Abstract
Background: To date, the benefit of successful revascularization of chronic total occlusions (CTOs) on prognosis remains uncertain, and there is a paucity of data on the impact of successful revascularization for CTO patients on long-term cardiovascular survival. This study aimed to investigate the long-term cardiovascular survival for patients with successful and unsuccessful CTO revascularization in a large cohort of patients.
Methods: There were 1,655 consecutive patients with at least one CTO included and were grouped into successful revascularization (n = 591) and unsuccessful revascularization (n = 1,064). Propensity score matching (PSM) was carried out to balance the clinical and the angiographic characteristics. Cardiac mortality was defined as the primary endpoint. Major adverse cardiac event (MACE) was assessed as a “secondary endpoint.”
Results: After 3.6 years of follow-up, there was no significant difference between the successful and the unsuccessful revascularization groups in the rate of cardiac mortality [adjusted hazard ratio (HR) 0.96, 95% confidence interval (CI) 0.59–1.58, p = 0.865]. After the PSM analysis (371 pairs) between the two groups, the cardiac mortality rate values (HR 0.51, 95% CI 0.23–1.15, p = 0.104) were equivalent, whereas the adjusted risk of MACE (HR 0.43, 95% CI 0.32–0.58, p = 0.001) and target-vessel revascularization (HR 0.41, 95% CI 0.29–0.58, p < 0.001) were significantly higher in patients with unsuccessful revascularization.
Conclusion: For the treatment of CTO patients, successful revascularization was not associated with a lesser risk for cardiac mortality as compared with unsuccessful revascularization. However, successful revascularization reduced MACE and target-vessel revascularization.
Keywords: cardiac mortality, coronary chronic total occlusions, major adverse cardiac event, medical therapy, percutaneous coronary intervention, successful revascularization, outcomes
Introduction
Coronary chronic total occlusion (CTO) revascularization is a challenging obstacle in the field of coronary intervention (1). Several observational studies demonstrated that better outcomes of successful CTO percutaneous coronary intervention (PCI) included angina reduction and improvement in both long-term survival and left ventricular function in comparison with unsuccessful procedures (2–6). However, CTO-PCI is attempted in 10–20.7% patients (7, 8) mainly because CTO-PCI procedures are costly, complex, and associated with higher complication rates as compared to non-CTO interventions (9, 10). Therefore, a large portion of patients with CTOs are treated by coronary artery bypass grafting (CABG) or medical therapy (MT), especially in patients with well-developed collateral circulation or multiple CTOs and multi-vessel coronary disease (11–15). However, the patients who receive MT without a CTO-PCI attempt were rarely considered previously (16, 17). To date, the prognosis of successful revascularization of CTO remains uncertain, and there is limited data on the impact of successful revascularization for CTO patients on long-term cardiovascular survival.
In this study, we sought to investigate the long-term clinical outcomes of CTO patients treated with successful and unsuccessful CTO revascularization in a large cohort of population.
Materials and Methods
Study Population
A total of 1,702 patients with at least one CTO were enrolled at our institution between 2007 and 2016 (18). The exclusion criteria were: (1) prior CABG and (2) acute ST-segment elevation myocardial infarction (MI). After exclusion, a final population of 1,655 patients was left. The subjects were classified into either successful revascularization group or unsuccessful revascularization group based on the initial therapeutic modalities. The patients referred for revascularization had presence of symptomatic angina and/or myocardial viability in the territory of CTO or inducible ischemia, which were reported in our previously published article (18).
Clinical and procedural data and in-hospital outcomes were entered into a dedicated database. Clinical follow-up was performed through examination of hospital records and telephone follow-up or outpatient clinical visit. Our institutional review committee approved the present study in accordance with the Declaration of Helsinki.
Definitions and Clinical Endpoints
A CTO is defined as a coronary obstruction with thrombolysis in myocardial infarction (TIMI) antegrade grade 0 flow for more than 3 months based on previous coronary angiogram or clinical history (2). Patients who have undergone a successful CTO-PCI were implanted with first-generation drug-eluting stent (DES) from January 2006, including sirolimus-eluting and paclitaxel-eluting stents [Excel, Yinyi, Firebird and Firebird2 (China); Cipher and Taxus (USA)]. The angiographic success of CTO-PCI was defined as <20% residual stenosis and TIMI grade ≥2 flow after the implantation of a DES to the CTO vessel. The extent of collateral circulation flow was assessed according to the validated Rentrop classification scale (19). After PCI, all patients received aspirin indefinitely and clopidogrel for at least 12 months. The “primary efficacy endpoint” was cardiac mortality. A major adverse cardiac event (MACE) was assessed as a “secondary endpoint,” consisting of cardiac mortality, MI, or target-vessel revascularization (TVR). Definitions of cardiac mortality, MI, and TVR have been described in a previous article (18). All patients underwent two-dimensional echocardiography.
