Abstract
Background
Plastic surgery training in the UK continues to evolve towards an outcome-based rather than time-served curriculum. UK plastic surgery trainees are appointed nationally, and are assessed according to national standards, but training is delivered regionally. This study sought opinion from current UK plastic surgery trainees in order to highlight strengths and shortcomings of the higher surgical training programme.
Method
A cross-sectional study was designed and administered by the UK Plastic Surgery Trainees Association (PLASTA). A questionnaire was distributed to all UK plastic surgery trainees holding a National Training Number, using the REDCap web-based application.
Results
Of the 320 UK plastic surgery trainees, 131 (41%) participated in this survey, with responses from all 12 UK training regions. The most common subspecialty career aspirations for trainees were hand surgery, cleft lip and palate, lower limb and oncoplastic breast reconstruction. The survey highlighted regional variation in teaching programmes, the ability to achieve indicative operative logbook numbers, and training in aesthetic surgery. Of the trainees, 82% expressed a desire to undertake a fellowship within their training, but most did not know whether their deanery would support this. Fifteen per cent of the respondents were currently training flexibly and the majority of these had experienced negative behaviours towards their less than full time working status. Of the respondents, 44% reported stress, 25% reported a lack of autonomy and 17% reported feeling burnt out at work at least once a week. A total of 85% perceived that they did not have access to a mentoring service.
Conclusions
Plastic surgery remains a popular and highly competitive surgical speciality in the UK, and many trainees reported high levels of satisfaction during their training. Aspects of training that could be improved have been highlighted and recommendations made accordingly.
Keywords: Surgical training, Plastic surgery, PLASTA
Introduction
Plastic surgery training continues to evolve in the UK. It is recognised that various initiatives have had a significant impact on UK surgical training, including the Shape of Training Report,1 European Working Time Directive2 and the drive for a consultant-delivered health service.3 As a result of these healthcare drivers, there is a movement towards a shorter training programme with an outcome-based rather than a time-served curriculum. The quality of surgical training in plastic surgery, therefore, has never been more important.
The UK plastic surgery training pathway, following graduation from medical school, involves completion of the Foundation Programme (2 years) followed by the Core Surgery Programme (2 years), before entrance into the plastic surgery training programme (6 years). Plastic surgery trainees are awarded a National Training Number (NTN) and are allocated to one of the 12 deaneries in the UK. The Joint Committee for Surgical Training (JCST) is responsible for the national administration of training and has published 22 quality indicators, which include 2 h of facilitated formal teaching per week and the opportunity to receive simulation training.4 The JCST has also published guidance for the Certification of Completion of Training (CCT), which include the achievement of indicative numbers in a range of emergency and elective operative procedures (Table 1).5
Table 1.
JCST Indicative Surgical Logbook numbers for UK plastic surgery training to be completed by each trainee during their 6-year training programme.5
| Operation | Indicative Number | |
|---|---|---|
| Elective Competencies | Dupuytren's contracture surgery | 24 |
| Lymph node clearance | 15 | |
| Free tissue transfer | 27 | |
| Breast reconstruction | 40 | |
| Aesthetic | 100 | |
| Excision skin lesion | 100 | |
| Cleft surgery | 35 | |
| Emergency Competencies | Zones 1–2 flexor tendon repair | 30 |
| Microvascular anastomosis | 35 | |
| Burns resuscitation | 18 | |
| Excisional burns surgery | 60 | |
| Hand fracture fixation | 45 | |
| Neurosynthesis | 50 | |
| Lower limb trauma | 50 |
This study aimed to determine the training experiences of current plastic surgery trainees in order to demonstrate the strengths of the UK programme and to identify areas for improvement. This is the first reported National Survey of Plastic Surgery Trainees in the UK.
