Abstract
STUDY QUESTION
What are the reported data on cycles in ART, IUI and fertility preservation (FP) interventions in 2016 as compared to previous years, as well as the main trends over the years?
SUMMARY ANSWER
The 20th ESHRE report on ART and IUI shows a progressive increase in reported treatment cycle numbers in Europe, with a decrease in the number of transfers with more than one embryo causing a reduction of multiple delivery rates (DR), as well as higher pregnancy rates and DR after frozen embryo replacement (FER) compared to fresh IVF and ICSI cycles, while the outcomes for IUI cycles remained stable.
WHAT IS KNOWN ALREADY
Since 1997, ART aggregated data generated by national registries, clinics or professional societies have been collected, analysed by the European IVF-monitoring Consortium (EIM) and reported in 19 manuscripts published in Human Reproduction and Human Reproduction Open.
STUDY DESIGN, SIZE, DURATION
Yearly collection of European medically assisted reproduction (MAR) data by EIM for ESHRE. The data on treatments performed between 1 January and 31 December 2016 in 40 European countries were provided by either National Registries or registries based on personal initiatives of medical associations and scientific organizations.
PARTICIPANTS/MATERIALS, SETTING, METHODS
In all, 1347 clinics offering ART services in 40 countries reported a total of 918 159 treatment cycles, involving 156 002 with IVF, 407 222 with ICSI, 248 407 with FER, 27 069 with preimplantation genetic testing, 73 927 with egg donation (ED), 654 with IVM of oocytes and 4878 cycles with frozen oocyte replacement (FOR). European data on IUI using husband/partner’s semen (IUI-H) and donor semen (IUI-D) were reported from 1197 institutions offering IUI in 29 and 24 countries, respectively. A total of 162 948 treatments with IUI-H and 50 467 treatments with IUI-D were included. A total of 13 689 FP interventions from 11 countries including oocyte, ovarian tissue, semen and testicular tissue banking in pre-and postpubertal patients were reported.
MAIN RESULTS AND THE ROLE OF CHANCE
In 20 countries (18 in 2015) with a total population of approximately 325 million inhabitants, in which all ART clinics reported to the registry, a total of 461 401 treatment cycles were performed, corresponding to a mean of 1410 cycles per million inhabitants (range 82–3088 per million inhabitants). In the 40 reporting countries, after IVF the clinical pregnancy rates (PR) per aspiration and per transfer in 2016 were similar to those observed in 2015 (28.0% and 34.8% vs 28.5% and 34.6%, respectively). After ICSI, the corresponding rates were also similar to those achieved in 2015 (25% and 33.2% vs 26.2% and 33.2%). After FER with own embryos, the PR per thawing is still on the rise, from 29.2% in 2015 to 30.9% in 2016. After ED, the PR per fresh embryo transfer was 49.4% (49.6% in 2015) and per FOR 43.6% (43.4% in 2015). In IVF and ICSI together, the trend towards the transfer of fewer embryos continues with the transfer of 1, 2, 3 and ≥4 embryos in 41.5%, 51.9%, 6.2% and 0.4% of all treatments, respectively (corresponding to 37.7%, 53.9%, 7.9% and 0.5% in 2015). This resulted in a proportion of singleton, twin and triplet DRs of 84.8%, 14.9% and 0.3%, respectively (compared to 83.1%, 16.5% and 0.4%, respectively in 2015). Treatments with FER in 2016 resulted in twin and triplet DR of 11.9% and 0.2%, respectively (vs 12.3% and 0.3% in 2015). After IUI, the DRs remained similar at 8.9% after IUI-H (7.8% in 2015) and at 12.4% after IUI-D (12.0% in 2015). Twin and triplet DRs after IUI-H were 8.8% and 0.3%, respectively (in 2015: 8.9% and 0.5%) and 7.7% and 0.4% after IUI-D (in 2015: 7.3% and 0.6%). The majority of FP interventions included the cryopreservation of ejaculated sperm (n = 7877 from 11 countries) and of oocytes (n = 4907 from eight countries).
LIMITATIONS, REASONS FOR CAUTION
As the methods of data collection and levels of completeness of reported data vary among European countries, the results should be interpreted with caution. A number of countries failed to provide adequate data about the number of initiated cycles and deliveries.
WIDER IMPLICATIONS OF THE FINDINGS
The 20th ESHRE report on ART and IUI shows a continuous increase of reported treatment numbers and MAR-derived livebirths in Europe. Being already the largest data collection on MAR in Europe, continuous efforts to stimulate data collection and reporting strive for future quality control of the data, transparency and vigilance in the field of reproductive medicine.
STUDY FUNDING/COMPETING INTEREST(S)
The study has no external funding and all costs were covered by ESHRE. There are no competing interests.
Keywords: IVF / ICSI / IUI / egg donation / frozen embryo replacement / surveillance / vigilance / registry / data collection / fertility preservation
Introduction
This is the 20th annual report of the European IVF-monitoring Consortium (EIM) under the umbrella of ESHRE containing the data on ART, IUI and fertility preservation (FP) as reported by 40 participating European countries in 2016 (Supplementary Data).
Eighteen previous reports published in Human Reproduction (https://www.eshre.eu/Data-collection-and-research/Consortia/EIM/Publications.aspx) and one in Human Reproduction Open (De Geyter et al., 2020) covered treatment cycles from 1997 to 2015. As in previous reports, the printed version contains the five most relevant tables. Twenty additional supplementary tables (Supplementary Tables SI–SXX) are available online. The settings of the data are consistent with those published in the previous reports, aiming at easier comparison and assessment of trends. For the first time, an additional set of data dealing with FP was collected and added to this report.
Material and methods
Data collected on an aggregate basis were provided by 40 European countries, covering the following treatment modalities: IVF, ICSI, frozen embryo replacement (FER), egg donation (ED), IVM, pooled data on preimplantation genetic testing (PGT) and frozen oocyte replacement (FOR). With regards to IUI, split data for use of husband’s/partner’s semen (IUI-H) and donor semen (IUI-D) were included. The report includes treatments started between 1 January and 31 December 2016. Data on pregnancies and deliveries were derived from follow-up of treatments performed in 2016. In addition, data on FP, including numbers and types of cryostored material and interventions for use of stored material between 1 January and 31 December 2016, were provided by 11 countries and reported as aggregated data of events that occurred during a 1-year period.
The national representatives of 44 countries were asked to fill out questionnaires, with other involved stakeholders when applicable. The same data sets as in 2015 and additional data on FP for a total of 10 specific modules were sent using software designed for the specific requirements of this data collection (Dynamic Solutions, Barcelona, Spain). Besides evaluation of the plausibility of the results by the software, other detected inconsistencies were clarified through contacts between the administrator of the ESHRE central office (V.G.) and the national representative.
The data were analysed and presented similarly to previous reports (although with some additional subgroups of interventions) and footnotes to the tables were added for clarification on diverging results reported by individual countries, when applicable.
The terminology used was based on the glossary of the International Committee for Monitoring Assisted Reproductive Technology (Zegers-Hochschild et al., 2017).
Results
Participation and data completeness
Table I shows the number of institutions or clinics offering ART services with all available treatment modalities and those performing IUI (IUI-H and IUI-D). In comparison to the 2015 data, both the total number of reporting clinics (1343 in 2015 to 1347 in 2016) and the overall number of reported treatments (849 811 in 2015 to 918 159 in 2016, +8.0%) increased. Among the 51 European countries, 44 are EIM members including 28 that are members of the European Union (Supplementary Table SI). Non-EIM members are mainly smaller countries not offering ART services. In 2016, 40 countries delivered data to EIM with Luxemburg providing data as a new EIM member. Croatia, Georgia, Slovakia and Turkey failed to deliver data (9.1% of EIM members, 11.6% in 2015). In 18 countries (45% of reporting countries), all of the ART clinics within the country reported data sets. Currently, 1347 clinics reported their data (91.8% of all known clinics in Europe, 90.6% in 2015). As in 2015, the four European countries with the largest treatment numbers in 2016 were Spain (140 909), Russia (121 232), France (104 773) and Germany (99 226).
Table I.
Treatment frequencies after ART in European countries in 2016.
| Country | IVF clinics in the country |
Cycles/million* |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IVF clinics | Included IVF clinics | IUI labs | Included IUI labs | IVF | ICSI | FER | PGT | ED | IVM | FOR | All | Women aged 15–45 years | Population | |
| Albania | 10 | 1 | 0 | 83 | 63 | 0 | 29 | 0 | 0 | 175 | ||||
| Armenia | 5 | 2 | 6 | 2 | 66 | 112 | 107 | 61 | 346 | |||||
| Austria | 26 | 26 | 1459 | 5600 | 2662 | 0 | 9721 | 5886 | 1110 | |||||
| Belarus | 8 | 7 | 10 | 7 | 1310 | 1394 | 270 | 7 | 16 | 0 | 0 | 2997 | ||
| Belgium | 18 | 18 | 29 | 29 | 2715 | 13 628 | 12 052 | 1100 | 1163 | 176 | 95 | 30 929 | 14 136 | 2738 |
| Bosnia-Herzegovina, Federation part | 6 | 1 | 0 | 89 | 46 | 135 | ||||||||
| Bulgaria | 35 | 35 | 1 | 1 | 920 | 6879 | 1813 | 379 | 1018 | 11 009 | 7153 | 1544 | ||
| Cyprus | 6 | 6 | 158 | 942 | 325 | 31 | 271 | 1727 | 9089 | 2020 | ||||
| Czech Republic | 41 | 40 | 0 | 15 020 | 12 258 | 5265 | 32 543 | |||||||
| Denmark | 19 | 19 | 35 | 33 | 6319 | 5703 | 5059 | 112 | 484 | 0 | 19 | 17 696 | 15 917 | 3088 |
| Estonia | 6 | 6 | 6 | 6 | 641 | 1184 | 927 | 2 | 191 | 0 | 7 | 2952 | 11 515 | 2245 |
| Finland | 17 | 17 | 22 | 22 | 2756 | 1970 | 3661 | 73 | 731 | 0 | 9191 | 9116 | 1673 | |
| France | 102 | 102 | 181 | 181 | 22 773 | 45 214 | 33 792 | 1422 | 1158 | 70 | 344 | 104 773 | 9066 | 1619 |
| Germany | 134 | 128 | 17 594 | 56 587 | 25 045 | 99 226 | ||||||||
| Greece | 39 | 39 | 39 | 39 | 2304 | 15 121 | 4785 | 1251 | 4462 | 2 | 51 | 27 976 | 13 922 | 2603 |
| Hungary | 13 | 11 | 1049 | 3902 | 632 | 25 | 5608 | |||||||
| Iceland | 1 | 1 | 1 | 1 | 199 | 162 | 229 | 0 | 54 | 0 | 0 | 644 | 9248 | 1928 |
| Ireland | 1 | 215 | 231 | 260 | 706 | |||||||||
| Italy | 200 | 200 | 360 | 360 | 7584 | 46 322 | 14 990 | 2844 | 4359 | 1460 | 77 559 | 7014 | 1280 | |
| Kazakhstan | 10 | 5 | 994 | 1671 | 958 | 154 | 683 | 4460 | ||||||
| Latvia | 6 | 3 | 6 | 3 | 352 | 527 | 515 | 7 | 127 | 1528 | ||||
| Lithuania | 6 | 5 | 6 | 5 | 295 | 371 | 92 | 0 | 0 | 758 | ||||
| Luxembourg | 1 | 1 | 5 | 0 | 312 | 354 | 314 | 0 | 0 | 0 | 0 | 980 | 1684 | |
| Malta | 2 | 2 | 2 | 0 | 7 | 273 | 0 | 0 | 0 | 0 | 79 | 359 | 3624 | 822 |
| Moldova | 4 | 3 | 5 | 3 | 0 | 739 | 181 | 14 | 934 | |||||
| Montenegro | 5 | 4 | 5 | 4 | 7 | 501 | 58 | 566 | ||||||
| North Macedonia | 7 | 5 | 0 | 0 | 420 | 2100 | 288 | 0 | 122 | 0 | 4 | 2934 | ||
| Norway | 11 | 11 | 11 | 11 | 3587 | 3330 | 3363 | 0 | 0 | 10 280 | 10 101 | 1963 | ||
| Poland | 39 | 39 | 0 | 38 | 881 | 16 984 | 11 375 | 692 | 1085 | 33 | 299 | 31 349 | 816 | |
| Portugal | 24 | 24 | 26 | 26 | 2462 | 3751 | 2008 | 127 | 988 | 1 | 28 | 9365 | 1726 | 907 |
| Romania | 19 | 11 | 19 | 11 | 1445 | 2034 | 1495 | 6 | 29 | 5009 | ||||
| Russia | 199 | 151 | 34 058 | 43 766 | 31 051 | 4420 | 7122 | 260 | 558 | 121 235 | ||||
| Serbia | 12 | 3 | 12 | 3 | 170 | 93 | 23 | 0 | 0 | 0 | 0 | 286 | ||
| Slovenia | 3 | 3 | 3 | 3 | 1017 | 2268 | 1389 | 37 | 7 | 0 | 7 | 4725 | 12 717 | 2288 |
| Spain | 247 | 240 | 366 | 291 | 5624 | 56 640 | 27 559 | 10 238 | 39 530 | 41 | 1277 | 140 909 | ||
| Sweden | 18 | 17 | 0 | 6235 | 6088 | 6080 | 304 | 282 | 18 989 | |||||
| Switzerland | 27 | 27 | 1042 | 5059 | 4859 | 10 960 | 10 329 | 1309 | ||||||
| The Nederlands | 13 | 13 | 90 | 0 | 6781 | 7803 | 12 545 | 772 | 27 901 | 5403 | 1639 | |||
| Ukraine | 46 | 38 | 17 | 17 | 1167 | 9454 | 6967 | 1658 | 1157 | 8 | 20 411 | |||
| UK | 82 | 82 | 101 | 101 | 21 084 | 23 273 | 18 311 | 1433 | 3494 | 71 | 642 | 68 308 | 5240 | 1041 |
| All | 1467 | 1347 | 1364 | 1197 | 156 002 | 407 222 | 248 407 | 27 069 | 73 927 | 654 | 4878 | 918 159 | 7794 | 1410 |
Treatment cycles in IVF and ICSI refer to initiated cycles.
