Abstract
Objective
Closing-wedge high tibial osteotomy (CWHTO) for medial osteoarthritis of the knee is one of the effective osteotomy methods, especially for patients with cartilage damage of the patellofemoral joint, flexion contracture, and requiring a large correction angle.While the bone union at the osteotomy site is finally obtained after CWHTO, there are often differences in the period of the bone union. The purpose of the present study is to investigate the factors affecting the timing of bone union after CWHTO.
Methods
16 cases of CWHTO were included; they were performed by the same surgeon using precisely the same implants. Among 16 cases in the present study, nobody used low-intensity pulsed ultrasound (LIPUS) within three months after the operation. The patients were divided into two Groups using Plane X-ray and CT within three months after surgery: Group D (8 knees; bone healing was not seen at all) and Group E (8 knees; bone healing was seen).
Results
There were no significant differences in mean age between the two groups, but body mass index (BMI) and bone mineral density (BMD) were significantly higher in Group D (p < 0.05).
Conclusion
The present study suggests that BMI and BMD may affect the timing of bone union after CWHTO.
Background
Closing-wedge high tibial osteotomy (CWHTO) for medial osteoarthritis of the knee is one of the effective osteotomy methods. The frequency of selecting CWHTO in our hospital in Japan is high, especially for patients with cartilage damage of the patellofemoral joint, flexion contracture, and requiring a large correction angle. On the other hand, while the bone union at the osteotomy site is obtained with both procedures, there are often differences in bone union time for CWHTO compared to Opening-wedge high tibial osteotomy (OWHTO). This difference might affect the early clinical outcome of the operations. We hypothesized that there is some factor to affect bone healing of CWHTO for individual patients.
Purpose
To investigate the factors affecting the timing of bone union after CWHTO.
Keywords: Closing-wedge high tibial osteotomy(CWHTO), BMD, BMI, Bone union timing, Delayed union, Risk factor
1. Material and methods
16 cases of CWHTO were performed by the same surgeon in our hospital from 2017 to 2019 with precisely the same implants (Lateral HTO plate manufactured by Olympus Inc). Included patients did not use low-intensity pulsed ultrasound (LIPUS) within three months after surgery.
Surgery was performed by bi-plane osteotomy from 4 cm distal to the lateral tibial joint surface. The ascending cut was performed while maintaining the thickness of flange (thickness of tubercle) at one third of the tibia, with the cutting angle of the ascending plane being 100° to the oblique plane. Fibula osteotomy was initially performed from 15 mm to 20 mm (depend on correction angle) in the mid portion. No bone transplantation was performed in all cases.
The day after the operation, knee range of motion training was started. Partial wright bearing was started one week after the operation according to the patient’s pain.
Bone healing was investigated retrospectively using the plane X-ray and Computerized tomography (CT), which were performed within three months after surgery. In eight cases, bone healing was not seen at all, and these cases were designated as the delayed group (Group D). Group D was compared with Group E (which consists of the other eight knees, which showed visible bone healing at three months after the surgery) (Table 1).
Table 1.
- ∙The student t-test was used for the statistical method.
- ∙N.S.: not significant.
| Delayed Group (n = 8) | Early Group (n = 8) | ||
|---|---|---|---|
| Age | 55 (42–60) | 59 (47–73) | NS |
| Men/women | 6/2 | 2/6 | |
| BMI (kg/m2) | 25.6 (22.4–29.5) | 22.1 (19.6–25.7) | p < 0.05 |
| Correction angle (deg) | 12 (8–17) | 10 (6–15) | NS |
| Implants | Lateral HTO, 8 | Lateral HTO, 8 | |
| BMD(g/㎠) | 1.37 | 0.99 | p < 0.05 |
| Smokers | 1 | 3 |
Keywords; closing wedge HTO, BMD, BMI, bone union.
We examined age, body mass index (BMI), correction angle, and bone mineral density (BMD) measured at the lumbar spine. The student t-test was used for the statistical method.
2. Results
Patients in Group D had an average age of 55 years (42–60) compared to 59 years (47–73) in Group E; there was no significant difference between the two groups. The correction angles were 12 ± 2° (8–17) and 10 ± 2° (6–15), respectively, and no significant difference was observed. On the other hand, BMI was 25.6 kg/m2 (22.4–29.5) for Group D, 22.1 kg/m2 (19.6–25.7) for Group E, BMD was 1.37 ± 0.16 g/㎠ for Group D and 0.99 ± 0.2 g/㎠ for Group E, that was also significantly higher in Group D (p < 0.05) (Table 1).
