Abstract
Aim
The aim of the study was to evaluate the influence of autologous platelet-rich fibrin (PRF) on soft tissue healing and bone regeneration following tooth extraction clinically and radio-graphically.
Materials and methods
30 Patients between the age group of 18–40 years requiring extraction of bilateral mandibular molars except third molars were selected to conduct a split-mouth study after ethical approval. Teeth extraction was done on both sides in the same appointment. Autologous PRF was placed into the socket on one side randomly, and the socket on the other side was taken as control side. Parameters evaluated were soft tissue healing and bone regeneration. Soft tissue healing was evaluated on post-extraction day-3, day-7 and day-14 using healing index by Landry et al. Bone regeneration was assessed immediately and 4 months post-extraction by observation of change in radiopacity through digital panoramic-radiograph. Data obtained was statistically analysed and comparison of outcome variables was done using Mann-Whitney U-test, p < 0.05 was considered statistically significant.
Results
Case group had better soft tissue healing when compared to the control group with the p-value of 0.025 at 3rd day 0.039 at 7th day and 0.00 at 14th day. The rise in radiopacity at the end of 16th week for PRF group was higher as compared to control group but did not differ significantly.
Conclusion
PRF is significantly better in promoting soft tissue healing and also hastens bone formation in extraction socket. PRF may be recommended as a valuable material for encouraging soft tissue healing and bone regeneration.
Keywords: Bone regeneration, Platelet rich fibrin, Wound healing, Post extraction socket
1. Introduction
Extraction of teeth because of pulpal, periapical and periodontal disease is one of the most common procedures in oral surgery.1,2 Following tooth extraction, the wound healing and loss of alveolar bone volume is unpredictable. This can pose a problem for future rehabilitation with conventional as well as implant-supported prosthesis. For these reasons, socket grafting has now become a popular practice for the preservation of the extraction socket. In pursuit of that various biocompatible, biodegradable, and non-toxic synthetic or natural biomaterials have been quested and tested against time for their competency to achieve accelerated healing and to reduce alveolar ridge dimensional changes post-extraction, however, none of those have shown promising results in prevention of resorption.3 In this regards autologous platelet concentrates including platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) have gained significant popularity in tissue engineering.
The Platelet-rich fibrin (PRF) is a second-generation derivative of natural fibrin-based biomaterial derived by centrifugation of harvested blood. No anticoagulant or bovine thrombin is needed for this technique thus it is simpler, economic and biochemically safe to prepare.4 Besides, the preparation is rich in platelets and leucocytes within the mesh of fibrin enriched in all the constituents essential for wound healing and bone regeneration including various cytokines, and circulating stem cells.5
Extensive research is undergoing on the regenerative potential and reparative capacity of PRF on soft and hard tissue in various clinical settings. One potential aspect of research that has gained tremendous popularity in recent years is the impact of PRF in the management of dimensional changes of the alveolar bone following tooth extraction.
Multiple reports have demonstrated the positive impact of PRF on Alveolar ridge preservation following the tooth extraction, while some have noted the inadequacy of the evidence on its effectiveness on bone regeneration. A concern raised by Castro et al.6 in the systematic review on the assessment of the effect of platelet-rich fibrin on bone regeneration after tooth extraction states that most studies performed for this purpose were undertaken following surgical extraction of third molars. Buccal mucoperiosteal flap elevation for third molar extraction hinders the blood supply to the buccal cortical bone results in greater resorption and increases the risk of gingival recession.7,8 Several other factors can affect the healing process and bone regeneration after surgical extraction of the third molar compared to the extraction of other teeth like complexity and difficulty involved and the amount of bone removal required in the extraction. Moreover, the third molar after extraction rarely replaced with conventional or implant-supported prosthesis hence the true therapeutic potential of PRF does not seems to be clinically demonstrated in socket preservation using third molars. Thus this study was carried out on mandibular molars except for the third molars, require prosthetic rehabilitation. As molar crests have higher resorption rates than in premolar and anterior regions, so the current research was conducted on mandibular molars.9 The study aimed to evaluate the outcome of platelet-rich fibrin (PRF) on soft tissue healing and bone regeneration in the extraction socket and verify them clinically and radiographically. This was done with a goal to provide an insight into tissue regeneration and the reparative potential of PRF as sole graft material.