Statistical Analysis
The data are listed as mean ± standard deviation for continuous variables and as percentages for categorical variables. The variables were compared between groups by using Student's t-test for continuous variables and chi-square or Fisher exact test for discrete variables. Propensity score matching (PSM) analysis was constructed to adjust for any potential confounder between the two groups based on multivariable logistic regression model. Survival—free of adverse events—was calculated by Kaplan–Meier analysis and compared using log-rank test. In multivariable models, the covariates with p < 0.1 on univariate analysis were considered as candidate variables. Cox regression was used to compare adjusted hazard rates based on age, gender, history of MI, chronic kidney disease (CKD), left ventricular ejection fraction (LVEF), taking renin–angiotensin system blockade, left anterior descending coronary artery (LAD) and left circumflex coronary artery (LCX) involvement, multivessel disease, calcification, blunt stump, Japanese-chronic total occlusion (J-CTO) score, and coronary dissection in the total population. In the propensity-matched population, Cox regression was based on blunt stump, bending >45°, J-CTO score, coronary dissection, and perforation. All analyses were carried out with Stata V.15 software (StataCorp, College Station, TX, USA). All tests were conducted at the 0.05 level.
Results
Clinical and Angiographic Characteristics
Among the 1,655 patients, of whom 944 were CTOs, 800 patients were treated with medication and 855 were treated with revascularization. In the successful revascularization group, 470 patients underwent successful CTO-PCI and 121 patients got successful CTO CABG. In the unsuccessful revascularization group, 800 patients received MT and 264 patients had a failed PCI. Five CTO-dedicated operators performed the procedures during the study period. A total of 36 patients underwent reattempted CTO-PCI after the prior failed CTO-PCI, and 24 patients got a successful reattempt. The success rate of reattempted CTO-PCI was 66.7%.
Table 1 shows the baseline clinical characteristics of CTO patients between each therapeutic group. As compared to patients who had MT, the patients who had CABG were younger and more often had a familial history of coronary artery disease (CAD). Compared with patients who underwent PCI, the patients who underwent CABG were younger and more frequently had a familial history of CAD and low LVEF. Compared with patients who had MT, those who had PCI were younger and had mostly previously undergone PCI, whereas they less often have a history of MI, with high total cholesterol, high-density lipoprotein cholesterol, and LVEF, but with low low-density lipoprotein cholesterol.
Table 1.
Baseline clinical characteristics in CTO patients of each therapeutic group.
| Variable | MT (A) | PCI (B) | CABG (C) | P-value | |||
|---|---|---|---|---|---|---|---|
| (n = 800) | (n = 734) | (n = 121) | Overall | B vs. A | C vs. A | C vs. B | |
| Age, years | 64.8 ± 10.7 | 63.2 ± 9.7 | 63.0 ± 9.4 | 0.001 | <0.001 | 0.046 | 0.995 |
| Male, % | 623 (77.9) | 572 (77.9) | 97 (80.2) | 0.845 | 0.980 | 0.570 | 0.581 |
| Smoking, % | 326 (40.8) | 309 (42.1) | 48 (39.7) | 0.809 | 0.592 | 0.822 | 0.616 |
| Hypertension, % | 548 (68.5) | 482 (65.7) | 75 (62.0) | 0.480 | 0.255 | 0.153 | 0.431 |
| Diabetes mellitus, % | 290 (36.3) | 252 (34.3) | 50 (41.3) | 0.350 | 0.307 | 0.281 | 0.136 |
| Dyslipidemia, % | 577 (72.1) | 536 (73.0) | 97 (80.2) | 0.263 | 0.388 | 0.104 | 0.235 |
| TC, (m mol/L) | 4.64 ± 1.28 | 4.50 ± 1.34 | 4.61 ± 1.30 | 0.029 | 0.009 | 0.672 | 0.320 |
| TG, (m mol/L) | 1.6 (1.1–2.4) | 1.5 (1.1–2.4) | 1.7 (1.2–2.3) | 0.632 | 0.856 | 0.363 | 0.309 |
| HDL-C, (m mol/L) | 1.24 ± 0.38 | 1.29 ± 0.69 | 1.19 ± 0.33 | <0.001 | 0.049 | 0.095 | 0.046 |
| LDL-C, (m mol/L) | 2.77 ± 0.87 | 2.58 ± 0.94 | 2.75 ± 0.92 | <0.001 | <0.001 | 0.944 | 0.175 |
| Familial history of CAD, % | 93 (11.6) | 96 (14.1) | 28 (23.1) | 0.002 | 0.387 | <0.001 | 0.004 |
| Previous MI, % | 406 (50.8) | 320 (43.6) | 58 (47.9) | 0.020 | 0.005 | 0.564 | 0.373 |
| Previous PCI, % | 78 (9.8) | 105 (14.3) | 14 (11.6) | 0.023 | 0.006 | 0.534 | 0.421 |
| CKD, % | 83 (10.3) | 51 (6.9) | 8 (6.6) | 0.041 | 0.018 | 0.196 | 0.892 |
| LVEF, % | 51.7 ± 9.6 | 54.1 ± 8.1 | 51.7 ± 9.6 | <0.001 | <0.001 | 0.856 | 0.009 |
CABG, coronary artery bypass grafting; CAD, coronary artery disease; CKD, chronic kidney disease; CTO, chronic total occlusion; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; MI, myocardial infarction; MT, medical therapy; PCI, percutaneous coronary intervention; TC, total cholesterol; TG, total triglyceride.
The characteristics of the enrolled patients are shown in Tables 2, 3. Older patients, previous MI, CKD, and taking renin–angiotensin–aldosterone system blockers were more common among the unsuccessful revascularization group than in the successful revascularization group, whereas high LVEF was more prevalent in the successful revascularization patients. Regarding lesion and procedural characteristics, blunt stump, multivessel disease, LCX involvement, calcification, high J-CTO score, and coronary dissection were more common in the unsuccessful revascularization group, whereas CTO location in LAD was more frequent in the successful revascularization group.