Methods
Questionnaire design and distribution
A questionnaire-based cross-sectional study was designed by the UK Plastic Surgery Trainees Association (PLASTA UK, www.plasta.org), with reference to previously published guidance6 and reported according to the CHERRIES checklist for web-based surveys.7 Inspiration for the survey design was derived from annual surveys performed by the British Junior Cardiologists Association.8 The survey was built and managed using the secure web application REDCap (www.project-redcap.org) and piloted by the 14 members of the PLASTA Committee to ensure that questions were concise and without bias.
The survey questions (available online as supplementary material) covered the following seven domains:
-
1.
Demographics of participants
-
2.
Subspecialty career aspirations with options derived from subspecialties identified in a national workforce planning report9
-
3.
Training opportunities available within each region in line with the JCST quality indicators.4
-
4.
Additional qualifications achieved during training
-
5.
Fellowship aspirations during training
-
6.
Flexible working and pregnancy during training
-
7.
The risk of burnout was investigated by asking respondents how often they experienced risk factors, including stress and a lack of autonomy, and additionally, how often they felt ‘burnt out’ at work. Response options were ‘never’, ‘rarely’, ‘once a month’, ‘once a week’ and ‘most days’.
UK plastic surgery trainees in England, Wales, Scotland and Northern Ireland with a current NTN were eligible for inclusion and were sent to the closed survey link via email and web-based messaging platforms. Trainees were given a 6-month window between November 2018 and April 2019 to respond to the survey. Trainees were rewarded for completing the survey by being given the opportunity to enter into a prize draw by anonymous text message in an attempt to increase the response rate.10
Data analysis
Only fully completed surveys were included in the analysis. Survey responses were analysed using the REDCap application, which facilitated completeness checks and descriptive analysis. Statistical subgroup analysis by sex and stage of training within categorical data outcomes was performed using the chi-square test within the R Project for Statistical Computing (http://www.R-project.org/). Risk ratios, 95% confidence intervals and P values were reported. Survey sample size calculations were based on standard published formulae for categorical data collection in surveys.11
Results
Demographics of survey participants
Out of the 320 current UK plastic surgery trainees (41%), 131 submitted complete responses to the questionnaire. Among these trainees, 53% were male and 47% were female. The respondents spanned all 6 years of higher surgical training from ST3 to 8 as shown in Figure 1. Responses were obtained from trainees in all 12 UK regions as shown in Table 2.
Figure 1.
Bar chart to show the number of respondents in each of the six training years from ST3 to 8.
Table 2.
Location by region of respondents.
| Region | Number of trainees per region in 2018/2019 | Number of survey respondents (% per region) |
|---|---|---|
| East of England | 31 | 7 (23%) |
| East Midlands | 11 | 4 (36%) |
| London and Southeast | 70 | 29 (41%) |
| North East | 21 | 8 (38%) |
| North West | 40 | 12 (30%) |
| Thames Valley/Wessex | 30 | 17 (57%) |
| South West | 15 | 9 (60%) |
| West Midlands | 24 | 13 (54%) |
| Yorkshire and Humber | 29 | 14 (48%) |
| Wales | 11 | 6 (54%) |
| Scotland | 37 | 9 (24%) |
| Northern Ireland | 4 | 3 (75%) |
| Total | 320 | 131 (41%) |
Subspecialty aspirations
The most popular first choice career subspecialisation areas were hand surgery (20%), cleft lip and palate (12%), lower limb reconstruction (12%) and oncoplastic breast reconstruction (12%) as shown in Figure 2.
Figure 2.
Bar chart to portray the first choice subspecialty aspirations of UK plastic surgery trainees for 15 subspecialty areas within plastic surgery.
Training opportunities
The majority of respondents (75%) said that deaneries tailored their rotations to the context of individual training needs. Trainees identified positive and negative attributes of the departments that they rotated through in their regions (Table 3).
Table 3.
