Abstract
Emergence from anesthesia can be associated with a wide spectrum of cognitive and behavioral dysregulation in children, including delirium or acute brain dysfunction. This period of neurobehavioral recovery can be further confounded by pain, anxiety, and fear. The implementation of monitoring for level of consciousness, pain, and delirium using valid pediatric tools is necessary to avoid misdiagnosis due to overlapping symptomatology and support appropriate management. Understanding the epidemiology of delirium in the postoperative setting will require consistent use of accurate terminology in the medical literature. The current interchangeable use of the terms “emergence agitation” and “emergence delirium” needs to be highlighted and awareness of differences in patient conditions and assessment tools is essential. We discuss epidemiology of emergence agitation and delirium in the pediatric population, and the challenges for future delineation of monitoring and management. Furthermore, we describe the possible impact of long-term consequences of emergence delirium among infants and children, and the necessary areas of future research.
Keywords: emergence, delirium, agitation, excitation, pediatrics, postoperative, sedation, perioperative
Clinical Case
A 3-year-old anxious male with obstructive sleep apnea presents for tonsillectomy and adenoidectomy. His intraoperative anesthetic care includes an inhalational induction with nitrous oxide/oxygen/sevoflurane, followed by intravenous (IV) catheter placement, intubation, and maintenance of general anesthesia with sevoflurane and analgesia with opioid administration. Upon emergence in the PACU, he is thrashing about in the bed, crying, and not following commands.
Introduction
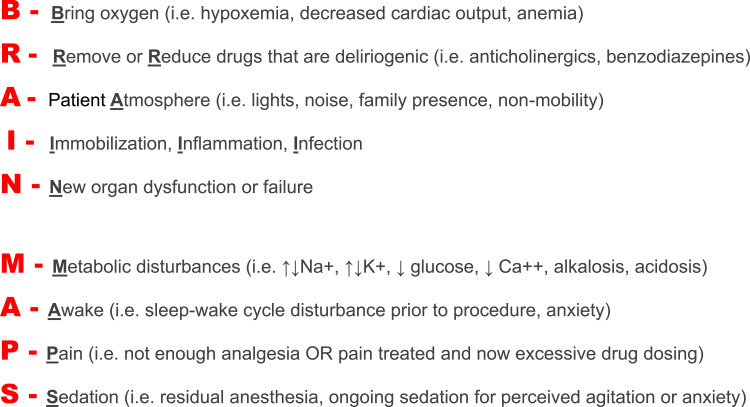
Emergence from general anesthesia can be complicated by alterations in level of consciousness and mental status, often encompassing disruptive behaviors observed during the immediate post-anesthesia period particularly in pediatric patients. In the 1960s, Eckenhoff et al first described their observations of “neurologic excitement” during emergence from general anesthesia, with patients being in a dissociated state of consciousness.1 This period of behavioral dysregulation has been interchangeably referred to as emergence excitation, emergence agitation (EA), and emergence delirium (ED). However, these terms are not synonymous with one another. Agitation is an “unpleasant state of extreme arousal”,2,3 and can be a commonly observed symptom in patients suffering from pain, anxiety, fear, and more complex neurobehavioral syndromes such as delirium. Pediatric patients commonly exhibit oppositional behaviors in the setting of unfamiliar stressors; therefore, postoperative agitation alone will not always suggest delirium.4 Delirium, or acute brain dysfunction, is defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM) as a disturbance of consciousness and cognition characterized by an acute change or fluctuating course of mental status or awareness, a cardinal feature of inattention, and the inability to receive, process, store, or recall information.2,5 Delirium or acute brain dysfunction occurs in the setting of systemic disease or derangement such as hypoxia, hypotension, electrolyte abnormality, or as a consequence of sedation choice/duration (BRAIN MAPS6). (Figure 1) Whereas in the anesthesia literature, emergence delirium (ED) is described as a state of mental confusion, agitation, and disinhibition marked by some degree of hyperexcitability during recovery from general anesthesia.7 In order to promote greater understanding of the neuropsychiatric recovery of infants and children during the complex process of emergence, applying well defined, standard terms should be paramount.4 The goal becomes using tools that distinguish between conditions that may have similar symptoms or behaviors (agitation, pain, delirium) so that the epidemiology of the post-anesthesia period can be better understood and, more importantly, patients can receive the appropriate care.
Figure 1.
Consideration of causes for delirium “BRAIN MAPS”.6 Delirium develops due to various disease states or imbalances that lead to acute brain dysfunction. Much emphasis has been placed on excessive sedation/anesthesia as a first-line cause of delirium. However, it should be highlighted that common postoperative complications such as hypoxia, hypoventilation, pain, and foreign patient atmosphere/caregivers may be prevalent and delirium being a sensitive and early sign of possible postoperative problems. BRAIN MAPS can be used to quickly review possible delirium causes. Reproduced from Smith HAB, Brink E, Fuchs C, Ely EW, Pandharipande PP. Pediatric delirium: monitoring and management in the pediatric intensive care unit. Pediatr Clin North Am. 2013;60(3):741–760. doi:10.1016/j.pcl.2013.02.010, with permission from Elsevier.6
Delirium Subtypes
In the setting of delirium, the imbalance in excitatory and inhibitory neurotransmission can lead to non-specific manifestations consisting of a wide-range of behaviors observed across afflicted patients.6 The continuum of manifestations can complicate diagnosis when a valid delirium screening tool is not used. These same manifestations are used to categorize delirium into subtypes including hyperactive, hypoactive, and mixed.8
Patients with hyperactive delirium are often more readily identified because they exhibit characteristic heightened psychomotor behaviors or “positive symptomatology,” ranging from mild agitation to combativeness, or even psychosis. Although hyperactive delirium may be more easily recognized, it is the least common form of both adult and pediatric ICU-delirium (<10%).8–10 The traditional terms of Emergence Agitation and Emergence Delirium may be consistent with hyperactive delirium in some patients following anesthesia, however, the current assessment tools used in the PACU do not all specifically rely on DSM criteria for delirium diagnosis. Indeed, the presence of agitation alone is not imperative for the diagnosis of delirium, rather agitation is a symptom. Though agitated patients require immediate hands-on management within the PACU, the discernment of etiology remains an important challenge for anesthesia and critical care clinicians.
Patients who suffer from hypoactive delirium exhibit “negative symptomatology” ranging from apathy, to withdrawal, or lethargy, and often go unnoticed by the medical team. Indeed, patients with “quiet delirium” rarely require 1:1 care and are often referred to as “good” patients.6 Parents, however, may alert the medical team that their child is “just not themselves.” This rarely results in a change in medical care or further assessment, and felt to be part of the normal recovery from anesthesia. This subtype of delirium is the most common among both adult and pediatric ICU-delirium (>50%).8–10 As we do not routinely assess for hypoactive delirium in the PACU, the impact of hypoactive delirium on outcomes following general anesthesia is not known. Similarly, patients with delirium who are hospitalized and monitored over time may oscillate between positive and negative symptoms, and classified as mixed delirium. Understanding these concepts will help guide the ongoing conversation regarding accurate diagnosis of delirium and recognition of agitation in the post-anesthesia state.