For Austria, Belgium, Iceland, Lithuania and Malta, treatment cycles IVF refer to aspirations. For Austria, Belgium, Iceland and Lithuania, treatment cycles ICSI refer to aspirations. For Austria and Belgium, the total number of initiated cycles was only available for IVF and ICSI together, being 10 097 and 19 163, respectively.
For the Czech Republic, no distinction between IVF and ICSI is made. All cycles are counted as ICSI. For Belgium, there are 824 extra aspiration cycles for which it is not known whether IVF or ICSI was performed.
Treatment cycles in frozen embryo replacement (FER) refer to thawings.
For Finland, Hungary, Kazakhstan, Sweden and the Netherlands, treatment cycles refer to transfers.
Treatment cycles in preimplantation genetic testing (PGT) contain both fresh and frozen cycles and refer to initiated cycles in the fresh cycles and aspirations in the frozen cycles.
Treatment cycles in egg donation (ED) refer to donation cycles and contain fresh and frozen cycles.
ED fresh: for France and Iceland, treatment cycles refer to aspirations. ED frozen: for France, Iceland, Kazakhstan, Spain, Sweden and the UK, treatment cycles refer to aspirations.
Treatment cycles in IVM refer to aspirations.
Treatment cycles in frozen oocyte replacement (FOR) refer to thawings.
Size of the clinics and reporting methods
The size of reporting clinics, defined by the number of treatment cycles, remains highly variable between and inside countries (Supplementary Table SII). In 2016, clinics with cycle numbers between 200 and 499 were the most common (29.5% vs 29.9%). Small clinics providing less than 100 treatments cycles per year were present in 16 countries (40% of the countries) and the proportion of clinics performing more than 1000 treatment cycles per year seems on a slight rise over the years with 19.4% in 2016, 17.9% in 2015, 18.3% in 2014, 17.8% in 2013 and 16.9% in 2012.
Country-specific requirements and reporting methods are presented in Supplementary Table SIII. Data collection was either voluntary (19 out of 40 countries) or compulsory. Twenty countries had only a partial reporting and provided the data mainly on a voluntary basis (16/20 countries) to medical organizations/professional societies (10 countries), based on a single person’s initiatives (five countries) or to the national health authority (one country).
By contrast, complete reporting was achieved mainly when data collection was compulsory (17/20 countries) with subsequent data communication to the national health authority (all but two countries).
Transfer of data was mostly done on an aggregate basis (26 countries/40 in 2016, as in 2015).
Number of treatment cycles per technique and availability
In 2016, 918 159 treatment cycles were reported to EIM (68 348 more than in 2015, +8.0%). Since 1997 increasing numbers of clinics reported to EIM, which so far recorded more than 9 772 904 treatments cycles and the birth of more than 1 861 760 infants (Table II). As shown in Table I, compared to 2015, 10 countries reported fewer treatment cycles, but Ireland and Luxemburg were now able to provide data. Furthermore, the largest increment in reported treatment numbers was recorded in Spain (+21 034, +9 clinics), France (+10 855, same number of clinics) and Russia (+10 512, +7 clinics). The numbers of treatment cycles per technique in 2016 are presented in Table I: ICSI was the most used (407 222, 44.4% of treatment cycles vs 45.4% in 2015). Cycles of IVF, FER, ED, FOR, PGT and IVM represented 17%, 27%, 8.1%, 0.5%, 2.9% and 0.0007% of all cycles, respectively. While the distribution of the available techniques remained similar to 2015 (IVF, FER, ED, FOR, PGT and IVM, respectively 18.4%, 25.7%, 7.6%, 0.5%, 2.5% and 0.0003%), for each single technique higher cycle numbers were registered. The steepest rise in treatment numbers was observed in FER (+13.9%), in ED (+14.7%), in FOR (+13.6%), in PGT (+27.4%) and IVM (+246.8%). The proportion of FER relative to fresh treatments (IVF + ICSI) is still on the rise (44.1% vs 40.3% in 2015 and 37.8% in 2014). The highest proportions were reached in Armenia (75.9%), Belgium (73.7%), Czech Republic (81.6%), Finland (77.5%), Switzerland (79.6%) and The Netherlands (86.0%). No FER were reported/performed in Malta according to their legislation.
Table II.
Number of institutions offering ART services, treatment cycles and infants born after ART in Europe, 1997–2016.
| Year | Countries | Clinics | Cycles | Cycle increase (%) | Infants born |
|---|---|---|---|---|---|
| 1997 | 18 | 482 | 203 225 | 35 314 | |
| 1998 | 18 | 521 | 232 225 | +14.3 | 21 433 |
| 1999 | 21 | 537 | 249 624 | +7.5 | 26 212 |
| 2000 | 22 | 569 | 275 187 | +10.2 | 17 887 |
| 2001 | 23 | 579 | 289 690 | +5.3 | 24 963 |
| 2002 | 25 | 631 | 324 238 | +11.9 | 24 283 |
| 2003 | 28 | 725 | 365 103 | +12.6 | 68 931 |
| 2004 | 29 | 785 | 367 056 | +0.5 | 67 973 |
| 2005 | 30 | 923 | 419 037 | +14.2 | 72 184 |
| 2006 | 32 | 998 | 458 759 | +9.5 | 87 705 |
| 2007 | 33 | 1029 | 493 420 | +7.7 | 96 690 |
| 2008 | 36 | 1051 | 532 260 | +7.9 | 107 383 |
| 2009 | 34 | 1005 | 537 463 | +1.0 | 109 239 |
| 2010 | 31 | 991 | 550 296 | +2.4 | 120 676 |
| 2011 | 33 | 1314 | 609 973 | +11.3 | 134 106 |
| 2012 | 34 | 1354 | 640 144 | +4.9 | 143 844 |
| 2013 | 38 | 1169 | 686 271 | +7.2 | 149 466 |
| 2014 | 39 | 1279 | 776 556 | +13.1 | 170 163 |
| 2015 | 38 | 1343 | 849 811 | +10.2 | 187 542 |
| 2016 | 40 | 1347 | 918 159 | +8.0 | 195 766 |
| Total | 9 772 904 | 1 861 760 |
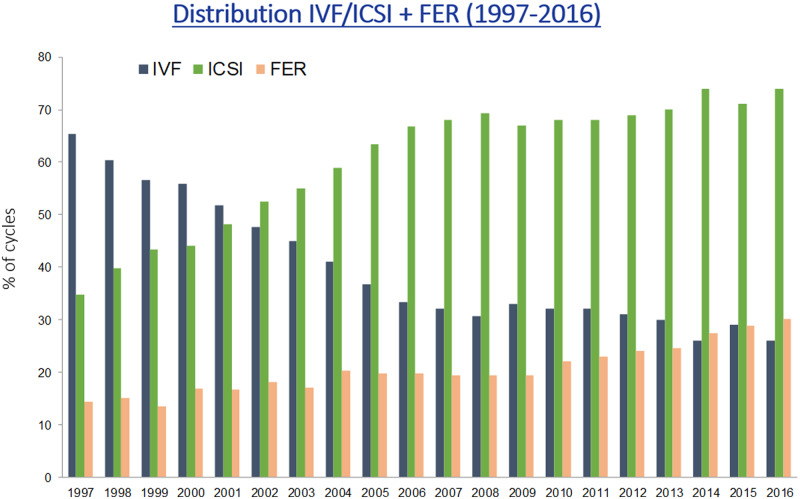
Among the total of 563 224 fresh treatments (ICSI + IVF), 72.3% were performed with ICSI, showing a rise of +1.2% compared to 2015. Figure 1 shows the evolution and continuing preponderance of ICSI over conventional IVF and the increase in the proportion of FER cycles relative to fresh cycles (IVF + ICSI).
Figure 1.
Proportion of IVF versus ICSI and frozen embryo replacement (FER) in Europe, 1997–2016.
The number of cycles per million women of reproductive age and per million inhabitants is shown in Table I and Supplementary Table SIV. Availability of ART was calculated for the 20 countries with full coverage (Supplementary Table SIV). While there is a huge variability in availability (range 1726–15 917 per million women aged 15–45 years), ART was most available in Denmark and least available in Portugal. Consequently, the proportion of newborns resulting from ART born in Denmark was 5.1% of all newborns in that country. Other countries that reported high proportions were Austria (6.2%) and Slovenia (5.5%).