Attributes of UK plastic surgery units that were perceived by respondents as being good at training or poor at training.
| Attributes of good training units | Attributes of poor training units |
|---|---|
| Supportive consultants and positive team atmosphere | Lacking support and mentorship from the consultant body |
| Autonomy to make decisions | Lack of autonomy |
| Regular protected teaching | Lack of protected teaching |
| Access to teaching facilities such as a microsurgery wet lab | More time spent providing service provision rather than training |
| Broad range of subspecialty exposure | Low volume unit for indicative procedures |
| Positive team atmosphere | Negative team atmosphere |
| Rota gaps and staff shortages |
Of the respondents, 60% received 2 h of protected teaching time a week locally and four regional training days per year. In white space responses, respondents emphasised the importance of formalised teaching and voiced their frustration at the adhoc nature of teaching in many training regions. Thirty-five per cent of respondents reported a cadaveric simulation training programme provided within their deanery.
Of the 14 JCST indicative procedures, five were highlighted by respondents as difficult to achieve and these were lymph node dissections, Dupuytren's contracture surgery, cleft surgery, aesthetic surgery and burns resuscitation. A total of 43% respondents thought it was possible to achieve all of their indicative operative numbers within their own training region. Of the trainees, who could not satisfy their indicative numbers in their allocated training region, 39% reported the existence of a formal pathway for them to go out of their region to achieve the required indicative operative numbers and 82% respondents said that their deanery did not provide integrated aesthetic training.
Additional qualifications
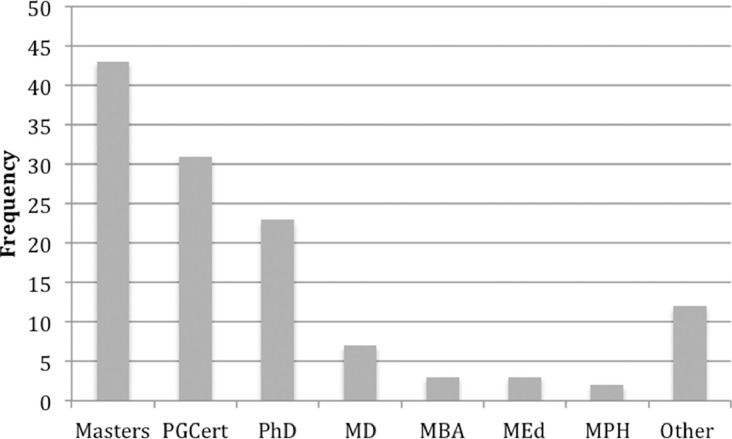
Of the respondents, 89 (68%) had gained at least one additional qualification during training (see Figure 3), but only 23% respondents had taken time out of training to obtain these qualifications. There was no significant difference between the proportion of male and female trainees who had taken time out for additional qualifications during training (male 23% vs female 21%; risk ratio 1.07; 95% confidence interval 0.5–0.2, p = 0.8).
Figure 3.
Bar chart to show frequency of additional qualifications achieved during training by 89 (68%) respondents in this survey. Common degree programmes included Masters, Postgraduate Certificate (PGCert), Doctor of Philosophy (PhD), Doctor of Medicine (MD), Masters of Business (MBA), Master of Education (MEd) and Master of Public Health (MPH).
Fellowships
Most of the respondents (89%) had not yet been on a fellowship. Of the respondents, 82% said that they wanted to undertake a pre-CCT fellowship. Of the respondents, 81% said that they would consider a UK-based Training Interface Group (TIG) fellowship and 53% said that they would consider a non-TIG fellowship. Many trainees did not know whether their deanery would be supportive of them undertaking a pre-CCT fellowship or in what form they would be taken (i.e. Out Of Programme for Experience (OOPE), or Out Of Programme for Training (OOPT)).
Flexible training
Sixty-six per cent of respondents were not familiar with eligibility guidelines relating to flexible training (working less than full time). Nineteen respondents (15%) were currently engaged in flexible training and this was mostly for childcare purposes (90%). Out of these 19, only one (5%) was male. Of the respondents, 84% currently training flexibly reported the application process to be easy, but the practicalities were less straightforward with 32% having secured a contract to reflect expected working hours and 10% told in writing what they would get paid. Ninety per cent reported experiencing negative attitudes and behaviours in the work place regarding their flexible training status.