Emergence Behaviors
Many pediatric patients emerging from general anesthesia will suffer a period of dysregulated behavior. Malarbi et al completed an observational study in children aged 18 months - 6 years assumed to have Emergence Delirium by clinical observation alone, demonstrating symptoms such as eye staring or averting, involuntary movements, kicking, and inconsolability.11 Children may also exhibit psychomotor agitation and neuropsychiatric derangement during emergence including: moaning, thrashing, back arching, inconsolable crying, yelling, kicking, and pulling at lines or bandages, or emotional lability, and altered levels of consciousness.12 Patients with extremes of behavioral dysregulation may be unable to be comforted even with familiar objects such as a favorite toy or parental presence. While many of these behaviors may occur in patients with delirium, the lack of consistent use of an objective tool for screening limits the advancement of knowledge regarding the emergence period in children.13
Emergence Delirium/Agitation – Prevalence and Risk Factors
The incidence of ED/EA is highly variable in the literature, ranging from 10–80%.14–16 Patient characteristics, anesthetic technique, surgical case type, and a host of different metrics used to assess for ED/EA all contribute to this variance in reported incidence. Emergence delirium/agitation typically presents in the early phase of emergence, on average 14 minutes (± 11 minutes) following cessation of general anesthesia, however ED/EA has been reported as late as 45 minutes following conclusion of general anesthesia.17 The course of ED/EA is often a self-limited phenomenon and therefore the benefit of medical intervention remains controversial. However, associated consequences such as untimely loss of intravenous catheters or drainage tubes, patient or staff injury, parental and staff dissatisfaction, and increased utilization of PACU resources remain concerning.18,19 Long-term outcomes such as postoperative cognitive dysfunction or maladaptive behaviors in children following general anesthesia remain poorly delineated and any associations with ED have not been studied.
Risk factors for EA/ED are presented in three major categories: patient-related, anesthesia-related, and surgical factors. Patient related risk factors associated with an increased incidence of EA/ED include male gender, preschool age, higher preoperative anxiety level, and baseline sleep-disordered breathing.20 Younger patients that tend to be more emotional or impulsive, less social or adaptable at baseline appear to be at particularly high risk for the development of EA/ED.17,21,22 The intensity of preoperative anxiety is influenced by a host of factors including parental anxiety, young age, previous medical experiences, and immature social skills. Patients with preoperative anxiety are six times more likely to develop EA/ED compared to those who are less anxious (p < 0.005).23,24 Mohkamkar et al1 demonstrated that if individuals experienced agitation during induction of anesthesia that they were much more likely to have agitation upon emergence. Moreover, agitation upon emergence was significantly associated with ED in the post-anesthesia unit (OR 4, 95% CI 1.7–9.4).25
Precipitating factors such as anesthesia exposure and surgical intervention also impact the likelihood of EA/ED. Intravenous anesthesia is not commonly associated with EA/ED, touted as having a protective effect, versus the nearly four times more common occurrence following volatile agents.14,26 A step-wise titration protocol for discontinuation of sevoflurane was not associated with a decrease in the development of EA/ED.27 Rapid versus slow emergence may lead to greater risk of emergence delirium, but this relationship has yet to be clearly demonstrated.28 Emergence time was found to impact EA in a recent study of 121 pediatric patients undergoing dental rehabilitation where high-dose midazolam premedication was associated with a longer emergence time and lower rate of agitation upon emergence.25 In the transition from the general anesthesia to recovery, patients with symptoms of EA/ED more often are reported to have high pain scores, which emphasizes the challenges we currently have in differentiating between pain and EA/ED.21
Finally, surgical risk factors for EA/ED appear to be linked with the type of procedure such as ear, nose, throat (ENT) or ophthalmologic interventions, and the length of procedure, with shorter interventions associated with an increased incidence of EA/ED.1 This may be related to the abrupt cessation of volatile anesthesia and emergence from anesthesia versus the actual length of surgical intervention. Interestingly, Eckenhoff et al29 surmised that a feeling of suffocation during emergence from anesthesia following head and neck surgery was responsible for the high frequency of observed emergence agitation. The approach to anesthesia should consider type and length of surgical procedures, necessary emergence style (i.e. awake, deep), and immediate postoperative issues (i.e. pain) in order to minimize the impact of all of these factors to the development of emergence agitation or delirium.
Emergence Delirium/Agitation – Pathophysiology
There is limited understanding of the pathophysiology of EA/ED. Working hypotheses have included uncontrolled pain, pre-operative anxiety, and differential clearance of various anesthetic agents.30 Although severe, unrelenting pain may very well be a precipitating factor for the development of delirium, it is not a suggested predictive measure as delirium can clearly occur in the absence of pain.31 In fact, even patients undergoing “painless” procedures such as general anesthesia for MRI have been reported to experience EA/ED.32 The theory of differential clearance describes how various volatile anesthetic agents are cleared in distinctive ways from the central nervous system leading to varying recovery rates of cognitive functions.17,33 Hence emergence delirium may be an imbalance in the rate of recovery for a patient’s arousal state versus their content of consciousness.34 This may lead to an “awake” patient but one who is unable to perceive information from the environment and respond or interact appropriately.
Patient Assessment
Emergence Agitation Scales
Emergence agitation is most commonly referred to as a state of mild-moderate restlessness and distress that, unlike delirium, is not always associated with a significant change in behavior or cognition.35 The intensity of agitation can be readily observed and scored by using tools such as the CRAVERO and WATCHA scales.36–38 The Cravero and Watcha scales rank levels of consciousness or arousal, being versions of typical sedation scales such as the Richmond Agitation-Sedation Scale (RASS)39 used in both the postoperative and ICU environments.(Table 1) Using the RASS, caregivers observe the patient for spontaneous awakening and eye opening (RASS 0) and varied levels of agitation (RASS +1 to +4). If no spontaneous eye opening, then the caregiver stimulates the patient with voice, observing levels of depressed arousal (RASS −1 to −3). If no response to voice, then physical stimulus is provided with either response to touch (RASS −4) or no response (RASS −5), which is considered comatose. The Watcha scale is a four level arousal scale ranging from a “calm” patient (Score of 1) to “agitation with thrashing around” (Score of 4).13,40 A severely elevated level of arousal on the Watcha scale (Score of 3 or 4) may be consistent with EA. The Cravero scale categorizes five levels of arousal ranging from “obtunded with no response to stimulation” (Score of 1) to “thrashing behavior that requires restraint” (Score of 5).41 After attempts of active calming, patients who have severe levels of agitation on the Cravero scale (Score of 4 or 5) are referred to as EA.12,41 Some researchers suggest that emergence agitation is analogous to emergence delirium in patients with severe levels of agitation, as agitation is reported more commonly than depressed levels of arousal in patients thought to have emergence delirium.12,17 This argument highlights the lack of understanding of delirium versus agitation. Agitation is not a DSM-criterion for delirium, and symptoms of agitation are more commonly reported in the anesthesia literature in part due to the lack of monitoring for all delirium subtypes in the post-anesthesia care unit. Both the Watcha and Cravero scales are level of consciousness scales, assessing for levels of agitation, and may identify some patients with coinciding hyperactive delirium. However, symptoms used to describe levels of agitation measured by the Cravero and Watcha scales are also symptoms consistent with untreated pain and in valid and reliable pain assessment scales, such as the Faces, Legs, Activity, Cry and Consolability (FLACC) scale, the Children’s Hospital of Eastern Ontario Pain Scale (CHEOPS), and the Children’s and Infants’ Postoperative Pain Scale (CHIP-PS).42–44 Therefore, other considerations during the assessment of agitation, in particular, is the high likelihood that it is associated with pain, anxiety, hunger, or parental separation and should not be assumed to be a consequence of delirium or even emergence from general anesthesia.13
Table 1.
