Abstract
Background
The painful conditions of the Upper quarter region (UQR) such as chronic Craniofacial Pain (CFP) and Cervicobrachial Pain (CBP) usually occur with a plethora of symptoms. Although biological and psychosocial factors are attributed to such conditions, the involvement of the Deep Cervical Fascia (DCF) is ambiguous and needs further exploration.
Objective
We reported a case of CFP and CBP with an intent to showcase the possible involvement of impaired DCF in such presentations and to explore the short-term effect of Fascia directed approach (Fascial Manipulation).
Methods
This is a report of a 25-year-old female college student with chronic head, temporomandibular, neck, and arm pain over the past four years with acute pain exacerbation. After identifying the densified Centre of Coordination points along the myofascial continuum of the DCF, Fascial Manipulation (FM) was performed by deep manual friction. The patient-reported outcomes such as the Numerical Pain Rating Scale (NPRS), Temporomandibular disability index (TMDI), and Patient-Specific Functional Scale (PSFS) were assessed.
Results
Following FM treatment, there is a reduction in pain and improved function between the baseline and follow up evaluation after one week based on all the outcomes (NPRS, PSFS, and TMDI).
Conclusion
This case report highlights the possible role of dysfunction of the DCF and the importance of assessing myofascial chains in patients with pain in the UQR. The report has also shown that FM may be beneficial and can be considered an adjunct in the rehabilitation of chronic CFP and CBP. Nevertheless, future studies with multiple sessions and follow-ups are imperative.
Keywords: Anatomy, Clinical research, Evidence-based medicine, Eye-ear-nose-throat, Health sciences, Musculoskeletal system, Ophthalmology, Respiratory system, Cervical pain, Connective tissue, Facial pain, Headache, Myofascial pain, Orofacial pain
Anatomy; Clinical research; Evidence-based medicine; Eye-ear-nose-throat; Health sciences; Musculoskeletal system; Ophthalmology; Respiratory system; Cervical pain; Connective tissue; Facial pain; Headache; Myofascial pain; Orofacial pain.
1. Introduction
Craniofacial pain (CFP) is the complex, painful condition of the head, face, and related structures with multiple etiologies and treatment strategies. It is difficult to ascertain the source of CFP as the pain-sensitive structures in the head and neck are interconnected. Secondary headaches such as cervicogenic headache disorders (CHD) may contribute to CFP. Chronic neck pain patients usually complain of associated pain in the temporomandibular and the craniofacial regions. A cluster of such symptoms classified as Cervico-Craniofacial Pain (CCFP) poses a significant health problem, as they are the chief sources of discomfort interfering with daily activities [1]. Cervicobrachial pain (CBP) syndrome is defined as “the presence of neck pain associated with tingling, numbness, or discomfort in the arm with or without associated headache” [2]. As the nervous system is a continuous structure, the usual source of neck and arm symptoms is considered to be of neural origin. But Gangavelli et al. have reported that only 20% of CBP cases are of neurogenic origin [3]. Butler has highlighted that a positive Upper limb neural tension (ULNT) test does not necessarily indicate the adverse mechanical disorder of the nervous system [4]. A multitude of problems unrelated to “neural tension” may create a painful response in patients with positive ULNT test. Furthermore, these painful conditions usually remain undiagnosed because of the complexities involved in the diagnosis and management [5].
The non-neural source of chronic CCFP could be due to the involvement of Deep Fascia (DF), which links the upper quarter region (UQR). Thus, the DF forms the myofascial continuum (MC), which may provide pathways for myofascial force transmission [6, 7]. Stecco et al. have demonstrated the existence of anterior myofascial expansions where the deep fascia connects the different muscles of the volar aspect of the upper quarter, thus forming the MC [8].
Impairment of the Deep Cervical Fascia (DCF) may lead to Musculoskeletal pain (MP) and dysfunctions of the UQR. It has recently been purported that the innervation of the fascia with its potential nociceptive function may be considered a possible mechanism in MP [9]. The extent of involvement of DCF and its proximal and distal continuum in chronic CFP and CBP, were not explored. This case report intended to add literature by describing the anatomical continuity of the DCF and its possible role in chronic painful conditions of the upper quarter region. In addition, this case report reported the influence of Fascial Manipulation (FM) on the anatomical myofascial continuum of the DCF in a patient with CCFP.