Pregnancies and deliveries after treatment
Table III shows PR and delivery rates (DR) after IVF or ICSI and after FER (after both IVF and ICSI). Because, as in previous years, data on numbers of initiated cycles were incomplete, the outcome data were calculated per aspiration.
Table III.
Results after ART in 2016.
| Country | IVF |
ICSI |
FER |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Initiated cycles IVF + ICSI | Aspirations | Pregnancies per aspiration (%) | Deliveries per aspiration (%) | Aspirations | Pregnancies per aspiration (%) | Deliveries per aspiration (%) | Thawings | Pregnancies per thawing (%) | Deliveries per thawing (%) | ART infants † | ART infants per national births (%) | |
| Albania | 83 | 83 | 41.0 | 33.7 | 63 | 41.3 | 23.8 | 70 | ||||
| Armemia | 178 | 66 | 24.2 | 21.2 | 112 | 25.9 | 21.4 | 107 | 36.4 | 28.0 | 114 | 0.3 |
| Austria | 10 097 | 1459 | 33.9 | 5600 | 28.5 | 46.5 | 2662 | 34.3 | 5479 | 6.2 | ||
| Belarus | 2704 | 1241 | 35.9 | 27.2 | 1328 | 34.7 | 24.9 | 270 | 25.9 | 14.8 | 798 | 0.7 |
| Belgium | 19 163 | 2715 | 27.8 | 20.3 | 13 628 | 24.2 | 16.0 | 12 052 | 27.8 | 17.1 | 5566 | 4.6 |
| Bosnia-Herzegovina, Federation part | 89 | 80 | 33.8 | 26.3 | 46 | 23.9 | 13.0 | 31 | ||||
| Bulgaria | 7799 | 868 | 21.7 | 13.6 | 5660 | 26.3 | 19.7 | 1813 | 32.2 | 25.0 | ||
| Cyprus | 1100 | 146 | 39.0 | 33.6 | 813 | 39.1 | 37.4 | 325 | 40.6 | 33.5 | ||
| Czech Republic | 15 020 | 14 661 | 22.5 | 15.0 | 12 258 | 30.2 | 18.9 | 6278 | 5.6 | |||
| Denmark | 12 022 | 6309 | 20.9 | 14.1 | 5701 | 22.5 | 17.7 | 5059 | 24.7 | 19.9 | 3157 | 5.1 |
| Estonia | 1825 | 635 | 25.2 | 19.2 | 1184 | 28.0 | 20.9 | 927 | 22.8 | 15.6 | 664 | 4.7 |
| Finland | 4726 | 2573 | 23.8 | 18.3 | 1879 | 23.8 | 18.3 | 1607 | 3.0 | |||
| France | 67 987 | 20 058 | 21.1 | 18.3 | 41 587 | 21.4 | 18.8 | 33 792 | 21.4 | 18.3 | 20 187 | 2.6 |
| Germany | 74 181 | 16 234 | 28.8 | 19.4 | 52 235 | 27.0 | 18.2 | 25 045 | 27.6 | 17.4 | 20 540 | |
| Greece | 17 425 | 2256 | 26.9 | 18.6 | 13 082 | 23.0 | 15.3 | 4785 | 36.7 | 23.9 | 6346 | |
| Hungary | 4951 | 1043 | 31.4 | 3871 | 32.3 | |||||||
| Iceland | 199 | 25.6 | 23.1 | 162 | 30.2 | 25.3 | 229 | 29.3 | 20.1 | 155 | 3.8 | |
| Ireland | 446 | 183 | 40.4 | 33.9 | 214 | 38.8 | 30.4 | 260 | 38.8 | 30.0 | 213 | |
| Italy | 53 906 | 6857 | 21.6 | 15.1 | 41 899 | 18.7 | 12.3 | 14 990 | 27.5 | 19.3 | 12 053 | 2.5 |
| Kazakhstan | 2665 | 974 | 40.1 | 26.4 | 1648 | 38.3 | 25.9 | 1497 | 0.4 | |||
| Latvia | 879 | 352 | 36.9 | 22.2 | 527 | 27.5 | 15.2 | 515 | 40.2 | 28.3 | 366 | |
| Lithuania | 295 | 52.9 | 7.1 | 371 | 42.6 | 1.6 | 92 | 23.9 | 38 | 0.1 | ||
| Luxembourg | 666 | 296 | 13.2 | 9.8 | 319 | 19.7 | 16.9 | 314 | 25.8 | 17.2 | 155 | 2.6 |
| Malta | 273 | 7 | 187 | 40 | 0.9 | |||||||
| Moldova | 739 | 731 | 41.9 | 34.7 | 181 | 51.9 | 45.3 | |||||
| Montenegro | 508 | 7 | 57.1 | 28.6 | 496 | 27.0 | 21.4 | 58 | 31.0 | 27.6 | 156 | 2.1 |
| Norway | 6917 | 3412 | 28.8 | 24.2 | 3172 | 29.6 | 24.8 | 3363 | 23.5 | 18.6 | ||
| North Macedonia | 2520 | 390 | 33.8 | 10.5 | 2068 | 35.5 | 18.9 | 288 | 34.4 | 21.2 | 628 | 3.4 |
| Poland | 17 865 | 873 | 28.6 | 23.1 | 16 935 | 25.8 | 15.6 | 11 375 | 35.9 | 23.6 | 6336 | |
| Portugal | 6213 | 2279 | 29.4 | 22.6 | 3676 | 23.0 | 17.4 | 2008 | 30.9 | 22.8 | 2333 | 2.7 |
| Romania | 3479 | 1399 | 31.6 | 23.4 | 1954 | 28.3 | 22.7 | 1495 | 30.6 | 19.7 | 1288 | 0.7 |
| Russia | 77 824 | 33 129 | 29.9 | 21.8 | 42 542 | 25.9 | 18.4 | 31 051 | 38.5 | 27.5 | 30 770 | 1.7 |
| Serbia | 263 | 166 | 25.9 | 21.7 | 87 | 41.4 | 37.9 | 23 | 39.1 | 39.1 | 100 | 0.2 |
| Slovenia | 3285 | 916 | 33.0 | 25.8 | 2220 | 25.8 | 20.7 | 1389 | 31.3 | 23.0 | 1116 | 5.5 |
| Spain | 62 264 | 5229 | 26.3 | 19.1 | 45 373 | 22.4 | 16.3 | 27 559 | 34.4 | 22.9 | 31 715 | 7.7 |
| Sweden | 12 323 | 5803 | 29.3 | 24.3 | 5744 | 27.4 | 23.2 | 4923 | 4.1 | |||
| Switzerland | 6101 | 958 | 24.3 | 17.8 | 4621 | 24.5 | 19.1 | 4859 | 23.4 | 16.6 | 2160 | 2.5 |
| The Nederlands | 14 584 | 5819 | 31.0 | 22.2 | 7038 | 32.9 | 24.6 | |||||
| Ukraine | 10 621 | 1141 | 36.8 | 25.7 | 9243 | 30.1 | 24.6 | 6967 | 46.0 | 38.6 | 7622 | 1.9 |
| UK | 44 357 | 18 483 | 32.8 | 28.5 | 23 097 | 33.1 | 28.8 | 18 311 | 34.2 | 29.5 | 21 265 | 2.7 |
| All | 568 048 | 144 770 | 28.0 | 20.8 | 375 828 | 25.0 | 18.5 | 224 531 | 30.9 | 22.0 | 195 766 | 2.9 |
Total rates refer to these countries were all data were reported for the given technique:
ART infants also include ED.
For IVF and ICSI, there were for Austria, Czech Republic, Finland, France, Greece, Kazakhstan, Latvia, Poland, Portugal, Russia, Serbia, Spain and Sweden, respectively 2650, 3, 810, 14, 254, 43, 13, 319, 4, 817, 1, 345 and 4 deliveries with unknown outcome. These were accepted as singletons to calculate the ART infants.
For FER, there were for Czech Republic, Finland, France, Greece, Kazakhstan, Latvia, Poland, Russia, Spain and Sweden, respectively 1, 797, 8, 42, 4, 15, 228, 471, 89 and 2 deliveries with unknown outcome. These were accepted as singletons to calculate the ART infants.
For ED, there were for Germany, Italy, Kazakhstan, Romania and Slovenia, respectively 3, 17, 14, 222 and 7582 deliveries with unknown outcome. These were accepted as singletons to calculate the ART infants.
For PGD, there were for Finland, Germany and Romania, respectively 1, 1 and 154 deliveries with unknown outcome. These were accepted as singleton to calculate the ART infants.
In the Czech Republic, IVF and ICSI were reported together, no details on pregnancies and deliveries.
Among the 40 reporting countries, 33 were able to provide both pregnancy and delivery data per aspiration after IVF and ICSI and per thawing for FER (completeness rate for both: 82.5%). In Supplementary Table SIV, the numbers of deliveries for the 20 countries that had full coverage of the reporting are presented.
As in all previous reports, the PR and DR (for all types of treatment cycles) varied significantly from one country to another. Per aspiration, PR ranged from 13.2% to 57.1% and DR from 12.3% to 46.5% in fresh cycles after IVF or ICSI (excluding Lithuania where DR was not available for two of the five centres reporting pregnancies). After FER per thawing, the PR were between 21.4% and 51.9% and the DR varied between 13% and 45.3%. Overall, PR and DR were higher for FER cycles (per thawing) than for both fresh IVF and ICSI cycles (per aspiration) (Table III).
For the third time, «freeze all» cycles were collected (Supplementary Table SV) including cryopreservation of all oocytes reported by 10 countries (six in 2015 and 2014) and of all embryos by 22 countries (21 in 2015 and 2014). The highest proportions of freeze all cycles per aspiration were 3.5% at the oocyte and 17.3% at the embryo level.
Cycle numbers, aspirations, transfers, pregnancies, deliveries in IVF, ICSI and FER (after both IVF and ICSI) by country are given in the Supplementary Tables SV–SVII.
As in 2015, ED cycle numbers were available for 26 countries although 29 provided outcome data (Supplementary Table SVIII). Most donation cycles were carried out in Spain, Russia, the Czech Republic and Greece. Freshly collected oocytes were used in 33 406 ED cycles and frozen oocytes (FOR) in 11 757 ED cycles. PR were only available per embryo transfer for freshly donated oocytes (49.4%, in 2015 49.6%) and for thawed oocytes (41%, in 2015 40.3%). Outcomes for the different countries show a high variability ranging between 9.7% and 66.5%% for fresh oocytes and between 29.5% and 67.4% for thawed oocytes. A total of 22 497 deliveries were reported (19 849 in 2015 and 17 259 in 2014) representing a further increase of +13.3%.
Age distribution
As seen in Supplementary Tables SIX and SX, age distributions of women treated with IVF and ICSI varied between countries. Not all countries were able to provide data on the age distribution in ICSI (six missing) and in IVF (seven missing), some because no IVF treatments were carried out. The highest percentage of women aged40 years and older undergoing aspiration for IVF was found in Greece (as in 2015), whereas the highest percentage of women aged <34 years was found in Montenegro (as in 2015) followed by Ukraine. For ICSI, the highest percentage of women aged 40 years and older undergoing aspiration was found in Greece (as in 2015), whereas the highest percentage of women undergoing aspiration aged <34 years was recorded in Kazakhstan (in Albania in 2015 and 2014). As expected, there was an age-dependent decline of the reported PR and DR for IVF and ICSI treatment cycles with DR in women aged 40 years and older, ranging between 0% and 13.1%, and 0% and 42.9% (on small numbers), respectively. With regard to FER (Supplementary Table SXI), the age-related decline was also visible and DR among women aged 40 years and older ranged between 0% and 34.3%.