2. Materials and methods
2.1. Participants selection
The present study was carried out on 30 patients who visited the Oral Surgery outpatient department over a period of 2 years, undergoing extraction of mandibular teeth simultaneously on both sides. The study was designed as a prospective split-mouth clinical trial and the study protocol was approved by the Institutional Ethical committee. The study was performed as per the Helsinki declaration. Inclusion criteria consisted of healthy patients of age group between 18 and 45 years requiring extraction of bilateral mandibular molars except third molars were included in the study (Fig. 1A). Patients with possible allergies or hypersensitivity to drugs such as antibiotics and anti-inflammatory drugs, medically compromised patient, Pregnant females, Teeth with periodontal or periapical infection i.e. large abscess or any pathological condition i.e. cyst were excluded from the study. All patients were informed about the benefits and risks associated with the procedure after which a written, valid, informed consent was taken from all the patients. Selection of case side to which the PRF was placed decided by computer-generated program research randomizer,10 and the unique set of 15 numbers that were generated by the program was considered as the number of patients in which case side to be taken on right side of mandible and control on the left side.
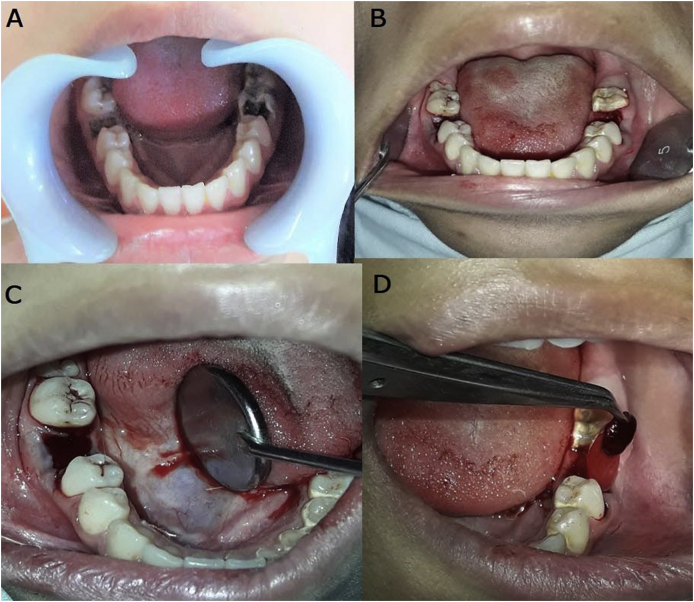
Fig. 1.
(A) Grossly carious mandibular first molar bilaterally.(B) Extraction of mandibular first molar bilaterally.(C) No PRF placement in extraction socket on control side.(D) PRF placement in extraction socket on experimental side.
Hence two groups were formed consisting of 30 extraction sites each.
Case Group: Extraction sockets which received platelet-rich fibrin.
Control Group: Extraction sockets were allowed to heal normally.
2.2. Surgical procedure
All patients received local anesthetic blockade of buccal, lingual and inferior alveolar nerves bilaterally via 3 ml of 2% lignocaine with 1:200,000 adrenaline to achieve profound subjective and objective dental anesthesia. Just prior to surgery, 6 ml intravenous blood was collected in a 10-ml sterile tube without anticoagulant and immediately centrifuged in the LabTech AVI-532-BL centrifugation machine at 3000 rpm for 10 min and the fresh autologous PRF was prepared.11 Extraction of the tooth on both case and control side was done as atraumatic as possible in the same appointment (Fig. 1B). After the tooth extraction, No PRF was placed in the extraction socket on the control side and the socket was allowed to heal naturally with no suture placement (Fig. 1C). PRF was inserted into the extraction socket in the case group (Fig. 1D) and a figure of eight suture was placed to prevent accidental removal of PRF from the socket. (this suture was removed on 3rd day post extraction). All patients were given postoperative instructions along with an appropriate course of antibiotics (amoxicillin 500 mg TDS) and analgesic (diclofenac 50 mg TDS) for a minimum period of three days.
