a widely used definition of neighborhood [46], was collected at each interview, which allows us to create a life-course measure of exposure to neighborhood poverty. There were 12,686 respondents aged 14–22 in the first wave of NLSY79 [47]. This study uses data from the interview waves between 1979 and 2010. Over this 32-year time span, the retention rate is 76% [48].
The respondents needed to meet several criteria to be included in our analytic sample. First, respondents needed to have completed the questions in the 40-year-old health module (see below), particularly those dealing with physical health conditions and self-rated health. Second, their census tracts of residence needed to be recorded for the survey waves in 1980, 1990, 2000, 2010, as well as the year when respondents completed the 40-year-old health module. Third, if the census tract of residence was unknown at any of these five time points, it needed to be able to be substituted with the census tract reported within 2 years of that time point. For example, if the census tract code was missing in 1990, we needed to replace the missing value with the tract information in either 1991 or 1992. If the tract information was still missing in these years, we then use the tract information in 1989 or 1988 to replace the missing value. Should we fail to find the tract information in the 2-year span, this respondent will be excluded from the analysis. Our final samples consist of 3025 non-Hispanic white respondents, 1595 non-Hispanic black individuals, and 1076 Latinos.
Dependent Variables
We measure physical health with two variables—a summary scale of specific health conditions and a single item measure of self-rated health. The NLSY79 employs the short-form 12-question (SF-12) summary scores to assess an individual’s overall physical health in the 40-year-old health module. The SF-12 scale was developed by Ware et al. [49] and designed to evaluate the respondents’ physical conditions irrespective of their proclivity to use health services [48]. The scale includes questions such as “during the past 4 weeks, how much did pain interfere with your normal work?” and “how does your health now limit you in moderate activities, such as moving a table, pushing a vacuum cleaner, bowling, or playing golf?” The reliability and validity of the SF scales have been confirmed [50]. Following the guidelines by Ware et al. [49], the NLSY79 calculates the summary scores for respondents and releases the data to the main dataset. The SF-12 scores range from 0 (lowest level of health) to 100 (highest level of health), and in general, a respondent with a score over 50 has better health than a typical person in the population [51].
Respondents’ self-rated health is originally recorded in five categories: poor, fair, good, very good, and excellent. Following previous research [4], we re-classify the five categories into two groups with respondents reporting poor or fair health scored 0 and respondents reporting good, very good, or excellent health scored 1. For stylistic convenience, we refer to the latter category as “good health.” As self-rated health is reflective of both current health conditions and future risk [4], it may capture the impact of current neighborhood poverty on overall health better than the SF-12 physical health measure.
Independent Variables
Neighborhood poverty is the key independent variable of interest. Following conventional practice, we use census tracts to represent neighborhoods. Because census tract boundaries change frequently, we use the Neighborhood Change Database [52] to normalize census tract boundaries to the 2010 census definition, thus facilitating comparisons across survey waves. The 1980–2010 decennial US censuses and the American Community Survey are the major data sources for calculating neighborhood poverty, which is defined as the ratio of the population with incomes below the official poverty line to the total population in a tract. We use linear interpolation to estimate the neighborhood poverty rate from non-census years [18, 19]. We calculate two single-year, point-in-time measures of neighborhood poverty. The first measure taps early-life exposure to neighborhood poverty, referring to the poverty ratio of an individual’s residential neighborhood in 1980. The second measure taps current exposure to neighborhood poverty; this is the poverty ratio of the neighborhood where respondents resided when their physical health status and self-rated health were assessed in the age 40 module.
In addition to these two conventional neighborhood poverty measures, this study creates a measure of respondents’ exposure to high-poverty neighborhoods over the life course. We first categorize all census tracts in 1980, 1990, 2000, and 2010 into two groups: high-poverty neighborhoods (i.e., with poverty ratios ≥ 0.2) and low-poverty neighborhoods (i.e., with poverty ratios < 0.2). The cutoff point (0.2) is the criterion used by the Census Bureau to designate poverty areas and has been commonly used in studies of the effect of neighborhood conditions on health [53]. Living in high-poverty neighborhoods is coded 1, otherwise 0. We then perform a latent class analysis (LCA) [54] using the four dummy variables to identify classes of respondents who shared similar trajectories of exposure to high-poverty neighborhoods between 1980 (when respondents were ages 15 to 23) and 2010 (when respondents were between ages 45 and 53). A general LCA model that identifies distinctive trajectories based on the probability of living in high-poverty neighborhoods can be expressed as:
where P(Xvi = 1) refers to the unconditional probability that a respondent v lived in a high-poverty neighborhood (X = 1) at a given time period i (i = 1, …, 4). The parameter πig refers to the conditional solution probability that respondent v lived in a high-poverty neighborhood given a certain latent class membership (P(Xvi = 1| G = g)). πg indicates the class size parameter and gauges the unconditional probability of being classified into a certain latent class g (g = 1, …G). The sum of πg is 1.
Following previous research [55], we use Bayesian information criterion (BIC) to decide the number of latent class memberships by comparing models with different numbers of latent classes. Lower BIC values suggest better model fits [56]. We initially implemented unconditional models with two, three, four, and five latent classes and found that the model with four latent classes has the lowest BIC value (i.e., 29,649.357) and the BIC starts to increase after five latent classes (i.e., 29,657.852). The entropy value for four latent classes is above 0.8, suggesting that these classes separate from each other well [57], and the likelihood-ratio tests suggest that using five classes does not improve the model fit. Consequently, respondents are classified into four latent classes.
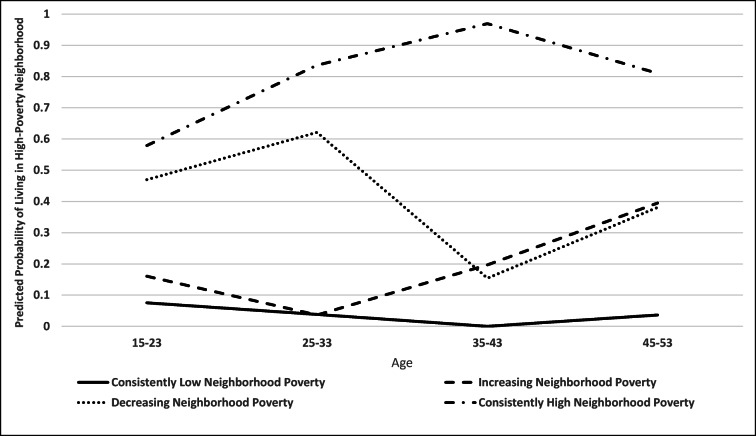
We present the latent class patterns in Fig. 1. The Y-axis indicates the predicted probability of living in a high-poverty neighborhood, and the X-axis indicates the respondents’ age. In our analytic sample, roughly 54% of respondents experience consistently low probabilities of being exposed to high-poverty neighborhoods between ages 15–23 and 45–53. We refer to this group as the consistently low neighborhood poverty group. In sharp contrast, approximately 17% of respondents are consistently exposed to high-poverty neighborhoods over the study period. We refer to this class as the consistently high neighborhood poverty group. About 15% of respondents experience low probabilities of living in a high-poverty neighborhood from their mid-teens to their early 30s but an increasing risk thereafter. We refer to this group of respondents as the increasing neighborhood poverty group. Finally, 13% of our sample face a comparatively high risk of exposure to high-poverty neighborhoods in early life (i.e., before age 33) but generally lower neighborhood poverty in midlife. We call this group the decreasing neighborhood poverty group. In the subsequent analysis, we use the consistently low neighborhood poverty group as the reference group and include dummy variables for the other three groups to capture life-course exposure to high neighborhood poverty.