Twenty-three respondents (38% of the female cohort) had been pregnant during plastic surgery training. Of these, 57% felt well supported and well informed by their employer throughout pregnancy. Forty-four per cent reported continuing with working practices that they felt were unsafe for their stage of pregnancy for reasons including feeling concerned about colleague perception and missing training opportunities if they did not perform these practices.
Burnout
Of the respondents, 57% reported the workload during training to be just right, 44% reported feelings of stress at work, 25% reported insufficient autonomy and 17% reported feeling burnt out at least once a week. Gender or grade did not affect the risk of being stressed or for lack of autonomy, but there was a trend for a higher risk of feeling burnt out among senior trainees (see Table 4). Eighty-five per cent of the trainees said that there was no formal mentoring service available to them other than clinical and educational supervisors.
Table 4.
The frequency of experiencing of stress, lack of autonomy and burnout at least once a week at work by plastic surgery trainees. Analysis by sex (male/female) and level of seniority (ST3–5/ST6–8) with risk ratios, 95% confidence intervals (CI) and P values were reported.
| Percentage | Risk ratio | 95% CI | P value | ||
|---|---|---|---|---|---|
| Stress | |||||
| Male | 40 | 0.9 | 0.6–1.4 | 0.6 | |
| Female | 44 | ||||
| ST3–5 | 45 | 1.1 | 0.7–1.6 | 0.8 | |
| ST6–8 | 43 | ||||
| Lack of Autonomy | |||||
| Male | 27 | 1.3 | 0.7–2.8 | 0.3 | |
| Female | 20 | ||||
| ST3–5 | 23 | 0.8 | 0.4–1.6 | 0.3 | |
| ST6–8 | 28 | ||||
| Burnout | |||||
| Male | 19 | 1.3 | 0.5–3 | 0.6 | |
| Female | 15 | ||||
| ST3–5 | 11 | 0.45 | 0.2–1 | 0.05 | |
| ST6–8 | 24 | ||||
Discussion
This survey offers a unique insight into the training experience of UK plastic surgery trainees, which can be used to inform workforce planning and highlight strengths and weaknesses of the training programme.
The most popular desired subspecialties for trainees were hand, cleft lip and palate, oncoplastic breast and lower limb reconstruction. This correlates, in part, with the most common UK plastic surgery consultant sub-specialty interests reported in 2018.9 Skin cancer was not within the top four subspecialty trainee preferences, despite being the most common plastic surgery consultant interest. Skin cancer forms a vital element of plastic surgery workflow due to the volume and prevalence of the disease, so the data from this survey may be used in mentoring discussions with trainees about aligning career aspirations with the reality of UK workforce demands. The popularity of cleft lip and palate surgery in this survey is not in line with the small number of specialist cleft training opportunities and indicates the competitive nature of entering into this interface subspecialty.12
This survey reports high levels of satisfaction from trainees regarding the way in which their training was delivered on a regional basis as per previous assessments of the UK plastic surgery training programme.13,14 Unsurprisingly, good training units were characterised by a supportive atmosphere, protected teaching and the ability for trainees to work autonomously, with the opposite being true for units considered to train poorly. Training regions should strive to facilitate training placements with a regular, well-organised teaching programme that fosters a supportive training environment.
The survey results suggest regional variation within UK plastic surgery training with inequality in the delivery of the JCST quality indicators or opportunities for trainees to achieve indicative logbook numbers. Forty per cent of the respondents were not getting access to the minimum requirement of 2 h of protected teaching each week. Deaneries that provided simulated cadaveric teaching should be commended, but were in the minority. The JCST should ensure that their quality indicators are delivered in each region, and if opportunities to achieve certification do not exist locally, then a formalised pathway should be in place for trainees to access areas of the curriculum externally.
