Abstract
Posttraumatic Stress Disorder (PTSD) is characterized by heightened avoidance, cognitive inflexibility, and impaired reward processing. Maladaptive behavior in PTSD may reflect an imbalance between approach and avoidance, but no research has investigated approach-avoidance conflict (AAC) in PTSD. The current study investigated approach-avoidance behavior in PTSD using a trauma-related AAC (trAAC) task in two independent samples. In Study 1, 43 women with a current diagnosis of PTSD and 18 healthy comparison subjects were recruited from the community. In Study 2, 53 women with trauma exposure and a range of PTSD symptoms were recruited from a correctional institution. Trials were separated into two phases: Conflict (the option most likely to win points was most likely to show a trauma-related image) and Congruent (the option most likely to win points was least likely to show a trauma-related image). In Study 1, reward obtainment varied with the task manipulation (i.e., fewer points earned during Conflict compared to Congruent Phase) in PTSD but not healthy subjects. These results indicate that when avoidance is advantageous (Congruent Phase), individuals with PTSD show increased task performance, whereas when avoidance is maladaptive (Conflict Phase), individuals with PTSD show increased sacrifice of reward. In Study 2, higher PTSD symptoms predicted decreased reward earning during the Conflict Phase, again indicating a sacrifice of reward when avoidance is maladaptive. Across both studies, PTSD associated with increased AAC and sacrifice of reward in the presence of trauma-related stimuli. These studies shed light on AAC in PTSD and could inform more targeted therapy approaches.
Keywords: Posttraumatic Stress Disorder, Approach-Avoidance Conflict, Sacrifice of Reward, Avoidance Bias
Approach-avoidance conflict is a key aspect of Posttraumatic Stress Disorder but has not been explicitly tested using behavioral tasks. The results of this study indicate that PTSD is associated with greater approach-avoidance conflict than healthy subjects, and this conflict is associated with a sacrifice of reward.
Experiencing trauma over one’s lifetime is remarkably common, with over 70% of adults reporting exposure to at least one traumatic event, and over 30% reporting exposure to four or more traumatic events (Benjet et al., 2016; Kessler et al., 2017). Further, an estimated two percent of men and three percent of women worldwide meet criteria for a lifetime diagnosis of posttraumatic stress disorder (PTSD) (Fazel & Baillargeon, 2011). Symptoms of PTSD are often chronic, with 40% of individuals reporting symptoms six years following their onset (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Chronic PTSD is associated with adverse mental and physical health sequalae, including poor self-reported health, depression, increased risk of suicide, and substance use (Kessler, 2000; Olatunji, Cisler, & Tolin, 2007). Current treatments for PTSD, including prolonged exposure (PE), emphasize repeated contact with avoided stimuli (e.g., emotions, memories of the trauma), and have garnered empirical support (Foa et al., 1991, 1999). Though considered the gold-standard treatment for PTSD, PE does not lead to symptom improvement in all cases, with only 40–60% showing significant symptom remission (Foa et al., 1991, 1999). As such, identification of individualized psychological and behavioral mechanisms responsible for the maintenance or improvement of PTSD symptoms is essential for improving treatment.
A hallmark symptom of PTSD is avoidance, and presence of at least one avoidance symptom is required for diagnosis (American Psychiatric Association, 2015). To decrease anxiety associated with trauma-related stimuli, individuals may avoid thoughts, memories, or stimuli that evoke traumatic memories. While avoidance provides short-term relief, avoidance behavior is associated with onset and maintenance of PTSD symptoms and increased distress over time (Boden et al., 2012; Kumpula et al., 2011; Marx & Sloan, 2005). Furthermore, avoidance can exacerbate other symptoms, resulting in a negative feedback loop (Kumpula et al., 2011). Whereas avoiding trauma reminders may be adaptive in dangerous situations (Marks & Nesse, 1994), the generalization and inflexibility of avoidance comes at the high cost of functional impairment and sacrifice of reward (Hayes, 1976). Therefore, an inability to resolve conflict between approaching reward and avoiding trauma-related stimuli may be one mechanism for the maintenance of PTSD symptoms.
While the majority of research on PTSD has focused on fear conditioning and emotion dysregulation, other deficits, such as reward-processing, may contribute to the maintenance of PTSD symptoms (Nawijn et al., 2015; Stein & Paulus, 2009). Emotional numbing and anhedonia, or the loss of interest/pleasure, are highly prevalent among PTSD populations, consistent with reward processing deficits among individuals with PTSD (Pietrzak et al., 2011). In addition, PTSD is related to lower expectations of reward and lower satisfaction in surprising rewards (Hopper et al., 2008), indicating that emotional numbing/anhedonia may arise from dysfunctional reward processing. These alterations in reward processing may alter approach tendencies in those with PTSD, leading to decreased tendencies to approach reward.
Approach and avoidance processes rarely act in isolation. Coupled with high levels of avoidance maintained by negative reinforcement, deficits in reward processing might interfere with the ability to effectively pursue reward when conflict arises between approaching rewards and avoiding trauma reminders. People regularly encounter cues that afford potential reward and distress simultaneously. One must navigate the competing outcome contingencies of reward and threat to resolve the conflict. For example, although physical intimacy may be rewarding, an individual with PTSD following sexual assault may avoid physical intimacy due to trauma-related memories. After avoiding physical intimacy and the subsequent relief from avoidance, the individual may avoid future opportunities for intimacy in response to anticipatory anxiety about trauma-related memories. Therefore, the range of available behaviors becomes restricted to those that do not elicit unwanted emotions, memories, and other internal experiences. Thus, the individual must choose to either: engage in reward in the presence of trauma-related stimuli (approach) or sacrifice reward to avoid trauma-related stimuli (avoidance).
Prior research has demonstrated the ability to probe this type of conflict resolution behavior using approach-avoidance conflict (AAC) paradigms in a variety of populations, including those with various anxiety disorders (Pittig, Brand, et al., 2014; Pittig, Pawlikowski, et al., 2014). Imbalances in AAC (i.e., biases in favor of avoidance) have been linked to increased trait anxiety, such that participants with higher levels of anxiety sacrifice greater reward in order to avoid negative stimuli (Aupperle et al., 2011). Emerging research demonstrates the importance of conceptualizing PTSD as a dynamic, heterogeneous disorder involving both avoidance and reward-processing dysregulation (Nawijn et al., 2015; Stein & Paulus, 2009). This multi-system imbalance underlying anxiety-related disorders (Kirlic et al., 2017) can be studied behaviorally via AAC tasks, and could provide mechanistic explanations of symptom maintenance in PTSD and suggest novel directions for treatment outcome research.
Objectives of the Current Studies
The current study aims to expand understanding of AAC in PTSD in two independent samples. We administered a novel interpersonal trauma (IPT)-specific approach-avoidance conflict (trAAC) task – a paradigm presenting images related to IPT in order to elicit a conflict between gaining rewards (points) and avoiding negative images. The trAAC task manipulates reward-punishment congruency, which at times, creates a conflict wherein the behavior most likely to produce a reward (winning points) is also most likely to produce an aversive stimulus (a trauma-related image).
Study 1
We investigated differences in AAC among women with current PTSD related to IPT as compared to healthy, non-trauma exposed women. We hypothesized that 1) compared to healthy subjects, individuals with PTSD would display increased AAC during the trAAC task. That is, we predict that individuals with PTSD will change their behavior when reward earning conflicts with the avoidance of threatening images, and therefore gain less points during that phase compared to a phase with no conflict. We predict that healthy subjects will not display this behavior change (i.e., will show similar reward earning during each task phase). Relatedly, we hypothesized that 2) within the PTSD group, higher PTSD symptom severity and avoidance symptoms would associate with heightened AAC, predicting fewer points during the Conflict Phase, and greater points during the Congruent Phase.
Method
Participants.
Women with PTSD (n=43) and female healthy comparison subjects (n=18) aged 21–50 were recruited from the community as part of a larger study approved by the university’s Institutional Review Board. Inclusion criteria for the PTSD group were a current diagnosis of PTSD and history of direct interpersonal assault exposure (i.e., physical or sexual assault). Exclusion criteria for all participants were current major medical disorders, history of psychotic symptoms, and current substance use disorder. Exclusion criteria for healthy controls were history of trauma exposure, current DSM-5 Axis I mental illness, or current psychotropic medication use. Demographic information for Study 1 participants is presented in Table 1.
Table 1.
Demographic information, PTSD symptom severity and trauma exposure in Study 1.
| Variable | PTSD Group n=43 | Range | Control Group n=18 | Range |
|---|---|---|---|---|
| Age | 31.9 (8.7) | 21 – 50 | 33.4 (9.0) | 22 – 48 |
| IQ | 108.5 (19.6) | 55 – 169 | 113.7 (20.3) | 73 – 145 |
| Ethnicity | ||||
| Caucasian (%) | 74.4 | -- | 88.9 | |
| African American (%) | 18.6 | -- | 5.55 | -- |
| Other (%) | 7.0 | -- | 5.55 | -- |
| Current Depressive Disorder (%) | 25.6 | -- | 0.0 | -- |
| Current Anxiety Disorder (%) | 67.4 | -- | 0.0 | -- |
| CAPS-5 Total Score | 43.3 (12.2) | 24 – 76 | -- | -- |
| CAPS-5 Avoidance | 5.1 (1.6) | 3 – 8 | -- | -- |
| CAPS-5 Hyperarousal | 11.2 (4.1) | 4 – 20 | -- | -- |
| CAPS-5 Re-experiencing | 10.6 (4.0) | 4 – 20 | -- | -- |
| CAPS-5 Neg. | 16.4 (5.2) | 6 – 28 | -- | -- |
| Cognitions/Mood | ||||
| BDI Total Score | 25.0 (10.5) | 6 – 49 | 1.1 (2.6) | 0 – 9 |
| Direct Assault | 4.9 (2.6) | 2 – 13 | -- | -- |
| Direct Assault (%) | 100.0 | -- | -- | -- |
| Sexual Assault | 2.0 (0.88) | 0 – 4 | -- | -- |
| Sexual Assault (%) | 97.7 | -- | -- | -- |
| Physical Assault | 2.88 (2.3) | 0 – 10 | -- | -- |
| Physical Assault (%) | 86.0 | -- | -- | -- |
| Witnessed Violence | 2.9 (2.7) | 0 – 11 | -- | -- |
| Witnessed Violence (%) | 76.7 | -- | -- | -- |
| Trauma Total Score | 7.81 (4.6) | 2 – 22 | -- | -- |
Note. PTSD=Post-traumatic stress disorder. IQ=Intelligence quotient. CAPS-5=Clinician-Administered PTSD Scale for DSM-5.