Fig. 1.
Latent class trajectories of residence in high-poverty neighborhoods: National Longitudinal Survey of Youth, 1979–2010
In addition to the neighborhood poverty measures, the analysis includes several individual-level characteristics as independent variables. We classify these variables into two groups—background characteristics and current socioeconomic status. Among the former, race/ethnicity has three groups: non-Hispanic whites (reference group), non-Hispanic blacks, and Latinos. We include two dummy variables to represent the minority groups in the analysis. Age at 1979 is measured in years and sex is coded 1 for females and 0 for males. Native-born respondents are coded 1 for nativity status with the foreign-born individuals serving as the reference group. If respondents lived in a family that received public assistance (AFDC, TANF, SSI, or other benefits) in 1978, they are coded 1 on public assistance; otherwise, they are coded 0. Parental education is measured by father’s years of schooling reported in 1979. If father’s information is missing, we replace it with mother’s education. Number of siblings is also taken from the 1979 interview.
With respect to current socioeconomic status, we use the data collected in the interview when respondents turned 40 years old to create four variables. Number of weeks worked since last interview reflects an individual’s working history in approximately the past 2 years. Marital status is a dichotomous variable in which married individuals are coded 1 and other statuses (e.g., singled or divorced) are coded 0. Individual income is log-transformed to address the skewness of income distribution. Respondents’ educational attainment is measured by their completed years of schooling.
Analytic Strategy
Our analytic strategy proceeds in two stages. We first conduct a descriptive analysis for the total sample and separately by latent class membership. The descriptive results offer a basic understanding of the bivariate associations of interest. We then apply Ordinary Least Squares (OLS) regression modeling to SF-12 physical health scores and logistic regression to self-rated health, respectively. For the multivariate analysis, we implement a series of models to understand how neighborhood poverty affects health. Model 1 includes all background and current socioeconomic status variables. We add early exposure to neighborhood poverty to model 2 and estimate the impact of concurrent exposure to neighborhood poverty on health in model 3. We then add the measure of life-course exposure to high-poverty neighborhoods to models 2 and 3, respectively, in order to evaluate the impacts of life-course exposure to neighborhood poverty on health net of the effects of early life (model 4) and contemporaneous (model 5) neighborhood poverty.
Results
Descriptive Findings
Descriptive statistics for all variables are presented in Table 1. Several differences across the four groups of life-course exposure to high neighborhood poverty are worth noting. First, respondents exposed to consistently low neighborhood poverty between the age of 15–23 and 45–53 have better health outcomes in middle adulthood than those in the other neighborhood poverty trajectory groups. Specifically, the average SF-12 physical health score is the highest in the consistently low neighborhood poverty group (53.048) and the lowest among those who have been consistently exposed to high neighborhood poverty (50.277). However, differences across the three groups that were exposed at least at some point in the life course to high-poverty neighborhoods are fairly small. In particular, respondents who were exposed to high-poverty neighborhoods only in midlife (the increasing neighborhood poverty group) exhibit SF-12 scores (50.987) that are quite similar to the consistently high neighborhood poverty group (50.277).
Table 1.
Descriptive statistics for variables used in analysis of health outcomes, by latent class: National Longitudinal Survey of Youth, 1979–2010 (N = 5696).
| Life-course exposure to high-poverty neighborhoods | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Total | Consistently low | Increasing | Decreasing | Consistently high | |||||
| Mean/% | S.D. | Mean/% | S.D. | Mean/% | S.D. | Mean/% | S.D. | Mean/% | S.D. | |
| Dependent variables | ||||||||||
| SF-12 physical health score | 52.061 | 7.955 | 53.048 | 6.922 | 50.987 | 9.456 | 51.559 | 8.039 | 50.277 | 8.969 |
|
Self-rated health (Good/Very Good/Excellent = 1) |
87.6% | – | 92.0% | – | 83.4% | – | 85.0% | – | 79.4% | – |
| Neighborhood Poverty | ||||||||||
| Early exposure (ages 15-23) | 0.131 | 0.133 | 0.091 | 0.100 | 0.123 | 0.120 | 0.177 | 0.141 | 0.230 | 0.163 |
| Current exposure (approximately age 40) | 0.161 | 0.123 | 0.088 | 0.051 | 0.252 | 0.102 | 0.178 | 0.113 | 0.300 | 0.132 |
| Life-course exposure | ||||||||||
| Consistently low neighborhood poverty | 54.3% | – | – | – | – | – | – | – | – | – |
| Increasing neighborhood poverty | 15.2% | – | – | – | – | – | – | – | – | – |
| Decreasing neighborhood poverty | 13.6% | – | – | – | – | – | – | – | – | – |
| Consistently high neighborhood poverty | 17.1% | – | – | – | – | – | – | – | – | – |
| Background characteristics | ||||||||||
| Race/ethnicity | ||||||||||
| Non-Hispanic white | 53.1% | – | 72.5% | – | 46.0% | – | 33.8% | – | 13.0% | – |
| Non-Hispanic black | 28.0% | – | 14.0% | – | 32.5% | – | 42.7% | – | 56.9% | – |
| Latino | 18.9% | – | 13.5% | – | 21.5% | – | 23.5% | – | 30.1% | – |
| Age at 1979 | 17.479 | 2.252 | 17.595 | 2.284 | 17.434 | 2.187 | 17.264 | 2.272 | 17.322 | 2.169 |
| Female | 52.3% | – | 51.7% | – | 53.2% | – | 53.7% | – | 53.8% | – |
| Receiving public assistance in 1978 | 1.6% | – | 0.8% | – | 1/6% | – | 2.5% | – | 3.3% | – |
| Nativity status (1 = native-born) | 94.0% | – | 94.3% | – | 94.2% | – | 93.7% | – | 92.7% | – |
| Parental education | 10.829 | 3.310 | 11.650 | 2.841 | 10.445 | 3.410 | 10.118 | 3.445 | 9.121 | 3.641 |
| Number of siblings | 3.819 | 2.633 | 3.281 | 2.251 | 4.128 | 2.760 | 4.246 | 2.811 | 4.918 | 3.027 |
| Current socioeconomic status | ||||||||||
| Number of weeks worked | 93.032 | 57.388 | 96.993 | 53.240 | 91.398 | 62.282 | 92.911 | 55.558 | 82.017 | 65.018 |
| Marital status (1 = married) | 58.5% | – | 69.6% | – | 48.2% | – | 49.7% | – | 39.0% | – |
| Logged income | 10.271 | 2.182 | 10.773 | 1.637 | 9.867 | 2.420 | 9.985 | 2.299 | 9.258 | 2.2822 |
| Years of education | 13.263 | 2.498 | 13.787 | 2.477 | 12.782 | 2.341 | 13.014 | 2.439 | 12.221 | 2.294 |
Note: Standard deviations (S.D.) for dummy variables not shown
Regarding self-rated health, 92% of respondents in the consistently low neighborhood poverty group report good health, but this figure drops fairly sharply for the other groups. Notably, only 79% of respondents experiencing consistently high neighborhood poverty report being in good health.