2.3. Clinical and radiographic evaluation
Patients were recalled on post-extraction day 3, day 7 and day 14 for evaluation of soft tissue healing. Healing index by Landry R.G., Turnbull R.S., Howley T.12 was adapted which involved 5 scoring levels for each of the 4 parameters (Table 1) on day 3, day 7 and day 14 by the same investigator and appropriate response was recorded. Bone regeneration was expressed as a rise in radiopacity and interpreted as higher optical density in the radiographic image of the bone. Mean grayscale value was obtained by the addition of the grayscale values of all the pixels in the region of interest divided by the number of pixels. Mean grayscale value provides the numerical values about radiopacity, thus indicating bone healing. Bone regeneration evaluation in the present study was done by direct observation of grayscale value through digital panoramic radiographs with software Radiant DICOM Viewer (version 4.0.3) to calculate image density of the socket after extraction. This software quantified image contrast density with the mean of pixel value or Hounsfield units for computerized axial tomography images indicating relative bone densities.13 For every patient, Digital Panoramic Radiograph was done immediately after extraction and after 16 weeks, all exposures were standardized at 75 Kvp 10 mA for 15.29 s.
Table 1.
Components of Soft Tissue Healing Index by Landry et al.
| Grade | Remark |
|---|---|
| 1.Very poor | Tissue color ≥50% gingiva red Response to palpation:bleeding Granulation tissue:present Suppuration:present |
| 2.Poor | Tissue color ≥50% of gingiva red Response to palpation: bleeding Granulation tissue: present Suppuration:none |
| 3.Good | Tissue color ≥25% but <50% of gingiva red Response to palpation: no bleeding Granulation tissue:none Suppuration:none |
| 4.Very good | Tissue color <25% gingiva red Response to palpation: no bleeding Granulation tissue:none Suppuration:none |
| 5.Excellent | Tissue color:all tissue is pink and healthy Response to palpation:no bleeding Granulation tissue: none Suppuration: none |
Using the ellipse tool in the image viewer of the Digital Panoramic Radiograph the same dimensions of the region of interest of each extraction socket were studied on both case and control side immediately after extraction and after 16th week.
Data obtained were subjected to statistical analysis using Statistical package for social sciences (SPSS) Statistics for Windows, version 21.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics like mean age & other numerical variables, percentage & frequencies of gender-wise distribution & other nominal variables have been depicted. Kolmogorov-Smirnov test was used to check the normality of data. Comparison of outcome variables like soft tissue healing, mean grayscale value & change in grayscale value between the groups was done using the Mann-Whitney U test. For the statistical test, p < 0.05 was considered to be statistically significant, keeping α error at 5% and β error at 20%, thus giving power to the study as 80%.
3. Results
A total of 30 patients, 14 (46.7%) male, and 16 (53.3%) female patients were selected with a total of 60 surgical sites (30 cases and 30 controls). The age of the patients included in the study ranged between 18 and 45 years with the mean age of 23.90 yrs.