In ED cycles (Supplementary Table SXII), the age of the recipient women did not influence outcome data and overall PR and DR were higher than in fresh and FER cycles (in partner donation).
Numbers of embryos transferred and multiple births
The subgroups defined by the number of embryos transferred after IVF and ICSI together as well as multiple births are presented in Table IV. Five countries did not report on either the number of replaced embryos per treatment cycle or on multiplicity. While overall most transfers involved the replacement of two embryos (51.9% of the transfer cycles), the proportion of transfers of only one embryo per cycle continued to rise (41.5% vs 37.7% in 2015), and the number of transfers of three or more embryos continued to decrease (Fig. 2). The number of countries reporting more than 50% of single embryo transfers (elective or not) increased to 10 (same eight as in 2015 plus Slovenia and UK). As in 2015, only Serbia reported more than 50% of transfers with three embryos. The highest proportion of transfers of four or more embryos was recorded in Greece (4.2% vs 4.9% in 2015). Information on the type of embryos (cleavage or blastocyst) transferred was not available for each of the subgroups but, for the first time, the embryo stage at the transfer was collected. Taking into account that the embryo stage at transfer was unknown for 44.5% of the fresh (IVF+ICSI) cycles, 41.9% of the transfers were performed at the blastocyst stage and the corresponding figure for FER was 62.2%.
Table IV.
Number of embryos transferred after ART and deliveries in 2016.
| Country | IVF + ICSI |
FER | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fresh transfers total | Fresh transfers cleavage stage | Fresh transfers blastocyst stage | Fresh transfers unkown stage | % Fresh transfers cleavage stage** | % Fresh transfers blastocyst stage** | 1 embryo (%) | 2 embryos (%) | 3 embryos (% ) | 4+ embryos (%) | Deliveries | Twin (%) | Triplet (%) | Deliveries | Twin (%) | Triplet (%) | |
| Albania | 74 | 72 | 2 | 0 | 97.3 | 2.7 | 9.5 | 90.5 | 0.0 | 0.0 | 28 | 35.7 | 0.0 | 15 | 20.0 | 0.0 |
| Armemia | 114 | 99 | 15 | 0 | 86.8 | 13.2 | 11.4 | 83.3 | 5.3 | 0.0 | 38 | 15.8 | 0.0 | 30 | 10.0 | 0.0 |
| Austria | 8702 | 2484 | 6219 | 0 | 28.5 | 71.5 | 65.7 | 34.0 | 0.3 | 0.0 | 5210 | 10.2 | 0.1 | |||
| Belarus | 2300 | 1462 | 838 | 0 | 63.6 | 36.4 | 18.2 | 73.1 | 8.7 | 0.0 | 668 | 10.5 | 0.3 | 40 | 15.0 | 0.0 |
| Belgium | 13 081 | 8856 | 4225 | 0 | 67.7 | 32.3 | 62.8 | 31.9 | 4.7 | 0.6 | 2734 | 9.2 | 0.1 | 2055 | 7.4 | 0.0 |
| Bosnia-Herzegovina, Federation part | 67 | 31 | 36 | 0 | 46.3 | 53.7 | 46.3 | 50.7 | 3.0 | 0.0 | 21 | 14.3 | 0.0 | 6 | 16.7 | 0.0 |
| Bulgaria | ||||||||||||||||
| Cyprus | ||||||||||||||||
| Czech Republic | 10 727 | 10 727 | 70.0 | 29.4 | 0.6 | 0.0 | 2199 | 7.7 | 0.1 | 2313 | 9.0 | 0.2 | ||||
| Denmark | 9567 | 4832 | 2300 | 2435 | 67.8 | 32.2 | 71.0 | 28.7 | 0.2 | 0.0 | 1895 | 4.9 | 0.0 | 1008 | 4.4 | 0.0 |
| Estonia | 1549 | 976 | 573 | 0 | 630. | 37.0 | 44.7 | 48.9 | 6.3 | 0.0 | 370 | 14.3 | 0.3 | 145 | 16.6 | 0.0 |
| Finland | 3396 | 3396 | 85.7 | 14.3 | 0.0 | 0.0 | 810 | 797 | ||||||||
| France | 45 534 | 45 534 | 46.5 | 48.7 | 4.5 | 0.3 | 11 506 | 13.1 | 0.1 | 6189 | 7.8 | 0.1 | ||||
| Germany | 56 413 | 39 850 | 16 563 | 0 | 70.6 | 29.4 | 21.6 | 69.2 | 9.2 | 0.0 | 12 688 | 21.0 | 0.5 | 4352 | 15.2 | 0.4 |
| Greece | 9494 | 6367 | 3127 | 0 | 67.1 | 32.9 | 22.5 | 59.3 | 14.0 | 4.2 | 2415 | 22.4 | 0.3 | 1146 | 23.6 | 0.0 |
| Hungary | 4505 | 4505 | 22.9 | 56.4 | 18.1 | 2.6 | ||||||||||
| Iceland | 287 | 287 | 84.3 | 15.7 | 0.0 | 0.0 | 87 | 1.1 | 0.0 | 46 | 4.3 | 0.0 | ||||
| Ireland | 338 | 338 | 0 | 100.0 | 0.0 | 127 | 4.7 | 0.0 | 78 | 2.6 | 0.0 | |||||
| Italy | 36 038 | 36 038 | 30.2 | 50.3 | 17.9 | 1.6 | 6196 | 15.6 | 0.4 | 2890 | 7.4 | 0.2 | ||||
| Kazakhstan | 2238 | 2238 | 0 | 0 | 100.0 | 0.0 | 674 | 11.3 | 0.0 | 405 | 32.9 | 0.0 | ||||
| Latvia | 630 | 428 | 182 | 10 | 69.0 | 29.4 | 48.4 | 51.3 | 0.3 | 0.0 | 158 | 13.1 | 0.7 | 146 | 7.6 | 0.8 |
| Lithuania | 661 | 78 | 30 | 553 | 72.2 | 27.8 | 13.0 | 52.8 | 34.3 | 0.0 | 27 | 33.3 | 3.7 | |||
| Luxembourg | 424 | 416 | 8 | 0 | 98.1 | 1.9 | 38.4 | 61.6 | 0.0 | 0.0 | 83 | 15.7 | 0.0 | 54 | 9.3 | 0.0 |
| Malta | 181 | 181 | 0 | 0 | 100.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 34 | 17.6 | 0.0 | |||
| Moldova | ||||||||||||||||
| Montenegro | 448 | 377 | 71 | 0 | 84.2 | 15.8 | 16.7 | 43.8 | 39.1 | 0.4 | 108 | 25.9 | 0.0 | 16 | 25.0 | 0.0 |
| Norway | ||||||||||||||||
| North Macedonia | 2059 | 1650 | 409 | 0 | 80.1 | 19.9 | 25.6 | 66.1 | 8.2 | 0.0 | 432 | 16.2 | 0.7 | 61 | 14.8 | 0.0 |
| Poland | 12 345 | 7104 | 5241 | 0 | 57.5 | 42.5 | 52.8 | 46.6 | 0.6 | 0.0 | 2848 | 7.6 | 0.1 | 2686 | 7.1 | 0.0 |
| Portugal | 4382 | 3382 | 1000 | 0 | 77.2 | 22.8 | 32.6 | 66.1 | 1.3 | 0.0 | 1155 | 19.4 | 0.3 | 457 | 13.6 | 0.0 |
| Romania | 2376 | 967 | 1408 | 1 | 40.7 | 59.3 | 22.5 | 60.0 | 17.1 | 0.4 | 771 | 21.3 | 0.1 | 294 | 16.7 | 0.7 |
| Russia | 57 621 | 15 612 | 30 092 | 11 917 | 34.2 | 65.8 | 40.1 | 56.8 | 3.0 | 0.1 | 15 044 | 17.7 | 0.4 | 8529 | 14.7 | 0.2 |
| Serbia | 227 | 223 | 4 | 0 | 98.2 | 1.8 | 12.8 | 26.9 | 60.4 | 0.0 | 69 | 23.5 | 4.4 | 9 | 0.0 | 0.0 |
| Slovenia | 2582 | 1362 | 1220 | 0 | 52.7 | 47.3 | 53.1 | 46.5 | 0.4 | 0.0 | 695 | 9.2 | 0.0 | 319 | 8.8 | 0.0 |
| Spain | 32 982 | 26 354 | 5385 | 1243 | 83.0 | 17.0 | 31.5 | 65.0 | 3.5 | 0.0 | 8378 | 17.0 | 0.2 | 6319 | 13.7 | 0.1 |
| Sweden | 9482 | 7065 | 2417 | 0 | 74.5 | 25.5 | 82.5 | 17.5 | 0.0 | 0.0 | 2746 | 3.0 | 0.1 | 1909 | 2.6 | 0.1 |
| Switzerland | 4253 | 3274 | 979 | 0 | 77.0 | 23.0 | 31.0 | 62.0 | 7.0 | 0.0 | 1053 | 15.6 | 0.5 | 808 | 15.0 | 0.2 |
| The Nederlands | ||||||||||||||||
| Ukraine | 6861 | 1863 | 4998 | 0 | 27.2 | 72.8 | 27.7 | 60.7 | 11.5 | 0.0 | 2571 | 21.9 | 0.2 | 2691 | 20.6 | 0.0 |
| UK | 36 986 | 15 572 | 21 414 | 0 | 42.1 | 57.9 | 54.7 | 42.0 | 3.3 | 0.0 | 11 927 | 11.2 | 0.2 | 5406 | 11.0 | 0.2 |
| All* | 376 348 | 153 513 | 108 756 | 116 646 | 59.1 | 41.9 | 41.5 | 51.9 | 6.2 | 0.4 | 95 765 | 14.9 | 0.3 | 51 219 | 11.9 | 0.2 |
Totals refer only to these countries where data on number of transferred embryos and on multiplicity were reported.
Percentages of cleavage and blastocyst stage transfers are calculated on the proportion of transfers where the day of transfer is known.
The day of transfer is unknown in 25.5%, 1.6%, 83.7%, 0.05%, 20.7% and 3.8% of all transfers in Denmark, Latvia, Lithuania, Romania, Russia and Spain, respectively.
Figure 2.
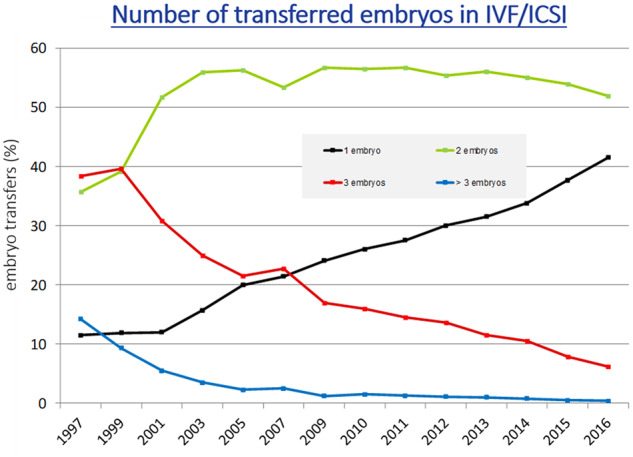
Number of embryos transferred in IVF and ICSI during fresh cycles in Europe, 1997–2016.