Table 2.
Baseline clinical characteristics in the successful and the unsuccessful revascularization groups.
| Total population | Propensity-matched population | |||||
|---|---|---|---|---|---|---|
| Successful revascularization (n = 591) | Unsuccessful revascularization (n = 1,064) | P-value | Successful revascularization (n = 371) | Unsuccessful revascularization (n = 371) | P-value | |
| Age, years | 63.0 ± 9.7 | 64.5 ± 10.4 | 0.003 | 63.3 ± 9.3 | 64.2 ± 10.1 | 0.280 |
| Male, % | 442 (74.8) | 850 (79.9) | 0.016 | 281 (75.7) | 277 (74.7) | 0.734 |
| Smoking, % | 239 (40.4) | 444 (41.7) | 0.610 | 148 (39.9) | 141 (38.0) | 0.598 |
| Hypertension, % | 388 (65.7) | 717 (67.4) | 0.473 | 242 (65.2) | 357 (69.3) | 0.241 |
| Diabetes mellitus, % | 211 (35.7) | 381 (35.8) | 0.966 | 135 (36.4) | 139 (37.5) | 0.761 |
| Dyslipidemia, % | 433 (73.3) | 777 (73.0) | 0.820 | 280 (75.5) | 284 (76.5) | 0.731 |
| TC, (m mol/L) | 4.54 ± 1.34 | 4.59 ± 1.28 | 0.255 | 4.57 ± 1.36 | 4.58 ± 1.24 | 0.831 |
| TG, (m mol/L) | 1.61 (1.14–2.41) | 1.57 (1.11–2.36) | 0.906 | 1.69 (1.16–2.41) | 1.60 (1.09–2.33) | 0.532 |
| HDL-C, (m mol/L) | 1.30 ± 0.62 | 1.23 ± 0.49 | 0.347 | 1.33 ± 0.69 | 1.19 ± 0.37 | 0.207 |
| LDL-C, (m mol/L) | 2.62 ± 0.92 | 2.72 ± 0.90 | 0.056 | 2.62 ± 0.91 | 2.72 ± 0.88 | 0.322 |
| Familial history of CAD, % | 83 (14.0) | 134 (12.6) | 0.402 | 48 (12.9) | 49 (13.2) | 0.913 |
| Previous MI, % | 241 (40.8) | 543 (51.0) | <0.001 | 161 (43.4) | 169 (45.6) | 0.555 |
| Previous PCI, % | 77 (13.0) | 120 (11.3) | 0.292 | 45 (12.1) | 40 (10.8) | 0.564 |
| CKD, % | 33 (5.6) | 109 (10.5) | 0.001 | 22 (5.9) | 32 (8.6) | 0.158 |
| LVEF, % | 53.9 ± 8.4 | 52.1 ± 9.3 | 0.002 | 53.6 ± 8.5 | 56.6 ± 8.7 | 0.474 |
| Stable angina, % | 148 (25.0) | 335 (31.5) | 0.006 | 100 (26.9) | 109 (29.4) | 0.463 |
| UA/NSTEMI, % | 336 (56.8) | 486 (45.7) | <0.001 | 199 (53.6) | 178 (48.1) | 0.123 |
| Baseline medication | ||||||
| Aspirin, % | 578 (97.8) | 1,042 (97.9) | 0.858 | 361 (97.3) | 365 (98.4) | 0.312 |
| Clopidogrel, % | 554 (93.7) | 969 (91.1) | 0.055 | 346 (93.3) | 332 (89.5) | 0.067 |
| Statin, % | 555 (93.9) | 1,008 (94.7) | 0.482 | 350 (94.3) | 347 (93.5) | 0.644 |
| β blocker, % | 438 (74.1) | 804 (75.6) | 0.513 | 279 (75.2) | 276 (74.4) | 0.800 |
| ACEI or ARB, % | 341 (57.7) | 691 (64.9) | 0.004 | 206 (55.5) | 211 (56.9) | 0.711 |
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin-receptor blocker; CAD, coronary artery disease; CKD, chronic kidney disease; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NSTEMI, non-ST elevation myocardial infarction; PCI, percutaneous coronary intervention; TC, total cholesterol; TG, total triglyceride; UA, unstable angina.
Table 3.
Lesion characteristics, procedural characteristics, complications of CTO revascularization, and in-hospital death in the successful and the unsuccessful revascularization groups.