In terms of early exposure and current exposure to neighborhood poverty, respondents in the consistently low neighborhood poverty group resided in neighborhoods during both adolescence/young adulthood (i.e., ages 15–23) and midlife (i.e., ages 45–53) having average poverty rates of less than 10%. In sharp contrast, respondents exposed to consistently high neighborhood poverty resided in adolescence/young adulthood in neighborhoods with an average poverty rate of 23%. The disadvantaged situation of this group worsens in middle adulthood when the average neighborhood poverty increases to 30%. Respondents in the increasing neighborhood poverty group experience the largest difference in neighborhood poverty rates between adolescence/young adulthood and middle adulthood as the average neighborhood poverty increases by almost 13 percentage points (25.2–12.3%).
There is a considerable variation in the racial/ethnic composition of the latent classes. Almost three-quarters of respondents in the consistently low neighborhood poverty group (72.5%) are non-Hispanic whites, but whites comprise only 13% of the consistently high neighborhood poverty group. By contrast, non-Hispanic blacks constitute 57% of the consistently high neighborhood poverty group but only 14% of the persistently low neighborhood poverty group. Somewhat similarly, the percentage of Latinos is the lowest in the consistently low neighborhood poverty group (13.5%) and increases to at least 22% in other groups.
The mean age and sex composition are fairly similar across the four groups, but not surprisingly, respondents in the consistently high neighborhood poverty group are more disadvantaged than members of the other groups on several of the background variables. For example, compared to individuals in other groups, individuals who have been consistently exposed to high-poverty neighborhoods are more likely to have received public assistance in 1978, to have parents with low educational attainment, and to have more siblings.
The disadvantaged conditions faced in adolescence/young adulthood by members of the consistently high neighborhood poverty group extend to midlife socioeconomic status. For example, the average number of weeks worked since last interview is at least 9 weeks fewer among respondents who are consistently exposed to high neighborhood poverty compared to members of the other groups. Similarly, average income is the lowest in the consistently high neighborhood poverty group.
Analysis of SF-12 Physical Health
Table 2 presents the results of the linear regression analysis of the SF-12 physical health scores. As shown in model 1, SF-12 physical health scores are significantly associated with several background characteristics and indicators of current socioeconomic status. Net of other covariates, the physical health score among female respondents is 0.951 points lower than that of males. Native-born respondents report a worse physical health score than do foreign born respondents (b = − 1.319). Parental education is positively associated with individual’s physical health in middle adulthood. Every 1 year increase in parental education is associated with 0.107 points increase in SF-12 scores when respondents turn age 40. Respondents who work more weeks or have more years of schooling are healthier than those who work less often or have less education. Married individuals tend to have higher SF-12 scores (b = 0.600) than the unmarried. Among the four indicators of current socioeconomic status, log-transformed income is the only factor that is not significantly related to physical health.
Table 2.
Linear regression analysis of SF-12 physical health score at age 40 or older: National Longitudinal Survey of Youth, 1979–2010
| Variables | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | S.E. | β | S.E. | β | S.E. | β | S.E. | β | S.E. | ||||||
| Neighborhood poverty | |||||||||||||||
| Early exposure (ages 15-23) | −2.013 | (0.865) | * | −1.318 | (0.887) | ||||||||||
| Current exposure (approximately age 40) | −4.195 | (0.927) | *** | −1.603 | (1.170) | ||||||||||
|
Life-course exposure (ref: Consistently low neighborhood poverty) |
|||||||||||||||
| Increasing neighborhood poverty | −1.360 | (0.304) | *** | −1.126 | (0.351) | *** | |||||||||
| Decreasing neighborhood poverty | −0.880 | (0.328) | ** | −0.822 | (0.337) | * | |||||||||
| Consistently high neighborhood poverty | −1.439 | (0.333) | *** | −1.244 | (0.392) | ** | |||||||||
| Background characteristics | |||||||||||||||
| Race/ethnicity (ref: non-Hispanic white) | |||||||||||||||
| Non-Hispanic black | −0.205 | (0.258) | 0.031 | (0.277) | 0.112 | (0.267) | 0.409 | (0.287) | 0.319 | (0.276) | |||||
| Latino | 0.308 | (0.318) | 0.525 | (0.331) | 0.489 | (0.320) | 0.753 | (0.333) | * | 0.642 | (0.323) | * | |||
| Age at 1979 | −0.002 | (0.046) | 0.000 | (0.046) | −0.006 | (0.045) | −0.013 | (0.046) | −0.015 | (0.046) | |||||
| Female | −0.951 | (0.205) | *** | −0.957 | (0.205) | *** | −0.948 | (0.205) | *** | −0.948 | (0.205) | *** | −0.944 | (0.205) | *** |
| Receiving public assistance in 1978 | −1.483 | (0.822) | −1.466 | (0.822) | −1.378 | (0.821) | −1.339 | (0.821) | −1.324 | (0.821) | |||||
| Nativity status (1 = native-born) | −1.319 | (0.453) | ** | −1.324 | (0.453) | ** | −1.211 | (0.453) | ** | −1.195 | (0.453) | ** | −1.168 | (0.453) | ** |
| Parental education | 0.107 | (0.039) | ** | 0.102 | (0.039) | ** | 0.087 | (0.039) | * | 0.080 | (0.039) | * | 0.078 | (0.039) | * |
| Number of siblings | −0.016 | (0.043) | −0.019 | (0.043) | −0.012 | (0.043) | −0.007 | (0.043) | −0.005 | (0.043) | |||||
| Current socioeconomic status | |||||||||||||||
| Number of weeks worked | 0.027 | (0.002) | *** | 0.027 | (0.002) | *** | 0.027 | (0.002) | *** | 0.027 | (0.002) | *** | 0.027 | (0.002) | *** |
| Marital status (1 = married) | 0.600 | (0.225) | ** | 0.568 | (0.225) | * | 0.493 | (0.225) | * | 0.449 | (0.225) | * | 0.448 | (0.226) | * |
| Logged income | 0.084 | (0.053) | 0.076 | (0.053) | 0.057 | (0.053) | 0.049 | (0.053) | 0.048 | (0.053) | |||||
| Years of education | 0.398 | (0.046) | *** | 0.401 | (0.046) | *** | 0.376 | (0.046) | *** | 0.378 | (0.046) | *** | 0.371 | (0.046) | *** |
| Constant | 43.757 | (1.197) | *** | 44.004 | (1.201) | *** | 45.124 | (1.232) | *** | 45.310 | (1.223) | *** | 45.481 | (1.236) | *** |
| N | 5696 | 5696 | 5696 | 5696 | 5696 | ||||||||||
| R2 | 0.084 | 0.085 | 0.088 | 0.090 | 0.090 | ||||||||||
Note: Standard errors (S.E.) in parentheses
***p < 0.001, **p < 0.01, *p < 0.05
We include early-life exposure to neighborhood poverty in model 2 and find that on average every 10 percentage point increase in exposure to neighborhood poverty during adolescence/young adulthood decreases an individual’s SF-12 score by 0.201 points (− 2.013*0.1). Thus, even after adjusting for background characteristics and current socioeconomic status, early-life exposure to neighborhood poverty appears to have an adverse impact on individual physical health in middle adulthood. Including an individual’s early exposure to neighborhood poverty has little effect on the associations between background characteristics or current socioeconomic status and SF-12 scores found in model 1.