Difficulties regarding indicative logbook numbers were largely related to elective procedures as opposed to emergency operative procedures. These included Dupuytren's contracture surgery that is often contracted outside of mainstream National Health Service (NHS) to independent providers.15 Access to aesthetic surgery is problematic for trainees as many training regions have not reacted to the changes in NHS practice and developed an integrated model for training in aesthetic surgery within training programmes.16 Lymph node basin dissections have become less commonly performed following the recommendations of the Multicentre Selective Lymphadenectomy Trial 2 (MSLT2)17 and the rapid non-operative advances that are taking place in the management of stage 3 and 4 melanomas.18 Cleft lip and palate surgery and management of burns are only accessible in certain units due to centralisation of services.19,20 While it is likely that the training body as a whole would support maintaining the breadth of the curriculum in plastic surgery, alteration of the indicative numbers to align with the service that UK plastic surgeons provide should be considered. Furthermore, there is an urgent need for the JCST, Royal Surgical Colleges and specialty Associations to work together with the independent sector to develop a model for training in aesthetic surgery that adequately meets the needs of trainees and the health service in the UK. This aligns with the Paterson inquiry report, that recommended up-regulation of the independent health sector to match standards within the NHS.21
The most common postgraduate qualifications obtained by trainees were master's degrees and postgraduate certificates, which tend to be 1–2-year duration and can often be undertaken part-time alongside training. These data would also suggest that completion of a higher research degree, such as an MD or PhD, is increasingly becoming the preserve of trainees who wish to pursue academia as part of their consultant job plan. The pathway is becoming an increasingly formalised through the development of academic clinical fellow posts. It is vital to ensure that those who wish to pursue academia have access to appropriate research opportunities that are of high quality will lead to the maintenance of the academic basis for plastic surgery to promote future advancement and innovation.
Trainees clearly demonstrated their support for pre-CCT and TIG fellowships in particular. TIG Fellowships have been available to trainees over the past decade and can currently be undertaken in hand surgery, cleft lip and palate, oncoplastic breast surgery, head and neck surgery and trauma surgery.22 Plastic surgery trainees are in direct competition with trainees from other parent surgical specialties during the application process. Training programme directors should be encouraged to be transparent about their position on fellowships so that trainees can prepare for competitive application processes well in advance.
Flexible training is becoming more common in UK surgical training.23 It is not surprising that this survey showed the vast majority of plastic surgery trainees training flexibly were female. For the last 25 years, females have outnumbered males entering medical school24 and plastic surgery has one of the highest proportions of female trainees, measured at 40% in 2018.25 In this survey, 90% of trainees training flexibly reported experiencing negative attitudes from colleagues at work and these results are similar to a previous survey of UK surgical trainees.23 There is an opportunity to improve the experience for trainees training flexibly by putting support systems in place to ensure the risk of discrimination is minimised.
It is concerning that pregnant trainees were performing activities that they thought could cause risk to their unborn baby. Increasing number of females in higher surgical training means that a greater proportion of trainees will be pregnant during their training.26 Poor institutional maternity support has been previously highlighted by plastic surgeons in the United States27 and by UK surgical trainees.28 It is essential that Plastic Surgery Departments ensure that they have good quality systems in place to support pregnant trainees, so that they continue to be attracted to the specialty and are able to train safely.
In this survey, 60% reported their workload to be just right, which correlates with recent General Medical Council (GMC) surveys to show that satisfaction among plastic surgery trainees is well above the national average for specialist trainees in general.29 This may be one of the reasons why plastic surgery remains a popular specialty for UK surgical training and is one of the most competitive specialties with competition ratios for NTNs at 4:1 in 2019.30 Of great concern, however, was the number of trainees was reporting feelings of stress, lack of autonomy and burnout. Burnout is most commonly defined according to Maslach's concept and consists of three elements: emotional exhaustion, depersonalisation and reduced sense of personal accomplishment.31 For physicians, risk factors for burnout include stress and lack of autonomy at work.32 Burnout correlates with impairment of the professional and personal lives of surgeons, and reduces quality of care to patients.33 Surveys performed in the United States of America have found plastic surgeons to be at high risk for burnout.34,35 A recent systematic review has estimated the risk of burnout among plastic surgery trainees to be 36%.33
It is important to be able to diagnose burnout in order to effectively prevent it.32 Our survey findings suggest a higher prevalence of feeling burnt out at least once a week among senior trainees (ST6–8), but it is clear that risk factors (stress and lack of autonomy) are problems shared across all of the trainee subgroups. PLASTA would advocate the formation of a nationally recognised mentoring system for plastic surgery to facilitate the diagnosis and swift action to support trainees with symptoms of burnout.
