Abstract
It has been well known for decades that prone positioning (PP) improves oxygenation. However, it has gained widespread acceptance only in the last few years since studies have shown significant survival benefit. Many centers have established prone ventilation in their treatment algorithm for mechanically ventilated patients with severe acute respiratory distress syndrome (ARDS). Physiologically, PP should also benefit awake, non-intubated patients with acute hypoxemic respiratory failure. However, proning in non-intubated (PINI) patients did not gain any momentum until a few months ago when the Coronavirus disease 2019 (COVID-19) pandemic surged. A large number of sick patients overwhelmed the health care system, and many centers faced a dearth of ventilators. In addition, outcomes of patients placed on mechanical ventilation because of COVID-19 infection have been highly variable and often dismal. Hence, increased focus has shifted to using various strategies to prevent intubation, such as PINI. There is accumulating evidence that PINI is a low-risk intervention that can be performed even outside intensive care unit with minimal assistance and may prevent intubation in certain patients with ARDS. It can also be performed safely at smaller centers and, therefore, may reduce the patient transfer to larger institutions that are overwhelmed in the current crisis. We present a case series of 2 patients with acute hypoxemic respiratory failure who experienced significant improvements in oxygenation with PP. In addition, the physiology of PP is described, and concerns such as proning in obese and patient’s anxiety are addressed; an educational pamphlet that may be useful for both patients and health care providers is provided.
Keywords: proning, prone positioning, proning in non-intubated, awake proning, prone positioning in obese, shape matching
Background
It has been known for decades that prone positioning (PP) in mechanically ventilated patients with moderate to severe acute respiratory distress syndrome (ARDS) improves oxygenation. However, it has gained widespread acceptance only in the last few years, after publication of meta-analyses and the PRO-SEVA trial showing significant survival benefit.1,2 Since then, many centers have started using PP in their treatment algorithm for mechanically ventilated patients with severe ARDS. Physiologically, PP should also benefit awake, non-intubated patients with ARDS. However, proning in non-intubated (PINI) patients was limited in the medical literature and practice until the Coronavirus disease 2019 (COVID-19) pandemic surged. Health care systems have been overwhelmed with large numbers of intubated patients and the lack of sufficient medical personnel and supplies. In addition, outcomes of patients placed on mechanical ventilation because of COVID-19 infection have been highly variable and sometimes dismal.3 Hence, there has been an increased focus on strategies to safely prevent invasive mechanical ventilation, such as PINI.
This article will discuss the successful use of PINI in 2 patients, review the physiology of prone ventilation, review the published literature, and discuss its bedside implementation.
Patient 1
A 42-year-old-male with no major past medical history was admitted to the hospital for 1 week of fever, sore throat, and body aches. Vital signs in the emergency department (ED) were temperature of 100.1 F, pulse rate of 98/min, respiratory rate of 22/min, and blood pressure of 132/78 mm Hg. Pulse oximetry (SpO2) on room air was 88%. On examination, he appeared mildly tachypneic but was able to speak in full sentences. Lung auscultation revealed scattered crackles bilaterally. The rest of the examination was unremarkable. Initial lab testing revealed normal complete blood count (WBC count of 4.5 K/mL-80% neutrophils, 9.8% lymphocytes), and serum chemistries were significant for mild transaminitis. C-reactive protein, ferritin, and D-dimers were significantly elevated, while procalcitonin level was low. Chest imaging showed bilateral patchy infiltrates. His test for COVID-19 resulted positive. He was placed on 2 L/min supplemental oxygen through nasal cannula (NC) to maintain SpO2 >90%. Treatment with hydroxychloroquine and azithromycin was started but his oxygen requirements steadily increased, necessitating transfer to the medical intensive care unit (ICU), where he was placed on high-flow nasal cannula (HFNC) at FiO2 of 0.5 and flow of 30 L/min. His hypoxemia continued to worsen over the next 2 days with FiO2 requirement reaching 0.7. While his oxygen requirements continued to increase his apparent work of breathing remained minimal and he was able to carry on a full conversation.
Prone positioning was suggested due to severe hypoxemia in the absence of significantly observed work of breathing; however, its success was limited due to anxiety and resultant inability to reach a comfortable position. Alprazolam and Hydroxyzine were started with a positive response, and the next day, the patient was better able to tolerate PP. With continued encouragement from the health care team to lie on his abdomen along with a written education pamphlet, the patient was successfully able to prone himself for 2 to 3 hours at a time. Within few hours of proning, his SpO2 values improved from 92% to 98%, and FiO2 was titrated down to 0.5. With continued positive reinforcement, he continued to prone himself regularly and was able to wean down to 3 L/min NC by day 3 of proning. Figure 1 shows the results of PP on oxygen requirements. It took him a few additional days to be on room air, after which he was successfully discharged home.