Model 3 estimates the impact of concurrent neighborhood poverty on physical health. Net of other covariates, a 10 percentage point increase in poverty of current residential neighborhoods is associated with a 0.420 point decrease in SF-12 scores (− 4.195*0.1). In contrast to the impact of early exposure to neighborhood poverty (model 2), the effect of concurrent exposure to neighborhood poverty is stronger, highlighting the importance of current residential neighborhoods in shaping individual health at midlife. These negative impacts of neighborhood poverty on physical health in models 2 and 3 offer support for our first hypothesis.
Model 4 of Table 2 includes both the measures of early-life exposure to neighborhood poverty and the trajectories of life-course exposure to high-poverty neighborhoods as captured by the latent classes. Compared to respondents who were consistently exposed to low-poverty neighborhoods (the reference group), all three groups that experienced at least some exposure to high-poverty neighborhoods exhibit significantly worse health at midlife. Not surprisingly, the largest difference is between respondents in the consistently high neighborhood poverty group and the consistently low neighborhood poverty group (1.439). However, physical health scores among the other groups are fairly similar. The physical health score is 1.36 points lower in the increasing neighborhood poverty group than in the consistently low neighborhood poverty group. Respondents in the decreasing neighborhood poverty group have an average physical health score that is 0.88 points lower than that reported by individuals who were consistently exposed to low-poverty neighborhoods.
Moreover, including the dummy variables capturing life-course exposure to high-poverty neighborhoods drives the coefficient for the early-life neighborhood poverty rate to statistical non-significance, supporting hypothesis 4. This finding suggests that early-life neighborhood poverty influences midlife health in large measure by shaping the subsequent life-course trajectory of neighborhood poverty. In addition, life-course exposure to high poverty neighborhoods tends to suppress the physical health advantage of Latinos compared to whites; the difference in health status between Latinos and non-Hispanic whites becomes statistically significant in model 4 (as well as model 5) when life-course exposure to neighborhood poverty is controlled.
Model 5 adds the life course neighborhood poverty dummy variables to model 3. As with model 4, the coefficients for the three neighborhood poverty latent classes are all negative and statistically significant. Also similar to model 4, the previously significant coefficient for the current neighborhood poverty ratio (model 3) becomes non-significant when life-course exposure to high neighborhood poverty is included in the model. Hence, the observed association between contemporaneous neighborhood poverty and physical health may be a consequence of an individual’s history of exposure to high neighborhood poverty. The findings in models 4 and 5 support hypotheses 2 and 4.
Analysis of Self-Rated Health
The logistic regression analysis of self-rated health is presented in Table 3. Without adjusting for any of the neighborhood poverty measures (model 1), the likelihood of reporting good self-rated health is significantly associated with a range of background characteristics and current socioeconomic status. For example, the odds that Latinos report being in good health are 23% lower than the corresponding odds for non-Hispanic whites ((exp(− 0.263) − 1)*100%). A single year increase in parental education is associated with a 3.25% increase in the odds of good self-rated health ((exp(0.032) − 1)*100%). Like the findings for the SF-12 physical health summary score, among the four current socioeconomic status variables, log-transformed income is the only factor that is not significantly associated with self-rated health.
Table 3.