1.1. Concomitant occurrence of headache and neck pain
1.1.1. Myofascial continuum of Deep Cervical Fascia
The anatomical continuity of the DCF or Fascia colli is an intricate network of connections. The DCF has three laminae, including the superficial layer (investing layer), a middle layer (pretracheal Fascia), and a deep layer (prevertebral Fascia). The investing layer or superficial lamina envelopes the neck like a collar. It splits and encloses the muscles like sternocleidomastoid, trapezius, as well as the parotid and submandibular glands [10]. The superficial lamina of the DCF continues proximally as the parotideomassetric Fascia and temporal Fascia. This proximal continuity of the superficial lamina of the DCF envelopes the masseter and temporalis muscles. The dysfunction of this proximal continuum could be a contributing factor for temporomandibular pain and headache. Distally, DCF continues down as the pectoral fascia and latissimus epimysial fascia, thus enveloping pectoralis major and latissimus dorsi muscles [11]. Laterally, it continues down as the brachial fascia surrounding the arm, which could contribute to symptoms in the brachium and elbow, and then the ante-brachial fascia enclosing the forearm as shown in Figure 1 [12].
Figure 1.
Myofascial continuum of the upper quarter (© Antony Cruz and Prabu Raja) [6, 10, 11].
The craniofacial and cervicobrachial is usually associated with local and referred pain (RP) proximal and distal to the neck, respectively. Even though the RP pattern may mimic nerve entrapment syndromes and radiculopathy, any dysfunctions of the DCF and its continuum may result in RP, which can be considered the myofascial pain syndrome of the upper quarter region [13].
1.1.2. Myodural Bridge
The Myodural Bridge (MDB) is the connective tissue present in the epidural space of the cervical region. The MDB connects the suboccipital muscle fascia and dura, thus considered as an essential structure in monitoring the dural tension [14]. The dysfunction of the MDB is also found to be associated with the aetiology of Cervicocephalic pain syndromes [14, 15].
1.1.3. Trigeminal-cervical complex
The neural link between the neck and head is due to the Trigemino-cervical complex (TCC), where the trigeminal and the cervical inputs converge. TCC is located in the dorsal horn of the upper cervical spinal segments. The concomitant occurrence of neck pain with the craniofacial and orofacial pain is due to the interchange of nociceptive information, resulting in Cervico - Craniofacial pain (CCFP) [16].
1.2. Fascia directed treatment approaches
Most of the studies emphasize on the anatomy and pathology of specific structures such as thoracolumbar Fascia, plantar fascia, and the iliotibial tract. Although the attention towards Fascia directed treatment (FDT) approaches have been increasing in manual therapy, many FDT approaches do not consider the human fascial system as an interconnected structure [7]. They do not provide specific treatment indications. Fascial Manipulation (FM) provides a biomechanical model for the human fascial system as fibrous connective tissues, which may have a reciprocal influence throughout the body. Thus, FM emphasizes the musculoskeletal system's global treatment approach, using movement and palpation verification. Besides, FM is supported by Cadaveric, Histological and Biomechanical studies concerning the architecture, innervation, and the potential mechanism of action, thus justifying the use of the FM approach in this patient [7, 8].
1.2.1. Stecco's biomechanical model
The Stecco biomechanical model (SBM) describes the fascial system as a three-dimensional continuum. Based on this model, the upper quarter is classified into the following segments: Caput, Collum, Scapula, Humerus, Cubitus, Carpus, and Digiti [8]. Each segment of the upper quarter includes six myofascial units (MFU). The MFU is considered as the structural and functional unit of the locomotor system and co-ordinates the movements at each joint. Each MFU comprises several motor units, muscles, fascia, and the corresponding joint. The dysfunctions of these MFU occur due to the failure of the DF to elongate and accommodate to the tension imparted by the underlying muscle fibers. The movements are described as Antemotion (AN) and Retromotion (RE) in the sagittal plane, Lateromotion (LA) and Mediomotion (ME) in the frontal plane, Intrarotation (IR) and Extrarotation (ER) in the horizontal plane. Within each MFU, there are specific points in the DF, termed as the Centre of coordination (CC), which is the convergent point of the muscle force vectors that act on a body segment during a specific movement. The MFU of the different body segments unites to form the Myofascial sequences (MS), which monitor the uniplanar movement of several segments in the same plane.