| Total population | Propensity-matched population | |||||
|---|---|---|---|---|---|---|
| Successful revascularization (n = 591) | Unsuccessful revascularization (n = 1,064) | P-value | Successful revascularization (n = 371) | Unsuccessful revascularization (n = 371) | P-value | |
| One CTO lesion, % | 483 (81.7) | 902 (84.8) | 0.108 | 303 (81.7) | 312 (84.1) | 0.380 |
| Two CTO lesions, % | 99 (16.8) | 152 (14.3) | 0.180 | 61 (16.4) | 51 (13.7) | 0.305 |
| LAD, % | 231 (39.1) | 356 (33.5) | 0.022 | 142 (38.3) | 151 (40.7) | 0.499 |
| LCX, % | 144 (24.4) | 322 (30.3) | 0.011 | 97 (26.1) | 105 (28.3) | 0.509 |
| RCA, % | 294 (49.7) | 517 (48.6) | 0.652 | 184 (49.6) | 169 (45.6) | 0.270 |
| Multivessel disease, % | 447 (75.9) | 904 (85.2) | <0.001 | 332 (81.8) | 312 (76.8) | 0.083 |
| Proximal or mid, CTO location, % | 456 (77.2) | 802 (75.4) | 0.416 | 277 (74.7) | 275 (74.1) | 0.866 |
| Blunt stump, % | 237 (40.1) | 636 (59.8) | <0.001 | 149 (40.2) | 177 (47.7) | 0.038 |
| Calcification, % | 103 (17.4) | 230 (21.6) | 0.042 | 67 (18.1) | 86 (23.2) | 0.085 |
| Bending >45°, % | 277 (46.9) | 545 (51.2) | 0.090 | 161 (43.4) | 195 (52.6) | 0.012 |
| Length ≥20 mm, % | 369 (62.4) | 692 (65.0) | 0.291 | 226 (60.9) | 231 (62.3) | 0.706 |
| Collateral flow ≥ 2* | 439 (74.2) | 817 (76.7) | 0.254 | 271 (73.0) | 276 (74.3) | 0.739 |
| J-CTO score | 1.63 ± 1.15 | 1.95 ± 1.21 | <0.001 | 1.58 ± 1.16 | 1.82 ± 1.31 | 0.014 |
| SYNTAX score | 21.7 ± 8.7 | 23.3 ± 8.9 | 0.18 | 22.1 ± 8.6 | 21.8 ± 8.3 | 0.724 |
| Myocardial ischemia, % | 386 (65.3) | 560 (52.6) | <0.001 | 217 (58.4) | 204 (55.0) | 0.335 |
| Complete revascularization (except CTO), % | 441 (74.6) | 762 (71.6) | 0.170 | 279 (75.2) | 267 (72.1) | 0.318 |
| Number of stents** | 1.13 ± 1.03 | 0 | – | 1.08 ± 1.05 | 0 | – |
| Stent type** | ||||||
| SES | 386 (82.1) | – | – | 240 (83.6) | – | – |
| PES | 84 (17.9) | – | – | 47 (16.4) | – | – |
| Coronary dissection, % | 0 | 19 (1.7) | 0.001 | 0 | 7 (2.1) | 0.008 |
| Perforation, % | 0 | 8 (0.7) | 0.057 | 0 | 4 (1.1) | 0.045 |
| In-hospital death, % | 2 (0.3) | 6 (0.6) | 0.719 | 0 | 2 (0.5) | 0.157 |
Collateral circulation flow (Rentrop grade).
Stents data were only available for patients who underwent successful CTO-PCI.
CTO, chronic total occlusion; J-CTO, Japanese-chronic total occlusion; LAD, left ascending coronary artery; LCX, left circumflex coronary artery; PCI, percutaneous coronary intervention; PES, paclitaxel-eluting stent; RCA, right coronary artery; SES, sirolimus-eluting stent.
After PSM, 371 pairs of patients were matched. A total of 287 (77.4%) patients had successful CTO-PCI and 84 (22.6%) patients underwent CTO CABG in the successful revascularization group in the propensity-matched population. As for the patients in the unsuccessful revascularization group among the propensity-matched population, 301 (81.1%) patients received MT and 70 (18.9%) patients underwent failed CTO-PCI. The clinical baseline characteristics were not different between the successful and the unsuccessful revascularization groups after PSM.
Clinical Follow-Up
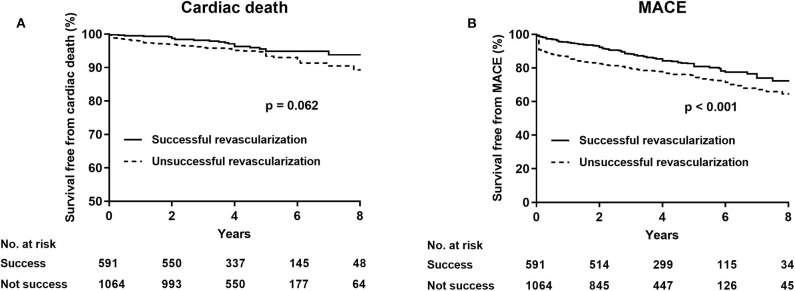
After a follow-up of 3.6 (interquartile range: 2.1–5.0) years, cardiac death (successful revascularization vs. unsuccessful revascularization: 4.2 vs. 6.0%, unadjusted HR 0.65, 95% CI 0.41–1.03, p = 0.065) was similar between the successful and the unsuccessful revascularization groups. After multivariate analyses, no statistically significant difference was observed in terms of cardiac mortality (adjusted HR 0.96, 95% CI 0.59–1.58, p = 0.865) and MI (HR 0.88, 95% CI 0.39–2.01, p = 0.762), whereas the rate of MACE (HR 0.67, 95% CI 0.53–0.85, p = 0.001) and of TVR (HR 0.70, 95% CI 0.52–0.95, p = 0.020) were significantly higher in the unsuccessful revascularization group than in the successful revascularization group (Table 4; Figure 1).
Table 4.