Comparison of a Common Level of Consciousness or Sedation Scale with Pediatric Scales for Emergence Agitation (EA)
| Patient Response or Symptom | Level of Consciousness Scales | ||
|---|---|---|---|
| RASSa | WATCHAb | CRAVEROc | |
| Combative: violent, immediate danger to staff | +4 | 4 | 5 |
| Aggressive: pulls to remove tubes or catheters | +3 | 3 | |
| Agitated: non-purposeful movement, may cry and inconsolable | +2 | 4 | |
| Anxious: apprehensive, consolable cry | +1 | 2 | 3 |
| Spontaneously awake and attentive | 0 | 1 | |
| Not fully alert: sustained awakening and eye contact to voice | −1 | ||
| Briefly awakens with limited eye opening/contact to voice | −2 | 2 | |
| Movement or eye opening to voice but no eye contact | −3 | ||
| No response to voice. Some response to physical stimulation | −4 | ||
| Comatose: No response to voice or physical stimulation | −5 | 1 | |
Notes: aRichmond Agitation-Sedation Scale (RASS) used for routine monitoring of level of consciousness or level of sedation. bThe WATCHA behavior scale used to determine emergence agitation (EA) based on observation (Level 3 or 4). cThe CRAVERO scale assesses for behaviors consistent with EA including Level 4 or 5.
Emergence Delirium Tools
The ability to accurately differentiate hyperactive delirium from other sources of agitation requires the assessment of more complex neurobehavioral symptoms.4 Alarmingly in critically ill patients, delirium goes undetected in up to three out of four patients when clinicians do not use a structured delirium screening tool.45,46 The Pediatric Anesthesia Emergence Delirium (PAED) scale (Table 2) assesses for DSM criteria for delirium including inattention (eye contact with the caregiver), disorganized thinking or dysregulated systems (unawareness of surroundings), changes in cognition (decrease in purposeful actions), and a disturbance in psychomotor behavior or acute alteration of consciousness (restlessness or inconsolability).27 Each of these five subdomains is scored using a Likert scale (not at all, just a little, quite a bit, very much, extremely), which may be cumbersome in a busy clinical setting, though worthwhile for delirium screening.12 A score of 9 or higher is consistent with hyperactive delirium, also known as emergence delirium. Though the PAED incorporates DSM criteria, it does not require the cardinal feature of inattention for delirium diagnosis.15 This deviates from the requirements of more robust and interactive delirium tools used in the ICU-setting that require inattention and altered/fluctuating mental status for delirium presence.9,47,48 Furthermore, it does not sufficiently screen for all delirium subtypes, including hypoactive delirium, the most common subtype reported in both adults and children in the ICU.
Table 2.
The Pediatric Anesthesia Emergence Delirium (PAED)15 Scalea
| Delirium Symptom | Not at All | Just a Little | Quite a Bit | Very Much | Extremely |
|---|---|---|---|---|---|
| Child makes eye contact with the caregiver | 4 | 3 | 2 | 1 | 0 |
| Child’s actions are purposeful | 4 | 3 | 2 | 1 | 0 |
| Child is aware of his/her surroundings | 4 | 3 | 2 | 1 | 0 |
| Child is restless | 0 | 1 | 2 | 3 | 4 |
| Child is inconsolable | 0 | 1 | 2 | 3 | 4 |
Notes: aPatients are observed for each of the 5 symptoms of delirium. Once an observation is complete, the clinician scores the severity of that delirium symptom subjectively using the Lickert scale (“not at all,” “just a little,” “quite a bit,” “very much,” and “extremely”). A total score of 10 or greater may be consistent with Emergence Delirium.
ICU Delirium Assessment
Advances in delirium epidemiology has been fueled by the creation and implementation of highly valid and reliable delirium bedside tools in the pediatric ICU setting in all patients from infancy to adolescence and either on or off mechanical ventilation.9,47–50 Further study of emergence in the post-anesthesia period, especially in the pediatric population, may benefit from tools that are efficient, easy to use, and help delineate behavioral symptoms from hyperactive and hypoactive delirium. The Preschool Confusion Assessment Method for the ICU (psCAM-ICU) (specificity of 91% and sensitivity of 75%) and the Pediatric CAM-ICU (pCAM-ICU) (specificity of 99% and a sensitivity of 83%) are highly valid and reliable bedside tools for delirium screening (Table 3).9,48,51 The pediatric CAM-ICU series follow a standardized approach to delirium assessment using DSM criteria, and Plum and Posner's’ definition of consciousness to assess for the key features of both arousal and content of consciousness. Patients are first assessed using a sedation scale (RASS) for their level of consciousness, as patients need to be at least reactive to voice (RASS −3 or above) in order to be clinically assessed for delirium (i.e. not comatose). The ps/pCAM-ICU then both assess for key DSM features of delirium: 1) fluctuation or an acute change in mental status, 2) inattention, 3) an acute alteration level of consciousness, and 4) disorganized systems/thinking. Delirium is present when a patient demonstrates Features 1 and 2, plus either Feature 3 or 4. This hierarchal approach allows for quick and efficient assessment (i.e. if Feature 1 or 2 are not present, then delirium is not present). The psCAM-ICU was adapted from the pCAM-ICU to assure that assessments for inattention and disorganized systems/thinking were developmentally appropriate for critically ill patients less than 5 years of age given the significant variation of language and cognitive maturity in the younger pediatric population.