As a result of decreasing numbers of embryos replaced per transfer, the proportion of both twin and triplet deliveries continued to decline. In 2016, twin and triplet rates for fresh IVF and ICSI cycles together were 14.9% (range 1.1–35.7) and 0.3% (range 0–4.4), respectively. Corresponding results for FER were 11.9% and 0.2%. In the two countries with the highest rates of single embryo replacement in fresh cycles (84.3% for Iceland and 82.5% for Sweden), twin rates were as low as 1.1% and 3%, respectively.
Additional information on pregnancy and delivery data are provided in Supplementary Tables SXIII and SXIV. The reported incidence of pregnancy loss was 16.4% after IVF + ICSI (in 2015: 16.4%) and 18.6% after FER (in 2015: 20.6%). The proportion of lost to follow-up was 7.8% after IVF+ICSI (in 2015: 6.3%) and 7.5% after FER (in 2015: 7.4%).
Perinatal risks and complications
In 2016, data on premature deliveries were available from 18 countries (18 countries in 2015). Premature DR based on multiplicity are presented in Supplementary Table SXV. Data from fresh IVF and ICSI, FER and ED are pooled. The incidence of extreme preterm birth (20–27 gestational weeks at delivery) was 1.1% in singletons (1.3% in 2015), 3.3% in twins (3.7% in 2015) and 8.4% in triplets (13.4% in 2015). Very premature birth rates (28–32 gestational weeks at delivery) were recorded in 2.2% of singletons, 10.5% of twin pregnancies (in 2015: 9.9%) and 45% in triplet pregnancies (in 2015: 39.2%). The evolution of the proportion of premature deliveries before 37 weeks per embryo transfer according to multiplicity is shown in Fig. 3. Term deliveries (≥37 weeks) were achieved in 85.9% (86.4% in 2015) of singleton pregnancies, 44.1% (44.7% in 2015) of twin pregnancies and 8.8% (7.5% in 2015) of triplet pregnancies.
Figure 3.
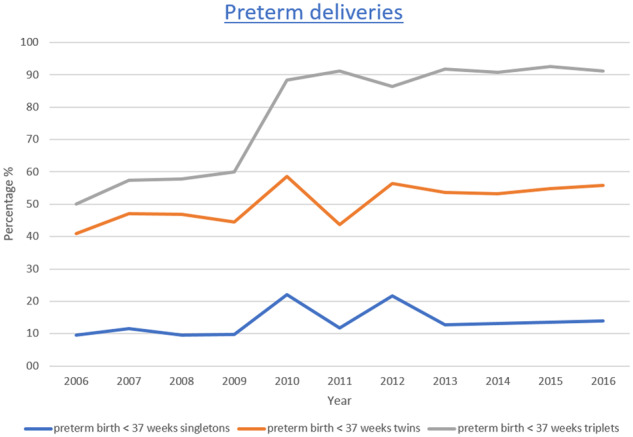
Proportion of premature deliveries (<37 weeks of gestation in relation to pregnancies ≥37 week of gestation) in singleton, in twin and in triplet pregnancies in Europe, 2006–2016.
Complications related to oocyte retrievals were reported by 33 countries (31 in 2015) and foetal reductions by 35 countries (26 in 2015) (Supplementary Table SXVI). The total number of reported cases of ovarian hyperstimulation syndrome (OHSS) (grades 3 to 5) was 1928, corresponding to a reported incidence of 0.21% (2167 cases in 2015; 0.25%). Other complications were less frequent (1471 cases) with a total reported incidence of 0.2% including 0.1% and 0.001% for bleeding and infection, respectively. No maternal death was reported in 2016 (2 out of 850 000 treatment cycles in 2015). A total of 553 foetal reductions were reported, the majority from UK, Belgium and Spain, as in 2015.
PGT/PGT-A
Table I includes PGT and PGT-A activities, which were reported from 22 countries (23 in 2015, 22 in 2014). The main contributors were Spain, Russia and Italy. The number of treatment cycles amounted to 27 069 representing 3.3% of initiated IVF + ICSI and FER cycles together (21 041; 2.8% in 2015). More details on PGT/PGT-A activities can be found in the annual reports of the ESHRE PGT consortium (De Rycke et al., 2017)
These treatments involved 19 461 fresh cycles and 7242 thawings, resulting in 5776 fresh and 6434 FER. In total, 2418 pregnancies (41.9% per transfer) and 1875 deliveries (32.5% per transfer) resulted from fresh cycles. Corresponding figures for FER were 2811 (43.7% per transfer) and 2259 (35.1% per transfer).
IVM
A total of 654 treatments with IVM were reported from eight countries (265 from eight countries in 2015) (Table I). Most IVM cycles were reported from Russia, as in 2015. A total of 391 transfers resulted in 103 pregnancies (26.3% per transfer) and 43 deliveries (11% per transfer).
FOR
A total number of 4878 thawing cycles were reported by 15 countries (4294 from 17 countries in 2015) (Table I) with Italy and Spain being the largest contributors (1460 and 1277 cycles, respectively). Among 3854 transfers, 1138 resulted in pregnancies (29.5%; 30.7% in 2015) and 808 in deliveries (21%; 20.6% in 2015).
IUI
For each participating country, the institutions performing and collecting data on IUI are listed in Table V. Data on IUI with husband semen (IUI-H, Supplementary Table SXVII) or using donors’ semen (IUI-D, Supplementary Table SXVIII) were collected by a total of 1197 institutions in 28 and 23 countries (25 and 21 in 2015, respectively. Among 113 450 IUI-H (139 050 in 2015) and 46 883 IUI-D (49 001 in 2015) reported cycles, the numbers were the highest for IUI-H in Spain, Italy and Belgium, and for IUI-D in Spain, Denmark and Belgium.
Table V.
IUI with husband (IUI-H) or donor (IUI-D) semen in 2016.
| Country | IUI-H |
IUI-D |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cycles | Deliveries | Deliveries (%) | Singleton (%) | Twin (%) | Triplet (%) | Cycles | Deliveries | Deliveries (%) | Singleton (%) | Twin (%) | Triplet (%) | |
| Albania | ||||||||||||
| Armemia | 275 | 68 | 24.7 | 79.6 | 20.4 | 0.0 | 48 | 11 | 22.9 | 88.9 | 11.1 | 0.0 |
| Austria | ||||||||||||
| Belarus | 1017 | 102 | 10.0 | 91.1 | 8.9 | 0.0 | 18 | 8 | 44.4 | 100.0 | 0.0 | 0.0 |
| Belgium | 12 296 | 904 | 7.4 | 95.2 | 4.6 | 0.1 | 8444 | 896 | 10.6 | 96.3 | 3.7 | 0.0 |
| Bosnia-Herzegovina, Federation part | 77 | 4 | 5.2 | 100.0 | 0.0 | 0.0 | ||||||
| Bulgaria | 2515 | 219 | 8.7 | 90.0 | 10.0 | 0.0 | 554 | 59 | 10.6 | 94.9 | 5.1 | 0.0 |
| Cyprus | ||||||||||||
| Czech Republic | ||||||||||||
| Denmark | 9977 | 1118 | 11.2 | 90.0 | 9.8 | 0.2 | 9390 | 569 | 6.1 | 94.4 | 5.5 | 0.2 |
| Estonia | 90 | 2 | 2.2 | 100.0 | 0.0 | 0.0 | 122 | 11 | 9.0 | 100.0 | 0.0 | 0.0 |
| Finland | 2936 | 249 | 8.5 | 1125 | 134 | 11.9 | ||||||
| France | 49 498 | 5254 | 10.6 | 90.4 | 9.4 | 0.2 | 2870 | 544 | 19.0 | 89.9 | 9.7 | 0.4 |
| Georgia | ||||||||||||
| Germany | ||||||||||||
| Greece | 3266 | 210 | 6.4 | 93.7 | 6.3 | 0.0 | 309 | 42 | 13.6 | 91.9 | 5.4 | 2.7 |
| Hungary | ||||||||||||
| Iceland | 69 | 6 | 8.7 | 100.0 | 0.0 | 0.0 | 167 | 21 | 12.6 | 100.0 | 0.0 | 0.0 |
| Ireland | 81 | 8 | 9.9 | 100.0 | 0.0 | 0.0 | ||||||
| Italy | 21 053 | 1531 | 7.3 | 91.2 | 8.2 | 0.6 | 714 | 98 | 13.7 | 83.7 | 11.2 | 5.1 |
| Kazakhstan | 2622 | 23 | 0.9 | 100.0 | 0.0 | 0.0 | ||||||
| Latvia | 103 | 13 | 12.6 | 100.0 | 0.0 | 0.0 | 64 | 5 | 7.8 | 100.0 | 0.0 | 0.0 |
| Lithuania | 246 | 15 | 6.1 | 100.0 | 0.0 | 0.0 | ||||||
| Luxembourg | 264 | 34 | 12.9 | 94.1 | 5.9 | 0.0 | 84 | 10 | 11.9 | 100.0 | 0.0 | 0.0 |
| Malta | ||||||||||||
| Moldova | 81 | 9 | 11.1 | 100.0 | 0.0 | 0.0 | ||||||
| Montenegro | 193 | 19 | 9.8 | 89.5 | 10.5 | 0.0 | ||||||
| Norway | 325 | 47 | 14.5 | 83.0 | 17.0 | 0.0 | 614 | 119 | 19.4 | 95.8 | 4.2 | 0.0 |
| North Macedonia | 1108 | 23 | 2.1 | 95.7 | 4.3 | 0.0 | 79 | 4 | 5.1 | 100.0 | 0.0 | 0.0 |
| Poland | 11 149 | 751 | 6.7 | 94.5 | 5.1 | 0.4 | 2053 | 225 | 11.0 | 91.7 | 7.9 | 0.5 |
| Portugal | 2095 | 190 | 9.1 | 85.7 | 13.8 | 0.5 | 185 | 42 | 22.7 | 92.9 | 7.1 | 0.0 |
| Romania | 2542 | 143 | 5.6 | 66.2 | 33.8 | 0.0 | 278 | 27 | 9.7 | 77.8 | 22.2 | 0.0 |
| Russia | 9106 | 1002 | 11.0 | 93.1 | 6.6 | 0.3 | 3897 | 545 | 14.0 | 93.4 | 6.3 | 0.4 |
| Serbia | 393 | 32 | 8.1 | 96.9 | 3.1 | 0.0 | ||||||
| Slovenia | 551 | 43 | 7.8 | 88.4 | 11.6 | 0.0 | ||||||
| Spain | 24 130 | 2404 | 10.0 | 90.5 | 9.2 | 0.3 | 12 333 | 1914 | 15.5 | 88.3 | 11.2 | 0.5 |
| Sweden | 1168 | 196 | 16.8 | 96.9 | 3.1 | 0.0 | ||||||
| Switzerland | ||||||||||||
| The Nederlands | ||||||||||||
| Ukraine | 1032 | 91 | 8.8 | 95.6 | 4.4 | 0.0 | 360 | 43 | 11.9 | 97.7 | 2.3 | 0.0 |
| UK | 4051 | 5398 | 707 | 13.1 | 92.6 | 6.8 | 0.6 | |||||
| All* | 162 948 | 14 495 | 8.9 | 91.0 | 8.8 | 0.3 | 50 467 | 6249 | 12.4 | 91.9 | 7.7 | 0.4 |
Total refers to these countries where data were reported, and mean percentage was computed on countries with complete information.