Densification of the CCs may lead to impairment in the gliding of fascial layers resulting in abnormal tension within a segment. By performing movement and palpation verifications of specific CC points over the MS, dysfunctional CC points can be identified [8, 17]. The CC points with excessive densification and less pain threshold will be determined by palpation over the respective agonist and antagonistic MS. Following that, the densified CCs relevant to the patient's movement dysfunction were identified for manipulation.
FM is considered to restore the restricted movement of collagen and elastin fibers within the ground substance through heat generated from manipulation of the densified CC points [18]. The manual friction (tangential oscillation) might modulate the state of hyaluronan from gel to fluid, thereby improving the fascial mobility and thus reducing pain [19, 20].
2. Case description
A 25-year-old, left-sided dominant recreational female tennis player, presented with complaints of acute exacerbation of pain on the left side of the head, neck, jaw, and arm without any sensory abnormalities. There was no history of trauma. She complains of restricted functional activities. She had similar episodes of symptoms intermittently over the past four years without any involvement or pertinent lesions of the somatosensory nervous system. In the past, these symptoms were relieved with medications (NSAIDs and analgesics). The pain history reveals a dull aching type of pain, which is insidious in onset. The pain was aggravated by prolonged sitting activities like reading, watching television, and using laptops. The pain distribution pattern did not correlate with the innervation of the peripheral nerve/root or somatotophic representation of the Upper quarter region (UQR).
None of the information that reveals the patient's identity was disclosed. The participant had given her consent for a thorough evaluation and publication of the report as well.
2.1. Initial clinical examination
After obtaining the patient's written informed consent, the therapist began with the evaluation.
On observation:
The patient's sagittal postural analysis revealed rounded shoulders, exaggerated thoracic kyphosis, and poked chin posture.
On Palpation:
Tenderness was graded by palpation using the tenderness-rating scale were grade I indicates minimal tenderness, and grade IV indicates severe tenderness [21]. The tenderness grades for the patient on the left side were as follows. Masseter (III), Temporalis (IV), Suboccipital muscles (III), Upper trapezius (IV), Sternocleidomastoid (II), Pectoralis minor (II), Deltoid (III) and Adductor pollicis (III). Tenderness was also present on the medial aspect of the scapula (III) and over the lateral epicondyle (IV) region.
On Examination:
Shoulder range of motion (ROM) was full, but she presented with painful end ranges on all movements. Cervical right lateral flexion, right rotation, and extension was restricted at the end range because of pain and stiffness on the left side of the neck. There was a slight deviation to the right on the initiation of the mouth opening.
- Differential diagnosis:
-
1)Referred pain patterns of head, neck, and arm with the presence of tender spots in the upper quarter region.
-
2)Pressure on the tender points reproduced the chief pain complaint.
-
3)Restriction in the cervical ROM.
-
4)Negative ULNT tests
-
1)
Considering the review of the grading system for neuropathic pain by Finner et al., the chronic pain in this patient can be regarded as nociceptive and not as neurogenic based on the following evaluation. There was no history of relevant neurological lesions as well as non-painful sensory symptoms. Also, the onset of pain is insidious, and pain pattern is different from peripheral nerve distribution. There were neither sensory nor motor deficits in the UQR and is based on the diagnostic principles of the International Association for the study of pain [22]. The evaluation showed that the source of pain might not be neurogenic. Thus, based on the subjective and objective evaluation, the subject was considered to have myofascial pain disorder of the upper quarter.
2.1.1. Myofascial evaluation based on Stecco's FM method
The site of pain is along the Lateral (LA) myofascial sequence. The patient complains of an increase in pain during the sideways movement of the left arm and neck suggestive of the involvement of Lateral-Humerus (LA-HU) and Lateral-Collum (LA-CL). Following this, movement and palpation verifications were performed.
2.1.1.1. Movement assessment
During the active movement assessment, the patient was asked to move the painful Humerus and Collum segments in all three planes. Frontal plane movements such as the abduction of the shoulder and lateral flexion of the neck were painful compared to the other planes of movements suggestive of the involvement of Lateral-Humerus (LA-HU) and Lateral-Collum (LA-CL). The movement examination is indicative of the involvement of the lateral myofascial sequences of the upper quarter.
2.1.1.2. Palpation assessment
Palpation of the CC points along the six-myofascial sequences was done, and the most painful and densified CC points were identified.