Logistic regression analysis of self-rated health at age 40 or older: National Longitudinal Survey of Youth, 1979–2010
| Variables | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | S.E. | β | S.E. | β | S.E. | β | S.E. | β | S.E. | ||||||
| Neighborhood poverty | |||||||||||||||
| Early exposure (ages 15-23) | −0.724 | (0.332) | * | −0.501 | (0.344) | ||||||||||
| Current exposure (approximately age 40) | −1.585 | (0.346) | *** | −0.969 | (0.428) | * | |||||||||
|
Life-course exposure (ref: consistently low neighborhood poverty) |
|||||||||||||||
| Increasing neighborhood poverty | −0.495 | (0.121) | *** | −0.351 | (0.138) | * | |||||||||
| Decreasing neighborhood poverty | −0.390 | (0.134) | ** | −0.336 | (0.138) | * | |||||||||
| Consistently high neighborhood poverty | −0.466 | (0.130) | *** | −0.323 | (0.152) | * | |||||||||
| Background characteristics | |||||||||||||||
| Race/ethnicity (ref: non-Hispanic white) | |||||||||||||||
| Non-Hispanic black | −0.200 | (0.105) | −0.110 | (0.114) | −0.061 | (0.110) | 0.027 | (0.119) | 0.003 | (0.115) | |||||
| Latino | −0.263 | (0.128) | * | −0.176 | (0.134) | −0.179 | (0.130) | −0.088 | (0.137) | −0.131 | (0.132) | ||||
| Age at 1979 | 0.001 | (0.019) | 0.002 | (0.019) | −0.001 | (0.019) | −0.003 | (0.019) | −0.003 | (0.019) | |||||
| Female | −0.199 | (0.087) | * | −0.204 | (0.087) | * | −0.198 | (0.087) | * | −0.195 | (0.087) | * | −0.193 | (0.087) | * |
| Receiving public assistance in 1978 | −0.151 | (0.284) | −0.144 | (0.284) | −0.108 | (0.287) | −0.108 | (0.285) | −0.096 | (0.286) | |||||
| Nativity status (1 = native born) | −0.501 | (0.200) | * | −0.505 | (0.201) | * | −0.454 | (0.201) | * | −0.465 | (0.201) | * | −0.445 | (0.201) | * |
| Parental education | 0.032 | (0.016) | * | 0.031 | (0.016) | * | 0.024 | (0.016) | 0.023 | (0.016) | 0.021 | (0.016) | |||
| Number of siblings | −0.011 | (0.016) | −0.013 | (0.016) | −0.011 | (0.016) | −0.010 | (0.017) | −0.009 | (0.017) | |||||
| Current socioeconomic status | |||||||||||||||
| Number of weeks worked | 0.009 | (0.001) | *** | 0.009 | (0.001) | *** | 0.009 | (0.001) | *** | 0.009 | (0.001) | *** | 0.009 | (0.001) | *** |
| Marital status (1 = married) | 0.351 | (0.092) | *** | 0.339 | (0.092) | *** | 0.308 | (0.093) | *** | 0.298 | (0.093) | *** | 0.293 | (0.093) | ** |
| Logged income | 0.008 | (0.018) | 0.006 | (0.018) | 0.001 | (0.018) | −0.000 | (0.018) | −0.001 | (0.018) | |||||
| Years of education | 0.185 | (0.021) | *** | 0.186 | (0.021) | *** | 0.177 | (0.021) | *** | 0.177 | (0.021) | *** | 0.174 | (0.021) | *** |
| Constant | −1.042 | (0.487) | * | −0.944 | (0.490) | −0.522 | (0.503) | −0.477 | (0.503) | −0.365 | (0.507) | ||||
| N | 5696 | 5696 | 5696 | 5696 | 5696 | ||||||||||
Notes: Self-rated health scored 1 = good/very good/excellent; 0 = fair/poor. Standard errors (S.E.) in parentheses
***p < 0.001, **p < 0.01, *p < 0.05
Model 2 shows that early-life exposure to neighborhood poverty is negatively associated with self-rated health, net of other covariates. Specifically, a 10 percentage point increase in early exposure to neighborhood poverty decreases the odds of reporting at least good self-rated health by almost 7% ((exp(− 0.724*0.1) − 1)*100%). Controlling for early-life exposure to neighborhood poverty causes the difference in self-rated health between Latinos and whites to become statistically nonsignificant, indicating that the difference in self-rated health between Latinos and non-Hispanic whites may be attributed to the difference in exposure to neighborhood poverty.
A detrimental impact of current (i.e., time of survey) neighborhood poverty on self-rated health is shown in model 3. The odds of reporting good self-rated health decrease by almost 15% with a 10 percentage point increase in the poverty rate of the current residential neighborhood ((exp(− 1.585*0.1) − 1)*100%). The magnitude of the health impact of current neighborhood poverty is over twice that of early exposure to neighborhood poverty (model 2 in Table 3), indicating that current neighborhood poverty may play a larger role in shaping self-rated health than early exposure to neighborhood poverty.
Model 4 of Table 3 adds to model 2 the dummy variables capturing the life-course trajectories of exposure to high-poverty neighborhoods. Respondents who had spent some time living in a high-poverty neighborhood, irrespective of whether those residential spells were persistent or fleeting, exhibit significantly lower odds of reporting good self-rated health compared to respondents who lived consistently in low-poverty neighborhoods. The odds of reporting good health are almost 40% lower ((1-exp(− 0.495))*100%) among respondents in the increasing neighborhood poverty group than among those in the consistently low neighborhood poverty group. Similar differences are found for the other two neighborhood poverty trajectory groups. After controlling for these trajectories, the coefficient for the poverty rate of the neighborhood inhabited during adolescence/early adulthood becomes non-significant.
Model 5 includes as predictors both the contemporaneous neighborhood poverty ratio and life-course exposure to high-poverty neighborhoods. Life-course exposure to high neighborhood poverty remains inversely related to self-rated health. The odds of reporting good health among respondents who have experienced any exposure to high-poverty neighborhoods over the observed life-course are roughly 30% lower than respondents in the consistently low neighborhood poverty group. After controlling for the life-course trajectories, the negative impact of the poverty ratio of the current residential neighborhoods on self-rated health drops by approximately 40%—from − 1.585 (model 3) to − 0.969 (model 5)—but remains statistically significant. The results of models 3 and 5 of Table 3 generally support both hypotheses 2 and 4.
We conducted several additional analyses to assess the robustness of our findings. We calculated variance inflation factors (VIFs) for models 4 and 5 in our tables. No VIF is higher than 2.15, and the average VIF for all independent variables is lower than 1.5. Thus, multicollinearity does not appear to present a problem for our analysis. In supplementary analyses, we also included more covariates in the regression models, including individual employment status and number of children. These effects of these covariates were not significant for either health outcome and so are omitted from our final models. Finally, we replicated our analysis using measures of health status from when the NLSY79 respondents turned age 50. The results from these analyses were generally similar to the results from the presented analyses using data from the NSLY79 age 40 health module.
Discussion and Conclusions
Much recent research has focused on the impact of neighborhood poverty on health, often yielding mixed findings [32, 33]. The typical research design in this area uses single point-in-time measures of poverty for either the current residential neighborhoods or for some a community inhabited in early life. The current study argues that attention to the extent of exposure to high-poverty neighborhoods over the life course may enhance our understanding of how neighborhood poverty affects physical health. Exploiting the restricted information on individual residential histories provided by the National Longitudinal Survey of Youth, this study identifies four latent classes of life-course exposure to high poverty neighborhoods and investigates how these trajectories both affect physical health at midlife and alter the observed effects of early-life and concurrent neighborhood poverty.
Our analysis is designed to test several hypotheses regarding the impact of life-course exposure to neighborhood poverty on two measures of physical health—the SF-12 summary score and self-rated health. We first hypothesized that exposure to high levels of neighborhood poverty compromises physical health. Our results offer evidence to support this hypothesis. Even after adjusting for various background characteristics and current socioeconomic status, individuals living in high poverty neighborhoods have poorer health outcomes than their counterparts in low poverty neighborhoods. This finding accords with other studies reporting that neighborhood poverty is a significant determinant of physical health conditions or overall self-rated health [32, 58]. Our findings suggest that the poverty rate of individuals’ current residential neighborhood (i.e., in middle adulthood) has a stronger impact on health than neighborhood poverty measured during adolescence or young adulthood.