The main strength of this study was the representative sample of UK plastic surgery trainees, which was inclusive of variation in sex, training progression and regional location. The response rate of 41% from the target population was sufficiently representative for categorical data analysis with an accepted 5% margin of error.11 The limitations inherent to survey design included recall bias and negative reporting bias that may be associated with responders to a survey perceived to highlight problems with training provision.
Conclusions and recommendations
Plastic surgery remains a popular and highly competitive surgical speciality in the UK, and many trainees reported high levels of satisfaction during their training. Areas of concern raised in this survey provide an opportunity to improve the delivery of plastic surgery training in the UK for present and future trainees.
PLASTA recommendations for UK plastic surgery training:
-
1.
The JSCT should ensure that the regional delivery of UK plastic surgery training is standardised according to its quality indicators. Specifically, trainees should receive 2 h of teaching each week and have the opportunity for simulation training in their deanery. If opportunities to achieve certification do not exist in the training region, then a formalised plan should be in place for trainees to access learning outside of the region.
-
2.
The JCST, Royal Surgical Colleges, Surgical specialty Associations and independent sector should work together to develop a model for training in aesthetic surgery within the UK independent healthcare sector that promotes responsible and regulated practice.
-
3.
Training regions should be transparent about their position on pre-CCT fellowships, so that the trainees can prepare for competitive application processes well in advance.
-
4.
Training regions should ensure support systems for plastic surgery trainees training flexibly and pregnant trainees are in place, to minimise the risk of discrimination.
-
5.
PLASTA would support the formation of a nationally recognised mentoring system for plastic surgery to facilitate the diagnosis and swift action for trainees and surgeons with symptoms of burnout.
-
6.
PLASTA should survey UK plastic trainees on an annual basis to report trends in training
Declaration of Competing Interest
The authors have no conflict of interest to declare. All authors were elected members of the PLASTA Committee. The PLASTA Committee received financial and logistical support from BAPRAS for the financial year 2018–2019 when this survey took place.
Acknowledgments
Funding
None
Acknowledgements
The authors are grateful to Matthew Gardiner and Kennedy REDcap for the use of the web-based questionnaire tool. This study did not receive any specific funding, and the authors are also thankful to PLASTA for its financial and logistical support from BAPRAS during the study period. The authors are grateful for the UK Plastic Surgery Trainees who responded to the national training survey.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jpra.2020.06.003.
Contributor Information
Matthew Fell, Email: mattfell@doctors.org.uk.
Collaborating Authors:
Kavit Amin, James Coelho, Michelle Collins, Elizabeth Concannon, Asmat Din, Susan Hendrickson, Calum Honeyman Amer Hussain, Ian King, Karen Lindsay, Serena Martin, Rikki Mistry, Nicholas Segeren, Vikram Sharma, Dimitris Reissis, Clare Rivers, Claire Sin-Hidge, Kirsty Smith, Natasha Wielogorska, Jennifer Wilson, Justin Wormald, and Katie Young
Appendix. Supplementary materials
References
- 1.Harries R.L., Williams A.P., Ferguson H.J.M. The future of surgical training in the context of the ‘Shape of Training’ Review: consensus recommendations by the Association of Surgeons in Training. Int J Surg. 2016;36:S5–S9. doi: 10.1016/j.ijsu.2016.08.238. [DOI] [PubMed] [Google Scholar]
- 2.Fitzgerald J.E., Caesar B.C. The European Working Time Directive: a practical review for surgical trainees. Int J Surg. 2012;10(8):399–403. doi: 10.1016/j.ijsu.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Mohan H.M., Gokani V.J., Williams A.P. Consultant outcomes publication and surgical training: consensus recommendations by the association of surgeons in training. Int J Surg. 2016;36:S20–S23. doi: 10.1016/j.ijsu.2016.09.077. [DOI] [PubMed] [Google Scholar]
- 4.Joint Committee for Surgical Training. Plastic Surgery Quailty Indicators. https://www.jcst.org/quality-assurance/quality-indicators/[Accessibility verified February 9, 2020].