Table 3.
| Preschool CAM-ICU (psCAM-ICU)a Less Than 5 Years of Age | Pediatric CAM-ICU (pCAM-ICU)a ≥ 5 Years of Age | Feature Present?c | |
|---|---|---|---|
|
Feature 1: Mental Statusb |
Acute change in mental status? OR Fluctuation in mental status? |
Acute change in mental status? OR Fluctuation in mental status? |
NO → STOP - Delirium Absent YES → Assess Feature 2 |
|
Feature 2: Inattentionb |
Show 10 pictures/mirror and count number patient has eye contact. Inattention present ≥ 3 no eye contact |
Vigilance A: ABADBADAAY “Squeeze my hand every time you hear the letter ‘A’.” Inattention present ≥ 3 errors |
NO → STOP - Delirium Absent YES → Assess Feature 3 |
|
Feature 3: Altered level of consciousness |
Does the patient currently have an altered level of consciousness? | Does the patient currently have an altered level of consciousness? |
YES → STOP - Delirium Present NO → Assess Feature 4 |
|
Feature 4: Disorganized Brain |
1) Sleep-wake cycle disturbance? OR 2) Patient unaware of surroundings and inconsolable? |
Ask 4 yes/no questions and give 1 two-step command Feature 4 present ≥ 2 errors |
YES → STOP - Delirium Present NO → STOP - Delirium Absent |
Notes: aThe Preschool Confusion Assessment Method for the ICU (psCAM-ICU) and the Pediatric CAM-ICU (pCAM-ICU) are highly valid and reliable pediatric delirium screening tools used in preschool (neonate – 5 years) and school-aged (≥ 5 years) critically ill patients who are at least responsive to voice. bThe cardinal features (acute change or fluctuating mental status and inattention) are required for delirium diagnosis using the hierarchal structure of these tools. cFollowing the ps/pCAM-ICU algorithm, once three features have been identified as “YES” or “PRESENT” then delirium is present and the assessment is complete.
Management of Emergence Agitation and Delirium
Appropriate patient management depends on adequate postoperative assessment, including monitoring of level of consciousness, pain, and delirium using valid bedside tools.
Preoperative Strategies
Non-pharmacologic strategies used in the preoperative setting to reduce both patient and parental preoperative anxiety have shown effectiveness in reducing the incidence of EA/ED.52,53 The impact of preoperative interventions on the development of EA/ED remains unresolved, however a recent RCT comparing oral benzodiazepine versus tablet-based interactive distraction (TBID) demonstrated improved baseline anxiety, tolerance of mask induction, earlier discharge, and lower rates of ED at 15 minutes post-emergence in the TBID group.54 Preoperative administration of intranasal dexmedetomidine (1–2 mcg/kg) at least 20 minutes prior to induction was associated with less preoperative anxiety and postoperative agitation, via PAED assessment, without prolonging postoperative recovery compared with placebo during a propofol TIVA.55 Preoperative oral dexmedetomidine, compared to oral benzodiazepine, was associated with significantly lower PAED scores (p<0.05) and ED rates [0% in Dex group, 19% in Midaz group (p=0.01)].56 Other agents with efficacy in the prevention of emergence delirium include preoperative administration of gabapentin,57 intraoperative magnesium infusion,58 intraoperative dexamethasone,59 and midazolam.60,61 Oral gabapentin (5 mg/kg) was shown to significantly reduce the incidence of EA by 20% in a cohort of 70 children aged 2–6 years of age undergoing strabismus surgery receiving desflurane maintenance.62
Intraoperative Strategies
The class of alpha-2 agonists, including clonidine14,60,63 and dexmedetomidine, have shown success in the prevention of emergence delirium when administered either systemically or via a regional technique. Use of dexmedetomidine in the prevention of emergence delirium has gained particular interest given that the medication also serves as an adjunct in the treatment of analgesia and prevention of postoperative nausea and vomiting.64,65 In multiple smaller cohort randomized controlled trials, administration of dexmedetomidine as an intravenous bolus (0.13–0.5 mcg/kg over 5–10 minutes) before the end of the procedure and/or low-dose continuous intraoperative infusion (0.4 mcg/kg/h) during sevoflurane general anesthesia is associated with significant reductions in rates of ED.66–70 Concerns have been raised that dexmedetomidine may be associated with increased postoperative care unit length of stay,71 however this has not been consistent across prospective pediatric studies.66 Despite this potential disadvantage, intraoperative dexmedetomidine administration has been associated with fewer adverse events in the PACU and less need for rescue opioid for pain.66,71
Total intravenous anesthesia (TIVA) with Propofol has been shown to be effective for both the prevention and treatment of EA/ED symptoms.72 An induction dose alone or a bolus following mask induction with volatile agents are not associated with a decrease in ED.14 Propofol administration just prior to emergence demonstrated mixed results at lower doses (1 mg/kg IV),14,73 compared to significant reductions in ED prevalence with higher doses (3mg/kg IV).73,74
The additive benefit of multiple intravenous agents on prevalence or duration of EA/ED has not been demonstrated. Cao et al reported that in a RCT of propofol anesthesia during tonsillectomy with added use of dexmedetomidine (1 mcg/kg bolus and 0.5 mcg/kg/h continuous infusion) had no affect on ED rates using the PAED compared to Propofol TIVA alone.71 Whereas, Tsiotou et al duplicated this anesthetic protocol in a similar sixty-patient cohort undergoing tonsillectomy and demonstrated a significant reduction in “ED” assessed using the WATCHA with both propofol and dexmedetomidine.75 This demonstrates the need to consistently use language describing outcomes and understand the difference between EA and ED and the assessment tools that are specific for both. Likely both studies may be correct in that use of dexmedetomidine in the setting of a propofol TIVA further decreases EA (WATCHA) upon emergence but does not further decrease the rates of ED (PAED) in the post-anesthesia care unit.
Acute Treatment
The evidence to support acute treatment of EA/ED remains ambiguous. Cleary patients with severe agitation may be at risk for self-harm or hurting others, and therefore the decision to treat becomes more straightforward for clinicians. The caregiver must quickly weigh the patient history, procedure, and recent course in the postoperative recovery unit to determine the most appropriate treatment. Contributing factors may include acute pain, absence of family, or restrictive elements such as peripheral IV, cast, dressing, or sensory changes following surgery (i.e. ophthalmologic). If a contributing factor can be quickly identified, then the clinician may be able to address that specific issue to improve agitation or delirium. However, the situation may require immediate response, and in these situations, reasonable methods for decreasing the severity and duration of the hyperactive symptoms include bolus administration of propofol (0.5–1 mg/kg IV),14,76,77 fentanyl (1–2.5 mcg/kg IV),41,78 dexmedetomidine (0.5 mcg/kg IV),14,79,80 or haloperidol (0.025–0.05 mg/kg IV).81 Of note, antipsychotics do not have an FDA indication for use in children with delirium, and attention to possible side effects such as prolonged QTc are necessary if use is deemed appropriate. With any acute intervention, the care team will have to monitor adequacy of ventilation and oxygenation and should be able to rescue acutely if needed. Remember that these interventions treat manifestations of hyperactive delirium, though do not “treat” the delirium. Delirium will resolve with correction of the causative insults such as residual volatile anesthesia effects, hypoxia, acidemia, or hypotension (BRAIN MAPS).