3.1. Soft tissue healing
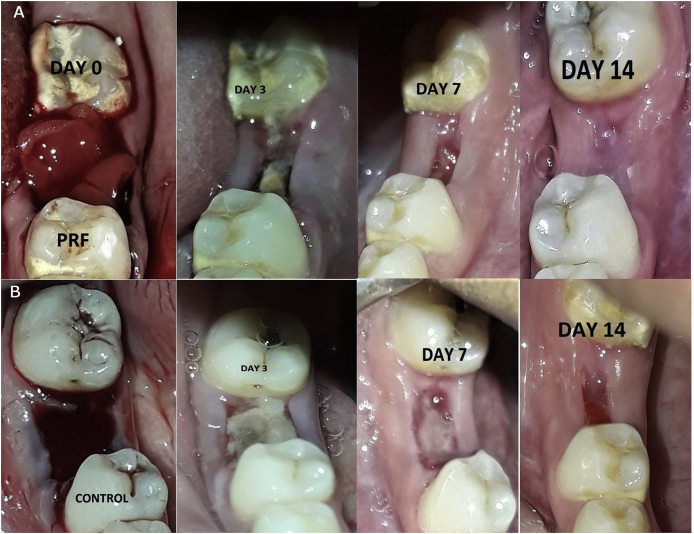
Soft tissue healing on the day 3 and day 7 post extraction was found to be better in cases than the controls and there was a statistically significant difference (p-value < 0.05) seen in soft tissue healing between the 2 groups with mean higher on the experimental side with the average value of (3.43 ± 0.504) at day 3 and (3.93 ± 0.254) at day 7 and (4.83 ± 0.379) at day 14 as contrary to experiment side the control side has average value (3.17 ± 0.379) at day 3 (3.73 ± 0.082) day 7, and (4.3 ± 0.46) at day 14 (Fig. 2A and B),with the p-value at 3rd and 7th and 14th post-extraction day are p = 0.025, p = 0.039, and p = 0.00 respectively (Table 2).
Fig. 2.
(A) Soft tissue healing at extraction socket with the platelet-rich fibrin application. (B) Soft tissue healing at extraction socket without platelet-rich fibrin at day 3, day 7 and day 14 respectively.
Table 2.
Comparison of Soft Tissue Healing between cases & controls at 3rd, 7th, 14th postextraction day.
| groups | N | Mean | Std. Deviation | Std. Error Mean | Median | Mann Whitney U value | p value | |
|---|---|---|---|---|---|---|---|---|
| STH 3D | Case | 30 | 3.43 | .504 | .092 | 3 | 330.0 | 0.025* |
| Control | 30 | 3.17 | .379 | .069 | 3 | |||
| STH 7D | Case | 30 | 3.93 | .254 | .046 | 4 | 360.0 | 0.039* |
| Control | 30 | 3.73 | .450 | .082 | 4 | |||
| STH 14D | Case | 30 | 4.83 | .379 | .069 | 5 | 210.0 | 0.000** |
| Control | 30 | 4.30 | .466 | .085 | 4 |
* = statistically significant difference (p < 0.05).
** = statistically highly significant difference (p < 0.01).
3.2. Bone regeneration
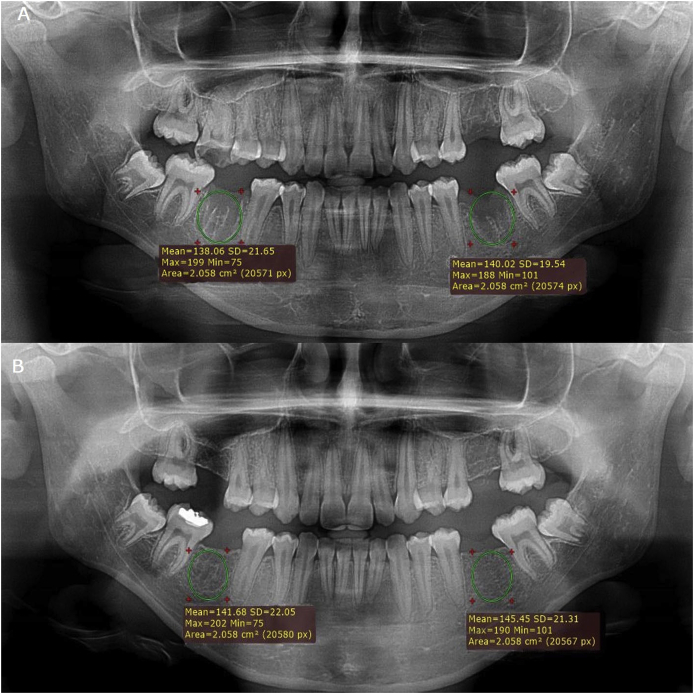
The difference between the increase in grayscale value was compared on the case and control side. The mean grayscale value was 87.816 in the case group and it was 85.378 in the control group immediately after extraction. After the 16th week mean grayscale value was 91.980 in the case group and it was 88.689 in the control group (Fig. 3A and B). There was no statistically significant difference in grayscale value (p-value > 0.05) but the radiological evidence of a rise in bone density between two groups at follow up periods was remarkable (Table 3).