Figure 1.
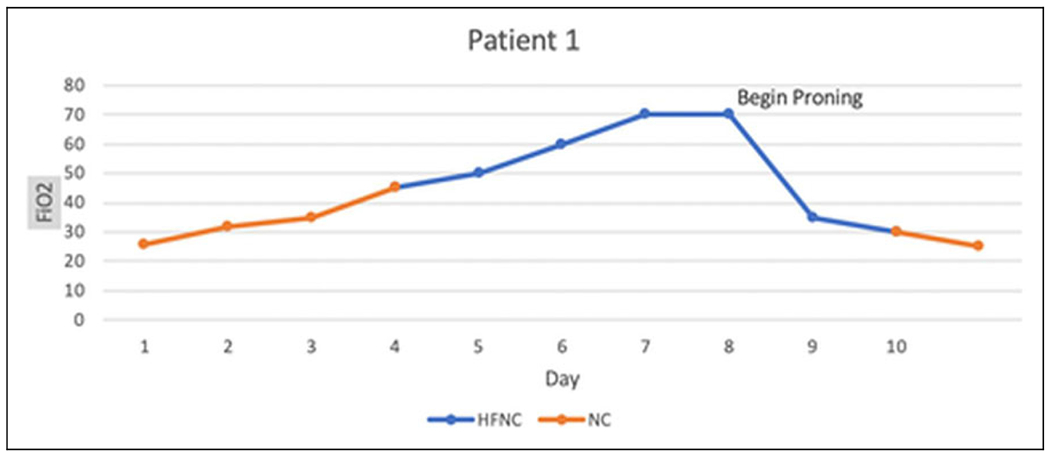
FiO2 (y-axis) on different days (x-axis). Orange line shows patient on NC. Blue line shows patient on HFNC. L/min on NC has been converted to approximate FiO2. HFNC indicates high-flow nasal cannula; NC, nasal cannula.
Patient 2
A 35-year-old male with a past medical history of mild persistent asthma, morbid obesity (body mass index [BMI] 65 kg/m2) and obstructive sleep apnea came to the ED with complaints of worsening dyspnea over the last few days. He denied fever, chills, sore throat, and body aches while endorsing a productive cough with yellow phlegm and increased wheezing. Initial vital signs were temperature of 98.9 F, pulse rate of 122/min, respiratory rate of 32/min, blood pressure of 144/78 mm Hg, and SpO2 of 80% on room air. On examination, he was morbidly obese, had accessory respiratory muscle use, diffuse wheezing on lung auscultation, and +1 leg edema bilaterally. His Mallampati score was 3. Chest X-ray in the ED showed increased pulmonary vascular congestion with no obvious infiltrates. Initial lab testing showed leukocytosis of 23K/mL (81% neutrophils). While his initial presentation was more consistent with an asthma exacerbation and volume overload, he was considered a person under investigation for COVID-19. With worsening respiratory status, he was intubated and admitted to the ICU. The initial diagnosis was acute respiratory failure with hypoxemia secondary to asthma exacerbation, pulmonary edema, and possible COVID-19 infection. He received intravenous steroids, diuretics, and nebulized bronchodilators using a closed circuit with viral filter. Initial ventilator settings were tidal volume of 420 mL (6 mL/kg) and a PEEP of 14 cm H2O, with FiO2 fluctuating between 0.6 and 0.7. Two COVID-19 tests resulted negative over the next 2 days. Renal replacement therapy was initiated by day 4 of hospital stay for acute kidney injury and volume removal. After a successful spontaneous breathing trial and a subsequent clear chest radiograph, he was extubated on day 7 to 3 L/min NC. However, he decompensated within hours of extubation and developed severe hypoxemia without clinical evidence of an infection. Respiratory support with high flow NC alternating with NIV was started and he met the criteria for severe ARDS with P/F ratio of 80. Chest X-ray showed diffuse bilateral infiltrates which were not present on imaging that morning. With acute bilateral airspace disease after extubation in a morbidly obese patient, the diagnosis of negative pressure pulmonary edema was considered (cardiac function was normal on echocardiogram). Daily hemodialysis with aggressive fluid removal was done without much improvement in oxygenation and his required FiO2 remained at 0.8. At that time, he was asked to prone himself but could not tolerate for more than 5 minutes due to anxiety and discomfort. After initiation of low dose alprazolam along with continued reinforcement and education about proning, the patient successfully tolerated PP for 2 hours at a time the following day. Within 1 hour of proning, there was notable improvement, with FiO2 requirements titrated down to 0.4; this improvement persisted even when returning to supine position. He continued to prone himself for 2 to 3 hours at a time, a minimum of 3 times per day. Within the next 48 hours, he was weaned to NC at 3 L/min. Figure 2 shows the effect of prone ventilation on oxygen requirements. Over the next few days, hemodialysis and supplemental oxygen were discontinued and he was discharged with his baseline asthma medications.