Measures
The Receptive One-Word Picture Vocabulary Test (4th edition) measures the ability to match images of objects, actions or concepts with spoken words to estimate verbal Intelligence Quotient (IQ) (Brownell, 2000). Total correct responses were summed for basal and ceiling scores and scaled by developmental age, resulting in a standardized IQ estimate.
The trauma portion of the National Women’s Survey and the National Survey of Adolescents (NSA) is a structured interview used to assess participants’ history of IPT exposure and has been used in prior epidemiological studies of interpersonal violence exposure and mental health functioning (Kilpatrick et al., 2000; Resnick et al., 1993). The assessment uses dichotomous questions to assess participants’ experience of specific traumatic events, including physical and sexual assault, childhood abuse, and witnessed violence.
The Clinician Administered PTSD Scale for DSM-5 (CAPS-5; past month version) is a 30-item structured clinical interview assessing symptom severity during the past month (Weathers et al., 2018). Symptoms are separated into four clusters based on the DSM-5 criteria B-E (Reexperiencing, Avoidance, Negative Cognitions/Mood, and Hyperarousal), rated from 0 (Absent) to 4 (Extreme/incapacitating). Diagnostic criteria require scores of 2 or above for at least one Reexperiencing, one Avoidance, two Negative Cognition/Mood, and two Hyperarousal symptoms.
Trauma-related Approach-Avoidance Conflict Task (trAAC).
In this novel behavioral task, participants were instructed that the objective of the task was to accrue as many points as possible. Participants saw three shapes (circle, square, hexagon) on a computer screen and were instructed to choose one of the three shapes on each trial (Figure 1). Following each choice, the shape was replaced by a photograph (presented for 2–3.25s) that was either 1) neutral (e.g., a cup; mean valence=5.7, mean arousal=3.3) or 2) IPT-related image (e.g., a woman being choked by a man; mean valence=2.3; mean arousal=6.5) from the International Affective Picture System (IAPS; (Lang et al., 1997). After a delay (.5-.75s), the point outcome for that trial appeared under the image (presented for 1.5–2.5s) while the image remained on screen, indicating a positive or negative value (e.g., +5 or −7). Trials were separated by a fixation cross, presented for .5–1.5s. The total number of points was displayed continuously at the bottom of the screen. See Figure 1 for the series of images seen by participants throughout the task. All participants completed the trAAC task after completing all other study materials.
Figure 1.
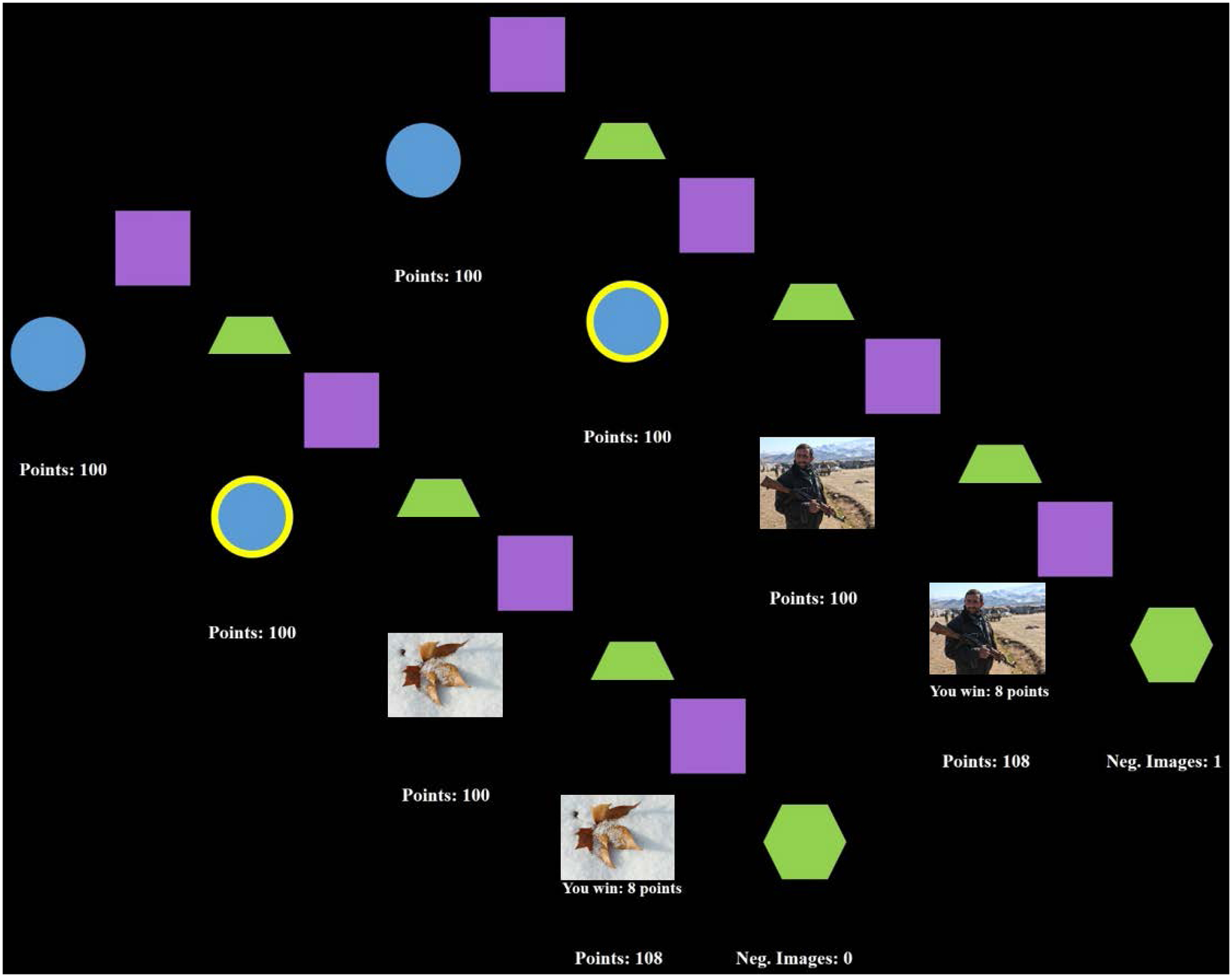
Trauma-related Approach-Avoidance Conflict (trAAC) task. Participants first were presented with three shapes (Decision Phase), then choose between the shapes. After choosing, the shape was highlighted in yellow (Choice Display). Then, the threat outcome was presented (either a neutral or trauma-related image). After a brief delay, the reward outcome (number of points won or lost) was presented.
The task was divided into two phases (Conflict, Congruent), separated into 4 blocks of trials. The Conflict Phase occurred when the option with the highest probability of point reward was also the most likely to show a trauma-related image, whereas the Congruent Phase occurred when the option with the highest probability of point reward was least likely to show a trauma-related image (Figure 2). The type of image (trauma-related or neutral) and the direction of points (positive, negative) were experimentally manipulated to reflect probabilities that aligned with the type of phase. The number of points won/lost was randomly generated (range: 1–10). Task Phases were not counterbalanced in order to allow for initial task structure learning before the introduction to the Conflict Phase. See Figures 2 and 3 for visual depiction of the differing probabilities across Phase and Block.
Figure 2.