Clinical outcomes in all patients during follow-up.
| Successful revascularization | Unsuccessful revascularization | Unadjusted HR (95% CI) | P-value | Adjusted HR (95% CI) | P-value | |
|---|---|---|---|---|---|---|
| (n = 591) | (n = 1,064) | |||||
| Cardiac death, % | 25 (4.2) | 64 (6.0) | 0.65 (0.41–1.03) | 0.065 | 0.96 (0.59–1.58) | 0.865 |
| MI, % | 34 (5.8) | 78 (7.3) | 0.73 (0.49–1.09) | 0.126 | 0.72 (0.47–1.10) | 0.127 |
| TVR, % | 68 (11.5) | 155 (14.6) | 0.73 (0.55–0.97) | 0.031 | 0.70 (0.52–0.95) | 0.020 |
| MACE, % | 105 (17.8) | 261 (24.5) | 0.65 (0.52–0.81) | <0.001 | 0.67 (0.53–0.85) | 0.001 |
CI, confidence interval(s); HR, hazard ratio; MACE, major adverse cardiovascular events; MI, myocardial infarction; TVR, target-vessel revascularization.
Figure 1.
Kaplan–Meier analysis for cardiac death (A) and major adverse cardiovascular events (B) in the successful revascularization and the unsuccessful revascularization of chronic total occlusion patients.
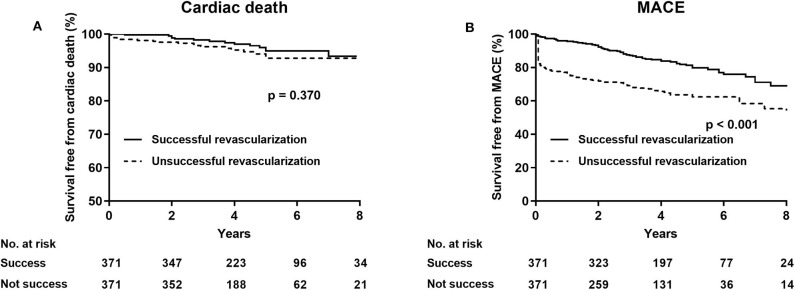
After PSM, the rate of cardiac death (successful revascularization vs. unsuccessful revascularization: 4.6 vs. 5.4%, HR 0.74, 95% CI 0.39–1.43, p = 0.347) was not significantly different in the two groups. After multivariate analyses, the rate of cardiac mortality (adjusted HR 0.68, 95% CI 0.36–1.32, p = 0.256) and of MI (HR 0.60, 95% CI 0.34–1.06, p = 0.080) were comparable, whereas the incidence of MACE (HR 0.43, 95% CI 0.32–0.58, p = 0.001) and of TVR (HR 0.41, 95% CI 0.29–0.58, p < 0.001) were significantly less in the successful revascularization group than in the unsuccessful revascularization group (Table 5; Figure 2).
Table 5.
Clinical outcomes in propensity-matched patients during follow-up.
| Successful revascularization | Unsuccessful revascularization | Unadjusted HR (95% CI) | P-value | Adjusted HR (95% CI) | P-value | |
|---|---|---|---|---|---|---|
| (n = 371) | (n = 371) | |||||
| Cardiac death, % | 17 (4.6) | 20 (5.4) | 0.74 (0.39–1.43) | 0.374 | 0.68 (0.36–1.32) | 0.256 |
| MI, % | 21 (5.7) | 30 (8.1) | 0.64 (0.37–1.13) | 0.123 | 0.60 (0.34–1.06) | 0.080 |
| TVR, % | 48 (12.9) | 99 (26.7) | 0.41 (0.29–0.58) | <0.001 | 0.41 (0.29–0.58) | <0.001 |
| MACE, % | 71 (19.1) | 132 (35.6) | 0.44 (0.33–0.58) | <0.001 | 0.43 (0.32–0.58) | 0.001 |
CI, confidence interval(s); HR, hazard ratio; MACE, major adverse cardiovascular events; MI, myocardial infarction; TVR, target-vessel revascularization.
Figure 2.
Kaplan–Meier curves for cardiac death (A) and major adverse cardiovascular events (B) in the successful revascularization and the unsuccessful revascularization of chronic total occlusion patients after propensity score adjustment.
Subgroup Analysis
Since acute ST-segment elevation myocardial infarction (STEMI) was excluded, the severity of unstable angina (UA) or of non-STEMI (NSTEMI) and stable angina are different, based on a subgroup analysis of the CAD subtype of stable angina and UA/ NSTEMI that we have done. No significant interaction was observed between treatment strategy and CAD groups (p for interaction = 0.098). The cardiac death rate was comparable for the successful and the unsuccessful revascularization groups between the subgroups analyzed (Table 6).
Table 6.
Comparative unadjusted hazard ratio of cardiac death for CAD subgroup according to successful and unsuccessful revascularization.
| CAD | Number of patients | Unadjusted HR (95% CI) | P value | P for interaction |
|---|---|---|---|---|
| Stable angina | 483 | 0.58 (0.23–1.48) | 0.258 | |
| UA/NSTEMI | 822 | 1.16 (0.63–2.13) | 0.618 | 0.098 |
CABG, coronary artery bypass grafting; CAD, coronary artery disease; CI, confidence interval(s); HR, hazard ratio; NSTEMI, non-ST elevation myocardial infarction; UA, unstable angina.
Discussion
We assessed the long-term cardiovascular survival of patients with successful and with unsuccessful CTO revascularization in a large cohort of patients and showed that successful CTO revascularization may not reduce cardiac mortality in comparison with unsuccessful revascularization. However, the patients who received unsuccessful revascularization tended to have a higher prevalence of MACE and target-vessel revascularization as compared with patients who underwent successful revascularization.