Long-Term Consequences
Emergence delirium has been associated with an increased risk of transient postoperative maladaptive behaviors.82 Maladaptive behaviors exhibited by children can range from increased general anxiety to sleep disturbances, nighttime crying, separation anxiety, temper tantrums, and enuresis. However, the relationship between the presence of emergence delirium and postoperative maladaptive behaviors is complex and influenced by confounding factors such as preoperative anxiety level in both the patient and the parent.21,23,83 Further research is needed to answer the very important questions of whether the occurrence and management of EA/ED is truly important for the well being of our patients following discharge to home.
Summary
Hyperactive behaviors during emergence have been described by different terms such as emergence excitation, agitation, and delirium. Literature provides evidence of a period of behavioral dysregulation, usually hyperactive in nature, and in its severest forms can place the patient and caregiver at risk for harm. However, it is important to recognize that there is a significant void in the understanding of the full spectrum of post-anesthesia delirium and agitation. The ability to accurately describe behavioral dysregulation during emergence hinges on our ability to have access to tools for the assessment of levels of consciousness and agitation, pain, and delirium. Future studies are needed to further define the full spectrum of cognitive and behavioral dysregulation as well as to better understand the potential mitigation strategies and long-term consequences associated with emergence agitation and delirium.
Case-Based Learning Discussion
You are called to the bedside of a thrashing, inconsolable 5-year-old male s/p incision and drainage of a neck abscess. Two PACU nurses are attempting to hold the patient and prevent him from pulling out his IV and his drain at his surgical site. What is your differential diagnosis? What are your initial concerns for this patient? How would you further assess the patient? What is your final management strategy?
A colleague comes to you and asks how you determine whether a patient has emergence agitation or delirium. How would you define EA/ED? What would you tell your colleague in regard to appropriate patient assessment for hyperactive behaviors? What challenges exist in measuring the incidence of emergence delirium?
Describe the risk factors for the development of EA/ED. What risk factors are modifiable to decrease the development of EA/ED?
In your discussion of risks and benefits of anesthesia with the patient’s family you mention emergence delirium. The patient’s mother wants to know how emergence delirium will affect her child. What would you tell her about the potential consequences associated with emergence delirium both acute and long term?
You are asked to give a lecture to staff in the post-anesthesia recovery unit (PACU) at your institution regarding the differences between emergence agitation and delirium. What are the key features you would focus on in your education? How would you promote differentiating these terms?
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Eckenhoff JE, Kneale DH, Dripps RD. The incidence and etiology of postanesthetic excitment. A clinical survey. Anesthesiology 1961;22: 667–73. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Publishing, Incorporated; 2013. doi: 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- 3.Tobias JD. Dexmedetomidine: applications in pediatric critical care and pediatric anesthesiology. Pediatr Crit Care Med. 2007;8(2):115–131. doi: 10.1097/01.PCC.0000257100.31779.41 [DOI] [PubMed] [Google Scholar]
- 4.Przybylo HJ, Martini DR, Mazurek AJ, Bracey E, Johnsen L, Cote CJ. Assessing behaviour in children emerging from anaesthesia: can we apply psychiatric diagnostic techniques? Paediatr Anaesth. 2003;13(7):609–616. doi: 10.1046/j.1460-9592.2003.01099.x [DOI] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). 4 ed. Vol. 1 Arlington, VA: American Psychiatric Association;2000. doi: 10.1176/appi.books.9780890423349 [DOI] [Google Scholar]
- 6.Smith HAB, Brink E, Fuchs C, Ely EW, Pandharipande PP. Pediatric delirium: monitoring and management in the pediatric intensive care unit. Pediatr Clin North Am. 2013;60(3):741–760. doi: 10.1016/j.pcl.2013.02.010 [DOI] [PubMed] [Google Scholar]
- 7.Stamper MJ, Hawks SJ, Taicher BM, Bonta J, Brandon DH. Identifying pediatric emergence delirium by using the PAED scale: a quality improvement project. AORN J. 2014;99(4):480–494. doi: 10.1016/j.aorn.2013.08.019 [DOI] [PubMed] [Google Scholar]
- 8.Meagher DJ, Leonard M, Donnelly S, Conroy M, Adamis D, Trzepacz PT. A longitudinal study of motor subtypes in delirium: relationship with other phenomenology, etiology, medication exposure and prognosis. J Psychosom Res. 2011;71(6):395–403. doi: 10.1016/j.jpsychores.2011.06.001 [DOI] [PubMed] [Google Scholar]
- 9.Smith H, Gangopadhyay M, Goben CM, et al. The preschool confusion assessment method for the ICU: valid and reliable delirium monitoring for critically ill infants and children. Crit Care Med. 2016;44(3):592–600. doi: 10.1097/CCM.0000000000001428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pandharipande P, Cotton BA, Shintani A, et al. Motoric subtypes of delirium in mechanically ventilated surgical and trauma intensive care unit patients. Intensive Care Med. 2007;33(10):1726–1731. doi: 10.1007/s00134-007-0687-y [DOI] [PubMed] [Google Scholar]
- 11.Malarbi S, Stargatt R, Howard K, Davidson A. Characterizing the behavior of children emerging with delirium from general anesthesia. Paediatr Anaesth. 2011;21(9):942–950. doi: 10.1111/j.1460-9592.2011.03646.x [DOI] [PubMed] [Google Scholar]
- 12.Reduque LL, Verghese ST. Paediatric emergence delirium. Continuing Education in Anaesthesia, Crit Care Pain. 2013;13(2):39–41. doi: 10.1093/bjaceaccp/mks051 [DOI] [Google Scholar]
- 13.Bajwa SA, Costi D, Cyna AM. A comparison of emergence delirium scales following general anesthesia in children. Paediatr Anaesth. 2010;20(8):704–711. doi: 10.1111/j.1460-9592.2010.03328.x [DOI] [PubMed] [Google Scholar]