Figure 2.
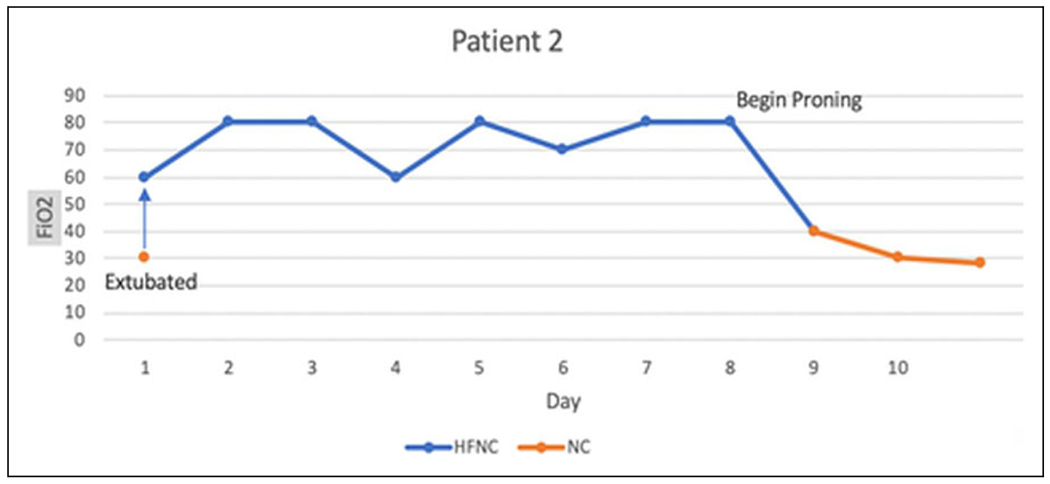
FiO2 (y-axis) on different days (x-axis). Orange line shows patient on NC. Blue line shows patient on HFNC. Blue arrow shows transition from NC to HFNC. HFNC indicates high-flow nasal cannula; NC, nasal cannula.
Discussion
Prone positioning helps improve pulmonary physiology and oxygenation through different mechanisms. These include:
Transpulmonary pressure (TPP) gradient and blood flow:
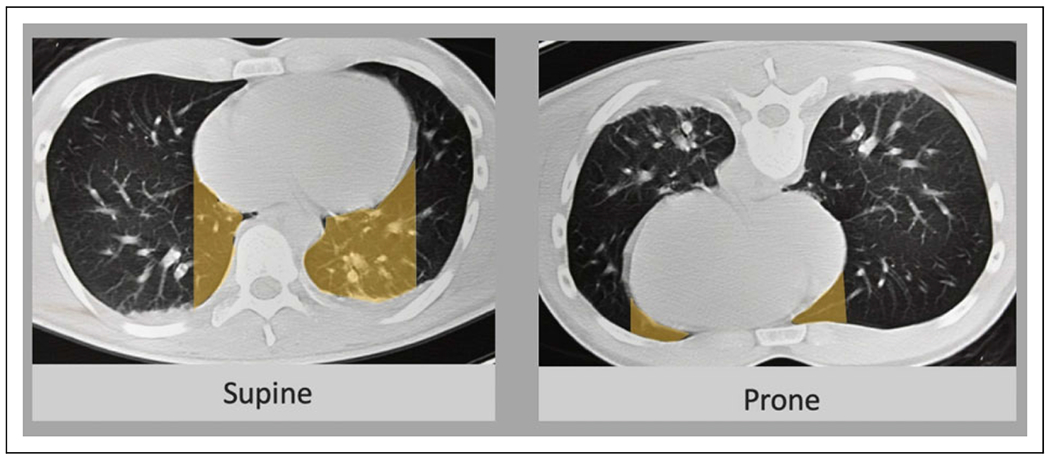
Transpulmonary pressure (airway opening [mouth]-pleural) is a key determinant of alveolar recruitment and decruitment. In supine position, pleural pressure is lowest (most negative) in the ventral lung and highest (least negative) in the dorsal lung due to the effect of gravity. As gravity has minimal effects on the airway opening pressure, TPP is higher in the ventral lung as compared to the dorsal.4 In a patient with ARDS, surfactant loss/dysfunction leads to alveolar collapse, making the ventral to dorsal TPP gradient critically important. Ventral lung is at risk of overdistention, while alveolar decruitment (atelectasis) occurs predominantly in the dorsal lung (Figure 3).4
Figure 3.