Fig. 3.
(A) Comparison of Gray scale value immediate post extraction. (B) Comparison of Gray scale value 16th week post extraction. (right side with PRF left side without PRF).
Table 3.
Comparison of Gray Scale Value between cases & controls at immediate postextraction and 16th week post extraction.
| groups | N | Mean | Std. Deviation | Std. Error Mean | Median | Mann Whitney U value | p value | |
|---|---|---|---|---|---|---|---|---|
| GSV IMMED | Case | 30 | 87.816 | 33.318 | 6.083 | 98.8 | 424.5 | 0.706 |
| Control | 30 | 85.378 | 28.211 | 5.150 | 91.6 | |||
| GSV 16W | Case | 30 | 91.980 | 33.7728 | 6.166 | 101.75 | 421.0 | 0.668 |
| Control | 30 | 88.689 | 28.5847 | 5.218 | 93.97 |
4. Discussion
Uncomplicated and accelerated healing of wounds always remains the prime concern of clinicians, for this inclusion of growth factors in the local environment is a well-known hypothesis. PRF being a rich source of growth factors is a potential biomaterial for enhancing wound healing and bone regeneration. The results of the present prospective split-mouth clinical trial study showed significant changes in soft-tissue contours with accelerated healing clinically in the case group between post-extraction day 3 to day 7 as compared to the control group. Values indicating bone regeneration at the end of the 16th week were higher on the case side as compared to the control side. Hence the results obtained justify the rationale of the use of PRF as sole graft material and support the positive influence of PRF in enhancing soft tissue healing and bone regeneration.
PRF consists of an intricate collection of cytokines, chemokines and structural glycoproteins entangled inside a gradually polymerized fibrin network including platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), transforming growth factor-1 (TGF-β1), bone morphogenetic protein-1 (BMP-1), coagulation factors, adhesion molecules and several other angiogenic factors that stimulate the activation and growth of the cells promoting wound healing and bone regeneration. These biochemical elements are released into the local micro-environment enabling faster angiogenesis and better remodeling of fibrin network into a more durable connective tissue that contributes to improved healing of soft tissue wounds.14 Platelets and leucocytes upon activation releases cytokines that have the potential to stimulate the bone cells thereby contributing to the regeneration of mineralized tissue. Besides, macrophages in PRF have also been found to stimulate bone formation.15
In the present study soft tissue healing was evaluated clinically using the modified healing index at 60 surgical sites from post-extraction day 3, day 7 and day 14. The magnitude of healing of soft tissue was higher on the experimental side on day 3, (p = 0.025) and day 7 (p = 0.039) as evident with the results. These results were consistent as reported by Gaetano M et al.16 to assess the influence of platelet-rich fibrin on soft tissue healing using the modified healing index after extractions of 108 teeth in 26 patients. At day 14 also it was evident that the magnitude of healing was greater on the experimental side with the mean value of healing index higher (4.83 ± 0.379) than the control side having a mean value of (4.30 ± 0.085) that is statistically significant with p-value (p = 0.000). Similar results of soft tissue healing were observed by Srinivas et al.,17 where significantly higher proportion of individuals in PRF group had better healing index when compared to without PRF group (P < 0.001) after extraction of 60 teeth from both maxilla and mandible in 30 patients.