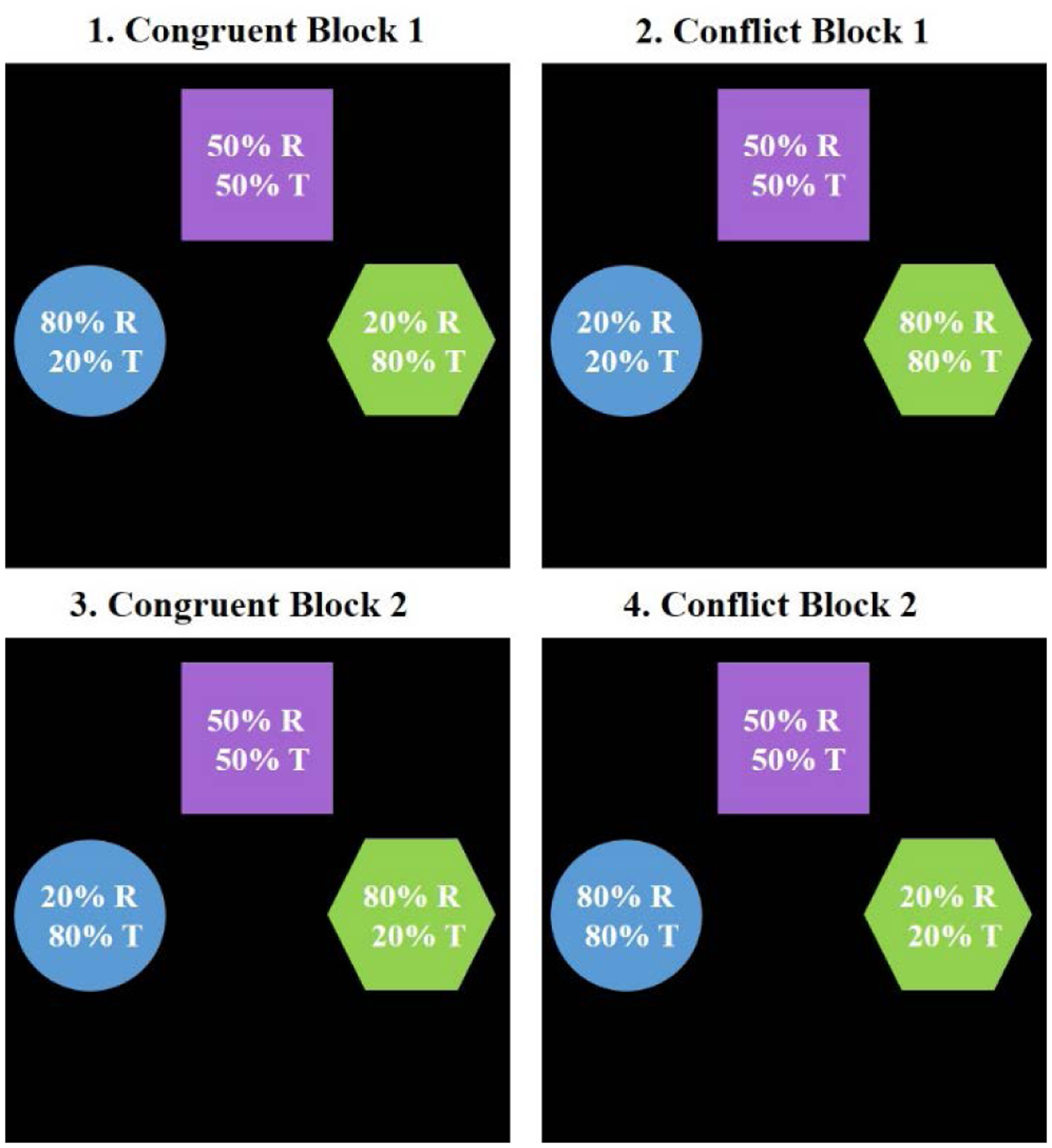
Reward probabilities of each option in each Block of the trAAC task in Study 1. Panes are numbered corresponding to the Block of trials they represent (referenced in Figure 3). In each shape, point reward (R) and threat image (T) probabilities are displayed. In Congruent trials, the option most likely to gain points is least likely to show a trauma-related image (e.g. 80% R, 20% T). In Conflict trials, the option most likely to gain points is most likely to show a trauma-related image (e.g. 80% R, 80% T).
Figure 3.
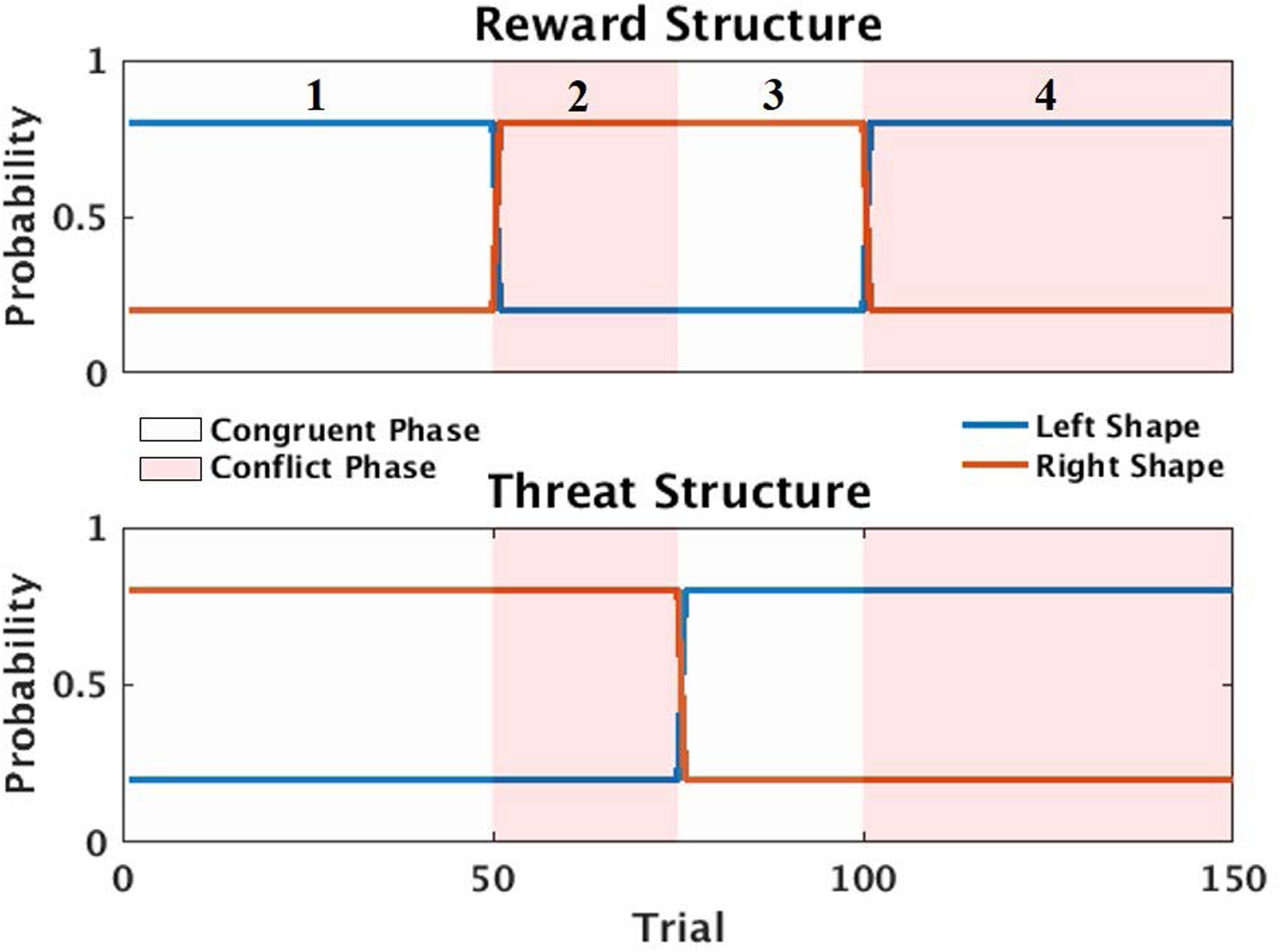
Reward structure of the trAAC task in Study 1. Reward structure shows the probability of reward outcomes (winning or losing points) for two of the three shapes across all trials. The Left and Right Shapes correspond to options seen in Figure 1. Probability of threat and reward outcomes remained at .5 throughout the entire task for the Middle Shape, therefore is not plotted. Threat structure shows the probability of a shape presenting a threat image. The alternation of reward and threat outcome probabilities created the Conflict and Congruent Phase manipulations; Conflict and Congruent phases are depicted in red and white. Therefore, when reward/threat structure = .8, there is an 80% chance of winning a number of points/seeing a threat image, and when probability = .2, there is a 20% chance of winning points/seeing a threat image. Blocks are numbered one through four in the Reward Structure pane, and correspond to the numbered Blocks in Figure 2.
On all trials, both outcomes (image type, point win/loss) had either an 80%, 50%, or 20% chance of occurring (Figures 2 and 3). The image type and point win/loss probabilities were independent from one another. Probabilities for each outcome for the left and right shape (circle and hexagon) were adjusted throughout the task to create the Conflict and Congruent Phases. For example, during Block 1 of the Conflict Phase, if a participant selected the right shape (hexagon), it would have an 80% probability of presenting a trauma-related image and 80% probability of positive points. During Block 2 of the Congruent Phase, however, if a participant chose the right shape, it would have a 20% probability of presenting a trauma-related image and 80% probability of positive points (Figure 2 and 3). The middle shape (square) remained at a 50% chance of reward and 50% chance of presenting a trauma-related image throughout the entirety of the task. Trials were separated into four total Blocks (two Conflict Blocks, two Congruent Blocks), with 75 trials of each type and 150 total trials (Figure 3). Optimal outcome probabilities were based on previous behavioral tasks indicating participants are able to distinguish between outcome probabilities as similar as 40% vs 60%, and previous reward-based learning tasks using outcomes probabilities of 20% vs 80% in individuals with PTSD (Bublatzky et al., 2017; Myers et al., 2013). Previous behavioral tasks indicate participants are able to learn task contingencies in as few as 10–20 trials, therefore to allow ample time for learning and to ensure any differences in behavior were not due to insufficient trials, a minimum of 25 trials were included in each Block (Myers et al., 2013; Pittig et al., 2015).
Data Analysis.