Our second hypothesis stated that life-course exposure to neighborhood poverty has a detrimental impact on midlife physical health even after controlling for the point-in-time exposure to neighborhood poverty during adolescence/young adulthood or middle adulthood. Our results yield strong support for this hypothesis. Categorizing life-course exposure to high-poverty neighborhoods into four groups via latent class analysis, we find that exposure to high neighborhood poverty has a consistent and adverse effect on physical health conditions and self-rated health measured when individuals are around 40 years old. This association exists even controlling for established individual-level predictors of physical health.
The third hypothesis posited that continuous exposure to high-poverty neighborhoods over the life-course has a stronger effect on midlife health outcomes than exposure to high neighborhood poverty experienced only during adolescence/young adulthood or only during middle adulthood. We find no support for this hypothesis. Differences in physical health between the consistently high neighborhood poverty group and both the increasing neighborhood poverty and decreasing neighborhood poverty groups are fairly small. This finding suggests that any fairly sustained exposure to high neighborhood poverty between adolescence/young adulthood and middle adulthood, regardless of whether this exposure occurs early or later in life, compromises individual health and that any additional exposure to neighborhood poverty does not seem to matter.
We also hypothesized that life-course exposure to neighborhood poverty at least partially accounts for the observed impacts of point-in-time exposure to neighborhood poverty during adolescence/young adulthood or middle adulthood. This hypothesis is largely supported by the results. When life-course exposure to neighborhood poverty is included in the analysis, the observed impacts of exposure to neighborhood poverty during adolescence/young adulthood (i.e., early exposure) on health outcomes become non-significant. This finding suggests that early-life exposure to neighborhood poverty affects later-life health at least partly by shaping the life-course trajectory of neighborhood poverty. A generally similar pattern is found for the relationship between exposure to neighborhood poverty during middle adulthood (i.e., contemporaneous exposure) and health outcomes (although for self-rated health the effect of contemporaneous neighborhood poverty remains significant). This finding suggests that measures of neighborhood poverty observed simultaneous to health outcomes are to a large extent capturing the effects of exposure to high-poverty neighborhoods over the life course.
This study contributes to the literature on neighborhoods and health in three main ways. First, our findings suggest that the relationship between neighborhood poverty and health may be better captured by considering the duration of exposure to poor neighborhoods over the life course than by utilizing single point-in-time measures of neighborhood poverty, either from early in the life course or at the time of survey [12, 33, 38, 39]. The failure of some prior cross-sectional studies [35, 59] to observe an effect of neighborhood poverty on later-life health may stem from their lack of attention to the duration of exposure to poor neighborhoods over the life course. Our findings also suggest that the oft-observed associations between the poverty rate of a neighborhood inhabited early in life or the current neighborhood of residence and health may in fact be capturing the influence of life-course exposure to neighborhood poverty. In the models of the SF-12 physical health score, the coefficients for both point-in-time measures of neighborhood poverty become non-significant when the measure of life-course exposure is included. Compared to prior research that focuses on change in neighborhood poverty or disadvantage [16, 17, 60, 61], our findings may be more robust because the LCA approach does not assume homogeneity within each trajectory and has greater statistical power. Importantly, our LCA analysis adopts an egocentric perspective [21] to identify trajectories experienced by individuals rather than patterns among neighborhoods (i.e., place-centric approach).
Second, although we observe generally more robust effects on midlife physical health of neighborhood poverty when measured over the life course than when measured at a single point in time, it nonetheless appears that point-in-time measures may serve as reasonable proxies for life-course measures. When life-course measures are excluded from the models, the neighborhood poverty rate measured either in adolescence/young adulthood or at midlife is significantly associated with midlife physical health. This finding might comfort researchers whose datasets lack respondent residential histories and who therefore must rely solely on neighborhood characteristics measured at a single time point, typically the survey date. Of course, whether this finding holds for other neighborhood characteristics and for other health outcomes awaits further research.
Third, our results suggest that among individuals who ever reside in a poor neighborhood, both the timing and duration of exposure to neighborhood poverty may be largely immaterial. We find only slight differences in physical health among individuals who consistently lived in high-poverty neighborhoods versus those who lived in high-poverty neighborhoods only during adolescence or only during mid-adulthood. One implication of this finding is that relocating individuals who grew up in a poor neighborhood to non-poor neighborhoods later in life may not completely eliminate the health disadvantages of early-life exposure to neighborhood poverty. Growing up in a poor neighborhood appears to exert a long-lasting influence on health even among individuals who reside in mostly low-poverty neighborhoods later in life. By the same token, the health-enhancing influence of growing up in a low-poverty neighborhood can be eliminated if individuals reside in mostly high-poverty neighborhoods during early and middle adulthood.
Of course, our study is not without limitations. First, the results and findings may be sensitive to how neighborhoods are defined. Though census tracts are widely used in neighborhood effects research [46], using a different administrative or geographical unit (e.g., block groups or ZIP codes) to define neighborhoods may lead to different conclusions [62]. Second, this study does not consider neighborhood conditions other than poverty. Although neighborhood poverty has been identified as a robust indicator that captures much of the association between neighborhood social environment and health [63], future research might benefit from adopting a life-course approach to the effects of other neighborhood conditions. Third, our findings may not be generalizable to other cohorts or populations as NLSY79 targets those who were born between 1957 and 1964. Fourth, our analysis does not explore the potential mechanisms through which neighborhood poverty may affect physical health [45, 64]. Due to the data limitations, several potential mediators, such as collective efficacy [5, 34], are not available in the NLSY79. Future research might profit from investigating how neighborhood poverty gets “under the skin” over the life course. Finally, the NLSY79 does not record respondents’ residential neighborhoods prior to the initial 1979 survey and thus we are unable to consider the effects of exposure to neighborhood poverty during early childhood (cf. [65]). Future effort might consider developing life-course measures of neighborhood poverty that incorporate the childhood years.
In sum, our results suggest that a life-course approach can enhance our understanding of how neighborhood poverty affects physical health. Physical health at midlife appears to be shaped by the frequency of lifetime exposure to high-poverty neighborhoods, and these effects appear stronger than more commonly used single-point-in-time measures of neighborhood poverty. Future research on the effects of neighborhood poverty on other health outcomes and related behaviors may likewise benefit from adopting a life-course approach.
Acknowledgement
We appreciate the constructive suggestions from the reviewers. We also thank the Bureau of Labor Statistics for helping us to access the restricted data (only available via contractual arrangements). We acknowledge the support from the Center for Social and Demographic Analysis, which receives funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R24-HD044943). In addition, the corresponding author would like to acknowledge the support from the Ministry of Science and Technology (Taiwan) and the Institute of Sociology, Academia Sinica (MOST 107-2420-H-001-003-SS2).