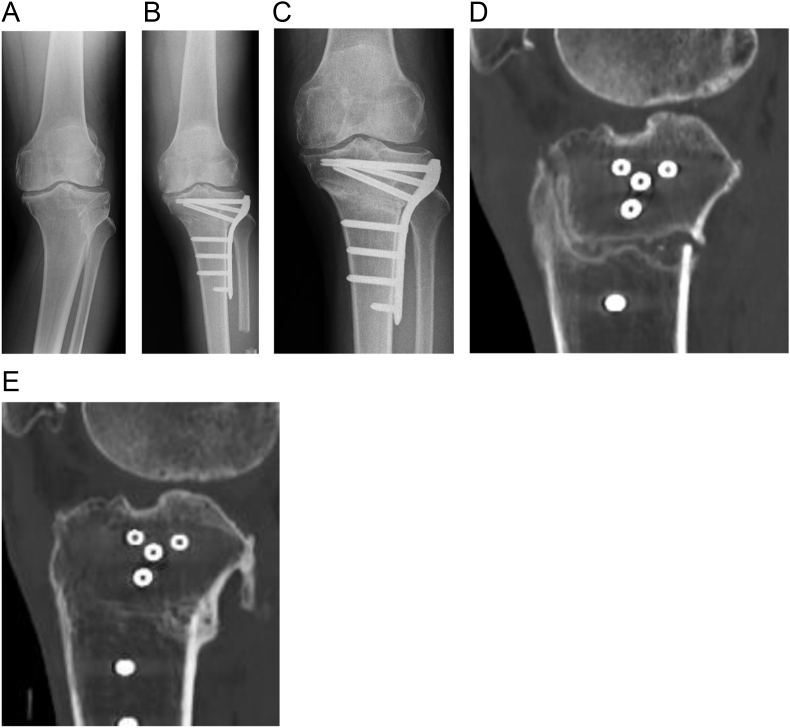
2.1. The representative case of Group D
60-year-old male (BMI was 25.5 kg/m2, no smoking history), CWHTO was performed for left knee osteoarthritis (Fig. 1a and b). The varus knee was corrected 12°, weight bearing line (WBL) was translated from 10 to 60% from the edge of the medial plateau in standing position.
Fig. 1.
a) (b) (c) (d) (e).
a) the plane X-ray in the Anteroposterior view before the operation
b) the plane X-ray in the Anteroposterior view after the operation
c) the plane X-ray in the Anteroposterior view 3 months after the operation
d) the sagittal section of the 3months postoperative CT
e) the sagittal section of the 10months postoperative CT.
The CT at ten months after surgery revealed bone union at osteotomy site (Fig. 1e). Still, at three months postoperatively no significant bone healing was seen at both ascending and descending planes (osteotomy line continuity) at the sagittal section of the CT. Partial bone resorption (which indicates delayed union) was seen on the descending plane (Fig. 1d).
At the final follow up, two years postoperatively, there was no correction loss. In this case, no use of LIPUS or other additional treatment was performed. KOOS improved from 181.3 (Symotoms21.4, PAIN33.3, ADL60.3, Sports 35.0, QOL31.3) before surgery to 348 (Symotoms75.0, PAIN66.7, ADL83.8, Sports 60.0, QOL62.5) after surgery.
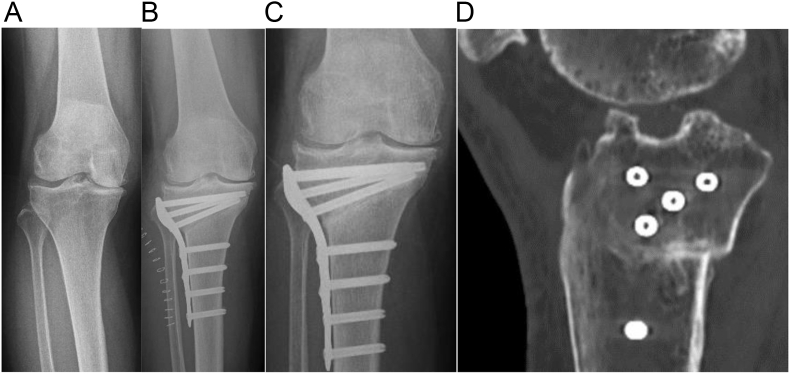
2.2. The representative case of Group E
57-year-old female (BMI was 23.6 kg/m2, no smoking history), CWHTO was performed for right knee osteoarthritis (Fig. 2a and b). The varus knee was corrected 10°, WBL was translated from 21 to 69% from the edge of the medial plateau in standing position.
Fig. 2.
a) (b) (c) (d).
a) the plane X-ray in the Anteroposterior view before the operation
b) the plane X-ray in the Anteroposterior view after the operation
c) the plane X-ray in the Anteroposterior view 3 months after the operation
d) the sagittal section of the 3months postoperative CT.
The plain X-ray showed osteosclerosis at the osteotomy site (Fig. 2c), and the Sagittal section of the CT at three months postoperatively revealed bone healing without osteotomy line continuity and bone resorption (Fig. 2d).
3. Discussion
CWHTO for medial osteoarthritis of the knee is one of the effective methods of osteotomy especially for patients accompanied by OA of the patellofemoral joint or by flexion contracture, and cases requiring a large correction angle.1,2 Though CWHTO produces the bone union, often there are differences in the timing. More men8 participated in this study, and BMIs and BMDs were significantly higher in Group D than in Group E.
There was no report about the relationship between bone union after osteotomy and BMD, as far as we are aware. In this study, BMD is significantly higher in Group D. High BMD may adversely affect bone union after CWHTO due to heat necrosis may occur or poor compression at the time of closing the osteotomy site. Still, this possibility is not definite at present, and further research is required.