- 14.Dahmani S, Stany I, Brasher C, et al. Pharmacological prevention of sevoflurane- and desflurane-related emergence agitation in children: a meta-analysis of published studies. Br J Anaesth. 2010;104(2):216–223. doi: 10.1093/bja/aep376 [DOI] [PubMed] [Google Scholar]
- 15.Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004;100(5):1138–1145. doi: 10.1097/00000542-200405000-00015 [DOI] [PubMed] [Google Scholar]
- 16.Doerrfuss JI, Kramer S, Tafelski S, Spies CD, Wernecke K-D, Nachtigall I. Frequency, predictive factors and therapy of emergence delirium: data from a large observational clinical trial in a broad spectrum of postoperative pediatric patients. Minerva Anestesiol. 2019;85(6):617–624. doi: 10.23736/S0375-9393.19.13038-6 [DOI] [PubMed] [Google Scholar]
- 17.Voepel-Lewis T, Malviya S, Tait AR. A prospective cohort study of emergence agitation in the pediatric postanesthesia care unit. Anesth Analg. 2003;96(6):. doi: 10.1213/01.ANE.0000062522.21048.61 [DOI] [PubMed] [Google Scholar]
- 18.Banchs RJ, Lerman J. Preoperative anxiety management, emergence delirium, and postoperative behavior. Anesthesiol Clin. 2014;32(1):1–23. doi: 10.1016/j.anclin.2013.10.011 [DOI] [PubMed] [Google Scholar]
- 19.Mukherjee A, Das A, Basunia SR, Chattopadhyay S, Kundu R, Bhattacharyya R. Emergence agitation prevention in paediatric ambulatory surgery: a comparison between intranasal dexmedetomidine and clonidine. J Res Pharm Pract. 2015;4(1):24–30. doi: 10.4103/2279-042X.150051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reynolds T, Sankaran S, Chimbira WT, Phan T, Nafiu OO. Severe obesity and sleep-disordered breathing as risk factors for emergence agitation in pediatric ambulatory surgery. J PeriAnesth Nurs. 2018;33(3):304–311. doi: 10.1016/j.jopan.2016.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kain ZN, Caldwell-Andrews AA, Maranets I, et al. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth Analg. 2004;99(6):. doi: 10.1213/01.ANE.0000136471.36680.97 [DOI] [PubMed] [Google Scholar]
- 22.Kain ZN, Mayes LC, Caldwell-Andrews AA, Karas DE, McClain BC. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics. 2006;118(2):651–658. doi: 10.1542/peds.2005-2920 [DOI] [PubMed] [Google Scholar]
- 23.Kain ZN, Mayes LC, O’Connor TZ, Cicchetti DV. Preoperative anxiety in children. Predictors and outcomes. Arch Pediatr Adolesc Med. 1996;150(12):1238–1245. doi: 10.1001/archpedi.1996.02170370016002 [DOI] [PubMed] [Google Scholar]
- 24.Gooden R, Tennant I, James B, et al. The incidence of emergence delirium and risk factors following sevoflurane use in pediatric patients for day case surgery, Kingston, Jamaica. Braz J Anesthesiol. 2014;64(6):413–418. doi: 10.1016/j.bjane.2013.09.012 [DOI] [PubMed] [Google Scholar]
- 25.Kawai M, Kurata S, Sanuki T, et al. The effect of midazolam administration for the prevention of emergence agitation in pediatric patients with extreme fear and non-cooperation undergoing dental treatment under sevoflurane anesthesia, a double-blind, randomized study. DDDT. 2019;13:1729–1737. doi: 10.2147/DDDT.S198123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu D, Chai W, Sun X, Yao L. Emergence agitation in adults: risk factors in 2000 patients. Can J Anaesth. 2010;57(9):843–848. doi: 10.1007/s12630-010-9338-9 [DOI] [PubMed] [Google Scholar]
- 27.Vlajkovic GP, Sindjelic RP. Emergence delirium in children: many questions, few answers. Anesth Analg. 2007;104(1):84–91. doi: 10.1213/01.ane.0000250914.91881.a8 [DOI] [PubMed] [Google Scholar]
- 28.Oh A-Y, Seo K-S, Kim S-D, Kim C-S, Kim H-S. Delayed emergence process does not result in a lower incidence of emergence agitation after sevoflurane anesthesia in children. Acta Anaesthesiol Scand. 2005;49(3):297–299. doi: 10.1111/j.1399-6576.2005.00687.x [DOI] [PubMed] [Google Scholar]
- 29.Eckenhoff JE, Kneale DH, Dripps RD. The incidence and etiology of postanesthetic excitement a clinical survey. Anesthesiology. 1961;22(5):667–673. doi: 10.1097/00000542-196109000-00002 [DOI] [PubMed] [Google Scholar]
- 30.Dahmani S, Delivet H, Hilly J. Emergence delirium in children: an update. Curr Opin Anaesthesiol. 2014;27(3):309–315. doi: 10.1097/ACO.0000000000000076 [DOI] [PubMed] [Google Scholar]
- 31.Currie P. Understanding and Treating Emergence Delirium (2015). Nurse Anesthesia Capstones. Available from: http://dune.une.edu/na_capstones/4. Accessed July 13, 2020. [Google Scholar]
- 32.Bonhomme V, Boveroux P, Brichant JF, Laureys S, Boly M. Neural correlates of consciousness during general anesthesia using functional magnetic resonance imaging (fMRI).. Arch Ital Biol. 2012;150(2–3):155–163. doi: 10.4449/aib.v150i2.1242 [DOI] [PubMed] [Google Scholar]
- 33.Taenzer AH, Havidich JE. The Postanesthesia Care Unit and Beyond. In: Cote CJ, Lerman J, Anderson BJ, eds. A Practice of Anesthesia for Infants and Children, Elsevier. 2013:980–992. [Google Scholar]
- 34.JBPM D, CBSM D, NSM D, FPM D. Plum and Posner’s Diagnosis of Stupor and Coma. Oxford University Press; 2007; doi: 10.1093/med/9780195321319.001.0001 [DOI] [Google Scholar]
- 35.Galford RE. Problems in Anesthesiology. Little Brown & Company; 1992. [Google Scholar]
- 36.Aono J, Ueda W, Mamiya K, Takimoto E, Manabe M. Greater incidence of delirium during recovery from sevoflurane anesthesia in preschool boys. Anesthesiology. 1997;87(6):1298–1300. doi: 10.1097/00000542-199712000-00006 [DOI] [PubMed] [Google Scholar]
- 37.Cravero J, Surgenor S, Whalen K. Emergence agitation in paediatric patients after sevoflurane anaesthesia and no surgery: a comparison with halothane. Paediatr Anaesth. 2000;10(4):419–424. doi: 10.1046/j.1460-9592.2000.00560.x [DOI] [PubMed] [Google Scholar]
- 38.Weldon BC, Bell M, Craddock T. The effect of caudal analgesia on emergence agitation in children after sevoflurane versus halothane anesthesia. Anesth Analg. 2004;321–326. doi: 10.1213/01.ANE.0000096004.96603.08 [DOI] [PubMed] [Google Scholar]
- 39.Sessler CN, Gosnell MS, Grap MJ, et al. The richmond agitation-sedation scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–1344. doi: 10.1164/rccm.2107138 [DOI] [PubMed] [Google Scholar]