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rumsfeld JS, MaWhinney S, McCarthy M Jr, Shroyer AL, VillaNueva C, O'Brien M, Moritz TE, Henderson WG, Grover FL, Sethi GK, Hammermeister KE. Health-related quality of life as a predictor of mortality following coronary artery bypass graft surgery. JAMA. 1999;281(14):1298–1303. doi: 10.1001/jama.281.14.1298. [DOI] [PubMed] [Google Scholar]
- 2.Lacson E, et al. A comparison of SF-36 and SF-12 composite scores and subsequent hospitalization and mortality risks in long-term dialysis patients. Clin J Am Soc Nephrol. 2010;5(2):252–260. doi: 10.2215/CJN.07231009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question: a meta-analysis. J Gen Intern Med. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69(3):307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 5.Stretton CM, Latham NK, Carter KN, Lee AC, Anderson CS. Determinants of physical health in frail older people: the importance of self-efficacy. Clin Rehabil. 2006;20(4):357–366. doi: 10.1191/0269215506cr946oa. [DOI] [PubMed] [Google Scholar]
- 6.Kawachi I, Kennedy BP, Glass R. Social capital and self-rated health: a contextual analysis. Am J Public Health. 1999;89(8):1187–1193. doi: 10.2105/ajph.89.8.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heard HE, Gorman BK, Kapinus CA. Family structure and self-rated health in adolescence and young adulthood. Popul Res Policy Rev. 2008;27(6):773–797. [Google Scholar]
- 8.Giatti L, Barreto SM, César CC. Household context and self-rated health: the effect of unemployment and informal work. J Epidemiol Community Health. 2008;62(12):1079–1085. doi: 10.1136/jech.2007.069740. [DOI] [PubMed] [Google Scholar]
- 9.Franks P, Gold MR, Fiscella K. Sociodemographics, self-rated health, and mortality in the US. Soc Sci Med. 2003;56(12):2505–2514. doi: 10.1016/s0277-9536(02)00281-2. [DOI] [PubMed] [Google Scholar]
- 10.Ellis C, Grubaugh AL, Egede LE. Factors associated with SF-12 physical and mental health quality of life scores in adults with stroke. J Stroke Cerebrovasc Dis. 2013;22(4):309–317. doi: 10.1016/j.jstrokecerebrovasdis.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 11.Fleishman JA, Lawrence WF. Demographic variation in SF-12 scores: true differences or differential item functioning? Med Care. 2003;41(7):III75–86. [DOI] [PubMed]
- 12.Wen M, Browning CR, Cagney KA. Poverty, affluence, and income inequality: neighborhood economic structure and its implications for health. Soc Sci Med. 2003;57(5):843–860. doi: 10.1016/s0277-9536(02)00457-4. [DOI] [PubMed] [Google Scholar]
- 13.Yen IH, Kaplan GA. Poverty area residence and changes in depression and perceived health status: evidence from the Alameda County study. Int J Epidemiol. 1999;28(1):90–94. doi: 10.1093/ije/28.1.90. [DOI] [PubMed] [Google Scholar]
- 14.Arcaya MC, Tucker-Seeley RD, Kim R, Schnake-Mahl A, So M, Subramanian SV. Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Soc Sci Med. 2016;168:16–29. doi: 10.1016/j.socscimed.2016.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lippert AM. Stuck in unhealthy places: how entering, exiting, and remaining in poor and nonpoor neighborhoods is associated with obesity during the transition to adulthood. J Health Soc Behav. 2016;57(1):1–21. doi: 10.1177/0022146515627682. [DOI] [PubMed] [Google Scholar]
- 17.Brazil N, Clark WA. Individual mental health, life course events and dynamic neighbourhood change during the transition to adulthood. Health Place. 2017;45:99–109. doi: 10.1016/j.healthplace.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 18.South SJ, Crowder K. Neighborhood poverty and nonmarital fertility: spatial and temporal dimensions. J Marriage Fam. 2010;72(1):89–104. doi: 10.1111/j.1741-3737.2009.00685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang T-C, South SJ. Neighborhood effects on body mass: temporal and spatial dimensions. Soc Sci Med. 2018;217:45–54. doi: 10.1016/j.socscimed.2018.09.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haan M, Kaplan GA, Camacho T. Poverty and health prospective evidence from the alameda county study. Am J Epidemiol. 1987;125(6):989–998. doi: 10.1093/oxfordjournals.aje.a114637. [DOI] [PubMed] [Google Scholar]
- 21.Sheehan CM, Cantu PA, Powers DA, Margerison-Zilko CE, Cubbin C. Long-term neighborhood poverty trajectories and obesity in a sample of California mothers. Health Place. 2017;46:49–57. doi: 10.1016/j.healthplace.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bodor JN, Rice JC, Farley TA, Swalm CM, Rose D. Disparities in food access: does aggregate availability of key foods from other stores offset the relative lack of supermarkets in African-American neighborhoods? Prev Med. 2010;51(1):63–67. doi: 10.1016/j.ypmed.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.LaVeist TA, Wallace JM. Health risk and inequitable distribution of liquor stores in African American neighborhood. Soc Sci Med. 2000;51(4):613–617. doi: 10.1016/s0277-9536(00)00004-6. [DOI] [PubMed] [Google Scholar]
- 24.Moore LV, Diez Roux AV. Associations of neighborhood characteristics with the location and type of food stores. Am J Public Health. 2006;96(2):325–331. doi: 10.2105/AJPH.2004.058040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42:258–276. [PubMed] [Google Scholar]
- 26.Boardman JD, Robert SA. Neighborhood socioeconomic status and perceptions of self-efficacy. Sociol Perspect. 2000;43(1):117–136. [Google Scholar]
- 27.Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. Am J Prev Med. 2008;34(1):16–22. doi: 10.1016/j.amepre.2007.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sampson RJ. The neighborhood context of well-being. Perspect Biol Med. 2003;46(3):S53–S64. [PubMed] [Google Scholar]
- 29.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Massey DS, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Cambridge, MA: Harvard University Press; 1993.