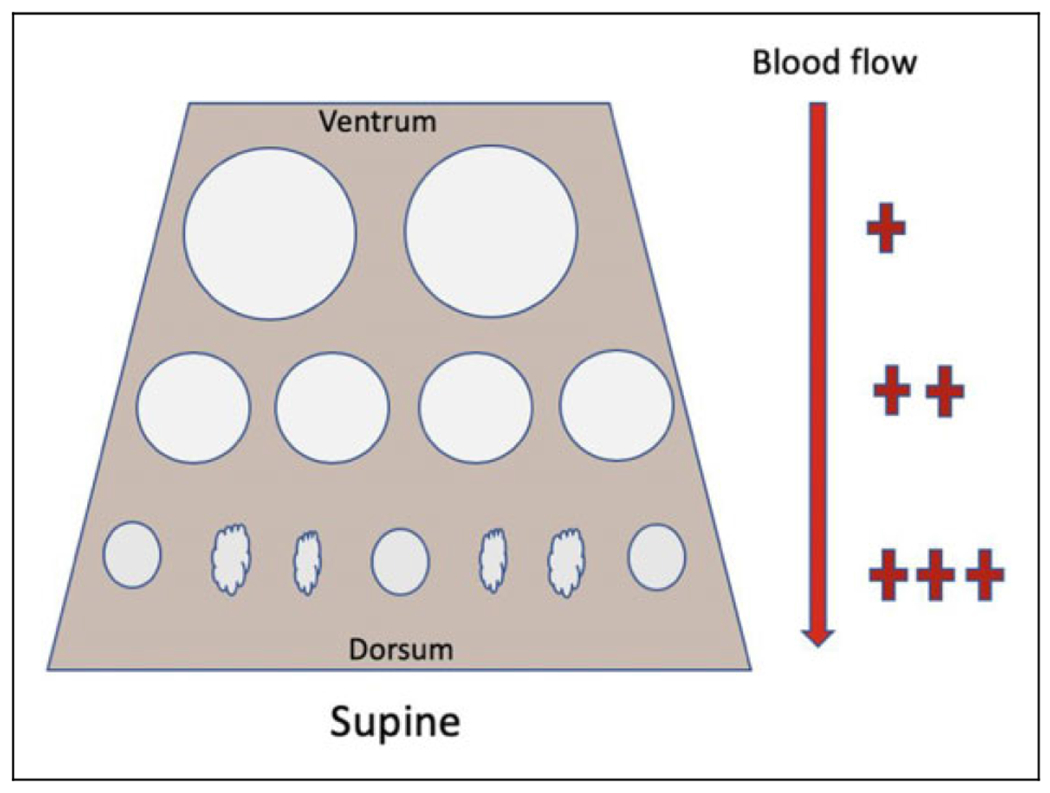
Alveolar collapse at bases due to lower TPP. Alveolar overdistention was seen in the ventral areas due to higher TPP.
Proning helps alveolar recruitment in the dorsal lung (now nondependent) by increasing the TPP (due to local drop in pleural pressure). Once recruited, the pressure required to maintain alveolar patency is typically lower than that required to open alveoli, such that alveolar recruitment can be maintained even with minimal or no PEEP; hence, the benefits may persist even after the patient returns to the supine position. Proning also reduces overdistention of the ventral lung (now dependent) due to drop in the TPP (because local pleural pressure increases; Figure 4).4 These physiological changes make ventilation more homogeneous throughout the lung (Figure 4). On the other hand, the blood flow pattern is relatively unaffected with change from supine to prone position. The dorsal region (now recruited) of the lung still receives majority of the blood flow, leading to better V/Q relationships (Figure 4), and improved oxygenation.4
Figure 4.