- 40.Watcha MF, Ramirez-Ruiz M, White PF, Jones MB, Lagueruela RG, Terkonda RP. Perioperative effects of oral ketorolac and acetaminophen in children undergoing bilateral myringotomy. Can J Anaesth. 1992;39(7):649–654. doi: 10.1007/BF03008224 [DOI] [PubMed] [Google Scholar]
- 41.Cravero JP, Beach M, Thyr B, Whalen K. The effect of small dose fentanyl on the emergence characteristics of pediatric patients after sevoflurane anesthesia without surgery. Anesth Analg. 2003;97(2):. doi: 10.1213/01.ANE.0000070227.78670.43 [DOI] [PubMed] [Google Scholar]
- 42.Willis M, Merkel SI, Voepel-Lewis T, Malviya S. FLACC behavioral pain assessment scale: a comparison with the child’s self-report. Pediatr Nurs. 2003;29(3):195. [PubMed] [Google Scholar]
- 43.McGrath PJ, Johnson G, Goodman JT, Schillinger J. CHEOPS: a behavioral scale for rating postoperative pain in children. Adv Pain Res Ther. 1985. [Google Scholar]
- 44.Büttner W, Finke W. Analysis of behavioural and physiological parameters for the assessment of postoperative analgesic demand in newborns, infants and young children: a comprehensive report on seven consecutive studies. Paediatr Anaesth. 2000;10(3):303–318. doi: 10.1046/j.1460-9592.2000.00530.x [DOI] [PubMed] [Google Scholar]
- 45.van Eijk MMJ, van Marum RJ, Klijn IAM, de Wit N, Kesecioglu J, Slooter AJC. Comparison of delirium assessment tools in a mixed intensive care unit*. Crit Care Med. 2009;37(6):1881–1885. doi: 10.1097/CCM.0b013e3181a00118 [DOI] [PubMed] [Google Scholar]
- 46.Spronk PE, Riekerk B, Hofhuis J, Rommes JH. Occurrence of delirium is severely underestimated in the ICU during daily care. Intensive Care Med. 2009;35(7):1276–1280. doi: 10.1007/s00134-009-1466-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). JAMA. 2001;286(21):2703–2710. doi: 10.1001/jama.286.21.2703 [DOI] [PubMed] [Google Scholar]
- 48.Smith HAB, Boyd J, Fuchs DC, et al. Diagnosing delirium in critically ill children: validity and reliability of the pediatric confusion assessment method for the intensive care unit*. Crit Care Med. 2011;39(1):150–157. doi: 10.1097/CCM.0b013e3181feb489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ely EW, Margolin R, Francis J, May L. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care. 2001. doi: 10.1097/00003246-200107000-00012 [DOI] [PubMed] [Google Scholar]
- 50.Schieveld JNM, Leroy PLJM, van Os J, Nicolai J, Vos GD, Leentjens AFG. Pediatric delirium in critical illness: phenomenology, clinical correlates and treatment response in 40 cases in the pediatric intensive care unit. Intensive Care Med. 2007;33(6):1033–1040. doi: 10.1007/s00134-007-0637-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.ICU delirium and cognitive impairment study group. Available from: http://www.icudelirium.org/. Accessed June6, 2020.
- 52.Yip P, Middleton P, Cyna AM, Carlyle AV. Non-pharmacological interventions for assisting the induction of anaesthesia in children. Cyna AM, ed. Cochrane Database Syst Rev. 2009;3:CD006447. doi: 10.1002/14651858.CD006447.pub2 [DOI] [PubMed] [Google Scholar]
- 53.Kain ZN, Caldwell-Andrews AA, Mayes LC, et al. Family-centered preparation for surgery improves perioperative outcomes in children: a randomized controlled trial. Anesthesiology. 2007;106(1):65–74. doi: 10.1097/00000542-200701000-00013 [DOI] [PubMed] [Google Scholar]
- 54.Stewart B, Cazzell MA, Pearcy T. Single-blinded randomized controlled study on use of interactive distraction versus oral midazolam to reduce pediatric preoperative anxiety, emergence delirium, and postanesthesia length of stay. J PeriAnesth Nurs. 2019;34(3):567–575. doi: 10.1016/j.jopan.2018.08.004 [DOI] [PubMed] [Google Scholar]
- 55.Li L-Q, Wang C, Xu H-Y, Lu H-L, Zhang H-Z. Effects of different doses of intranasal dexmedetomidine on preoperative sedation and postoperative agitation in pediatric with total intravenous anesthesia undergoing adenoidectomy with or without tonsillectomy. Medicine. 2018;97(39):e12140–e12147. doi: 10.1097/MD.0000000000012140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Keles S, Kocaturk O. Comparison of oral dexmedetomidine and midazolam for premedication and emergence delirium in children after dental procedures under general anesthesia: a retrospective study. DDDT. 2018;12:647–653. doi: 10.2147/DDDT.S163828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Salman AE, Camkıran A, Oğuz S, Dönmez A. Gabapentin premedication for postoperative analgesia and emergence agitation after sevoflurane anesthesia in pediatric patients. Agri. 2013;25(4):163–168. doi: 10.5505/agri.2013.98852 [DOI] [PubMed] [Google Scholar]
- 58.Abdulatif M, Ahmed A, Mukhtar A, Badawy S. The effect of magnesium sulphate infusion on the incidence and severity of emergence agitation in children undergoing adenotonsillectomy using sevoflurane anaesthesia. Anaesthesia. 2013;68(10):1045–1052. doi: 10.1111/anae.12380 [DOI] [PubMed] [Google Scholar]
- 59.Khalili G, Sajedi P, Shafa A, Hosseini B, Seyyedyousefi H. A randomized evaluation of intravenous dexamethasone versus oral acetaminophen codeine in pediatric adenotonsillectomy: emergence agitation and analgesia. Middle East J Anaesthesiol. 2012;21(4):499–504. [PubMed] [Google Scholar]
- 60.Zhang C, Li J, Zhao D, Wang Y. Prophylactic midazolam and clonidine for emergence from agitation in children after emergence from sevoflurane anesthesia: a meta-analysis. Clin Ther. 2013;35(10):1622–1631. doi: 10.1016/j.clinthera.2013.08.016 [DOI] [PubMed] [Google Scholar]
- 61.Köner O, Türe H, Mercan A, Menda F, Sözübir S. Effects of hydroxyzine-midazolam premedication on sevoflurane-induced paediatric emergence agitation: a prospective randomised clinical trial. Eur J Anaesthesiol. 2011;28(9):640–645. doi: 10.1097/EJA.0b013e328344db1a [DOI] [PubMed] [Google Scholar]
