The COVID-19 epidemic has threatened to overwhelm the health-care systems of European countries resulting in government decisions of extensive societal lockdowns. There have been considerable concerns regarding the collateral effects of the COVID-19 epidemic overshadowing the care of patients with other medical conditions including cardiovascular diseases. Of interest, decreases in the registered incidences of atrial fibrillation (AF) and ischemic stroke have been reported [1,2]. AF is a common reason for physician contact and AF patients are often recommended treatment with oral anticoagulants to mitigate the associated risk of thromboembolic events (TE). Due to the COVID-19 crisis, it could be feared that patients with AF would refrain from consulting their health-care provider resulting in suboptimal care potentially reflected by an increase in the proportion of thromboembolic complications related to AF.
Using Danish nationwide administrative registries, we examined patients with a hospital contact due to incident TE following the COVID-19 lockdown in Denmark (effectuated on the 12 March 2020) as well as the corresponding period in 2019. Data regarding the diseases of interest were obtained from diagnostic codes in the Danish National Patient Registry, which contains information on all hospital contacts in Denmark as described in more detail elsewhere [3,4]. We included all patients above 18 years of age with a hospital contact registered with a primary diagnosis of either ischemic stroke, transient ischemic attack or systemic embolism. Of interest, we analyzed the proportion of AF-related TEs to the total amount of TEs in the period. AF was defined as a registered diagnosis of AF prior to or in relation with hospitalization due to TE.
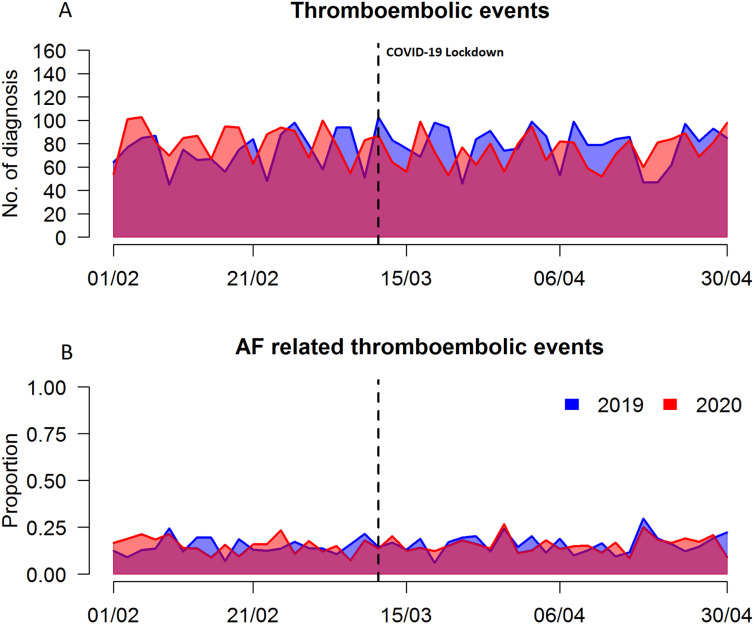
In the COVID-19 lockdown period in Denmark from the 12 March until 2 May 2020, we identified 1860 cases of incident TEs. In the same time period in 2019 there were 2067 cases of TEs (Fig. 1A). There were no major differences in patient characteristics between 2020 and 2019 with respect to median age (73 years, interquartile range [IQR] 63–80 vs. 72 years [IQR 62–80], P = 0.395) or sex (54.2% vs. 53.8% males, P = 0.952).
Fig. 1.
A: Plot depicting frequencies of thromboembolic events from 1 February to the end of April in 2020 (red) and the corresponding period in 2019 (blue). The COVID-19 lockdown illustrated by the dotted line. The y-axis depicts the number of thromboembolic events (No.) and the x-axis depicts days from 1 February in 2020.
B: Plot depicting the proportion of AF-related thromboembolic events from 1 February to the end of April in 2020 (red) and the corresponding period in 2019 (blue). The y-axis depicts the proportion of atrial fibrillation related thromboembolic events and the x-axis depicts days from 1 February in 2020. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
We did not observe any difference in the proportion of TEs related to AF during the lockdown in 2020 and the corresponding period in 2019 (15.7% vs. 15.6%, P = 0.945). The proportion of patients with AF-related TEs remained relatively stable throughout the period of interest (after 12 March) as well as the preceding weeks in both 2020 and 2019 (Fig. 1B).
The perspective of patients with acute or subacute conditions requiring medical attention refraining from seeking physician treatment due to COVID-19 is worrisome and warrants further investigations especially regarding the potential associated effects on patient outcomes [5]. It could be speculated that perceptions regarding symptom severity have been affected in the COVID-19 situation due to a desire to avoid healthcare providers out of fear of becoming infected or disturbing caregivers, especially in case of perceived mild symptoms.
Reassuringly, in a Danish context, we could not find indications that the proportion of AF-related TEs has increased as a result of inadequate anticoagulation strategies during the lockdown period as could be feared. However, it is unknown whether a delayed effect of the lockdown will be observed later on and the development in registered diseases should be closely monitored.
Consequently, contemporary Danish data do not point toward an excess of thromboembolic complications associated with AF during the COVID-19 lockdown suggesting timely treatment and visitation of AF patients. In this context, it is worth noting the major role telemedicine has played in the outpatient clinics during the lockdown and it could be speculated whether this has resulted in adequate care and could potentially continue to do so in the future.
Funding
There is no funding to declare for this study.
Declaration of competing interest
None of the authors have conflicts of interests to declare in relation to this study.
References
- 1.Holt A., Gislason G.H., Schou M., Zareini B., Biering-Sørensen T., Phelps M., Kragholm K., Andersson C., Fosbøl E.L., Hansen M.L., Gerds T.A., Køber L., Torp-Pedersen C., Lamberts M. New-onset atrial fibrillation: incidence, characteristics, and related events following a national COVID-19 lockdown of 5.6 million people. Eur. Heart J. 2020 doi: 10.1093/eurheartj/ehaa494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kansagra A.P., Goyal M.S., Hamilton S., Albers G.W. Collateral effect of Covid-19 on stroke evaluation in the United States. N. Engl. J. Med. 2020;383:400–401. doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rasmussen P.V., Dalgaard F., Gislason G.H., Brandes A., Johnsen S.P., Grove E.L., Torp-Pedersen C., Dybro L., Harboe L., Münster A.-M.B., Pedersen L., Blanche P., Pallisgaard J.L., Hansen M.L. Gastrointestinal bleeding and the risk of colorectal cancer in anticoagulated patients with atrial fibrillation. Eur. Heart J. 2020 doi: 10.1093/eurheartj/ehz964. [DOI] [PubMed] [Google Scholar]
- 4.Schmidt M., Schmidt S.A.J., Sandegaard J.L., Ehrenstein V., Pedersen L., Sørensen H.T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin. Epidemiol. 2015;7:449–490. doi: 10.2147/CLEP.S91125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur. Heart J. 2020;41(9):1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]