Based on the pain history, movement, and palpation verifications, the CC points on the Lateral and Medial myofascial sequences were identified to be involved. The CC points with the maximum pain and densification following palpation verification include the following.1) CC points on the Latero myofascial sequences - Latero-Caput 2 (LA-CP 2), Latero-Caput 3 (LA-CP 3), Latero-Collum (LA-CL), Latero-Humerus (LA-HU) and 2) CC points on the Medio myofascial sequences - Medio-Caput 3 (ME-CP 3), Medio-Collum (ME-CL), Medio-Scapula (ME-SC), Medio-Cubitus (ME-CU). The CC points for the Latero and Mediomotion sequences are as shown in Tables 1 and 2 [8].
Table 1.
Centers of Coordination points for Latero-motion MS of the UQR [8].
| CC points | Location |
|---|---|
| LA-CP 1 | Over the lateral angle of the eye aiming at the Lateral rectus muscle of the eye |
| LA-CP 2 | Centre of Temporalis muscle and their Temporal Fascia |
| LA-CP 3 | Centre of Masseter muscle and their Masseteric Fascia |
| LA-CL | The lateral border of Sternocleidomastoid muscle at the level of the thyroid cartilage |
| LA-SC | Over Scalenus medius between the Upper Trapezius and the Sternocleidomastoid |
| LA-HU | Over the deltoid muscle, in front of the greater tubercle where supraspinatus inserts |
| LA-CU | Over the Brachioradialis muscle, at the radial head and in the groove between Brachioradialis and Extensor carpi radialis longus. |
| LA-CA | Between the muscle bellies of the Extensor carpi radialis longus and brevis |
| LA-DI | Over the first Dorsal interosseous |
Adapted from: Stecco L, 2004.
CC-Centre of Coordination, LA –Lateromotion, CP 1- Caput 1, CP 2- Caput 2, CP 3- Caput 3, CL- Collum, SC- Scapula, HU-Humerus, CU-Cubitus, CA-Carpus, DI-Digitii [8].
Table 2.
Center of coordination points for Medio-motion MS of the UQR [8].
| CC points | Location |
|---|---|
| ME-CP 1 | Over the medial angle of the eye aiming at the Medial rectus muscle of the eye |
| ME-CP 2 | Raphe of the mylohyoid muscle under the chin |
| ME-CP 3 | Occipital insertion of the ligamentum nuchae below the occipital prominence |
| ME-CL | Anteriorly over the median raphe of the anterior cervical Fascia at the suprasternal notch/Posteriorly over the Ligamentum nuchae |
| ME-SC | Over the Serratus anterior, in the 6th intercostal space along the midline of the axilla |
| ME-HU | Behind Coracobrachialis on the lateral wall of the axillary cavity |
| ME-CU | Over the medial intermuscular septum where Flexor carpi ulnaris gets attached |
| ME-CA | Over flexor carpi ulnaris |
| ME-DI | Over the palmaris brevis muscle and flexor digiti minimi |
Adapted from: Stecco L, 2004.
CC-Centre of Coordination, ME- Mediomotion, SC- Scapula, HU-Humerus, CU-Cubitus, CP 1- Caput 1, CP 2- Caput 2, CP 3- Caput 3, CL- Collum, CA-Carpus, DI-Digitii [8].
2.2. Outcome measures
2.2.1. Numeric pain rating scale
The Numeric Pain Rating Scale (NPRS) is commonly used for neck pain patients. The Minimal clinically important difference (MCID) is 2 points after investigating in different groups of patients with various MP, and dysfunctions [23]. The patient in this report reported a value of seven on the NPRS scale during baseline evaluation.
2.2.2. The Patient-Specific Functional Scale
The Patient-Specific Functional Scale (PSFS) is one of the patients- reported outcome measures that allow the patients to communicate on their level of limitation in function to determine a meaningful change in functional status following interventions. The PSFS requires the patient to list three activities that are difficult to perform because of their symptoms. Each activity rated on 11 point scale, with 0 representing “inability to perform the activity” and 10 representing the “ability to perform the activity at prior level” [24, 25]. The PSFS is reliable, valid and responsive to change for patients with cervical radiculopathy, upper extremity musculoskeletal problems [26]. The patient identified four for writing, six for prolonged sitting and two for chewing as functional limitations, indicating a major functional limitation during baseline evaluation.
2.2.3. The Temporomandibular Disability Index (Steigerwald/Maher)
The Temporomandibular Disability Index (TMDI) consists of ten questions concerning disability associated with TMD, where each item is scored from 0-4. Higher scores represent more significant levels of disability. TMDI score on the first day of the evaluation was 14 [27].