- 62.Badawy AA, Kasem SA, Rashwan D, et al. The role of Gabapentin oral solution in decreasing desflurane associated emergence agitation and delirium in children after stabismus surgery, a prospective randomized double-blind study. BMC Anesthesiol. 2018;18(1):1648. doi: 10.1186/s12871-018-0533-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dahmani S, Brasher C, Stany I, et al. Premedication with clonidine is superior to benzodiazepines. A meta analysis of published studies. Acta Anaesthesiol Scand. 2010;54(4):397–402. doi: 10.1111/j.1399-6576.2009.02207.x [DOI] [PubMed] [Google Scholar]
- 64.Ali MA, Abdellatif AA. Prevention of sevoflurane related emergence agitation in children undergoing adenotonsillectomy: a comparison of dexmedetomidine and propofol. Saudi J Anaesth. 2013;7(3):296–300. doi: 10.4103/1658-354X.115363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chen J-Y, Jia J-E, Liu T-J, Qin M-J, Li W-X. Comparison of the effects of dexmedetomidine, ketamine, and placebo on emergence agitation after strabismus surgery in children. Can J Anaesth. 2013;60(4):385–392. doi: 10.1007/s12630-013-9886-x [DOI] [PubMed] [Google Scholar]
- 66.Hauber JA, Davis PJ, Bendel LP, et al. Dexmedetomidine as a rapid bolus for treatment and prophylactic prevention of emergence agitation in anesthetized children. Anesth Analg. 2015;121(5):1308–1315. doi: 10.1213/ANE.0000000000000931 [DOI] [PubMed] [Google Scholar]
- 67.Zhang Y-Z, Wang X, Wu J-M, Song C-Y, Cui X-G. Optimal dexmedetomidine dose to prevent emergence agitation under sevoflurane and remifentanil anesthesia during pediatric tonsillectomy and adenoidectomy. Front Pharmacol. 2019;10:1298. doi: 10.3389/fphar.2019.01091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Begum U, Singh P, Naithani B, Singh V, Singh GP, Tiwari T. Dexmedetomidine as bolus or low-dose infusion for the prevention of emergence agitation with sevoflurane anesthesia in pediatric patients. Anesth Essays Res. 2019;13(1):57. doi: 10.4103/aer.AER_177_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chai -D-D, Ji J. Effect of dexmedetomidine combined with sevoflurane for general anesthesia during dental treatment in pediatric patients. Shanghai Kou Qiang Yi Xue. 2018;27(1):85–88. [PubMed] [Google Scholar]
- 70.Shi M, Miao S, Gu T, Wang D, Zhang H, Liu J. Dexmedetomidine for the prevention of emergence delirium and postoperative behavioral changes in pediatric patients with sevoflurane anesthesia: a double-blind, randomized trial. DDDT. 2019;13:897–905. doi: 10.2147/DDDT.S196075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cao J-L, Pei Y-P, Wei J-Q, Zhang -Y-Y. Effects of intraoperative dexmedetomidine with intravenous anesthesia on postoperative emergence agitation/delirium in pediatric patients undergoing tonsillectomy with or without adenoidectomy. Medicine. 2016;95(49):e5566–e5566. doi: 10.1097/MD.0000000000005566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kanaya A, Kuratani N, Satoh D, Kurosawa S. Lower incidence of emergence agitation in children after propofol anesthesia compared with sevoflurane: a meta-analysis of randomized controlled trials. J Anesth. 2014;28(1):4–11. doi: 10.1007/s00540-013-1656-y [DOI] [PubMed] [Google Scholar]
- 73.Costi D, Ellwood J, Wallace A, Ahmed S, Waring L, Cyna A. Transition to propofol after sevoflurane anesthesia to prevent emergence agitation: a randomized controlled trial. anderson B, ed. Paediatr Anaesth. 2015;25(5):517–523. doi: 10.1111/pan.12617 [DOI] [PubMed] [Google Scholar]
- 74.Abbas MS, El-Hakeem EEA, Kamel HE. Three minutes propofol after sevoflurane anesthesia to prevent emergence agitation following inguinal hernia repair in children: a randomized controlled trial. Korean J Anesthesiol. 2019;72(3):253–259. doi: 10.4097/kja.d.18.00345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tsiotou AG, Malisiova A, Kouptsova E, Mavri M, Anagnostopoulou M, Kalliardou E. Dexmedetomidine for the reduction of emergence delirium in children undergoing tonsillectomy with propofol anesthesia: A double-blind, randomized study. Paediatr Anaesth. 2018;28(7):632–638. doi: 10.1111/pan.13397 [DOI] [PubMed] [Google Scholar]
- 76.Chen J, LI W, Hu X, Wang D. Emergence agitation after cataract surgery in children: a comparison of midazolam, propofol and ketamine. Paediatr Anaesth. 2010;20(9):873–879. doi: 10.1111/j.1460-9592.2010.03375.x [DOI] [PubMed] [Google Scholar]
- 77.Kim M-S, Moon B-E, Kim H, Lee J-R. Comparison of propofol and fentanyl administered at the end of anaesthesia for prevention of emergence agitation after sevoflurane anaesthesia in children. Br J Anaesth. 2013;110(2):274–280. doi: 10.1093/bja/aes382 [DOI] [PubMed] [Google Scholar]
- 78.Cohen IT, Finkel JC, Hannallah RS, Hummer KA, Patel KM. The effect of fentanyl on the emergence characteristics after desflurane or sevoflurane anesthesia in children. Anesth Analg. 2002;94(5):. doi: 10.1097/00000539-200205000-00023 [DOI] [PubMed] [Google Scholar]
- 79.Shukry M, Clyde MC, Kalarickal PL, Ramadhyani U. Does dexmedetomidine prevent emergence delirium in children after sevoflurane-based general anesthesia? Paediatr Anaesth. 2005;15(12):1098–1104. doi: 10.1111/j.1460-9592.2005.01660.x [DOI] [PubMed] [Google Scholar]
- 80.Ibacache ME, Muñoz HR, Brandes V, Morales AL. Single-dose dexmedetomidine reduces agitation after sevoflurane anesthesia in children. Anesth Analg. 2004;98(1):. doi: 10.1213/01.ANE.0000094947.20838.8E [DOI] [PubMed] [Google Scholar]
- 81.Kishk OA, Simone S, Lardieri AB, Graciano AL, Tumulty J, Edwards S. Antipsychotic treatment of delirium in critically ill children: a retrospective matched cohort study. J Pediatr Pharmacol Ther. 2019;24(3):204–213. doi: 10.5863/1551-6776-24.3.204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fortier MA, Del Rosario AM, Rosenbaum A, Kain ZN. Beyond pain: predictors of postoperative maladaptive behavior change in children. Paediatr Anaesth. 2010;20(5):445–453. doi: 10.1111/j.1460-9592.2010.03281.x [DOI] [PubMed] [Google Scholar]
- 83.Kain ZN, Wang SM, Mayes LC, Caramico LA, Hofstadter MB. Distress during the induction of anesthesia and postoperative behavioral outcomes. Anesth Analg. 1999;88(5):1042–1047. doi: 10.1213/00000539-199905000-00013 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- ICU delirium and cognitive impairment study group. Available from: http://www.icudelirium.org/. Accessed June6, 2020.