To test Hypothesis 1, participant behavior was modeled using Linear Mixed Effects Models (LMEM) on trial-wise outcomes (i.e., modeling outcomes on all trials for each participant). Predictors were included for Block (sections of trials within each Phase), Phase (Conflict = −1, Congruent = 1), Group (Control = −1, PTSD = 1), and Trial (z-scored within each Block) and regressed on Total Points (scaled from 0 to 1). In order to control for unexplained variance from age and general intelligence, we included Age and IQ as covariates in the model. In order to account for learning effects throughout the task, Trial and Block were also included in the interactive model. Trial was coded to account for learning within each Block (i.e., in a Block with 25 trials, Trial number (1–25) would be z-scored to represent linear learning throughout that Block). Modeling separate Blocks within each Phase allowed for the distinction between initial task learning (Block 1) and task behavior after initial learning (Block 2). Block was coded separately for Congruent and Conflict Phases to account for the differing number of trials within each Block in each Phase, but in both Phases Block 1 was coded as negative and Block 2 as positive. When in the Conflict Phase, Block 1 was coded as −1 (25 trials) and Block 2 was coded as .5 (50 trials). In the Congruent Phase, Block 1 was coded as −.5 (50 trials) and Block 2 was coded as 1 (50 trials). The model estimated a by-subject random intercept and a by-subject random slope for Phase, Block, Trial, and their interactions to account for individual variability. Therefore, the final LMEM was:
To decompose the hypothesized Phase*Group interaction, and to ensure this interaction indeed indicated greater AAC within individuals with PTSD, we calculated an individual Difference Score to represent the degree of “conflict” between the two task phases (Difference score = Mean Conflict Phase points – Mean Congruent Phase points). More negative Difference Scores reflect a higher degree of conflict between the two Phases (i.e., a greater difference in reward earning between Phases, with more points gained in the Congruent Phase). This Difference Score was then used in a subsequent LMEM decomposing the larger hypothesized interaction, again using Age and IQ added as covariates.
In order to test Hypotheses 2, two additional LMEMs were estimated by regressing Block, Phase, Trial, and Total Avoidance symptoms (z-scored) or Total PTSD symptoms (z-scored) on Total Points, with age and IQ as covariates. All other variables were coded as described in the initial LMEM. Total Trauma Score was included in follow up analyses to investigate the influence of trauma exposure on the relation between total PTSD symptoms and total points earned. Trauma Total Score was calculated as the total number of different traumatic experiences a participant reported (range 1–29).
Results
All results modeling trial-wise behavior are presented in Supplemental Table 1. Mean choices for the left and right shapes for both Groups are depicted in Supplemental Figure 1. Groups did not differ on overall points gained on the trAAC task, MPTSD = 174.88, SEPTSD = 17.45, MHC = 167.28, SEHC = 31.38, t(9132) = .268, p = .789.
The LMEM modeling participant trial-wise behavior showed a significant Phase*Block* Group interaction predicting the number of points gained during the trAAC task, β = .019, t(9132) = 3.21, p = .001, ƞp2 = .14, 95% CI [.02, .29], and no higher order interactions. The significant three-way interaction was first probed by exploring Block 1 and Block 2 separately. There was no main effect of Group, and no significant interactions in Block 1. In Block 2, analyses revealed a significant Group*Phase interaction, β = .018, t(4565) = 2.61, p = .009, ƞp2 = .10, 95% CI [.01, .25]. See Figure 4 for graphical depiction. All results from the main LMEM remained significant when controlling for current depressive symptoms (see Supplemental Material).
Figure 4.
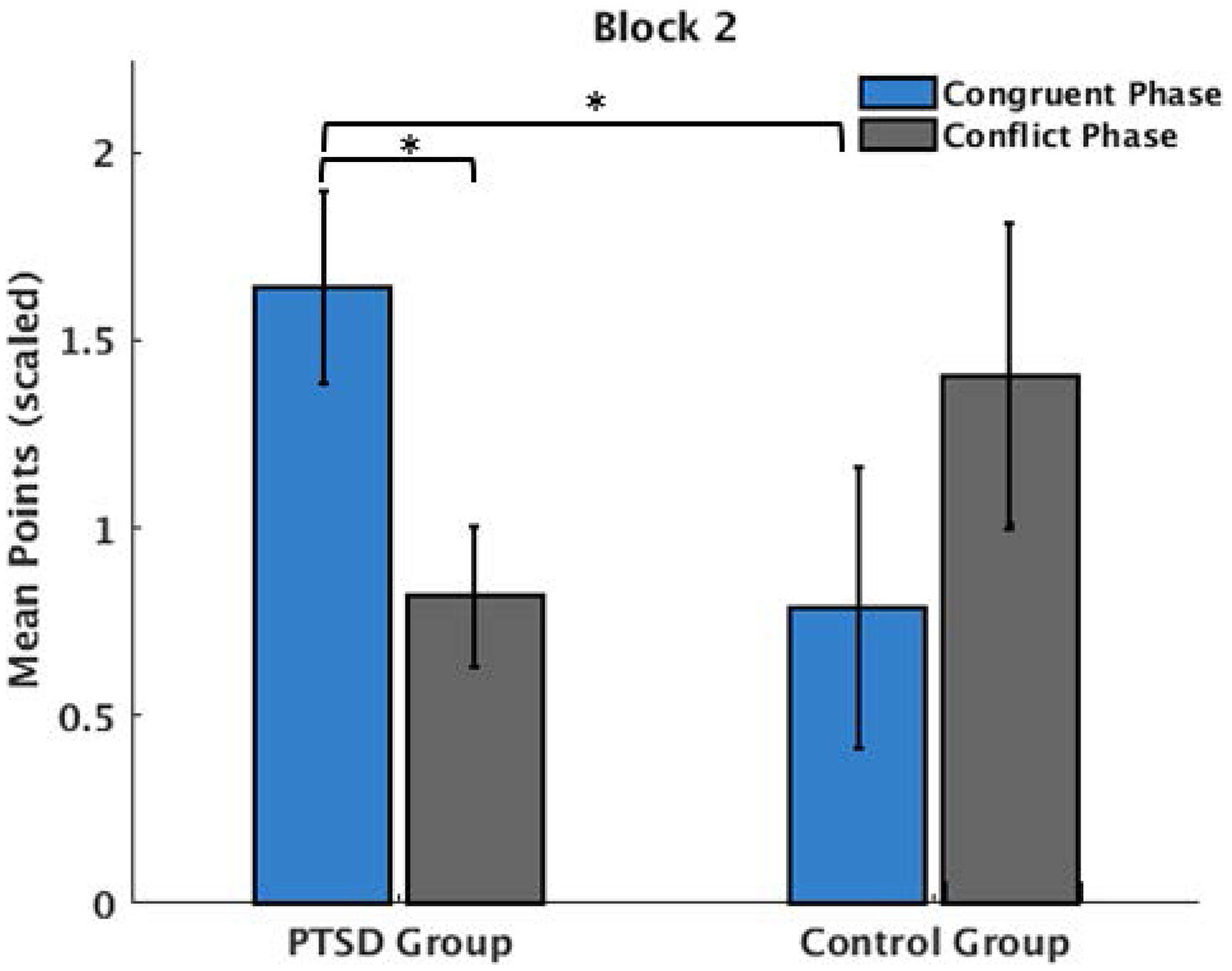
Graphical depiction of Block*Phase*Group interaction in Study 1. Mean points were scaled according to the number of trials within Block 2 of each Phase. Participants in the PTSD group gained significantly fewer points during Block 2 of the Conflict phase compared to the Congruent phase. PTSD participants also gained significantly more points during Congruent Block 2 compared to Controls. There was no difference in mean points gained between Conflict and Congruent phases in the Control group.
The significant three-way interaction was then probed by creating a Difference Score for Block 2 to represent behavior change (i.e., approach-avoidance conflict) induced by the Phase manipulation. Analyses revealed a significant main effect of Group on this Difference Score, with participants in the PTSD group showing greater AAC, and therefore greater reward earning discrepancies between Phase, β = .040, t(57) = −2.98, p = .004, ƞp2 = .13, 95% CI [.02, .29]; Supplemental Figure 2. These results support Hypothesis 1 of increased AAC in PTSD, such that reward obtainment was impaired in the Conflict Phase in those with PTSD compared to the Congruent Phase, but this sensitivity to Phase was not seen in healthy comparison subjects. However, these results were specific to Block 2 of the trAAC task.
Further analyses testing Hypothesis 2 failed to reveal any relations between total points earned and overall PTSD symptom severity or avoidance symptoms. Supplementary analyses controlling for Trauma Total Score also revealed no relation between PTSD symptom severity and total points earned.
Discussion – Study 1
The current study evaluated approach-avoidance conflict resolution in adult women with PTSD compared to healthy comparison subjects. We utilized a novel trauma-related approach-avoidance (trAAC) task with probabilistic reward contingencies in order to probe the competing motivations for approaching reward and avoiding trauma-related stimuli. Points earned during the Congruent Phase, where the choice most likely to provide reward was also most likely to reveal a neutral (i.e., non-threatening) image, were compared against points earned during the Conflict Phase, where the choice most likely to provide reward also is most likely to reveal a trauma-related image. Both groups demonstrated learning of the task contingencies. In Block 2 of the trAAC task, participants with PTSD demonstrated significantly greater AAC, demonstrated by altered reward obtainment depending on whether avoidance of threat was congruent or in conflict with task goals. Healthy participants did not demonstrate altered reward obtainment based on task phase. This supports Hypothesis 1, that increased AAC in the presence of trauma-related stimuli would be increased in those with PTSD but not healthy subjects.