- 31.South SJ, Huang Y, Spring A, Crowder K. Neighborhood attainment over the adult life course. Am Sociol Rev. 2016;81(6):1276–1304. doi: 10.1177/0003122416673029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Do DP, Finch BK. The link between neighborhood poverty and health: context or composition? Am J Epidemiol. 2008;168(6):611–619. doi: 10.1093/aje/kwn182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Browning CR, Cagney KA. Moving beyond poverty: neighborhood structure, social process, and health. J Health Soc Behav. 2003;44(4):552–571. [PubMed] [Google Scholar]
- 34.Browning CR, Cagney KA. Collective efficacy and health: neighborhood social capital and self-rated physical functioning in an urban setting. J Health Soc Behav. 2002;43(4):383–399. [PubMed] [Google Scholar]
- 35.Brown AF, Ang A, Pebley AR. The relationship between neighborhood characteristics and self-rated health for adults with chronic conditions. Am J Public Health. 2007;97(5):926–932. doi: 10.2105/AJPH.2005.069443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Osypuk TL, Acevedo-Garcia D. Beyond individual neighborhoods: a geography of opportunity perspective for understanding racial/ethnic health disparities. Health Place. 2010;16(6):1113–1123. doi: 10.1016/j.healthplace.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Robert SA. Socioeconomic position and health: the independent contribution of community socioeconomic context. Annu Rev Sociol. 1999;25(1):489–516. [Google Scholar]
- 38.Johnson RC, Schoeni RF, Rogowski JA. Health disparities in mid-to-late life: the role of earlier life family and neighborhood socioeconomic conditions. Soc Sci Med. 2012;74(4):625–636. doi: 10.1016/j.socscimed.2011.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Johnson RC, Schoeni RF. Early-life origins of adult disease: national longitudinal population-based study of the United States. Am J Public Health. 2011;101(12):2317–2324. doi: 10.2105/AJPH.2011.300252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Oakes JM, Andrade KE, Biyoow IM, Cowan LT. Twenty years of neighborhood effect research: an assessment. Curr Epidemiol Rep. 2015;2(1):80–87. doi: 10.1007/s40471-015-0035-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Murray ET, Diez Roux AV, Carnethon M, Lutsey PL, Ni H, O'Meara ES. Trajectories of neighborhood poverty and associations with subclinical atherosclerosis and associated risk factors: the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2010;171(10):1099–1108. doi: 10.1093/aje/kwq044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jimenez MP, Wellenius GA, Subramanian SV, Buka S, Eaton C, Gilman SE, Loucks EB. Longitudinal associations of neighborhood socioeconomic status with cardiovascular risk factors: a 46-year follow-up study. Soc Sci Med. 2019;241:112574. doi: 10.1016/j.socscimed.2019.112574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Elder GH. The life course as developmental theory. Child Dev. 1998;69(1):1–12. [PubMed] [Google Scholar]
- 44.Elder GH, Giele JZ, eds. The Craft of Life Course Research. New York, NY: The Guilford Press; 2009.
- 45.Galster GC. The mechanism (s) of neighbourhood effects: theory, evidence, and policy implications. In: van Ham M, Manley D, Bailey N, Simpson L, Maclennan D, editors. Neighbourhood Effects Research: New Perspectives. New York, NY: Springer; 2012. p. 23–56.
- 46.Matthews SA, Yang TC. Spatial Polygamy and Contextual Exposures (SPACEs): promoting activity space approaches in research on place and health. Am Behav Sci. 2013;57(8):1057–81. [DOI] [PMC free article] [PubMed]
- 47.Bureau of Labor Statistics, National Longitudinal Survey of Youth 1979 cohort, 1979–2010 (rounds 1–24). The Ohio State University. Center for Human Resource Research, Columbus, Ohio, 2010.
- 48.National longitudinal surveys. Retention & Reasons for Noninterview. 2014 [cited 2017 September 4]; Available from: https://www.nlsinfo.org/content/cohorts/nlsy79/intro-to-the-sample/retention-reasons-noninterview.
- 49.Ware JE, Kosinski M, Keller SD. SF-12: how to score the SF-12 physical and mental health summary scales: Health institute, New England Medical Center; Boston, Massachusetts 1995.
- 50.Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 51.Bureau of Labor Statistics, U.S. Department of Labor. National Longitudinal Survey of Youth 1979 cohort, 1979–2010 (rounds 1–24). 2012, roduced and distributed by the Center for Human Resource Research, Columbus, Ohio.
- 52.GeoLytics, Neighborhood Change Database [NCDB] Tract Data from 1970–2010. 2014: East Brunswick, NJ.
- 53.Margerison-Zilko C, Cubbin C, Jun J, Marchi K, Fingar K, Braveman P. Beyond the cross-sectional: neighborhood poverty histories and preterm birth. Am J Public Health. 2015;105(6):1174–1180. doi: 10.2105/AJPH.2014.302441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hagenaars JA, McCutcheon AL, eds. Applied Latent Class Analysis. New York, NY: Cambridge University Press; 2002.
- 55.Lanza ST, Rhoades BL. Latent class analysis: an alternative perspective on subgroup analysis in prevention and treatment. Prev Sci. 2013;14(2):157–168. doi: 10.1007/s11121-011-0201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Collins LM, Lanza ST. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences. Hoboken, NJ: Wiley & Sons; 2010.
- 57.Ramaswamy V, Desarbo WS, Reibstein DJ, Robinson WT. An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Mark Sci. 1993;12(1):103–124. [Google Scholar]
- 58.Kobetz E, Daniel M, Earp J. Neighborhood poverty and self-reported health among low-income, rural women, 50 years and older. Health Place. 2003;9(3):263–271. doi: 10.1016/s1353-8292(02)00058-8. [DOI] [PubMed] [Google Scholar]
- 59.Tomey K, Diez Roux AV, Clarke P, Seeman T. Associations between neighborhood characteristics and self-rated health: a cross-sectional investigation in the multi-ethnic study of atherosclerosis (MESA) cohort. Health Place. 2013;24:267–274. doi: 10.1016/j.healthplace.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jivraj S, Norman P, Nicholas O, Murray ET. Are there sensitive neighbourhood effect periods during the life course on midlife health and wellbeing? Health Place. 2019;57:147–156. doi: 10.1016/j.healthplace.2019.03.009. [DOI] [PubMed] [Google Scholar]
- 61.Kravitz-Wirtz N. Cumulative effects of growing up in separate and unequal neighborhoods on racial disparities in self-rated health in early adulthood. J Health Soc Behav. 2016;57(4):453–470. doi: 10.1177/0022146516671568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Openshaw, S., The Modifiable Areal Unit Problem. 1984, Norwich, England.
- 63.Krieger N, et al. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? The Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156(5):471–482. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 64.Turner RJ, Thomas CS, Brown TH. Childhood adversity and adult health: evaluating intervening mechanisms. Soc Sci Med. 2016;156:114–124. doi: 10.1016/j.socscimed.2016.02.026. [DOI] [PubMed] [Google Scholar]
- 65.Vartanian TP, Houser L. The effects of childhood neighborhood conditions on self-reports of adult health. J Health Soc Behav. 2010;51(3):291–306. doi: 10.1177/0022146510378241. [DOI] [PubMed] [Google Scholar]