Regarding bone union and BMI after osteotomy, it is thought that if BMI is significant, the fixability is relatively weak mechanically, and it works against the bone union. Dorofeev A et al.3 reported that a BMI of 30 kg/m2 or more was a predictor of mechanical complications after CWHTO. Furthermore, there is a possibility that height, weight, and BMI can be factors that affect BMD, and BMD increases as BMI increases. Głogowska-Szeląg J et al.4 reported higher BMD values with increasing BMI in postmenopausal women with osteoporosis, Ando A et al.5 reported high BMI was associated with an increase in femoral BMD. These reports are consistent with our results. Our study suggests that BMI, and BMD may affect the timing of bone union after CWHTO, and the same factors can predict bone union.
On the other hand, there is no significant difference in age in our study. There is a possibility that age may have an effect on the bone union at the osteotomy site since BMD is generally higher at a younger age.
In the present study, the number of cases is small. However, all our patients had been operated on using precisely the same implants and had not used LIPUS within three months of surgery. In addition, since it is statistically evaluated using the student t-test, it is considered that there is some reliability. On the other hand, postoperative rehabilitation has not been evaluated, which is a limitation of this study. The load start time was determined by the condition of the surgical wound and the pain, with the hospital stay between 2 and 8 weeks. The ADL from the time of discharge to the bone union was also different - some patients returned to work early, while others used crutches longer - making accurate assessment difficult. Thus, differences in the postoperative course may have influenced the results.
There are likely other factors that affect bone union after CWHTO. For example, the relationship between smoking and the time of bone union after distal femoral osteotomy6 or OWHTO7 has been reported. In our study, one smoker was in group D, three in Group E. Other factors may influence bone union besides smoking.
To accelerate the time of bone union, bone or osteophyte transplantation into closing osteotomy sites can be considered even in CWHTO, especially for patients with high BMI and high BMD. Akiyama et al.8 reported that filling the osteophyte collected under arthroscopy into the osteotomy site can be advantageous for bone healing in OWHTO. Also, among 16 cases in the present study, nobody used LIPUS within three months after the operation, so it can be another option to expedite the bone union after the procedure.
A limitation of this study is a small number of patients, so further research is needed to confirm our findings.
4. Conclusion
This study suggests that BMI, and BMD may affect the timing of bone union after CWHTO.
To accelerate the time of bone union, bone transplantation into closing osteotomy sites can be considered even in CWHTO, especially for patients with high BMI and high BMD.
Further research is required because a small number of patients were included in the present study.
References
- 1.Stoffel K., Willers C., Korshid O., Kuster M. Patellofemoral contact pressure following high tibial osteotomy: a cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2007;15(9):1094–1100. doi: 10.1007/s00167-007-0297-9. Sep. [DOI] [PubMed] [Google Scholar]
- 2.Bin S.I., Kim H.J., Ahn H.S., Rim D.S., Lee D.H. Changes in patellar height after opening wedge and closing wedge high tibial osteotomy;A meta-analysis. Arthroscopy. 2016;32(11):2393–2400. doi: 10.1016/j.arthro.2016.06.012. Nov. [DOI] [PubMed] [Google Scholar]
- 3.Dorofeev A., Tylla A., Drescher W., Stangl R. Al. Complication analysis after angle-stable CW and OW high tibial osteotomy. Orthopä. 2020 Jan;49(1):18–25. doi: 10.1007/s00132-019-03724-7. [DOI] [PubMed] [Google Scholar]
- 4.Głogowska-Szeląg J. Assessment of the relationship between bmd and body mass index bmi in women with postmenopausal osteoporosis. Wiad Lek. 2018;71(9):1714–1718. [PubMed] [Google Scholar]
- 5.Ando A., Mitsuhashi T., Honda M. Risk factors for low bone mineral density determined in patients in a general practice setting. Acta Med Okayama. 2019;73(5):403–411. doi: 10.18926/AMO/57370. Oct. [DOI] [PubMed] [Google Scholar]
- 6.Liska F., Haller B., Voss A. Smoking and obesity influence the risk of nonunion in lateral opening wedge, closing wedge and torsional distal femoral osteotomies. Knee Surg Sports Traumatol Arthrosc. 2018;26(9):2551–2557. doi: 10.1007/s00167-017-4754-9. Sep. [DOI] [PubMed] [Google Scholar]
- 7.Schröter S., Freude T., Kopp M.M. Smoking and unstable hinge fractures cause delayed gap filling irrespective of early weight bearing after open wedge osteotomy. Arthroscopy. 2015;31(2):254–265. doi: 10.1016/j.arthro.2014.08.028. Feb. [DOI] [PubMed] [Google Scholar]
- 8.Akiyama T., Okazaki K., Mawatari T., Ikemura S., Nakamura S. Autologous osteophyte grafting for open-wedge high tibial osteotomy. Arthrosc Tech. 2016;5(5):e989–e995. doi: 10.1016/j.eats.2016.04.026. Sep.5. [DOI] [PMC free article] [PubMed] [Google Scholar]