2.3. Tailored treatment program
Based on the movement examination and precise palpation verification of specific CC points defined by the Stecco method, the treatment program was directed towards CC points of the DCF. The involved densified CC points include LA-CP 2, LA-CP 3, LA-CL, LA-HU, ME-CP 3, ME-CL, ME-SC, ME-CU [28, 29, 30]. Manipulation was performed by deep manual friction using elbows or knuckles for 5–8 min at each CC point, as shown in Figure 2. During the treatment session, the patient was asked to stay relaxed and attain the required position of supine, side, or prone lying as per the application of technique [18, 28, 29].
Figure 2.
Application of FM on CC point (LA-CL) [8].
A follow-up session was conducted after seven days following the treatment session. The patient reported a reduction of pain and an improvement in the function. The repeated mechanical stimuli such as an abnormal posture in this patient might have resulted in the modification of the ground substance of the densely innervated CC points.
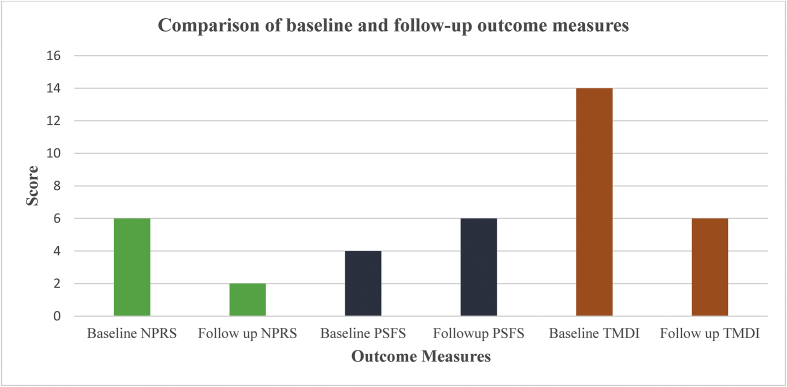
3. Results
The comparison between the baseline and follow-up outcomes measures following FM is shown in Figure 3. The follow-up assessment have shown that the average score of PSFS had improved from four during the first evaluation to six during follow-up, suggesting a moderate change in the functional scores. The patient had reported a reduction in the pain score from six to two in the NPRS. Also, the TMDI score had improved from fourteen to six during the follow-up assessment. These findings suggested that there was a reduction in pain and improvement of functions following a single session of FM.
Figure 3.
Outcome measures before and after FM [26, 27]. NPRS: Numeric Pain Rating Scale, PSFS: Patient-Specific Functional Scale, TMDI: Temporomandibular Disability Index.
4. Discussion
This report shows that the DCF and its continuum could be one of the potential contributors to the development of CFP and CBP. The patient showed a short-term reduction of pain and improvement in function following FM of the DCF and its continuum. The reduced symptoms and improved functions have shown that the patient has responded well to this myofascial treatment approach.
Fascia is described as a three-dimensional continuum by linking the skeletal muscles and the organs of the body. These linkages may help in transmitting tension generated by one muscle group to the other soft tissue structures. Dysfunctional breathing patterns were observed in patients with low back pain and were conjectured to occur due to anatomical link between the diaphragm and the thoracolumbar Fascia [31]. Such fascial connections provide the basic principles for the global treatment of painful conditions of the musculoskeletal system. Pathology of myofascia (densification) is due to the change in the viscosity of hyaluronic acid (HA). The excessive tension generated in the densified Fascia in one area transmits stress along the entire myofascial line leading to the myofascial pain reference pattern [20].
Abnormality in the fascial tissues was considered involved in the etiology of non-specific Chronic Low back pain (NCLBA). A study had reported a significant reduction of pain and improvement in function as well as quality of life when FM was administered within a course of Manual therapy (MT), in patients with NCLBA [32]. Similar to that study, FM performed on the myofascial continuum of the DCF, showed improvement in the patient-reported outcomes such as pain and function in this case study. Another study had reported a reduction in the shear strain of thoracolumbar Fascia in patients with low back pain for more than a year and have attributed it to the altered activation patterns of trunk muscles and/or abnormal connective tissues [33]. Considering the probable involvement of intrinsic pathology of DCF and its continuum in CFP and CBP, FM was provided. By creating a local heat through friction on specific densified points in DCF, FM might have modified the consistency of the ground substances of the deep Fascia. The improved gliding of DCF following FM, might have restored the coordination between the muscle fibers of MFU as well as between the MFU of the respective myofascial lines. In addition, recent research has reported the presence of endocannabinoid receptors in the myofascial tissue, suggesting the plausible role of endocannabinoid system in resolving myofascial pain by the stimulation of deep Fascia [34]. The improvement in the outcomes in this patient, suggested that the source of painful symptoms were addressed, thus adding interest to this area of practice and suggests an avenue for future research. Although the patient appeared to respond well to FM, the probability of a placebo effect cannot be ruled out, suggesting a limitation of this case report. Future studies comparing the effects of different treatment strategies in the management of CCFP are warranted.