As evidenced by the lack of group differences in Block 1 of each Phase, participants with PTSD were unimpaired in learning the structure of the trAAC task. This is in contrast to a previous study of avoidance behavior in social anxiety disorder, where the authors observed behavioral differences between patients and controls only during the first block (i.e., when participants are learning the task structure) of a modified Iowa Gambling task (Pittig, Pawlikowski, Craske, & Alpers, 2014). However, the current results demonstrate that heightened AAC in PTSD emerged only after the structure was first learned in Block 1, suggesting this difference in PTSD may be a strategic bias of avoiding treat (i.e., emerges only after learning the task structure), rather than an impairment in learning.
Strengths of the trAAC task include the use of disorder-specific stimuli, active decision-making (rather than passively presented stimuli), and a probabilistic learning structure. Disorder-specific stimuli allowed the task to probe avoidance specific to trauma-related stimuli, in contrast to negative stimuli not commonly encountered in daily life (e.g. shocks). Instead of including determined outcomes, the probabilistic learning structure allowed an investigation of subjects’ behavior when outcomes were sometimes ambiguous. This mimics more relevant, daily decisions, which do not always lead to the expected outcome. A notable limitation is the use of a group comparison between healthy subjects with no trauma history and participants with a current diagnosis of PTSD (i.e. all trauma-exposed); therefore, all trauma-exposed participants exhibit relatively high symptoms of PTSD. This limitation may obscure interpretation of the relationship between subthreshold PTSD symptoms and AAC resolution. In addition, all participants in the PTSD group had experienced an IPT, which may influence AAC resolution differently compared with different forms of trauma exposure. Because the influence of PTSD could not be disentangled from trauma exposure, a more specific investigation of the PTSD symptoms and AAC resolution, regardless of trauma exposure, is necessary.
Study 2
In order to investigate the relationship between PTSD symptom severity and approach-avoidance behavior, and to clarify the influence of PTSD symptoms separate from trauma exposure, Study 2 administered a similar trAAC paradigm in a sample of incarcerated women. Trauma among incarcerated samples is extremely high relative to normative samples, particularly among women, with 42% of incarcerated women reporting experience of childhood abuse compared to 26% of non-incarcerated women (Poister Tusher & Cook, 2010). Additionally, the prevalence of PTSD among incarcerated women is three- to five- times greater than non-incarcerated women (Karlsson & Zielinski, 2018; Kessler et al., 1995).
In Study 2, all women experienced IPT, and current PTSD severity varied from asymptomatic to severe. Administering the trAAC task in a sample with a range of PTSD symptoms allows investigation of a scalar relationship between PTSD symptoms and altered resolution of AAC. In addition, because all subjects in Study 2 experienced IPT, the influence of these continuous PTSD symptoms can be investigated separately from the experience of trauma. In contrast to Study 1, a continuous measure of PTSD symptom severity replaced the dichotomous variable of PTSD diagnosis. Therefore, individuals with subthreshold PTSD were included in these analyses, resulting in a much wider range of symptomatology (see Table 1 and Table 2 for PTSD symptom ranges). In addition, task structure was changed in Study 2 such that one Conflict Phase is preceded by a change in reward probability, and one Conflict Phase is preceded by a change in threat probability (Figure 5). This was in contrast to Study 1, where both Conflict Phase Blocks were preceded by a change in reward probability. This change in structure allowed analyses to more specifically address the influence of threat on AAC, unrelated to reward probability learning. In accordance with Study 1, we hypothesized 3) that higher PTSD symptoms would associate with increased approach-avoidance conflict in the presence of trauma-related stimuli, and therefore greater discrepancies in reward obtainment in those with higher PTSD symptoms depending on task Phase. We predicted this behavior change would associate with greater reward earning during the Congruent Phase (when avoidance is adaptive) and decreased reward earning during the Conflict Phase (when avoidance is maladaptive) in those with higher PTSD symptoms compared to those with low symptoms. Relatedly, we expected that 4) higher PTSD avoidance symptoms would relate to fewer points during the Conflict Phase, and more points during the Congruent Phase. We expected that the effect of PTSD symptoms would be present even when controlling for the effects of trauma exposure on task performance.
Table 2.
Demographic information, PTSD symptom severity and trauma exposure in Study 2, N=50.
| Variable | M(SD) | Range |
|---|---|---|
| Age | 33.2 (8.1) | 20 – 54 |
| IQ | 97.2 (12.0) | 74 – 128 |
| Ethnicity | ||
| Caucasian (%) | 54.9 | -- |
| African American (%) | 25.5 | -- |
| Other (%) | 19.6 | -- |
| -- | ||
| Current Depressive Disorder (%) | 6.0 | -- |
| Current Anxiety Disorder (%) | 29.4 | -- |
| PCL-5 Total Score | 29.2 (16.8) | 1 – 57 |
| PCL-5 Avoidance | 3.7 (2.5) | 0 – 8 |
| PCL-5 Hyperarousal | 8.0 (4.9) | 0 – 19 |
| PCL-5 Re-experiencing | 7.5 (5.4) | 0 – 16 |
| PCL-5 Negative | 10.1 (6.4) | 0 – 22 |
| Cognitions/Mood | ||
| Direct Assault | 5.7 (4.1) | 0 – 16 |
| Direct Assault (%) | 92.0 | -- |
| Sexual Assault | 2.1 (1.9) | 0 – 5 |
| Sexual Assault (%) | 68.0 | -- |
| Physical Assault | 3.6 (2.9) | 0 – 11 |
| Physical Assault (%) | 88.0 | -- |
| Witnessed Violence | 3.4 (2.4) | 0 – 8 |
| Witnessed Violence (%) | 86.0 | -- |
| Trauma Total Score | 9.1 (5.6) | 1 – 23 |
Note. PTSD=Post-traumatic stress disorder. IQ=Intelligence quotient. CAPS-5=Clinician-Administered PTSD Scale for DSM-5.
Figure 5.
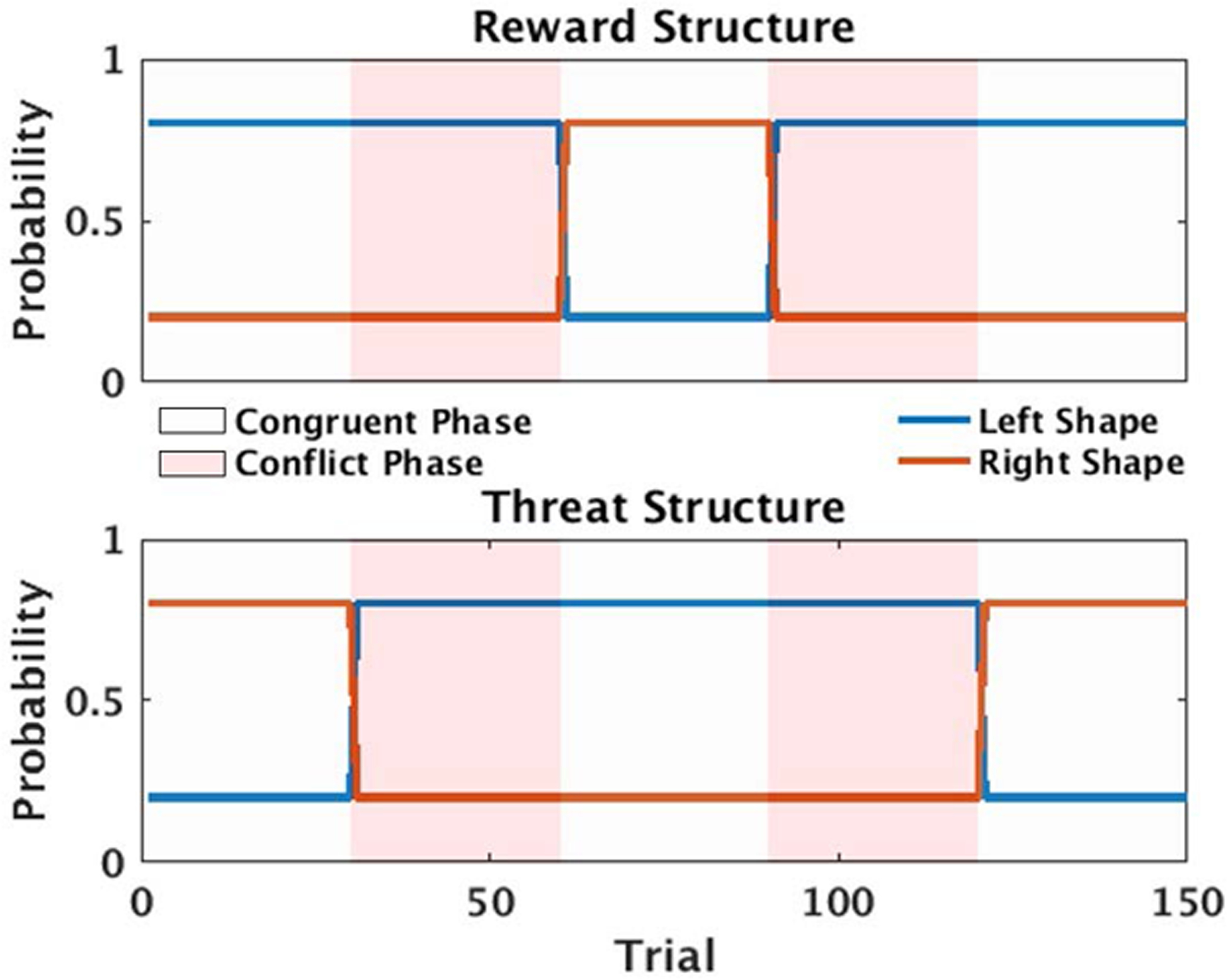
Task structure of the trAAC task in Study 2. Outcome probabilities were alternated such that the first Conflict Phase is preceded by a change in threat probability (probability of seeing a trauma-related image), and the second Conflict Phase is preceded by a change in reward probability (probability of winning points). Threat and Reward probabilities for the Middle Shape remain at .5 throughout the task, and therefore are not plotted. All other task details are explained in Figure 3.