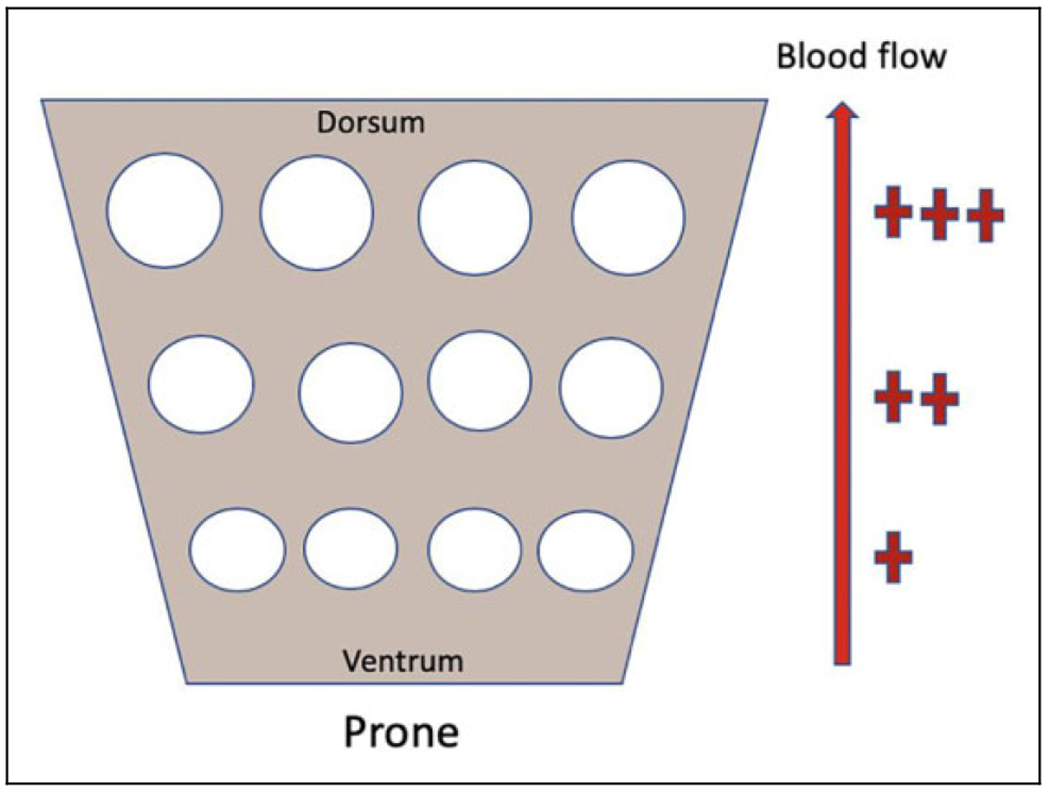
Recruitment of alveoli in dorsal lung. Less overdistention in the ventral lung. Improved V/Q matching as blood flow pattern remains unaffected.
Reduced lung compression:
In the supine position, heart and the abdominal organs exert a mass effect on the lungs. Abdominal organs push the diaphragm upwards, and this is exacerbated by the loss of diaphragmatic tone due to sedation and/or paralysis in intubated patients. Effects are compounded in morbidly obese patients due to excess tissue in the abdomen and chest wall. In prone position, the heart becomes dependent, potentially decreasing lung compression (Figure 5).5 Furthermore, the diaphragm is displaced caudally (especially in obese patients), decreasing compression of the lung.
Figure 5.
Comparison of lung compression by the heart in supine and prone positions (Adapted from the efficacy of prone position in acute respiratory distress syndrome patients: a pathophysiology-based review. V Koulouras, World J Crit Care Med. 2016;5(2): Page 126).
Shape matching:
Due to shape difference between the chest cavity (cylindrical) and the lung (conical), the ventral lung (smaller part of cone) expands to fit in the wider chest cavity leading to greater alveolar distention, and the dorsal lung (larger part of cone) gets compressed leading to smaller alveolar units.5 This is referred to as the shape matching effect. In supine position, effects of shape matching and gravity add up, promoting decruitment in the dorsal and overdistention in the ventral lungs (Figure 6).5
Figure 6.