Declarations
Author contribution statement
All authors listed have significantly contributed to the investigation, development and writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Garcia D.M., Martinez A.G., Lopez A.L., Villanueva I.L., Touche R.L., Carnero J.F. 2016. Chronic neck pain and cervico-craniofacial pain patients express similar levels of neck pain-related disability, pain catastrophizing and cervical range of motion: pain research and treatment; pp. 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elvey R.L., Hall T. Physical Therapy of the Shoulder. Churchill Livingstone; New York: 1997. Neural tissue evaluation and treatment. [Google Scholar]
- 3.Gangavelli R., Nair N.S., Bhat A.K., Solomon J.M. Cervicobrachial pain - How often is it Neurogenic? J. Clin. Diagn. Res. 2016;10(3):14–16. doi: 10.7860/JCDR/2016/16456.7492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Butler D.S., Gifford L.S. The concept of adverse mechanical tension in the nervous system. Part 1: Testing for ‘dural tension. Physiotherapy. 1989;75:622–629. [Google Scholar]
- 5.Richard P., Fabi D. Neural Mobilization: the impossible. J. Orthop. Sports Phys. Ther. 2001;31(5):224–225. [Google Scholar]
- 6.Purslow P.P. Muscle fascia and force transmission. J. Bodyw. Mov. Ther. 2010;14(4):411–417. doi: 10.1016/j.jbmt.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Schleip R., Findley T., Chaitow L., Huijing P. Churchill Livingstone, Elsevier; 2012. The Tensional Network of the Human Body. [Google Scholar]
- 8.Stecco L. Fascial Manipulation for Musculoskeletal Pain. Piccin; Padova: 2004. Manipulation of the myofascial sequences. Day JA; pp. 149–154. [Google Scholar]
- 9.Robert S., Adjo Z., Werner K. Biomechanical properties of fascial tissues and their role as pain generators. J. Muscoskel. Pain. 2010;18(4):393–395. [Google Scholar]
- 10.Simmathamby C.S. Elsevier; 2011. Head and Neck and Spine. Last's Anatomy- Regional and Applied; pp. 505–512. [Google Scholar]
- 11.Stecco C. Elsevier; 2015. Fasciae of the Head and Neck. Functional Atlas of the Human Fascial System; pp. 130–138. [Google Scholar]
- 12.Paoletti S. Eastland Press; Seattle: 2006. Anatomy of the Fasciae. The Fasciae, Anatomy, Dysfunction and Treatment; pp. 23–28. [Google Scholar]
- 13.Gerwin R.D. Myofascial pain syndromes in the upper extremity. J. Hand Ther. 1997;10(2):130–136. doi: 10.1016/s0894-1130(97)80067-1. [DOI] [PubMed] [Google Scholar]
- 14.Enix D.E., Scali F., Pontell M.E. The Cervical myodural bridge, a review of literature and clinical implications. J. Can. Chiropr. Assoc. 2014;58(2):184–192. [PMC free article] [PubMed] [Google Scholar]
- 15.Tagil S.M., Ozçakar L., Bozkurt M.C. Insight into understanding the anatomical and clinical aspects of supernumerary rectus capitis posterior muscles. Clin. Anat. 2005;18:373–375. doi: 10.1002/ca.20106. [DOI] [PubMed] [Google Scholar]
- 16.Castein R., Hertogh W.D. A neuroscience perspective of physical treatment of headache and neck pain. Front. Neurol. 2019;10:276. doi: 10.3389/fneur.2019.00276. 1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Day J.A., Stecco C., Stecco A. Application of Fascial Manipulation & technique in chronic shoulder pain-Anatomical basis and clinical implications. J. Bodyw. Mov. Ther. 2009;13:128–135. doi: 10.1016/j.jbmt.2008.04.044. [DOI] [PubMed] [Google Scholar]
- 18.Mathew N.P., Raja G.P., Davis F. Effect of fascial manipulation on glenohumeral internal rotation deficit in overhead athletes - a randomized controlled trial. Muscles Ligaments Tendons J. 2020;10(1):17–23. [Google Scholar]