Method
Participants.
Fifty-three women aged 18–55 and incarcerated at a women’s correctional institution were recruited as part of a larger study approved by the local Institutional Review Board. Exclusionary criteria included history of psychotic symptoms, reading level below fourth grade, and an IQ estimate of <70 (Wechsler, 1981). Women who met inclusion criteria after the initial interview were recruited for the additional task component of the study. Two participants had no history of trauma exposure, and one participant had incomplete PTSD symptom data, resulting in a final sample of 50 participants. All included participants endorsed experience of IPT. All demographic information for participants in Study 2 is presented in Table 2.
Measures
Due to logistical constraints related to research with an incarcerated sample, the National Women’s Survey and the National Survey of Adolescents (NSA) was modified from Study 1 to an abbreviated form in order to assess participants’ trauma exposure. In place of a structured clinical interview, all questions were adapted into a self-report questionnaire for participants to complete in the presence of the interviewer.
Severity of PTSD symptoms was assessed using the PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013). The PCL-5 is a 20-item, self-report questionnaire that assesses symptoms of PTSD related to a stressful event. Symptoms are assessed on a Likert scale from 0 (Not at all) to 4 (Extremely) present within the past month. Due to time constraints related to research with an incarcerated sample, the PCL-5 was used as the primary measure of PTSD symptoms.
Trauma-related Approach-Avoidance Conflict Task (trAAC) – Version 2.
Similar to Study 1, the Congruent Phase corresponded to trials in which the option with the highest probability (80%) of a point reward was also the most likely to show a neutral image, and during the Conflict Phase, the option with the highest probability (80%) of a point reward was also the most likely to show a trauma-related image. There were 150 total trials, with 90 trials occurring during the Congruent Phase and 60 trials occurring during the Conflict Phase. The Congruent Phase was divided into three Blocks of 30 trials; the Conflict Phase was divided into two Blocks of 30 trials (Figure 5). Total points earned were tracked on the screen for participant reference as in Study 1. In addition, the total number of trauma-related images was displayed on the screen continuously. Outcome probabilities were adjusted in Study 2 such that one Conflict Phase was preceded by a change in threat probabilities (images), and one Conflict Phase was preceded by a change in reward probabilities (points). This change was made in order to ensure any differences in behavior were not due to impairments in reward probability learning, and instead reflect specific effect of the task Phases. Participants completed the trAAC task and self-report measures in one visit and were compensated for their time.
Data Analysis.
Consistent with Study 1, participant behavior was modeled using Linear Mixed Effects Models (LMEM) to investigate Hypothesis 3, regressing Block, Phase (Conflict = −1, Congruent = 1), Trial (z-scored), and PCL-5 Total Score (z-scored) on Total Points (scaled between 0 and 1), with Age and IQ added as covariates. Participants with a Trauma Total Score of 0 were excluded from all analyses. As in Study 1, Block and Trial were included in the model in order to control for the effects of learning throughout the task. Block was again coded separately for Congruent and Conflict Phases in order to account for the number of Blocks within each Phase. To model the linear effect of Block, earlier Blocks were coded as negative and later Blocks as positive. In contrast to Study 1, all Blocks consisted of 30 trials. Therefore, in the Conflict Phase (consisting of two Blocks), Block was coded −.5 and .5. In the Congruent Phase (consisting of three Blocks), Block was coded −1 0 1. We allowed the model to estimate a by-subject random intercept and a by-subject random slope for Phase, Block, Trial, and their interactions. Therefore, the final LMEM was defined as such:
To determine the effect of Trauma Total Score on task performance, a separate LMEM included all predictors from the above model, and also included Trauma Total Score as a covariate. This model did not allow for the interaction of Trauma Total Score and PCL-5 Total Score, as trauma exposure and PTSD symptoms are highly collinear.
Difference Scores were again calculated (see Study 1 Methods) to decompose the hypothesized PCL-5 Total*Phase interaction. An additional LMEM regressed Difference Score on PCL-5 Score, with Age and IQ added as covariates.
In order to investigate Hypothesis 4, we modeled an additional LMEM regressing Block, Phase, Trial and PCL-5 Avoidance Score on Total Points, with age and IQ added as covariates. A separate LMEM included all predictors as well as Trauma Total Score to account for the effect of trauma exposure. All variables were coded as in the primary LMEM.
Results
Mean choices for the Left and Right shapes are depicted in Supplemental Figure 3. Supporting Hypothesis 3, the LMEM demonstrated a significant Phase*PCL-5 interaction, β = .012, t(7482) = 2.13, p = .033, ƞp2 = .07, 95% CI [0, .22], and no higher order interactions; Figure 6. When including Total Trauma score as a covariate, there was no effect of Total Trauma Score on task performance, β = −.009, t(7481) = −1.7, p = .08, ƞp2 = .04, 95% CI [0, .16], and the Phase*PCL-5 interaction remained significant, β = .012, t(7481) = 2.13, p = .033, ƞp2 = .07, 95% CI [0, .22]. These results remained significant when controlling for a current diagnosis of Major Depression (see Supplemental Material).
Figure 6.
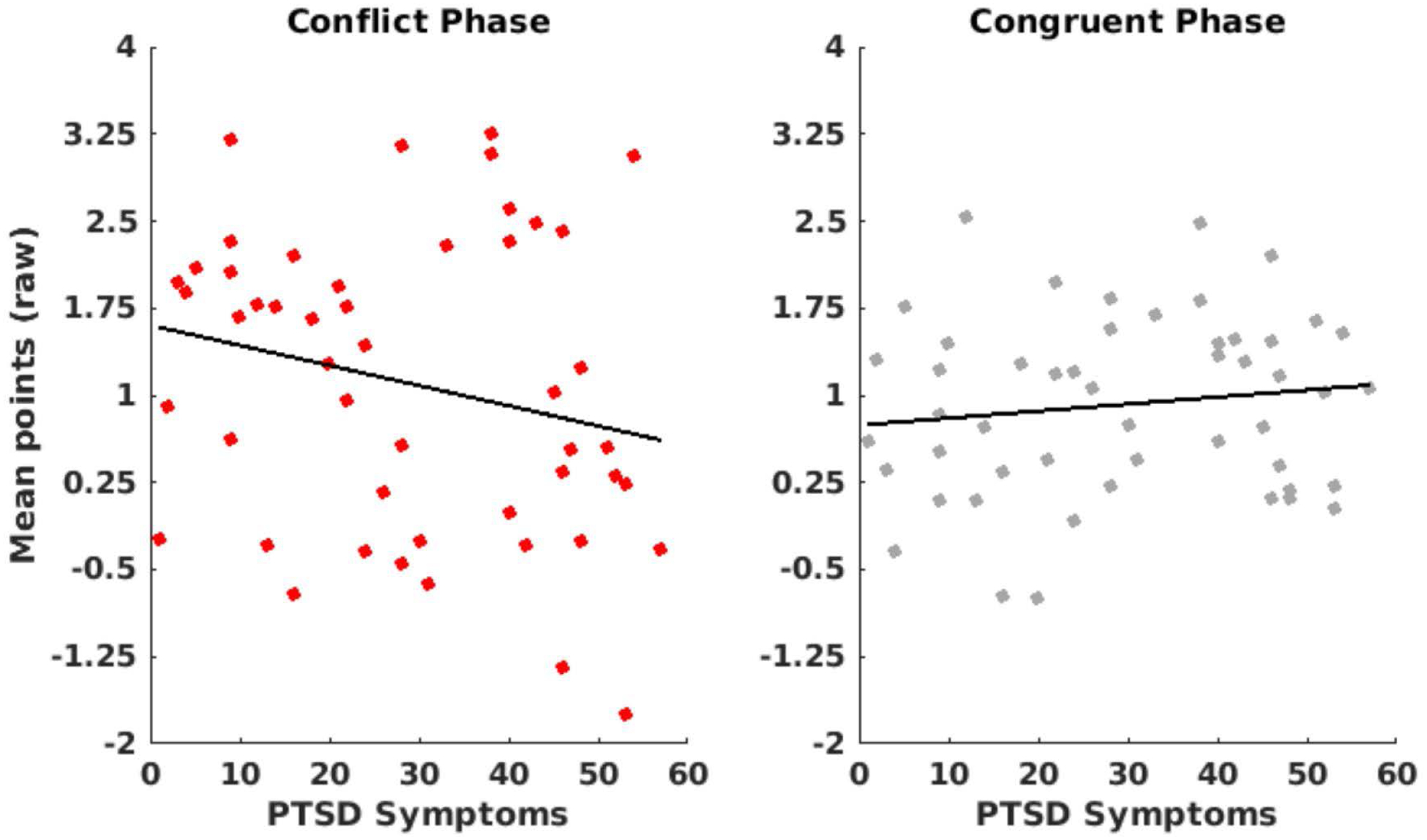
Depiction of PTSD Symptom*Phase interaction in Study 2. Points were scaled according to the number of trials within each Phase. 6a) The relationship between PTSD Symptoms and points gained during the Conflict Phase. Participants with higher PTSD symptoms gained fewer points compared to those with lower symptoms. This effect was not seen during the Congruent Phase, where PTSD Symptoms were not related to points gained (6b).