DR could be calculated for 109 399 IUI-H cycles (8.5% vs 7.8% in 2015) and 46 883 for IUI-D cycles (12% vs 12% in 2015).
Singleton deliveries were the most frequent regardless of the age group with an overall rate of 91.3% for IUI-H and 92% for IUI-D (90.6% in IUI-H, 92.1% in IUI-D in 2015). Twin and triplet rates were 8.4% and 0.3%, respectively for IUI-H, and 7.5% and 0.4% for IUI-D, respectively (in 2015: 8.9% and 0.5%, respectively for IUI-H and 7.3% and 0.6%, respectively for IUI-D).
Sum of fresh and FER (‘cumulative’) DR
Supplementary Table SXIX provides an estimate of a cumulative DR (different from a true cumulative DR including outcomes of all transfers performed from one aspiration). It was calculated as the ratio between the total number of deliveries from fresh embryo transfers and FER performed during a year (numerator) and the number of aspirations during the same year (denominator). The calculation included data from 38 countries (35 countries in 2015) where an overall rate of 29.6% was recorded. The benefit taken from additional FER (over the DR from fresh embryo transfers) was 10.5%, with the highest benefits recorded for Ukraine (+26.1%), Ireland (+19.6%), Finland and Albania (for both +18.1%) and the lowest for North Macedonia (+2.5%), Belarus (+1.6%) and Lithuania (0%).
Cross-border reproductive care
Ten countries reported data on cross-border patients: Albania, Belarus, Denmark, Greece, Montenegro, Portugal, Serbia, Slovenia, Spain and Switzerland. A total of 19 239 cycles (14 273 in 2015) were reported, 22.1% (29.4% in 2015) of which involved IVF/ICSI with the couple’s own gametes, 46.6% (47.1% in 2015) were oocyte donations and 21.8% (22.3% in 2015) were IVF or ICSI with semen donation. In addition, 7062 IUI with sperm donation (7714 in 2015) were registered. Information regarding the countries of origin was very incomplete and not reliable enough to obtain any conclusive information. The main reasons reported by patients were to have access to a technique not legally available in their home country (39.1%; 41.7% in 2015) or to seek a higher quality treatment (23.6%; 16.6% in 2015). In 13 291 cycles (mainly from Spain), there was another, not specified, reason to go abroad.
FP
For the first time data on FP are reported here. Eleven countries were able to provide data on a total number of 13 689 interventions (Supplementary Table SXX) in pre- and postpubertal patients, both for medical and non-medical reasons. The majority of interventions consisted of the cryopreservation of ejaculated sperm (n = 7877 from 11 countries) and the cryopreservation of oocytes (n = 4907 from eight countries). Ovarian tissue cryopreservation was reported by two and seven countries, respectively, for pre- and postpubertal patients with use of postpubertal tissue through transplantation reported in three countries (Greece, Portugal and Spain). Testicular tissue cryopreservation in postpubertal patients and prepubertal boys was reported from six countries and from France only (n = 124), respectively.
Discussion
This is the 20th annual report of the activity collected by EIM from European registries on ART, IUI and for the first time also on FP. From 1997 to 2016, the EIM of ESHRE has reported close to 10 million treatments cycles (9 772 904) that have led to the birth of more than 1.8 million infants.
Despite difficulties caused by the data collection system in a number of countries, the number of participating countries has increased over the years. The current report presents the analysis of data collected in 2016 from 40 European countries (38 in 2015) with Luxemburg providing data for the first time as a new EIM member. Non-EIM members are mainly smaller countries not offering ART services (n = 5), except for Azerbaijan and Kosovo. Amongst EIM members, Croatia, Georgia, Slovakia and Turkey did not deliver data most likely due to organizational problems or local regulatory problems (Calhaz-Jorge et al., 2020).
Excluding the five small European countries in which ART is not available, the rate of participation at the country level is as high as 87% of European countries (90.9% of EIM members) while at the level of IVF clinics, the proportion of those reporting data sets is 91.8% (vs 90.6% in 2015; De Geyter et al., 2020). Although the participation of some of the countries fluctuated over time, reported ART treatment numbers are on a continuous rise (+8% as compared to 2015) as are the infants born from ART (+4.4% compared to 2015).
Moreover, although the level of completeness is highly variable among countries, 20 countries were able to present data from all IVF clinics (in 2015: 18 and in 2014: 14 countries). Efforts to achieve increased participation and higher completeness of the data aim at an improved transparency and vigilance in reproductive care. However, because of the variety in collection systems, absence or limited presence of data validation methods, differences in definitions of collected items and country-specific practices (e.g. freeze all cycles, embryo transfer policy) that may, among other reasons, be influenced by economic issues, interpretation of the data should remain cautious. Progress towards harmonization of data collections could prove helpful in the future to achieve a higher quality of outcome data for professionals but also for other stakeholders involved in societal, political and economic decisions in medically assisted reproduction (MAR), as well as tissue and cell banking for FP.
Access to care is one of the important and very relevant pieces of information generated by the EIM. Considering that it was estimated that 1500 ART cycles per million inhabitants per year should cover the needs in infertility care (The ESHRE Capri Workshop group, 2008), we noticed that 60% of the countries in which complete data sets were available (12 out of 20) reached this level of access in 2016 (vs 55.6% in 2012, 64.3% in 2014 and 61.1% in 2015). Using the number of women of reproductive age as the denominator and eliminating thereby the impact of age differences among countries, access to care (based on all types of cycles) appeared highly variable, ranging from 1726 to 15 917 cycles per women aged 15–45 years. As the population needs in ART were estimated at a time when FER was not current practice (2001), any interpretation of treatment availability should be cautious. Indeed, FER cycles were included in the calculation on availability and represent a quite high proportion of ART cycles nowadays (in 2016, 44.1% of ART cycles when fresh IVF+ICSI cycles are used as the denominator). Moreover, considering that cross-border care may have an impact on accessibility in some countries, data interpretation will remain difficult before full traceability of all MAR procedures becomes available.
Considering the different treatment modalities, ICSI remains the most used and seems to have stabilized in recent years (Table I;Fig. 1), whereas FER is the second most used technique with a progressive increase over the years in the proportion of FER relative to fresh IVF and ICSI cycles (37.8% in 2014, 40.3% in 2015 and 44% in 2016). Changes in ART practices with higher numbers of freeze all cycles, a reduced number of embryos replaced per transfer and higher survival rates of cryopreserved embryos with the implementation of vitrification (Rienzi et al., 2017) may all explain this evolution. While freeze all cycles have been registered since 2014, showing a 42% increase in reported cycles in 2016 compared to 2015 (Supplementary Table SV), the distinction between techniques of cryopreservation could not be registered by EIM. Enhanced reporting of IVM, PGT, ED and FOR in 2016 may be a reflection of the increased use of these treatment modalities. Expanding the data collection in large registries such as EIM for techniques like IVM and PGT-A, or to other new techniques or laboratory adjuncts (Harper et al., 2017), could help to underscore analysis of their efficacy and safety in the future.
Owing to segmentation of treatments (i.e. treatment is not always a continuous sequence of single procedures but may, for example, include several oocyte retrievals for one transfer or several transfers for frozen cycles), such as for freeze all cycles, and the implementation of new technologies in ART, the cumulative DR per cycle or per aspiration will become the most important outcome indicator of treatment effectiveness. To date, the EIM has gathered data on an aggregate basis precluding thereby the calculation of true cumulative livebirths rates. Hence, as a surrogate indicator or proxy of true cumulative rates, fresh and FER during the same calendar year have been considered. Based on data from 38 countries, cumulative DR reached 29.6% during a 1-year period with a multiple DR of 13.8% and a rate of single embryo transfers of 41.5% in 2016. The absence of a link between cryopreserved embryos and their original cycle, and the limited observation period of 1 year where an unknown number of ART cycles was performed, do not allow comparisons with other registries. However, after seven consecutive ART cycles (fresh and frozen-thawed embryo transfer cycles counted consecutively) the 2011 data registered by the National Perinatal Epidemiology and Statistics Unit for Australia–New Zealand, including 73.2% single embryo transfers, showed a cumulative livebirth rate of 41.1% and a multiple DR of only 6.9% (National Perinatal Epidemiology and Statistics Unit, https://npesu.unsw.edu.au).
Besides local regulations and economic issues that may restrict treatment strategies, the improved awareness of ART outcomes by patients and physicians should guide future decisions. In this regard, the reduction in the number of embryos replaced in a cycle is a main trend that has been recorded by the EIM registry over the years (Fig. 2). While the transfer of two embryos remains the most frequently performed approach (51.9% of the transfers), single embryo transfers (whether elective or not) represented 41.5% of the transfers in 2016 and were carried out in the majority of treatment cycles for 10 of the countries. Transfers of four or more embryos were performed in very few countries and represent only 0.4% of all transfers. The evolution of the transfer policies in clinics often parallels the implementation of embryo culture to the blastocyst stage. However, the quality of evidence to support blastocyst transfers is still low (Glujovsky et al., 2016). For the first time in 2016, EIM data collection allowed separate analysis of blastocyst and cleavage stage embryo transfers, showing that the majority of embryos were transferred at the blastocyst stage (41.9% for fresh IVF + ICSI and 62.2% for FER). Although figures are not available for DR yet, PR per transfer were the highest for blastocysts (39.7% vs 28.3% for cleavage stage embryos). Keeping in mind that the objective of an IVF/ICSI treatment is the delivery of a single healthy child, with a twin pregnancy being regarded as a complication (Land and Evers, 2003), further progress towards a reduction of prematurity associated with multiple births should be obtained at the expense of a reduced proportion of double embryo transfers. Indeed, whereas triplet rates remain low after a significant drop over the years (Ferraretti et al., 2017), twin rates did not follow the same decreasing slope and the resulting prematurity (≤37 weeks) was still observed in more than half of the deliveries. Compared to singleton deliveries the risk of extreme prematurity was increased by 3-fold and of very preterm birth by nearly 5-fold for twin deliveries. Rates of twins and triplets were slightly lower after FER than after fresh IVF + ICSI treatments, which could also contribute to the decreasing multiple deliveries recorded in the recent years. Furthermore, the practice of foetal reduction for the prevention of multiple births was reported by 35 countries. However, it is not known which of these approaches is having the real impact on the reduction of multiples.
Regarding other safety aspects, no maternal death after ART was reported in 2016 (Supplementary Table SXVI) and the proportions of OHSS, infections and haemorrhage were low and quite stable over time although it is assumed that the complications of ART remain generally underreported.