With advancement in devices and skills, high procedural success rates could be achieved in CTO revascularization (20, 21). However, 44% of all CTO patients received conservative treatment (7). In the DECISION-CTO and EuroCTO trials, PCI was not associated with reducing death, repeated revascularization, and MACE compared to MT (22, 23). It was known that CABG was a common management of CTOs according to guidelines (24), especially in patients with multi-vessel coronary disease (14, 15). However, patients with CTOs who underwent CABG were not included in the two randomized trials.
Previous cohort studies mainly focused on the outcomes of successful PCI, as opposed to a failed procedure among CTO patients, and showed positive outcomes with respect to successful CTO-PCI (4, 25). However, to date, the prognosis of successful revascularization of CTO remains uncertain, and there is limited data on the impact of successful revascularization for CTO patients on long-term cardiovascular survival.
In the present study, patients who had unsuccessful revascularization were older and more likely to have LCX involvement, blunt stump, calcification, and high J-CTO score. A lower LVEF was also more frequently observed among them, which means worse cardiac function. These data were consistent with the finding of Yang and coworkers (26). Therefore, a large proportion of these patients with CTOs was unsuitable for revascularization or was more inclined to fail (27, 28).
To adjust for potential selection bias, we performed the PSM analysis and we found that the cardiac death rates were similar between the groups, concordant with the results of prior studies (29, 30). A prior study revealed that successful revascularization was not associated with reducing cardiac mortality compared to medical therapy (31). In the COURAGE trial comparing PCI with MT in patients with stable coronary heart disease (CHD), PCI did not have priority over medical therapy (32). Similarly, our analysis also demonstrated that successful revascularization did not improve long-term cardiovascular survival. The majority of the enrolled patients in our study were with stable CHD, and the COURAGE trial also included similar patients.
However, we also found that successful revascularization was associated with significantly less target-vessel revascularization and MACE compared with unsuccessful procedures, consistent with prior findings (13, 26, 29). The mechanism of revascularization in reducing the MACEs of CTO patients is unclear, but reducing or eliminating myocardial ischemia may have attributed to the good long-term clinical outcomes (33). The amount of viable myocardium viability in the CTO-related territory can have an influence on LVEF, and successful revascularization was associated with the recovery of hibernating myocardium and reduction in adverse left ventricular remodeling. Depressed LVEF is well-known to be associated with increased risk of MACEs, and the improvement of LVEF increased electrical stability, reduced ventricular arrhythmias (a main reason for cardiac death), and provided the collateral vessels with protection against future adverse events (34).
The difference in survival, free from MACE, dramatically became large in less than several months. We found that TVR was the predominant determinant of MACE. Many patients were with prior coronary stenosis, new lesion, or lesion progression before CTO location and they received, following CABG or repeat PCI for these stenotic lesions, when they had new or persistent angina after optimal medical therapy (13, 29). In addition, stent thrombosis and in-stent restenosis, which are caused by stent under-sizing, presence of residual dissection, and residual disease proximal or distal to the stent lesion, were other reasons for TVR and often appeared in the first few months, especially in first 30 days after PCI (35).
The cost-effectiveness of PCI vs. optimal medical therapy is also an important factor for clinical decision making. It was confirmed that the cost of CTO-PCI was superior to optimal medical therapy (10). A study showed that CTO-PCI satisfies the criteria for cost-effectiveness in a population with chronic stable angina, especially among patients with severe symptoms (10). CTO-PCI could yield a significantly higher cost-effectiveness ratio by reducing adverse outcomes and improving the quality of life as compared to optimal medical therapy. Additionally, reducing potentially preventable complications could reduce the costs of CTO-PCI and enhance the cost-effectiveness of revascularization procedures (36). These results indicate that CTO-PCI might be carefully considered in terms of operative complications, clinical outcomes, and cost-effectiveness.
Limitations should be taken into consideration. Firstly, this was not a randomized–controlled study, even though the potential confounding factors were minimized using PSM. Secondly, the residual ischemia-related CTO after revascularization, during the follow-up of the study patients, was not routinely evaluated by stress echocardiography or SPECT for every CTO patient in the large-sample-size study.