- 5.Joint Committee for Surgical Training. UK Plastic Surgery Certification Guidance. https://www.jcst.org/quality-assurance/certification-guidelines-and-checklists/[Accessibility verified February 9, 2020].
- 6.Jones T.L., Baxter M., Khanduja V. A quick guide to survey research. Ann R Coll Surg Engl. 2013;95(1):5–7. doi: 10.1308/003588413X13511609956372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) J Med Internet Res. 2004;14(1):e8. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yazdani M.F., Kotronias R.A., Joshi A. British cardiology training assessed. Eur Heart J. 2019;40(30):2475–2477. doi: 10.1093/eurheartj/ehz545. [DOI] [PubMed] [Google Scholar]
- 9.British Association of Plastic, Reconstructive and Aesthetic Surgeons. BAPRAS Workforce Planning. http://www.bapras.org.uk/media-government/news-and-views/view/workforce-planning-survey-now-available[Accessibility verified February 9, 2020].
- 10.Edwards P.J., Clarke M.J., Roberts I. Methods to increase response to postal and electronic questionnaires (Review) Cochrane Libr. 2009;3(3) doi: 10.1002/14651858.MR000008.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bartlett J.E., Kotrlik J., Higgins C. Organizational research: determining appropriate sample size in survey research appropriate sample size in survey research. Inf Technol Learn Perform J. 2001;19(1):43. [Google Scholar]
- 12.Drake-Lee A., Sandhu D. The future training of surgeons to manage patients with cleft lip and palate disorders. Br J Hosp Med. 2012;73(2):101–105. doi: 10.12968/hmed.2012.73.2.101. [DOI] [PubMed] [Google Scholar]
- 13.Kamali P., Van Paridon M.W., Ibrahim A.M.S. Plastic surgery training worldwide: part 1. The United States and Europe. Plast Reconstr Surg Glob Open. 2016;4(3):1–9. doi: 10.1097/GOX.0000000000000627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Highton L., Lamb A., Fitzgerald A. An analysis of the operative experience of plastic surgery trainees in the United Kingdom using eLogbook. J Plast Reconstr Aesthetic Surg. 2017;70(10):1464–1471. doi: 10.1016/j.bjps.2017.05.020. [DOI] [PubMed] [Google Scholar]
- 15.Shewring D., Hobby J., Warwick D. NHS plan to restrict funding is not based on high quality data. BMJ. 2018;362(September):3743. doi: 10.1136/bmj.k3743. [DOI] [PubMed] [Google Scholar]
- 16.Pantelides N.M., Highton L., Lamb A. An analysis of the cosmetic surgery experience acquired through UK plastic surgery training. J Plast Reconstr Aesthetic Surg. 2018;71(11):1532–1538. doi: 10.1016/j.bjps.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 17.Faries B., Thompson J.F., Cochran A.J. Completion dissection or observation for sentinel-node metastasis in melanoma. N Engl J Med. 2017;376(23):2211–2222. doi: 10.1056/NEJMoa1613210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peach H., Board R., Cook M. Current role of sentinel lymph node biopsy in the management of cutaneous melanoma: a UK consensus statement. J Plast Reconstr Aesthetic Surg. 2020;73(1):36–42. doi: 10.1016/j.bjps.2019.06.020. [DOI] [PubMed] [Google Scholar]
- 19.Colbert S.D., Green B., Brennan P.A. Contemporary management of cleft lip and palate in the United Kingdom. Have we reached the turning point? Br J Oral Maxillofac Surg. 2015;53(7):594–598. doi: 10.1016/j.bjoms.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 20.British Burns Association. National Burn Care Review Committee. Standards and Strategy for Burn Care: a Review of Burn Care in the British Isles 2001. https://www.britishburnassociation.org/national-burn-care-review/[Accessibility verified February 9, 2020].