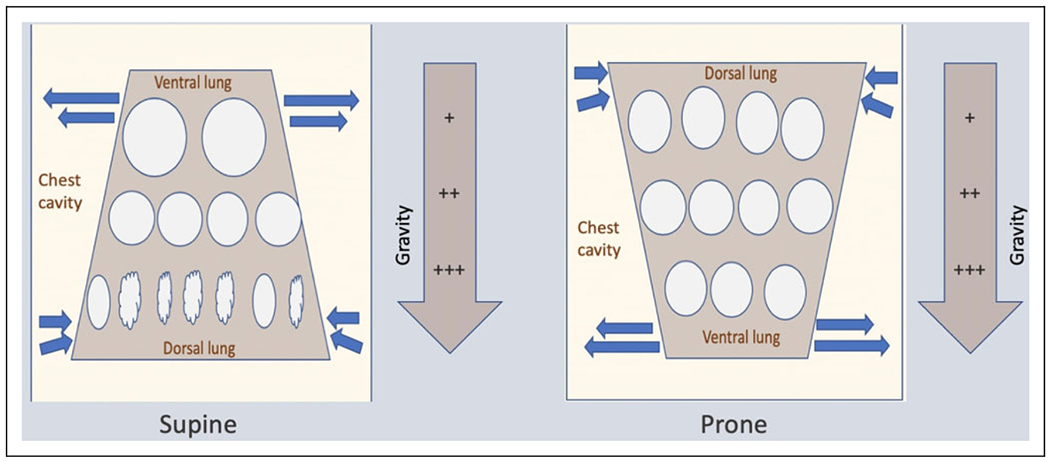
Blue arrows show the effect of shape matching. Supine position: Dorsal lung atelectasis due to combined effects of shape matching and gravity. Ventral lung-overdistention. Prone position: Ventral lung compression due to gravity is offset by expansion due to shape matching. Dorsal lung overdistention is prevented by compression due to shape matching.
Shape matching is unaffected with change from supine to prone position, as the anatomy of chest wall and lungs does not change. Thus, in prone position, the compressive effect of gravity on the ventral lung (now dependent) is offset by regional expansion due to shape matching; overdistention of the dorsal lung (now non-dependent) is prevented due to compressive effects of shape matching (Figure 6). This allows more homogenous ventilation.5,6
Improved secretion clearance:
Dorsal-to-ventral orientation of the major airways may allow more efficient drainage of secretions7 and has also shown to reduce the incidence of ventilator-associated pneumonia.8
Proning in Non-Intubated: Review of literature
Even though most published data on PP involves patients on mechanical ventilation, PP should also have similar effects on respiratory physiology in non-intubated patients. Thus, the changes in TPP, shape matching, alveolar recruitment, homogeneous ventilation, and better V/Q matching should also be seen in non-intubated patients who have acute hypoxemic respiratory failure. Surprisingly, there are very few studies published in the literature on PINI. Scaravilli et al retrospectively analyzed data on 15 non-intubated patients with acute hypoxemic respiratory failure who underwent PP and observed significant improvements in oxygenation.9 In a prospective cohort study, Ding et al used PP for 2 hours twice daily along with HFNC or NIV for 20 patients with moderate to severe ARDS. They observed an average increase in PaO2/FiO2 ratio by 25 to 35 mm Hg compared with the prior HFNC or NIV, and a decrease in the need for intubation in patients with moderate ARDS.10 Most recently, Caputo et al observed improvement in SpO2 levels within as little as 5 minutes time using PP in the emergency room for hypoxemic patients suspected of having COVID-19.11 Thus, based on the results of available data in proning in non-intubated as well as extrapolation from studies done in intubated patients, PINI can improve oxygenation and prevent intubation in certain patients with ARDS. Very likely, more studies will be published in the near future because of increasing utilization in the current times of COVID-19 pandemic.
Proning in Non-Intubated: Bedside Application
Based on the available evidence, PINI can be used in patients with varying severity of ARDS. As PINI is a low-risk intervention, it is also being considered for the hypoxemic patients who are not sick enough to meet the established ARDS criteria, as done by Caputo et al.11 Many institutions have developed or adopted protocols where hypoxemic patients requiring only NC are assessed for proning (Table 1).12,13 This is being done safely on medical floors outside of the ICU. Patients still need to be assessed frequently, as proning should not be considered a replacement therapy for intubation or transfer to ICU.13 The majority of published literature supports early proning, and some even begin in the ER as in the study done by Caputo et al11; however, if not done early, it should not deter providers from attempting later in the hospitalization. Both of our patients were proned relatively later in their hospital stay and still experienced significant benefits.
Table 1.