Conclusions
For treatment of CTO, successful revascularization is not associated with improved long-term cardiovascular survival compared with unsuccessful revascularization. However, successful revascularization is associated with significantly less MACE and target-vessel revascularization. Future randomized studies are warranted to confirm these findings.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the First Affiliated Hospital of Dalian Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
LG prepared the manuscript. All authors contributed to the data collection and analyses, edited the draft manuscript, and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Olivari Z, Rubartelli P, Piscione F, Ettori F, Fontanelli A, Salemme L, et al. Immediate results and one-year clinical outcome after percutaneous coronary interventions in chronic total occlusions: data from a multicenter, prospective, observational study (TOAST-GISE). J Am Coll Cardiol. (2003) 41:1672–8. 10.1016/S0735-1097(03)00312-7 [DOI] [PubMed] [Google Scholar]
- 2.Sianos G, Werner GS, Galassi AR, Papafaklis MI, Escaned J, Hildick-Smith D, et al. Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention. (2012) 8:139–45. 10.4244/EIJV8I1A21 [DOI] [PubMed] [Google Scholar]
- 3.Sirnes PA, Myreng Y, Mølstad P, Bonarjee V, Golf S. Improvement in left ventricular ejection fraction and wall motion after successful recanalization of chronic coronary occlusions. Eur Heart J. (1998) 19:273–81. 10.1053/euhj.1997.0617 [DOI] [PubMed] [Google Scholar]
- 4.George S, Cockburn J, Clayton TC, Ludman P, Cotton J, Spratt J, et al. Long-term follow-up of elective chronic total coronary occlusion angioplasty: analysis from the U.K. Central cardiac audit database. J Am Coll Cardiol. (2014) 64:235–43. 10.1016/j.jacc.2014.04.040 [DOI] [PubMed] [Google Scholar]
- 5.Valenti R, Migliorini A, Signorini U, Vergara R, Parodi G, Carrabba N, et al. Impact of complete revascularization with percutaneous coronary intervention on survival in patients with at least one chronic total occlusion. Eur Heart J. (2008) 29:2336–42. 10.1093/eurheartj/ehn357 [DOI] [PubMed] [Google Scholar]
- 6.Wijeysundera HC, Norris C, Fefer P, Galbraith PD, Knudtson ML, Wolff R, et al. Relationship between initial treatment strategy and quality of life in patients with coronary chronic total occlusions. EuroIntervention. (2014) 9:1165–72. 10.4244/EIJV9I10A197 [DOI] [PubMed] [Google Scholar]
- 7.Fefer P, Knudtson ML, Cheema AN, Galbraith PD, Osherov AB, Yalonetsky S, et al. Current perspectives on coronary chronic total occlusions: the Canadian multicenter chronic total occlusions registry. J Am Coll Cardiol. (2012) 59:991–7. 10.1016/j.jacc.2011.12.007 [DOI] [PubMed] [Google Scholar]
- 8.Ladwiniec A, Allgar V, Thackray S, Alamgir F, Hoye A. Medical therapy, percutaneous coronary intervention and prognosis in patients with chronic total occlusions. Heart. (2015) 101:1907–14. 10.1136/heartjnl-2015-308181 [DOI] [PubMed] [Google Scholar]
- 9.Rathore S, Matsuo H, Terashima M, Kinoshita Y, Kimura M, Tsuchikane E, et al. Procedural and in-hospital outcomes after percutaneous coronary intervention for chronic total occlusions of coronary arteries 2002 to 2008: impact of novel guidewire techniques. JACC Cardiovasc Interv. (2009) 2:489–97. 10.1016/j.jcin.2009.04.008 [DOI] [PubMed] [Google Scholar]
- 10.Gada H, Whitlow PL, Marwick TH. Establishing the cost-effectiveness of percutaneous coronary intervention for chronic total occlusion in stable angina: a decision-analytic model. Heart. (2012) 98:1790–7. 10.1136/heartjnl-2012-302581 [DOI] [PubMed] [Google Scholar]
- 11.Azzalini L, Jolicoeur EM, Pighi M, Millán X, Picard F, Tadros VX, et al. Epidemiology, management strategies, and outcomes of patients with chronic total coronary occlusion. Am J Cardiol. (2016) 118:1128–35. 10.1016/j.amjcard.2016.07.023 [DOI] [PubMed] [Google Scholar]
- 12.Tomasello SD, Boukhris M, Giubilato S, Marza F, Garbo R, Contegiacomo G, et al. Management strategies in patients affected by chronic total occlusions: results from the Italian registry of chronic total occlusions. Eur Heart J. (2015) 36:3189–98. 10.1093/eurheartj/ehv450 [DOI] [PubMed] [Google Scholar]
- 13.Jang WJ, Yang JH, Choi SH, Song YB, Hahn JY, Choi JH, et al. Long-term survival benefit of revascularization compared with medical therapy in patients with coronary chronic total occlusion and well-developed collateral circulation. JACC Cardiovasc Interv. (2015) 8:271–9. 10.1016/j.jcin.2014.10.010 [DOI] [PubMed] [Google Scholar]
- 14.Banerjee S, Master RG, Peltz M, Willis B, Mohammed A, Little BB, et al. Influence of chronic total occlusions on coronary artery bypass graft surgical outcomes. J Card Surg. (2012). 27:662–7. 10.1111/jocs.12021 [DOI] [PubMed] [Google Scholar]
- 15.Kappetein AP, Dawkins KD, Mohr FW, Morice MC, Mack MJ, Russell ME, et al. Current percutaneous coronary intervention and coronary artery bypass grafting practices for three-vessel and left main coronary artery disease. Insights from the SYNTAX run-in phase. Eur J Cardiothorac Surg. (2006) 29:486–91. 10.1016/j.ejcts.2006.01.047 [DOI] [PubMed] [Google Scholar]
- 16.Guo L, Zhang SF, Wu J, Zhong L, Ding HY, Xu JY, et al. Successful recanalisation of coronary chronic total occlusions is not associated with improved cardiovascular survival compared with initial medical therapy. Scand Cardiovasc J. (2019) 53:305–11. 10.1080/14017431.2019.1645351 [DOI] [PubMed] [Google Scholar]