The assessment of bone regeneration radiographically is a relative process that depends upon the radiographic modality used for assessment. Computed tomography is the most stable and repeatable tool for measuring bone regeneration, but it is complex and has a greater radiation exposure and also generates fairly large costs with regular follow-up. Due to the simplicity of access, low radiation exposure, and wide approval by patients and clinicians Digital Panoramic Radiography is the most commonly utilized method for the examination of hard tissues. In a Panoramic Radiograph the measurement of radiodensity of the region of interest on both case and control side is more feasible and can be done concomitantly in contrast to Intraoral periapical radiograph (IOPA) where multiple radiographs need to be taken for comparison of two sides. Multiple studies have demonstrated the utility of Panoramic Radiograph in bone regeneration in intra-bony defects using mean grayscale value. Mohammadzadeh et al.18 in an in-vitro study investigated the correlation between mean grayscale value in Digital Radiographs and bone density in Hounsfield units in CT-Scan in the jaw bones and found a positive correlation between HU and average gray scale value. According to their findings bone density of the mandible can be approximately estimated through the average gray levels of digital radiographs especially in the edentulous regions where there is no other recognizable opaque structure except the cancellous bone. This justified the possibility to estimate Hounsfield unit and bone density in the jaw bones using mean grayscale in a digital radiograph.
Kotze M et al.19 in an animal study evaluated the role of grayscale value in alveolar bone regeneration and concluded that a standardized radiological examination method, together with a computerized evaluation technique, could be applied to accurately determine relative bone density. Liang Gu and co-workers20 in a human study compared the bone quality before implant placement in the mandible and reported a linear correlation between the mean optical densities of Panoramic Radiograph and CT with significant results.
Chiapasco et al.21 evaluated bone healing in 27 patients having a large intra-bony defect using mean grayscale values on Panoramic Radiographs. Similarly, Zhao et al.22 investigated bone formation after the enucleation of mandibular odontogenic keratocysts by computed densitometry of Panoramic Radiographs in 58 patients using mean grayscale values.
In the present study, the rise in grayscale value was higher on the case side after 16 weeks with the mean rise of grayscale value (4.214 ± 5.1) while the mean rise in grayscale value on the control side was lesser (3.298 ± 4.09) than the case side indicating accelerated bone regeneration on the case side. Rao et al.23 also recorded higher mean value in cases compared to controls at all the time intervals viz., immediate post-op, 1-month post-op, 3 months post-op and 6 months post-op. However, the difference in the mean value recorded between the two groups was not statistically significant (p > 0.05). In the present study also the mean gray scale value was higher on the experimental side after 4-months post extraction but a statistically non-significant (p > 0.05) difference was seen with the intergroup comparison of increase in gray scale value after 4 months.
Baslarli et al.24 conducted a split-mouth study to radio-graphically evaluate the osteoblastic activity of PRF in the extraction socket of third molar using bone scintigraphy, Panoramic Radiograph was used to evaluate grayscale value as a supportive method. They reported no significant differences between PRF-treated extraction sockets and non-PRF-treated extraction sockets postoperatively after 4 weeks and 12 weeks in both methods.
Castillo GF et al.25 assessed the effectiveness of PRF in bone healing after surgical extraction of mandibular third molar using the same radiographic method as in the present study and reported a significant rise in bone density after 8 weeks in case group with p values < 0.015.
It has been hypothesized that socket healing with accelerated bone regeneration can be achieved using PRF. However, there are uncertainties in the literature as to the possible advantages of PRF for bone regeneration. Although some scholars have recorded substantial evidence of the effects of PRF in bone regeneration of extraction socket, others have not found many benefits. This difference in bone tissue regeneration among various studies previously done could be due to the varied technique of preparation of PRF or due to the duration of time taken in the assessment of bone tissue healing or could be the radiographic method used for evaluation of bone regeneration.
Nonetheless, most studies have an agreement that PRF has a beneficial influence on soft tissue healing and bone regeneration, thus can be used as a sole grafting material because it is easy to obtain and devoid of risk that is associated with other graft materials. However, limited human histological data of influence of PRF on soft tissue healing and bone regeneration is available therefore; it demands more investigation in the form of randomized clinical trials on a greater number of patients as the split-mouth design has a potential disadvantage of carry-across effects.