PINI is being considered in settings such as.
| • Adults with acute hypoxemia due to COVID-19 |
| • O2 requirements > 2 L/min to maintain SpO2 ≥ 92% |
| • No major distress |
| • Patient able to communicate, follow instructions, and manage any displaced cannula or mask |
| • Patient able to prone and supine himself/ herself with minimal assistance. |
Abbreviation: SpO2, pulse oximetry.
Unlike prone ventilation in intubated and sedated patients, where the health care team dictates when and for how long to continue the PP, the duration of PINI is dependent on patient’s tolerance and comfort. In review of numerous protocols,12–14 centers are encouraging patients to prone themselves for a wide range of 30 minutes to 8 hours, 2 to 3 times per day. As observed in studies, PP can be safely done on NC, HFNC, or even NIV as long as the patient is able to participate and tolerate.10,11 However, for a patient in obvious distress, PINI should be deferred and more immediate forms of treatment (intubation, NIV, or HFNC) should be considered. Apart from obvious distress, there are certain other conditions (Table 2), where PP should be avoided.15
Table 2.
PINI should be avoided in the following conditions.
| • Facial/neck trauma |
| • Spinal instability |
| • Recent sternotomy |
| • Significant hemoptysis |
| • Significant hemodynamic instability, or high risk of requiring CPR or defibrillation |
| • Pregnancy |
Current evidence suggests PP is significantly underutilized; however, the majority of available discussions is limited to intubated patients.16,17 In those patients, clinicians and nurses have concerns about hemodynamic instability, risk of pressure injuries, accidental tube displacement/obstruction, and technical challenges of turning the patient, despite studies suggesting that PP may be performed safely without significantly increasing adverse effects.16,17 Some of these concerns may be minimized in the non-intubated patient; these patients are able to position themselves appropriately after given instructions and will reposition frequently. However, there can be other concerns from both patients and the health care staff. Patients may have significant anxiety or physical discomfort with PP. Health care providers may be unfamiliar with PP or may hesitate to suggest due to obesity or concerns over monitoring in a non-ICU setting
Proning in Non-Intubated: Obesity
In obesity, the diaphragm is pushed upward due to excess abdominal fat reducing chest wall compliance and functional residual capacity. In the setting of acute hypoxemic injury in obese patients, ventral to dorsal lung TPP gradients are exaggerated, leading to easier decruitment of alveoli, as compared to nonobese. Thus, homogenization of ventilation and caudal movement of abdominal contents might have even more benefits in obese patients. A study by Pelosi et al supported that the PP in obese patients improves pulmonary function and increases functional residual capacity, lung compliance, and oxygenation.18 However, the study was limited to intubated patients. Prone positioning of an intubated obese patient has ergonomic challenges for the patient and requires numerous staff to perform it safely. This concern is reduced for the awake patient, as they prone themselves. Hence, obesity alone should not discourage PP, as long as the patient is able to tolerate the position and is monitored at appropriate intervals. Our patient with BMI of 65 kg/m2 was able to prone and supine himself without assistance or complications.
Proning in Non-Intubated: Improving Implementation
Patient comfort and health care education regarding PP are required for success (Figure 7). Anxiety is associated with any form of respiratory illness, but it seems to be heightened in current times due to uncertainty about treatment and prognosis of COVID-19. Furthermore, the majority of hospitals have very restricted visitor policies, reducing the availability of family support, and further increasing anxiety. Early consideration of low dose anxiolytics may facilitate tolerance of PP as was seen in both of our patients; however, caution should be observed for any negative effects on the respiratory drive. One could consider oral medications versus a continuous infusion such as dexmedetomidine (in an appropriately monitored setting). Additionally, increased education regarding PP (e.g., handouts) may help reduce anxiety and improve compliance.19 Both of our patients found the educational pamphlets very useful (see supplemental material).
Figure 7.
Proning in non-intubated (PINI): Key for successful bedside implementation.
Lastly, education of health care staff is essential, as many providers outside of an ICU may be involved with PP. Most tertiary centers are adept in proning patients and have already adopted PINI. However, there are many smaller hospitals, where the staff is unfamiliar or uncomfortable PP, and patients with significant hypoxemia are likely to be transferred to a tertiary hospital. That is becoming a challenge in current times as larger centers are experiencing a surge in volume of COVID-19 patients. Proning in non-intubated is a low-risk intervention that can be safely implemented even at smaller centers and may reduce transfer burden to some extent.