The future of MAR registries should focus on the health of infants as an increasing number of children are born after ART, with incidences as high as 5.1% of all newborns in Denmark and 7.7% in Spain in 2016. Moreover, considering the increasing use of ED, FOR and the extension of using FP measures for medical reasons to non-medical indications, including planned postponement of motherhood, we may expect ART to contribute more and more to demography. Hence, transparency and vigilance in ART will more than ever be essential to all stakeholders with, as a main requirement, the need to level up the quality of collected data. Prospective compulsory registration systems, including an international coding system to follow gametes and embryos across country borders, should therefore become available to countries rather than the current retrospective aggregate data registration (De Geyter et al., 2016; Kissin et al., 2019).
Authors’ roles
V.G. performed the calculations. C.W. wrote the manuscript. All other co-authors reviewed the final manuscript and made appropriate corrections and suggestions to improve it. In all, this document represents a fully collaborative work.
Funding
The study has no external funding; all costs are covered by ESHRE.
Conflict of interest
There are no competing interests.
Supplementary Material
Appendix
Contact persons who are collaborators and represent the data collection programmes in participating European countries, 2016.
Albania
Prof. Orion Gliozheni, University Hospital for Obstetrics & Gynecology, Department of Obstetrics & Gynecology, Bul. B. Curri, Tirana, Albania. Tel: +355 4222 36 32; Fax: +355 42 257 688; Mobile: +355 68 20 29 313; E-mail: glorion@abcom.al
Armenia
Mr Eduard Hambartsoumian, Fertility Center, IVF Unit, 4 Tigvan Nets, 375 010 Yerevan, Armenia. Tel: +374 10 544 368; E-mail: hambartsoumian@hotmail.com
Austria
Prof. Dr Heinz Strohmer, Dr Obruca & Dr Strohmer Partnerschaft Goldenes Kreuz-Kinderwunschzentrum, Lazarettgasse 16-18, 1090 Wien, Austria. Tel: +43 401 111 400; Fax: +43 401 111 401; E-mail: heinz.strohmer@kinderwunschzentrum.at
Belarus
Dr Elena Petrovskaya (Alena Piatrouskaya), ART centre ‘Embryo’, Filimonova 53, 220053 Minsk, Belarus. Tel: +375 293 830 570; Email: elenaembryoby@gmail.com
Dr Oleg Tishkevich, Centre For Assisted Reproduction ‘Embryo’ Belivpul, Filimonova Str. 53, 220 114 Minsk, Belarus. Tel: +375 296 222 722; Fax: +375 172 376 404; Mobile: +375 296 222 722; E-mail: tishol@tut.by
Belgium
Dr Kris Bogaerts, I-Biostat, Kapucijnenvoer 35 bus 7001, 3000 Leuven, Belgium. Tel: +32 (0) 16 33 68 90; Fax: +32 (0) 16 33 70 15; E-mail: kris.bogaerts@med.kuleuven.be
Prof. Christine Wyns, Gynaecology-Andrology, Cliniques Universitaires Saint Luc, Service FIV- Andrology, Université Catholique de Louvain; Av. Hippocrate, 10, 1200 Brussels, Belgium. Tel: +32 27646576; Fax: +32 27649050; Mobile: +32 477943374; E-mail: christine.wyns@uclouvain.be
Bosnia
Professor Dr Devleta Balic, Zavod za humanu reprodukciju ‘Dr Balic’, Kojsino 25, 75000 Tuzla, Bosnia, Herzegovina. Tel: +387 35 260 650; Mobile: +387 611 402 22; E-mail: drbalic@bih.net.ba
Bulgaria
Irena Antonova, ESHRE certified clinical embryologist (2011), Ob/Gyn Hospital Dr Shechterev, 25–31, Hristo Blagoev Strasse, 1330 Sofia, Bulgaria. Tel: +359 887 127 651; E-mail: irendreaming@gmail.com
Cyprus
Dr Michael Pelekanos, AKESO Fertility Centre, 1, Pavlou Nirvana strasse, 3021 Limassol, Cyprus. Tel: +357 99645333; Fax: +357 25824477; Mobile: +30 6944248433; E-mail: pelekanos@akeso.com
Czech Republic
Dr Karel Rezabek, Medical Faculty, University Hopsital, CAR-Assisited Reproduction Center, Gyn/Ob Department, Apolinarska 18, 12000 Prague, Czech Republic. Tel: +420 224 967 479; Fax: +420 224 922 545; Mobile: +420 724 685 276; E-mail: rezabek.ivf@seznam.cz
Mgr. Jitka Markova, Institute of Health Information and Statistics of the Czech Republic, Palackeho namesti 4, 12801 Prague, Czech Republic. Tel: +420 224 972 832; Mobile: +420 721 827 532; E-mail: jitka.markova@uzis.cz
Denmark
Dr Josephine Lemmen, Vitanova, Fertility clinic, Vester Voldgade 106, 1552 Copenhagen, Denmark. Tel: +45 333 371 01; E-mail: jglemmen@gmail.com
Estonia
Dr Deniss Sõritsa, Tartu University Hospital and Elitre Clinic, Tartu, Estonia. Tel: +372 740 9930; Fax: +372 740 9931; E-mail: soritsa@hotmail.com
Finland
Prof. Mika Gissler, THL National Institute for Health and Welfare, PO Box 30, 00271 Helsinki, Finland. Tel: +385 29 524 7279; E-mail: mika.gissler@thl.fi
Dr Sari Pelkonen, Oulu University Hospital, departement of Obstetrics and Gynaecology, PO Box 23, 90029 Oys, Finalnd. Tel:+358 8 3153040; E-mail: sari.pelkonen@fimnet.fi
France
Dr Fabienne Pessione, Agence de la biomedecine, 1 av stade de France, 93 Saint Denis, France. Tel: +33 1 5593 69 46; E-mail: fabienne.pessione@biomedecine.fr
Prof. Jacques de Mouzon, 15–29 rue Guilleminot, 75014 Paris, France. Tel: +33 143 224 679; Mobile: +33 662 062 274; E-mail: jacques.de.mouzon@gmail.com
Germany
Dr Andreas Tandler, Schneider, Fertility Center Berlin, Spandauer damm 130, 14050 Berlin, Germany. Tel: +49 30 233 20 81 10; Fax: +49 30 233 20 81 19; E-mail: tandler-schneider@fertilitycenter-berlin.de
Greece
Prof. Sophia Kalantaridou; National Authority of Medically Assisted Reproduction, Ploutarxou 3, PO 10675 Athens. Tel: +30 213 2072000; E-mail: secretary@eaiya.gov.gr
Hungary
Prof. Janos Urbancsek, Semmelweis University, 1st Dept. of Ob/Gyn, Baross utca 27, 1088 Budapest, Hungary. Tel: +36 1 266 01 15; Fax: +36 1 266 01 15; E-mail: urbjan@noi1.sote.hu
Prof. G. Kosztolanyi, University of Pecs, Department of Medical Genetics and Child Development, Jozsef A.u, 7., 7623 Pecs, Hungary. Tel: +36 7 2535977; Fax: +36 7 2535972; E-mail: gyorgy.kosztolanyi@aok.pte.hu
Iceland
Mr Hilmar Bjorgvinsson, IVF Klinikin Reykjavik, Alfheimum 74, 104 Reykjavik, Iceland. Tel: +354 430 4000; Fax: +354 430 4040; E-mail: Hilmar.bjorgvinsson@ivfklinikin.is
Ireland
Dr Edgar Mocanu, Human Assisted Reproduction Ireland Rotunda Hospital, HARI Unit, Master’s House, Parnell Square, 1 Dublin, Ireland. Tel: +353 180 72 732; Mobile: +353 86 818 839; Fax: +353 18 727 831; E-mail: emocanu@rcsi.ie
Jennifer Cloherty, Galway Fertility, Western distribution Road, Rahoon, Ireland. Tel: 35361476800; E-mail: JCloherty@GFU.ie
Italy
Dr Giulia Scaravelli, Istituto Superiore di Sanità, Registro Nazionale della Procreazione Medicalmente Assistita, CNESPS, Viale Regina Elena, 299, 00161 Roma. Tel: +3906 499 04 050; Fax: +39064 99 04 324; E-mail: giulia.scaravelli@iss.it
Dr Roberto de Luca, Istituto Superiore di Sanità, Registro Nazionale della Procreazione Medicalmente Assistita, CNESPS, Viale Regina Elena, 299, 00161 Roma. Tel: +3906 499 04 320; E-mail: roberto.deluca@iss.it
Kazakhstan
Prof. Dr Vyacheslav Lokshin, International Clinical Center for Reproductology ‘Persona’, Utepova street 32a, 00506 Almaty, Kazakhstan. Tel: +7 727 382 7777; Mobile: +7 701 755 8209; E-mail: v_lokshin@persona-ivf.kz
Dr Sholpan Karibayeva, International Clinical Center for Reproductology ‘Persona’, Utepova Street 32a, 00506 Almaty, Kazakhstan. Tel: +7 727 382 7777; E-mail: sh.karibaeva@gmail.com
Latvia
Dr Valeria Magomedova, Jusu Arsti Private Clinic, Apuzes 14, 1046 Riga, Latvia. Tel: +371 678 700 29; Fax: +371 678 704 29; E-mail: godunova@inbox.lv
Lithuania
Raminta Bausyte, Vilnius University Hospital Santaros Clinics, Santaros Fertility Center, Simono Staneviciaus 64-69, 07113 Vilnius, Lithuania. Tel: +370 620 86826; E-mail: raminta.bausyte@gmail.com
Ieva Masliukaite, Academic Medical Center, Center for Reproductive Medicine, Ijburglaan, 1086ZJ Amsterdam, The Netherlands. Tel: +31 653 688 815; E-mail: i.masliukaite@amc.uva.nl
Luxembourg
Dr Caroline Schilling, Centre Hospitalier de Luxembourg, Centre de Stérilité et de Médecine de Reproduction, Rue Fiederspiel 2, 1512 Luxembourg, Luxembourg. Tel: +352 44 11 32 30; Mobile: +352 66 13 13 912; E-mail: schilling.caroline@chl.lu
Malta
Dr Jean Calleja-Agius, University of Malta, 12, Mon Nid, Gianni Faure Street, TXN2421 Tarxien, Malta. Tel: +356 216 930 41; Mobile: +356 995 536 53; E-mail: jean.calleja-agius@um.edu.mt
Moldova
Prof. Dr Veaceslav Moshin, Medical Director at Repromed Moldova, Center of Mother @ Child protection, State Medical and Pharmaceutical University ‘N.Testemitanu’, Bd. Cuza Voda 29/1, Chisinau, Republic of Moldova. Tel: +37322 263855; Mobile: +37369724433; E-mail: mosin@repromed.md; veaceslavmoshin@yahoo.com
Montenegro
Dr Tatjana Motrenko Simic, Human Reproduction Center Budva, Prvomajska 4, 85310 Budva, Montenegro. Tel: +382 33402432; Mobile: +382 69 052 331; E-mail: motrenko@t-com.me
Dragana Vukicevic, Hospital ‘Danilo I’, Humana reprodukcija, Vuka Micunovica bb, 86000 Cetinje, Montenegro. Tel: +382 675 513 71; E-mail: vukicevic.dragana@yahoo.com
The Netherlands