5. Conclusion
Socket grafting with PRF seems to be an accepted minimally invasive technique with simple preparation, cost-effective, low risks, and satisfactory clinical results. Thus obviates the use of more complex socket intervention therapies for alveolar bone preservation and allows early prosthetic rehabilitation especially with dental implants. The results obtained with in the limitations of present study indicated a significant acceleration of soft tissue healing and an appreciable amount of bone regeneration on the case side at the end of 16 weeks, however, it failed to demonstrate very impressive results in terms of bone regeneration to declare it as an ideal grafting material. To further validate the impact of PRF alone on bone regeneration, more research work with a larger sample size is needed.
Financial support
None.
Declaration of competing interest
The authors declare no conflict of interest regarding the publication of this article.
Acknowledgment
NIL.
Contributor Information
Ankit Sharma, Email: drankitsharma2015@gmail.com, drankitsharma2020@gmail.com.
Snehal Ingole, Email: ingole.snehal@rediffmail.com.
Mohan Deshpande, Email: mohandevidas@gmail.com.
Pallavi Ranadive, Email: drpallaviranadive@gmail.com.
Sneha Sharma, Email: sneharajsharma@gmail.com.
Noaman Kazi, Email: dr.noaman.kazi@gmail.com.
Suday Rajurkar, Email: suday.rajurkar@gmail.com.
References
- 1.Gonda T., MacEntee M.I., Kiyak H.A., Persson G.R., Persson R.E., Wyatt C. Predictors of multiple tooth loss among socioculturally diverse elderly subjects. Int J Prosthod. 2013 Mar 1;(2):26. doi: 10.11607/ijp.2893. [DOI] [PubMed] [Google Scholar]
- 2.Buchwald S., Kocher T., Biffar R., Harb A., Holtfreter B., Meisel P. Tooth loss and periodontitis by socio‐economic status and inflammation in a longitudinal population‐based study. J Clin Periodontol. 2013 Mar;40(3):203–211. doi: 10.1111/jcpe.12056. [DOI] [PubMed] [Google Scholar]
- 3.Morjaria K.R., Wilson R., Palmer R.M. Bone healing after tooth extraction with or without an intervention: a systematic review of randomized controlled trials. Clin Implant Dent Relat Res. 2014 Feb;16(1):1–20. doi: 10.1111/j.1708-8208.2012.00450.x. [DOI] [PubMed] [Google Scholar]
- 4.Dohan D.M., Choukroun J., Diss A. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(3):e37–44. doi: 10.1016/j.tripleo.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Dohan D.M., Choukroun J., Diss A. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 march 1;101(3):e45–50. doi: 10.1016/j.tripleo.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Castro A.B., Meschi N., Temmerman A. Regenerative potential of leucocyte‐and platelet‐rich fibrin. Part B: sinus floor elevation, alveolar ridge preservation and implant therapy. A systematic review. J Clin Periodontol. 2017;44(2) doi: 10.1111/jcpe.12658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck T.M., Mealey B.L. Histologic analysis of healing after tooth extraction with ridge preservation using mineralized human bone allograft. J Periodontol. 2010 Dec;81(12):1765–1772. doi: 10.1902/jop.2010.100286. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Y., Ruan Z., Shen M. Clinical effect of platelet-rich fibrin on the preservation of the alveolar ridge following tooth extraction. Exper Therapeutic Med. 2018 Mar 1;15(3):2277–2286. doi: 10.3892/etm.2018.5696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pietrokovski J., Massler M. Alveolar ridge resorption following tooth extraction. J Prosthet Dent. 1967 Jan 1;17(1):21–27. doi: 10.1016/0022-3913(67)90046-7. [DOI] [PubMed] [Google Scholar]
- 10.Urbaniak G.C., Plous S. Research randomizer. 2013. http://www.randomizer.org/ (Version 4.0) [Computer software]. Retrieved on June 22, 2013, from.