- 19.Stecco A., Gesi M., Stecco C., Stern R. Fascial components of the myofascial pain syndrome. Curr. Pain Headache Rep. 2013 Aug 17;(8):352. doi: 10.1007/s11916-013-0352-9. [DOI] [PubMed] [Google Scholar]
- 20.Stecco C., Stecco A. Deep fascia of the shoulder and arm. In: Schleip R., editor. Fascia: the Tensional Network of the Human Body. Churchill Livingston: Elsevier; 2012. pp. 24–29. [Google Scholar]
- 21.Hubbard D.R., Berkoff G.M. Myofascial trigger points show spontaneous needle EMG activity. Spine (Phila Pa 1976) 1993;18:1803–1807. doi: 10.1097/00007632-199310000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Finnerup N.B., Haroutounian S., Kamerman Neuropathic pain: an updated grading system for research and clinical practice. Pain. 2016;157(8):1599–1606. doi: 10.1097/j.pain.0000000000000492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Young I.A., Duning J., Butts R., Mourad F., Cleland J.A. Reliability, construct validity and responsiveness of the neck disability index and numeric pain rating scale in patients with mechanical neck pain without upper extremity symptoms. Physiother. Theory Pract. 2018;1–8 doi: 10.1080/09593985.2018.1471763. [DOI] [PubMed] [Google Scholar]
- 24.Abbott J.H., Schmitt J. Minimum important differences for the patient-specific functional scale, 4 region-specific outcome measures, and the numeric pain rating scale. J. Orthop. Sports Phys. Ther. 2014;44(8):560–564. doi: 10.2519/jospt.2014.5248. [DOI] [PubMed] [Google Scholar]
- 25.Cheryl H., Abbott J.H., Richard A., Baxter G.D. The patient-specific Functional Scale: validity, Reliability and responsiveness in patients with upper extremity musculoskeletal problems. J. Orthop. Sports Phys. Ther. 2012;42(2):56–65. doi: 10.2519/jospt.2012.3953. [DOI] [PubMed] [Google Scholar]
- 26.Joshua A.C., Julie M.F., Julie M.W., Jessica A.P. The reliability and construct validity of the neck disability index and patient-specific functional scale in patients with cervical radiculopathy. Spine. 2006;32:598–602. doi: 10.1097/01.brs.0000201241.90914.22. [DOI] [PubMed] [Google Scholar]
- 27.Steigerwald D., Maher J. The Steigerwald/Maher TMD disability questionnaire. Today Chiropr. 1997:86–91. [Google Scholar]
- 28.Stecco L., Stecco C. Fascial manipulation. In: Day J.A., editor. Fascial Manipulation (Practical Part) Piccin; Padova: 2008. pp. 19–25. [Google Scholar]
- 29.Stecco L. The myofascial units of the upper limb. In: Day J.A., editor. Fascial Manipulation for Musculoskeletal Pain. Piccin; Padova: 2004. pp. 51–59. [Google Scholar]
- 30.Stecco L. The anatomy of the myofascial unit. In: Day J.A., editor. Fascial Manipulation for Musculoskeletal Pain. Piccin; Padova: 2004. pp. 23–29. [Google Scholar]
- 31.Shah S.G., Choezom T., Raja G.P. Comparison of respiratory parameters in participants with and without chronic low back pain. J. Bodyw. Mov. Ther. 2019;23:894–900. doi: 10.1016/j.jbmt.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 32.Branchini M., Lopopolo F., Andreoli E. Fascial Manipulation® for chronic aspecific low back pain: a single blinded randomized controlled trial. F1000Research. 2016;4:1208. doi: 10.12688/f1000research.6890.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Langevin Reduced thoracolumbar fascia shear strain in human chronic low back pain. BMC Muscoskel. Disord. 2011;12:203. doi: 10.1186/1471-2474-12-203. 1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fede C., Albertin G., Petrelli L., Sfriso M.M., Biz C., Caro R.D., Stecco C. Expression of the endocannabinoid receptors in human fascial tissue. Eur. J. Histochem. 2016;60:2643. doi: 10.4081/ejh.2016.2643. 130-134. [DOI] [PMC free article] [PubMed] [Google Scholar]