Dr Jesper M.J. Smeenk, St Elisabeth Hospital Tilburg, Department of Obstetrics and Gynaecology, Hilv, The Netherlands. Tel: +31 13 539 31 08; Mobile: +31 622 753 853; E-mail: j.smeenk@elisabeth.nl
North Macedonia
Mr Zoranco Petanovski, Hospital ReMedika, Nas. Zelezara, 1000 Skopje, Macedonia. Tel: +389 224 475 45; Fax: +389 226 031 00; E-mail: zpetanovski@yahoo.com
Norway
Dr Liv Bente Romundstad, Spiren Fertility Clinic, Nardoskrenten 11, 7032 Trondheim, Norway. Tel: +47 73523000; Mobile: +47 90550207; E-mail: libero@klinikkspiren.no
Poland
Dr Anna Janicka, VitroLive, Wojska Polskiego 103, 70-483 Szczecin, Poland. Tel: +48 91 88 69 260; E-mail anna.janicka@vitrolive.pl
Portugal
Prof. Dr Carlos Calhaz-Jorge, CNPMA, assembleia da Republica, Palacio de Sao Bento, 1249-068 Lisboa, Portugal. Tel: +351 21 391 93 03; Fax: +351 21 391 75 02; E-mail: calhazjorgec@gmail.com
Ms Joana Maria Mesquita Guimaraes, Hospital Geral Santo Antonio, Largo Professor Abel Salazar, 4050-011 Porto, Portugal. Tel: +351 96 616 02 37; E-mail: joanamesquitaguimaraes@gmail.com
Ms Ana Rita Laranjeira, CNPMA, Assembleia da Republica, Palaio de Sao Bento 1249-068 Lisboa, Portugal. Tel: +351 21 391 93 03; Fax: +351 21 391 75 02; E-mail: cnpma.correio@ar.parlamento.pt
Romania
Mrs Ioana Rugescu, Gen Secretary of AER Embryologist association and Representative for Human Reproduction Romanian Society. Tel: +40744500267; E-mail: irugescu@rdsmail.ro
Dr Bogdan Doroftei; University of Medicine and Pharmacy Iasi; Teaching Hospital Obgyn ‘Cuza Voda’, Cuza Voda Str. 34, 700038 Iasi, Romania. Tel: +40 232 213 000/int. 176; Mobile: +40 744 515 297; E-mail: bogdandoroftei@gmail.com; bogdan.doroftei@umfiasi.ro
Russia
Dr Vladislav Korsak, International Center for Reproductive Medicine, General Director, Liniya 11, Building 18B, Vasilievsky Island, 199034 St-Petersburg, Russia C.I.S. Tel: +7 812 328 2251; Fax: +7 812 327 19 50; Mobile: +7 921 9651977; E-mail: korsak@mcrm.ru
Serbia
Prof Nebojsa Radunovic, Institute for Obstetrics and Gynecology,Visegradska 26, 11000 Belgrade, Serbia. Tel: +38 111 361 55 92; Fax: +38 111 361 56 03; Mobile: +381 63 200 204; E-mail: radunn01@gmail.com
Dr Sci. Nada Tabs, Klinika za ginekologiju i akuserstvo, Klinicki centar Vojvodine, Branimira Cosica 37, 21000 Novi Sad, Serbia. Mobile: +381 63 50 81 85; E-mail: nada.tabs@yahoo.com
Slovenia
Prof. Irma Virant-Klun, University Medical Centre Ljubljana, Department of Obstetrics and Gynecology, Slajmerjeva 3, 1000 Ljubljana, Slovenia. Tel: +386 1 522 60 13; Fax: +386 1 431 43 55; Mobile: +38631625774; E-mail: irma.virant@kclj.si
Spain
Mrs Irene Cuevas Saiz, Hospital General de Alicante, Infertility Dept., Av Pintor Baeza, 12, 03010 Valencia, Spain. Tel: +34 961972000; Fax: +34 91 799 4407; Mobile: +34 677245650; E-mail: cuevas_ire@gva.es
Dr Fernando Prados Mondéjar, Hospital de Madrid-Montepríncipe, HM Fertility Center Monteprincipe, C/Montepríncipe 25, 28660 Boadilla del Monte, Spain. Tel: +34 917 089 931; Mobile: +34 646 737 237; E-mail fernandojprados@gmail.com
Sweden
Prof. Christina Bergh, Sahlgrenska University Hospital, Department of Obstetrics and Gynaecology, Bla Straket 6, 413 45 Göteborg, Sweden. Tel: +46 31 3421000; +46 736 889325; Fax: +4631 418717; Mobile: +46 736 889325; E-mail Christina.bergh@vgregion.se
Switzerland
Ms Maya Weder, Administration FIVNAT, Postfach 754, 3076 Worb, Switzerland. Tel: +41 (0)31 819 76 02; E-mail: fivnat@fivnat-registry.ch
Dr med. Marco Buttarelli, Centro Cantonale di Fertilità, Ospedale Regionale di Locarno ‘La Carità’, Via all’Ospedale 1, 6600 Locarno, Switzerland. Tel: +41 91 811 45 38; E-mail: fivnat@fivnat-registry.ch
Dr Marie-Pierre Primi, Laboratoire Andrologie et Biologie de la Reproduction (LABR), Unité de Médecine de la Reproduction, Maternité 07, CHUV, 1011 Lausanne, Switzerland. Tel: +41 21 314 34 26; E-mail: fivnat@fivnat-registry.ch
UK
Mr Howard Ryan, Data Analyst H.F.E.A, 10 Spring Gardens, London SW1A 2BU, UK. Tel: +44 (0)20 7291 8203; E-mail: howard.ryan@HFEA.GOV.UK
Mr Richard Baranowski, Deputy Information Manager, Human Fertilization and Embryology Authority (HFEA), Finsbury Tower, 103-105 Bunhill Row, London EC1 Y 8HF, UK. Tel: +44 (0) 20 7539 3329; Fax: +44 (0) 20 7377 1871; E-mail: richard.baranowski@hfea.gov.uk
Ukraine
Professor Dr Mykola Gryshchenko, IVF Clinic Implant Ltd, Academician V.I.Gryshchenko Clinic for Reproductive Medicine, 25 Karl Marx Str., 61000 Kharkiv, Ukraine. Tel: +380 57 124522; Fax: +380 57 705070703; Mobile: +380 57 705070703; E-mail: nggryshchenko@gmail.com
Contributor Information
The European IVF-monitoring Consortium (EIM)‡ for the European Society of Human Reproduction and Embryology (ESHRE):
Orion Gliozheni, Eduard Hambartsoumian, Heinz Strohmer, Elena Petrovskaya, Oleg Tishkevich, Kris Bogaerts, Christine Wyns, Devleta Balic, Irena Antonova, Michael Pelekanos, Karel Rezabek, Jitka Markova, Josephine Lemmen, Deniss Sõritsa, Mika Gissler, Sari Pelkonen, Fabienne Pessione, Jacques de Mouzon, Andreas Tandler, Sophia Kalantaridou, Janos Urbancsek, G Kosztolanyi, Hilmar Bjorgvinsson, Edgar Mocanu, Jennifer Cloherty, Giulia Scaravelli, Roberto de Luca, Vyacheslav Lokshin, Sholpan Karibayeva, Valeria Magomedova, Raminta Bausyte, Ieva Masliukaite, Caroline Schilling, Jean Calleja-Agius, Veaceslav Moshin, Tatjana Motrenko Simic, Dragana Vukicevic, Jesper M J Smeenk, Zoranco Petanovski, Liv Bente Romundstad, Anna Janicka, Carlos Calhaz-Jorge, Joana Maria Mesquita Guimaraes, Ana Rita Laranjeira, Ioana Rugescu, Bogdan Doroftei, Vladislav Korsak, Nebojsa Radunovic, Nada Tabs, Irma Virant-Klun, Irene Cuevas Saiz, Fernando Prados Mondéjar, Christina Bergh, Maya Weder, Marco Buttarelli, Marie-Pierre Primi, Howard Ryan, Richard Baranowski, and Mykola Gryshchenko
References
- Calhaz-Jorge C, De Geyter CH, Kupka MS, Wyns C, Mocanu E, Motrenko T, Scaravelli G, Smeenk J, Vidakovic S, Goossens V.. Survey on ART and IUI: legislation, regulation, funding and registries in European countries: The European IVF-monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). Hum Reprod Open 2020;2020:hoz044.eCollection 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Geyter Ch, Wyns C, Mocanu E, de Mouzon J, Calhaz-Jorge C.. Data collection systems in ART must follow the pace of change in clinical practice. Hum Reprod 2016;31:2160–2163. [DOI] [PubMed] [Google Scholar]
- De Geyter C, Calhaz-Jorge C, Kupka MS, Wyns C, Mocanu E, Motrenko T, Scaravelli G, Smeenk J, Vidakovic S, Goossens V; European IVF-monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). ART in Europe, 2015: results generated from European registries by ESHRE. Hum Reprod Open 2020;2020:hoz038. eCollection 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Rycke M., Goossens V., Kokkali G. Meijer-Hoogeveen M, Coonen E, Moutou C; ESHRE PGD Consortium data collection XIV-XV: cycles from January 2011 to december 2012 with pregnancy follow-up to October 2013. Hum Reprod 2017;32:1974. 10.1093/humrep/dex265. [DOI] [PubMed] [Google Scholar]
- Ferraretti AP, Nygren K, Andersen AN1, de Mouzon J, Kupka M, Calhaz-Jorge C, Wyns C, Gianaroli L, Goossens V; European IVF-Monitoring Consortium (EIM), for the European Society of Human Reproduction and Embryology (ESHRE). Trends over 15 years in ART in Europe: an analysis of 6 million cycles. Hum Reprod Open 2017;2017:hox012. eCollection 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glujovsky D, Farquhar C, Quinteiro Retamar AM, Alvarez Sedo CR, Blake D.. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev 2016;6:CD002118. [DOI] [PubMed] [Google Scholar]
- Harper J, Jackson E, Sermon K, Aitken RJ, Harbottle S, Mocanu E, Hardarson T, Mathur R, Viville S, Vail A, Lundin K.. Adjuncts in the IVF laboratory: where is the evidence for ‘add-on’ interventions? Hum Reprod 2017;32:485–491. [DOI] [PubMed] [Google Scholar]
- Kissin DM, Adamson GD, Chambers G, De Geyter C (eds). Assisted Reproductive Technology Surveillance. Cambridge, UK: Cambridge University Press, 2019. [Google Scholar]
- Land JA, Evers JL.. Risks and complications in assisted reproduction techniques: Report of an ESHRE consensus meeting. Hum Reprod 2003;18:455–457. [DOI] [PubMed] [Google Scholar]
- Rienzi L, Gracia C, Maggiulli R, LaBarbera AR, Kaser DJ, Ubaldi FM, Vanderpoel S, Racowsky C. Oocyte, embryo and blastocyst cryopreservation in ART: systematic review and meta-analysis comparing slow-freezing versus vitrification to produce evidence for the development of global guidance. Hum Reprod Update 2017;23:139–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The ESHRE Capri Workshop Group. Genetic aspects of female reproduction. Hum Reprod Update 2008;14:293. [DOI] [PubMed] [Google Scholar]
- Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, Rienzi L, Sunde A, Schmidt L, Cooke ID, et al. The international glossary on infertility and fertility care. HumReprod 2017; 2:1786. 10.1093/humrep/dex234 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.