Conclusion
With accumulating evidence that PINI improves oxygenation and may prevent intubation in select patients with acute hypoxemic respiratory failure, clinicians, and health care workers should be educated in this low-risk procedure. It is a simple low-risk intervention that may be employed in most circumstances, even on the medical floors. Ideally, it should be initiated early but can be attempted anytime during the hospital course. Additionally, obesity should not be considered a contraindication to PP. Further studies are needed to determine if PINI leads to improvement in other patient-centered outcomes such as mortality and hospital length of stay.
Acknowledgments
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Guerin C, Reignier J, Christophe RJ, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013; 368(23):2159–2168. [DOI] [PubMed] [Google Scholar]
- 2.Sud S, Friedrich JO, Taccone P, et al. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta-analysis. Intensive Care Med 2010;36(4):585–599. [DOI] [PubMed] [Google Scholar]
- 3.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malhotra A, Kacmarek RM. Prone ventilation for adult patients with acute respiratory distress syndrome In G Finlay MD ed. UpToDate. May 2, 2020 April 21, 2020. https://www.uptodate.com/contents/prone-ventilation-for-adult-patients-with-acute-respiratory-distress-syndrome
- 5.Koulouras V, Papathanakos G, Papathanasiou A, Nakos G. Efficacy of prone position in acute respiratory distress syndrome patients: a pathophysiology-based review. World J Crit Care Med. 2016;5(2):121–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Henderson AC, Carlos RS, Theilmann RJ, Buxton RB, Prisk GK, Hopkins SR. The gravitational distribution of ventilation-perfusion ratio is more uniform in prone than supine posture in the normal human lung. J Appl Physiol. 2013;115(3):313–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pelosi P, Brazzi L, Gattinoni L. Prone position in acute respiratory distress syndrome. Eur Respir J. 2002;20(4):1017–1028. [DOI] [PubMed] [Google Scholar]
- 8.Guerin C, Gaillard S, Lemasson S, et al. Effects of systematic prone positioning in hypoxemic acute respiratory failure: a randomized controlled trial. JAMA. 2004; 292(19):2379–2387. [DOI] [PubMed] [Google Scholar]
- 9.Scaravilli V, Grasselli G, Castagna L, et al. Prone positioning improves oxygenation in spontaneously breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective study. J Crit Care. 2015; 30(6):1390–1394. [DOI] [PubMed] [Google Scholar]
- 10.Ding L, Wang L, Ma W, He H. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Crit Care. 2020; 24(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caputo ND, Strayer RJ, Levitan R. Early self-proning in awake, non-intubated patients in the emergency department: a single ED’s experience during the covid-19 pandemic. Acad Emerg Med. 2020;27(5):375–378. doi: 10.1111/acem.13994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nebraska Medicine. COVID19 Proning Protocol - “PRONO-COL”. Published 2020. https://www.nebraskamed.com/sites/default/files/documents/covid-19/proning-protocol.pdf
- 13.Massachusetts General Hospital Prone Positioning for Non-Intubated Patients Guideline. April 2, 2020. Accessed May 10, 2020 https://www.massgeneral.org/assets/MGH/pdf/news/coronavirus/prone-positioning-protocol-for-non-intubated-patients.pdf
- 14.Gordon D, Weingart S. COVID19—awake pronation—a guest write-up by David Gordon, MD. Emcrit. April 6, 2020. Accessed May 10, 2020 https://emcrit.org/emcrit/awake-pronation
- 15.Scholten EL, Beitler JR, Prisk GK, Malhotra A. Treatment of ARDS with prone positioning. Chest. 2017;151(1): 215–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guerin C, Beuret P, Constantin JMG. prospective international observational prevalence study on prone positioning of ARDS patients: the APRONET (ARDS prone position Network) study. Intensive Care Med. 2018;44, 22–37. [DOI] [PubMed] [Google Scholar]
- 17.Hepokoski ML, Odish M, Malhotra A. Prone positioning in acute respiratory distress syndrome: why aren’t we using it more? J Thorac Dis. 2018;10(Suppl 9):S1020–S1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pelosi P, Croci M, Calappi E, et al. Prone positioning improves pulmonary function in obese patients during general anesthesia. Anesth. Analg 1996;83(3):578–583. [DOI] [PubMed] [Google Scholar]
- 19.Gordon D, Weingart S. COVID19—wake pronation—a guest write-up by David Gordon, MD. Emcrit. Self Proning Positioning Handouts; April 6, 2020. Accessed May 10, 2020 https://emcrit.org/wp-content/uploads/2020/04/Self-Proning-Positioning_Eng-n-Spanish.pdf [Google Scholar]