To decompose this interaction in accordance with Study 1, individual Difference Scores were again calculated and regressed onto PCL-5 Total Score, with Age and IQ added as covariates. These analyses demonstrated a significant effect of PCL-5 Total Score on Difference Score, with higher PCL-5 Total Scores resulting in more negative Difference Scores, β = −.02, t(46) = −2.40, p = .02, ƞp2 = .10, 95% CI [0, .27]; Supplemental Figure 4. These results support Hypothesis 3, indicating greater discrepancies in reward earning between task Phases were associated with higher PTSD symptoms. Therefore, as PTSD symptoms increased, the discrepancy in reward earning between the Congruent and Conflict Phase became greater, with decreased reward earning during the Conflict Phase. When controlling for Total Trauma Score, which was unrelated to the Difference Score, t(45)= −.75, p =.46, the relationship with the PCL remained similar, ƞp2 = .07, 95% CI [0, .22], but no longer met the p = .05 criterion for significance, t(45)=−1.89, p = .07.
In contrast with Hypothesis 4, predicting a specific effect of avoidance symptoms, and in line with Study 1, we observed no effect of PTSD avoidance symptoms on task performance. All results from the LMEM of participant trial-wise behavior are presented in Supplemental Table 2.
Discussion – Study 2
Study 2 investigated the effects of PTSD symptom severity on AAC during the trAAC task among incarcerated women with histories of trauma. Study 2 demonstrated support for Hypothesis 3 and exhibited an association between higher PTSD severity and decreased reward earning during Conflict Phase – when avoidance is maladaptive to task goals. This finding suggests a dimensional relationship between PTSD symptom severity and increased AAC in the presence of trauma-related stimuli that is not due to trauma exposure. While overall levels of PTSD symptoms were associated with AAC performance in this population, we observed no specific influence of PTSD Avoidance symptoms on task performance. Therefore, an individual’s behavior during conflict between approaching reward and avoiding trauma-related stimuli appears different than that same individual’s avoidance symptoms. For example, DSM-5 criteria require an individual “avoid external reminder of the stressful experience,” but does not measure whether that individual is willing to give up meaningful or rewarding activities in order to avoid those reminders. This suggests that AAC behavior may be a distinct construct from self-reported PTSD avoidance symptoms alone, and may represent a more consequential symptom of avoidance in those with severe PTSD.
Summary and Concluding Discussion
Overall, we found that participants with a current diagnosis of PTSD (Study 1) and higher PTSD symptoms (Study 2) demonstrated increased AAC during a reward learning task that also presented trauma-related stimuli. Both studies supported greater AAC in PTSD, such that participants with PTSD displayed increased conflict between approach and avoidance during the trAAC task. Across both studies, PTSD participants (diagnosis or higher symptoms) were most sensitive to differences in task contingencies when avoidance was rewarded versus conflicted with threat. However, sensitivity to contingencies presented differently across PTSD participant samples. In Study 1, PTSD was associated with increased AAC in Block 2 of the Conflict Phase, while Study 2 revealed increased AAC across all Blocks.
One explanation of this Block specificity seen in Study 1 but not Study 2 could be due to the structure of the task in Study 1, in which each Block of the Conflict Phase is preceded by a change in reward probability. Participants with PTSD are shown to value reward less than healthy subjects, therefore changes in the reward structure may be less salient to those with PTSD, exacerbated by the presence of trauma-related images (Hopper et al., 2008). In this way, the behavior change necessary to gain points after a switch from a Congruent to a Conflict Phase, may be less “worthwhile” for those with PTSD, because it would require choosing an option with a high likelihood of presenting a trauma-related image. In contrast, the change from Block 1 of the Conflict Phase to Block 2 of the Congruent Phase, where the rewarding option switches from being associated with trauma-related images to the “safe” option, would not require an explicit behavior change. Instead, individuals continue choosing the same shape, which becomes “safe” and rewarding after the threat structure change. This change may alleviate the conflict of the previous block, and explain why individuals with PTSD showed impaired AAC only during Block 2 of the trAAC task.
In contrast to Study 1, the increased AAC among individuals with higher PTSD symptoms in Study 2 was not restricted to later Blocks of the task. The lack of Block specificity in Study 2 could be due to the lower overall PTSD symptoms and greater range of symptoms among participants in Study 2, who, in contrast to Study 1, did not necessarily meet for a current diagnosis. While the results of Study 1 could not determine whether the Block specificity was due to the lower valuation of reward by those with PTSD, in Study 2, one Block of the Conflict Phase was preceded by a change in threat structure, therefore it is unlikely that the relationship between PTSD symptoms and task performance during the Conflict Phase was solely due to the change in reward structure.
While it is important to note the discrepancies between the results of the two studies, the implication of these differing results is also notable. The results of Study 1 could have been due to drastic group differences in trauma exposure, with healthy subjects experiencing no traumatic events. Because of this, the results of Study 2 are particularly important. Within a trauma-exposed sample, PTSD was related only to an impairment during the Conflict Phase, with no relationship during the Congruent Phase, which remained true when controlling for trauma exposure. This suggests that within traumatized populations (Study 1 PTSD group, Study 2), PTSD symptoms may specifically impair participants’ ability to reconcile approach and avoidance conflict situations involving trauma-related stimuli, leading to decreased performance when this conflict is present. In addition, results from the Congruent Phase of both Study 1 and Study 2 suggest reward sensitivity is intact among individuals with high symptoms of PTSD, which could be an essential component when considering AAC in the context of treatment.
Exposure therapy focuses on optimizing inhibitory learning to reduce maladaptive avoidance behavior in response to fear (Craske et al., 2008). The goal is to develop new secondary learning regarding trauma-related stimuli (e.g., reminders of trauma are different than the trauma itself). Craske and colleagues distinguish between fear reduction and fear toleration – noting the importance of feeling fear (Craske et al., 2008). This distinction is also highlighted in mindfulness- and acceptance-based approaches to treatment of trauma-related disorders: acceptance of painful internal experiences when in service of a valued life (Orsillo & Batten, 2005). Development of a connection with valued life directions may increase the reward’s value, even in the presence of the trauma-related stimuli’s aversive quality. Consideration of both the appetitive value of the point reward and the aversive value of the trauma-related image maps directly onto clinical implications for treatment, as a provider may consider increasing connection with reward in order to decrease avoidance of trauma-related stimuli, especially in exposure-based treatment settings.
One study of social anxiety disorder indicated that individual differences in AAC sensitivity may inform identification and choice of exposure exercises based on reward value (Pittig et al., 2015). In comparison, individuals with PTSD may avoid social gatherings, thus reducing social support and opportunity for positive interpersonal experiences, however new learning associated with positive social experiences may be particularly important in the aftermath of IPT. For those with high reward sensitivity in a behavioral task such as the trAAC task, attending to rewarding aspects of the social gathering may encourage persistent approach behavior and reduced avoidance, thereby increasing efficacy of exposure therapy. Behavior during approach-avoidance conflict can also inform therapy by characterizing an individual’s cognitive flexibility, or ability to shift from avoidant to approach tendencies when faced with trauma-related stimuli. Cognitive inflexibility is associated with increased symptom severity and predicts poorer treatment outcomes; therefore, a measure of this rigidity could be used to inform treatment progress in real time (Joseph & Gray, 2011; Keith et al., 2015). Cognitive flexibility has been shown to significantly predict posttraumatic growth and optimistic expectations (Keith et al., 2015), and trauma-focused therapies can lead to a shift in flexibility by increasing willingness to approach previously avoided stimuli (Sobel et al., 2009). Future studies should manipulate the magnitude of reward to identify the threshold and context in which avoidance is overruled by approach, as has been done in arachnophobia (Pittig, Hengen, Bublatzky, & Alpers, 2018). A task such as the trAAC task could utilize individual differences in AAC resolution to target aspects of already effective therapies, improving outcomes and reducing symptom maintenance.
The results present an argument for more dedicated research on the interaction between threat and reward processing for individuals with PTSD. Physiological hyperarousal measures may benefit future AAC research. Past research indicates that individuals with PTSD exhibit heightened heart rate and skin conductance response (SCR) towards threatening stimuli (Michopoulos, Norrholm, & Jovanovic, 2015). Similarly, participants with higher social anxiety and higher SCR preferentially avoided negatively-valenced social stimuli (Pittig, Pawlikowski, Craske, & Alpers, 2014). In addition to examining the role of autonomic arousal in AAC behaviors, replications of the current findings are necessary to corroborate the effects observed, particularly with regard to discrepancies between the two studies. For instance, a self-report measure of PTSD symptom severity replaced the CAPS-5 in Study 2 due to time constraints, which led to differing PTSD assessments. Additionally, a questionnaire version of the validated NSA was used in Study 2, in contrast with the in-person interview used in Study 1. While this was necessary given the functional limitations of completing research in an incarcerated population, future research should focus on validated clinical interviews to assess trauma exposure. Depressive symptoms are also known to influence reward processing, which could contribute to deficits in approach behavior seen in those with PTSD. While current depressive symptoms were added as a covariate in follow up analyses in Study 1 (see Supplemental Material), and a current diagnosis of depression did not influence the results of Study 2, continuous symptoms were not collected at the time of participation in Study 2. Therefore, future research should examine more closely the influence of depressive symptoms on AAC, especially among those with PTSD. Additional replications utilizing both continuous self-report measures and clinician determined diagnoses can help distinguish the unique effects of overall PTSD severity. While the small size of the healthy comparison group in Study 1 is a notable limitation, comparison to normative healthy samples is important to contextualize the findings in terms of diagnostic characteristics and symptom severity. Future studies should also consider approach-avoidance conflict behavior among those with PTSD symptoms when the aversive stimulus is not trauma-related, and should investigate whether the increased AAC shown in these two studies is limited to trauma-related contexts, or if individuals with PTSD are impaired in AAC resolution across contexts.