- 21.UK Government. Report of the Independent Inquiry into the Issues Raised by Paterson. https://www.gov.uk/government/publications/paterson-inquiry-report[Accessibility verified February 9, 2020].
- 22.Lees V., Henley M., Sandhu D. Interface specialty training in the UK. Ann R Coll Surg Engl. 2010;92:126–128. [Google Scholar]
- 23.Harries R.L., Gokani V.J., Smitham P. Less than full-time training in surgery: a cross-sectional study evaluating the accessibility and experiences of flexible training in the surgical trainee workforce. BMJ Open. 2016;6(4):1–7. doi: 10.1136/bmjopen-2015-010136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moberly T. Number of women entering medical school rises after decade of decline. BMJ. 2018;360:k254. [Google Scholar]
- 25.Moberly T. A fifth of surgeons in England are female. BMJ. 2018;363:1–2. doi: 10.1136/bmj.k4530. [DOI] [PubMed] [Google Scholar]
- 26.Turner P.L., Lumpkins K., Gabre J. Pregnancy among women surgeons: trends over time. Arch Surg. 2012;147(5):474–479. doi: 10.1001/archsurg.2011.1693. [DOI] [PubMed] [Google Scholar]
- 27.Furnas H.J., Li A.Y., Garza R.M. An analysis of differences in the number of children for female and male plastic surgeons. Plast Reconstr Surg. 2019;143(1):315–326. doi: 10.1097/PRS.0000000000005097. [DOI] [PubMed] [Google Scholar]
- 28.Mohan H., Ali O., Gokani V. Surgical trainees’ experience of pregnancy, maternity and paternity leave: a cross-sectional study. Postgrad Med J. 2019;95(1128):552–557. doi: 10.1136/postgradmedj-2018-135952. [DOI] [PubMed] [Google Scholar]
- 29.Miller R., Beaumont O., Pywell S. A review of satisfaction with plastic surgery training in the UK. Int J Surg. 2018;55(2018):S88. [Google Scholar]
- 30.Health Education England. Competition Ratios. https://specialtytraining.hee.nhs.uk/Competition-Ratios. [Accessibility verified February 9, 2020].
- 31.Galaiya R., Arulampalam T. Talking the Talk, but Not Walking the Walk : can interventiona programmes reduce levels of burnout? R Coll Surg Engl Bull. 2020;22(5):60–62. [Google Scholar]
- 32.Khansa I., Janis J.E. A growing epidemic: plastic surgeons and burnout – A literature review. Plast Reconstr Surg. 2019:298–305. doi: 10.1097/PRS.0000000000005875. [DOI] [PubMed] [Google Scholar]
- 33.Ribeiro R.V.E., Martuscelli O.J.D., Vieira A.C. Prevalence of burnout among plastic surgeons and residents in plastic surgery: a systematic literature review and meta-analysis. Plast Reconstr Surg Glob Open. 2018;6(8):1–5. doi: 10.1097/GOX.0000000000001854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shanafelt T.D., Balch C.M., Bechamps G.J. Burnout and career satisfaction among american surgeons. Ann Surg. 2009;250(3):463–470. doi: 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 35.Qureshi H.A., Rawlani R., Mioton L.M. Burnout phenomenon in U.S. Plastic Surgeons: risk factors and impact on quality of life. Plast Reconstr Surg. 2015;135(2):619–626. doi: 10.1097/PRS.0000000000000855. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.