- 17.Godino C, Bassanelli G, Economou FI, Takagi K, Ancona M, Galaverna S, et al. Predictors of cardiac death in patients with coronary chronic total occlusion not revascularized by PCI. Int J Cardiol. (2013) 168:1402–9. 10.1016/j.ijcard.2012.12.044 [DOI] [PubMed] [Google Scholar]
- 18.Guo L, Wu J, Zhong L, Ding HY, Xu JY, Zhou XC, et al. Two-year clinical outcomes of medical therapy vs. revascularization for patients with coronary chronic total occlusion. Hellenic J Cardiol. (2019). 10.1016/j.hjc.2019.03.006. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 19.Rentrop KP, Cohen M, Blanke H, Phillips RA. Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol. (1985) 5:587–92. 10.1016/S0735-1097(85)80380-6 [DOI] [PubMed] [Google Scholar]
- 20.Konstantinidis NV, Sofidis G, Kolettas V, Karvounis H, Sianos G. Bifurcation CTO recanalization with contemporary antegrade and retrograde techniques in a patient with two chronically occluded coronary arteries. Hellenic J Cardiol. (2016) 57:371–4. 10.1016/j.hjc.2016.11.029 [DOI] [PubMed] [Google Scholar]
- 21.Galassi AR, Tomasello SD, Reifart N, Werner GS, Sianos G. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention. (2011) 7:472–9. 10.4244/EIJV7I4A77 [DOI] [PubMed] [Google Scholar]
- 22.Lee SW, Lee PH, Ahn JM, Park DW, Yun SC, Han S, et al. Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion: the DECISION-CTO trial. Circulation. (2019) 139:1674–83. 10.1161/CIRCULATIONAHA.118.031313 [DOI] [PubMed] [Google Scholar]
- 23.Werner GS, Martin-Yuste V, Hildick-Smith D, Boudou N, Sianos G, Gelev V, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. (2018) 39:2484–93. 10.1093/eurheartj/ehy220 [DOI] [PubMed] [Google Scholar]
- 24.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention. A report of the American college of cardiology foundation/American heart association task force on practice guidelines and the society for cardiovascular angiography and interventions. J Am Coll Cardiol. (2011) 58:e44–122. 10.1016/j.jacc.2011.08.007 [DOI] [PubMed] [Google Scholar]
- 25.Jones DA, Weerackody R, Rathod K, Behar J, Gallagher S, Knight CJ, et al. Successful recanalization of chronic total occlusions is associated with improved long-term survival. JACC Cardiovasc Interv. (2012) 5:380–8. 10.1016/j.jcin.2012.01.012 [DOI] [PubMed] [Google Scholar]
- 26.Yang JH, Kim BS, Jang WJ, Ahn J, Park TK, Song YB, et al. Optimal medical therapy vs. percutaneous coronary intervention for patients with coronary chronic Total occlusion: a propensity-matched analysis. Circ J. (2016) 80:211–7. 10.1253/circj.CJ-15-0673 [DOI] [PubMed] [Google Scholar]
- 27.Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. (2011) 4:213–21. 10.1016/j.jcin.2010.09.024 [DOI] [PubMed] [Google Scholar]
- 28.Guo L, Lv HC, Huang RC. Percutaneous coronary intervention in elderly patients with coronary chronic total occlusions: current evidence and future perspectives. Clin Interv Aging. (2020) 15:771–81. 10.2147/CIA.S252318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee PH, Lee SW, Park HS, Kang SH, Bae BJ, Chang M, et al. Successful recanalization of native coronary chronic total occlusion is not associated with improved long-term survival. JACC Cardiovasc Interv. (2016) 9:530–8. 10.1016/j.jcin.2015.11.016 [DOI] [PubMed] [Google Scholar]
- 30.Guo L, Zhong L, Chen K, Wu J, Huang RC. Long-term clinical outcomes of optimal medical therapy vs. successful percutaneous coronary intervention for patients with coronary chronic total occlusions. Hellenic J Cardiol. (2018) 59:281–7. 10.1016/j.hjc.2018.03.005 [DOI] [PubMed] [Google Scholar]
- 31.Guo L, Lv H, Zhong L, Wu J, Ding HY, Xu JY, et al. Gender differences in long-term outcomes of medical therapy and successful percutaneous coronary intervention for coronary chronic total occlusions. J Interv Cardiol. (2019) 24:484–8. 10.1155/2019/2017958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boden WE, O'Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. (2007) 356:1503–16. 10.1056/NEJMoa070829 [DOI] [PubMed] [Google Scholar]
- 33.Shaw LJ, Berman DS, Maron DJ, Mancini GB, Hayes SW, Hartigan PM, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation. (2008) 117:1283–91. 10.1161/CIRCULATIONAHA.107.743963 [DOI] [PubMed] [Google Scholar]
- 34.Samy M, El Awady WS, Al-Daydamony MM, Abd El Samei MM, Shokry K. Echocardiographic assessment of left ventricular function recovery post percutaneous coronary intervention of chronic total occlusions in patients with low and mid-range left ventricular ejection fractions. Echocardiography. (2020) 37:239–46. 10.1111/echo.14582 [DOI] [PubMed] [Google Scholar]
- 35.Byrne RA, Joner M, Kastrati A. Stent thrombosis and restenosis: what have we learned and where are we going? The andreas grüntzig lecture ESC 2014. Eur Heart J. (2015) 36:3320–31. 10.1093/eurheartj/ehv511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Salisbury AC, Karmpaliotis D, Grantham JA, Sapontis J, Meng Q, Magnuson EA, et al. In-hospital costs and costs of complications of chronic total occlusion angioplasty: insights from the OPEN-CTO registry. JACC Cardiovasc Interv. (2019) 12:323–31. 10.1016/j.jcin.2018.10.025 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.