- 11.Dohan D.M., Choukroun J., Diss A. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Mar 1;101(3):e45–e50. doi: 10.1016/j.tripleo.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Landry R., Turnbull R., Howley T. Effectiveness of benzydamine HCl in the treatment of periodontal post-surgical patients. Res Clin Forums. 1988;10:105–118. [Google Scholar]
- 13.Frankiewicz M. RadiAnt DICOM VIEWER. 2016. http://www.radiantviewer.com/dicom-viewer-manual/ [Online] [cited 2015 September].Available from:
- 14.Choukroun J., Diss A., Simonpieri A. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. OOOOE. 2006 Mar 31;101(3):e56–60. doi: 10.1016/j.tripleo.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 15.Liu Y., Sun X., Yu J. Platelet-rich fibrin as a bone graft material in oral and maxillofacial bone regeneration: classification and summary for better application. BioMed Res Int. 2019;2019 doi: 10.1155/2019/3295756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marenzi G., Riccitiello F., Tia M., di Lauro A., Sammartino G. Influence of leukocyte-and platelet-rich fibrin (L-PRF) in the healing of simple postextraction sockets: a split-mouth study. BioMed Res Int. 2015 Jul 26:2015. doi: 10.1155/2015/369273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Srinivas B., Das P., Rana M.M., Qureshi A.Q., Vaidya K.C., Raziuddin S.J. Wound healing and bone regeneration in postextraction sockets with and without platelet-rich fibrin. Ann Maxillofacial Surg. 2018 Jan;8(1):28. doi: 10.4103/ams.ams_153_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohammadzadeh S., Khojastepour L., Jazayeri M., Omidi M. In vitro evaluation of the relationship between gray scales in digital intraoral radiographs and hounsfield units in CT scans. J South Afr Dent J Biomed Phys Eng. 2017;7(3) [PMC free article] [PubMed] [Google Scholar]
- 19.Kotze M.J., Kotze H.F., Butow K.W. A radiological method to evaluate alveolar bone regeneration in the Chacma baboon (Papio ursinus) South Afr Dent J. 2012 Jun 1;67(5):210–214. [PubMed] [Google Scholar]
- 20.Liang G.U., Li-ying Y.U., Yi Z.H., Chun X.I. Application of the bone quality of pre-implanted mandible through optical density measurement. Shanghai J Stomatol. 2008;17(5):479–482. [PubMed] [Google Scholar]
- 21.Chiapasco M., Rossi A., Motta J.J., Crescentini M. Spontaneous bone regeneration after enucleation of large mandibular cysts: a radiographic computed analysis of 27 consecutive cases. J Oral Maxillofac Surg. 2000 Sep 1;58(9):942–948. doi: 10.1053/joms.2000.8732. [DOI] [PubMed] [Google Scholar]
- 22.Zhao Y., Liu B., Wang S.P., Wang Y.N. Computed densitometry of panoramic radiographs in evaluation of bone healing after enucleation of mandibular odontogenic keratocysts. Chin J Dent Res. 2010;13(2):123. [PubMed] [Google Scholar]
- 23.Rao S.G., Bhat P., Nagesh K.S. Bone regeneration in extraction sockets with autologous platelet rich fibrin gel. J Maxillofacial Oral Surg. 2013 Mar 1;12(1):11–16. doi: 10.1007/s12663-012-0370-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baslarli O., Tumer C., Ugur O., Vatankulu B. Evaluation of osteoblastic activity in extraction sockets treated with platelet-rich fibrin. Med Oral, Patol Oral Cirugía Bucal. 2015 Jan;20(1):e111. doi: 10.4317/medoral.19999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Castillo G.F., Miranda M.E., Bojorque J.A., Barragán K.I., García D.V. Gingival and bone tissue healing in lower third molar surgeries. Comparative study between use of platelet rich fibrin versus physiological healing. Rev Odontol Mex. 2017;21(2):e1. [Google Scholar]