The two studies highlight a deficit in the conceptualization of PTSD maintenance via avoidance-based mechanisms, and future investigations are necessary to better understand the individual differences in AAC behavior. The study proposes a new trAAC task that may aid in the identification of ineffective avoidance behavior among trauma-exposed samples, and such an assessment may prove useful in further characterizing trauma-related disorders as rooted in avoidance. The clinical implications of a behavioral task measuring avoidance would likely be far-reaching.
Supplementary Material
Acknowledgments
Portions of this research were funded by the NIMH (MH108753, MH109329) and NIAAA (AA026290). Portions of this data were presented at the Society for Mathematical Biology, the Society of Biological Psychiatry, and the Health Emotions Research Symposium. Study approval was granted by the University of Wisconsin – Madison Institutional Review Board (#2016-1313, #2017-0736, #2014-0350).
References
- Aupperle RL, Sullivan S, Melrose AJ, Paulus MP, & Stein MB (2011). A reverse translational approach to quantify approach-avoidance conflict in humans. Behavioural Brain Research, 225(2), 455–463. 10.1016/j.bbr.2011.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, Shahly V, Stein DJ, Petukhova M, Hill E, Alonso J, Atwoli L, Bunting B, Bruffaerts R, Caldas-de-Almeida JM, de Girolamo G, Florescu S, Gureje O, Huang Y, … Koenen KC (2016). The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327–343. 10.1017/S0033291715001981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden MT, Bonn-Miller MO, Vujanovic AA, & Drescher KD (2012). A Prospective Investigation of Changes in Avoidant and Active Coping and Posttraumatic Stress Disorder Symptoms among Military Veteran. Journal of Psychopathology and Behavioral Assessment, 34(4), 433–439. 10.1007/s10862-012-9293-6 [DOI] [Google Scholar]
- Brownell R (2000). Receptive one-word picture vocabulary test: Manual. Academic Therapy Publications. [Google Scholar]
- Bublatzky F, Alpers GW, & Pittig A (2017). From avoidance to approach: The influence of threat-of-shock on reward-based decision making. Behaviour Research and Therapy, 96, 47–56. 10.1016/j.brat.2017.01.003 [DOI] [PubMed] [Google Scholar]
- Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, & Baker A (2008). Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy, 46(1), 5–27. 10.1016/j.brat.2007.10.003 [DOI] [PubMed] [Google Scholar]
- Fazel S, & Baillargeon J (2011). The health of prisoners. The Lancet, 377(9769), 956–965. 10.1016/S0140-6736(10)61053-7 [DOI] [PubMed] [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, & Street GP (1999). A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology, 67(2), 194–200. http://dx.doi.org.ezproxy.library.wisc.edu/10.1037/0022-006X.67.2.194 [DOI] [PubMed] [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, & Murdock TB (1991). Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive behavioral procedures and counseling. Journal of Consulting and Clinical Psychology, 59(5), 715–723. http://dx.doi.org.ezproxy.library.wisc.edu/10.1037//0022-006X.59.5.715 [DOI] [PubMed] [Google Scholar]
- Hayes SC (1976). The role of approach contingencies in phobic behavior. Behavior Therapy, 7(1), 28–36. 10.1016/S0005-7894(76)80216-X [DOI] [Google Scholar]
- Hopper JW, Pitman RK, Su Z, Heyman GM, Lasko NB, Macklin ML, Orr SP, Lukas SE, & Elman I (2008). Probing reward function in posttraumatic stress disorder: Expectancy and satisfaction with monetary gains and losses. Journal of Psychiatric Research, 42(10), 802–807. 10.1016/j.jpsychires.2007.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph JS, & Gray MJ (2011). The Utility of Measuring Explanatory Flexibility in PTSD Research. Cognitive Therapy and Research, 35(4), 372–380. 10.1007/s10608-010-9301-7 [DOI] [Google Scholar]
- Karlsson ME, & Zielinski MJ (2018). Sexual Victimization and Mental Illness Prevalence Rates Among Incarcerated Women: A Literature Review. Trauma, Violence, & Abuse, 1524838018767933. 10.1177/1524838018767933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keith J, Velezmoro R, & O’Brien C (2015). Correlates of cognitive flexibility in veterans seeking treatment for posttraumatic stress disorder. The Journal of Nervous and Mental Disease, 203(4), 287–293. 10.1097/NMD.0000000000000280 [DOI] [PubMed] [Google Scholar]
- Kessler RC (2000). Posttraumatic stress disorder: The burden to the individual and to society. The Journal of Clinical Psychiatry, 61 Suppl 5, 4–12; discussion 13–14. [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C., Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, Degenhardt L, de Girolamo G, Dinolova RV, Ferry F, Florescu S, Gureje O, Haro JM, Huang Y, Karam EG, Kawakami N, Lee S, Lepine J-P, Levinson D, … Koenen KC (2017). Trauma and PTSD in the WHO World Mental Health Surveys. European Journal of Psychotraumatology, 8(sup5). 10.1080/20008198.2017.1353383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, & Schnurr PP (2000). Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology, 68(1), 19–30. [DOI] [PubMed] [Google Scholar]
- Kirlic N, Young J, & Aupperle RL (2017). Animal to human translational paradigms relevant for approach avoidance conflict decision making. Behaviour Research and Therapy, 96, 14–29. 10.1016/j.brat.2017.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumpula MJ, Orcutt HK, Bardeen JR, & Varkovitzky RL (2011). Peritraumatic dissociation and experiential avoidance as prospective predictors of posttraumatic stress symptoms. Journal of Abnormal Psychology, 120(3), 617–627. 10.1037/a0023927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang PJ, Bradley MM, & Cuthbert BN (1997). International affective picture system (IAPS): Technical manual and affective ratings. NIMH Center for the Study of Emotion and Attention, 1, 39–58. [Google Scholar]
- Marks I. fM., & Nesse RM (1994). Fear and fitness: An evolutionary analysis of anxiety disorders. Ethology and Sociobiology, 15(5–6), 247–261. 10.1016/0162-3095(94)90002-7 [DOI] [Google Scholar]
- Marx BP, & Sloan DM (2005). Peritraumatic dissociation and experiential avoidance as predictors of posttraumatic stress symptomatology. Behaviour Research and Therapy, 43(5), 569–583. 10.1016/j.brat.2004.04.004 [DOI] [PubMed] [Google Scholar]
- Myers CE, Moustafa AA, Sheynin J, VanMeenen KM, Gilbertson MW, Orr SP, Beck KD, Pang KCH, & Servatius RJ (2013). Learning to Obtain Reward, but Not Avoid Punishment, Is Affected by Presence of PTSD Symptoms in Male Veterans: Empirical Data and Computational Model. PLOS ONE, 8(8), e72508 10.1371/journal.pone.0072508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nawijn L, van Zuiden M, Frijling JL, Koch SBJ, Veltman DJ, & Olff M (2015). Reward functioning in PTSD: A systematic review exploring the mechanisms underlying anhedonia. Neuroscience and Biobehavioral Reviews, 51, 189–204. 10.1016/j.neubiorev.2015.01.019 [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, & Tolin DF (2007). Quality of life in the anxiety disorders: A meta-analytic review. Clinical Psychology Review, 27(5), 572–581. 10.1016/j.cpr.2007.01.015 [DOI] [PubMed] [Google Scholar]
- Orsillo SM, & Batten SV (2005). Acceptance and commitment therapy in the treatment of posttraumatic stress disorder. Behavior Modification, 29(1), 95–129. 10.1177/0145445504270876 [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, & Grant BF (2011). Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25(3), 456–465. 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittig A, Alpers GW, Niles AN, & Craske MG (2015). Avoidant decision-making in social anxiety disorder: A laboratory task linked to in vivo anxiety and treatment outcome. Behaviour Research and Therapy, 73, 96–103. 10.1016/j.brat.2015.08.003 [DOI] [PubMed] [Google Scholar]
- Pittig A, Brand M, Pawlikowski M, & Alpers GW (2014). The cost of fear: Avoidant decision making in a spider gambling task. Journal of Anxiety Disorders, 28(3), 326–334. 10.1016/j.janxdis.2014.03.001 [DOI] [PubMed] [Google Scholar]
- Pittig A, Pawlikowski M, Craske MG, & Alpers GW (2014). Avoidant decision making in social anxiety: The interaction of angry faces and emotional responses. Frontiers in Psychology, 5 10.3389/fpsyg.2014.01050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poister Tusher C, & Cook SL (2010). Comparing Revictimization in Two Groups of Marginalized Women. Journal of Interpersonal Violence, 25(10), 1893–1911. 10.1177/0886260509354513 [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, & Best CL (1993). Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology, 61(6), 984–991. [DOI] [PubMed] [Google Scholar]
- Sobel AA, Resick PA, & Rabalais AE (2009). The effect of cognitive processing therapy on cognitions: Impact statement coding. Journal of Traumatic Stress, 22(3), 205–211. 10.1002/jts.20408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MB, & Paulus MP (2009). Imbalance of Approach and Avoidance: The Yin and Yang of Anxiety Disorders. Biological Psychiatry, 66(12), 1072–1074. 10.1016/j.biopsych.2009.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, Keane TM, & Marx BP (2018). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383–395. 10.1037/pas0000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5).
- Wechsler D (1981). Wechsler Adult Intelligence Scale-Revised. In Psychological Corporation; New York, NY. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


