Abstract
Paralabral cysts of the shoulder are a rare cause of shoulder pain. Their association with neurological symptoms is uncommon. This case report presents an antero-inferior paralabral cyst in a painful atraumatic shoulder causing axillary and musculocutaneous nerve palsy.
The patient in the present study showed a rapidly worsening active shoulder function with dull pain in the posterior shoulder and hypoesthesia over the deltoid. Magnetic resonance imaging revealed an antero-inferior paralabral cyst. Electromyography showed a profuse denervation of the deltoid, teres minor and biceps brachii muscles.
The patient was diagnosed with a axillary and musculocutaneous nerve compression neuropathy caused by the cyst. Shoulder arthroscopy was performed with the goal of decompressing the cyst and explore the terminal branches of the brachial plexus. During surgery a partial labral tear was detected and anatomically repaired after cyst resection. Exploration of the terminal roots of the plexus brachialis showed the presence of dense fibrotic tissue that was released. Shoulder function recovered completely after surgery.
Paralabral cysts are rare and surgical management consists of cyst removal and labral repair. In presence of neurological symptoms exploring the retrocoracoid plexus may be a useful option to check for fibrosis around the nerves that could limit or slow down nerve recovery.
Keywords: Axillary, Cyst, Musculocutaneous, Nerve, Palsy, Shoulder
1. Introduction
Paralabral cysts located in anterior-inferior region are very rare and their association with neurological symptoms is uncommon.1 This case report presents an antero-inferior paralabral cyst in a painful atraumatic shoulder, causing both axillary and musculocutaneous nerve palsy.
2. Case report
A 19-year-old woman was examined in the beginning of December 2017 complaining of numbness and progressively worsening motion impairment of her right shoulder that started two months earlier without trauma. The patient was in good health and not on any regular medication. She worked as an employee and occasionally played soccer.
She complained about dull pain in the posterior aspect of the shoulder during day and night with hypoesthesia over the deltoid muscle. She had scapular dyskinesis type 2,2 loss in active shoulder motion with abduction limited to 120° and external rotation in abduction limited to 60°. Both Jobe and Palm-up tests were positive for weakness. The Lift-off and Bear-hug tests were positive with mild pain. There were no signs of shoulder instability. The patient had mild weakness in active elbow flexion when compared to the other side. Clinical examination of the cervical spine was normal. A neurological evaluation ruled out the presence of brachial plexopathies. Shoulder strength was recorded with a hand-held dynamometer (HHD) (Wunder Sa.Bi. srl, Italy) applied to the wrist (Table 1) showing significant loss of force. Magnetic resonance imaging (MRI) of the shoulder showed an antero-inferior paralabral cyst (25×10 × 10mm) not extending into the quadrilateral space (Fig. 1, Fig. 2). There were no signs of labral pathology, no rotator cuff lesions nor signs of muscle atrophy/fatty infiltration.
Table 1.
Shoulder strength recorded by HHD.
| Right shoulder | Left shoulder | |
|---|---|---|
| ER force with arm at side | 6,2 kg | 12,4 kg |
| ABD force with arm at 90° of ABD | 4 kg | 12,3 kg |
| FE force with arm at 70° of FE | 4,3 kg | 14,1 kg |
| IR force with arm at side | 9,8 kg | 20,8 kg |
ER: external rotation; ABD: abduction; FE: forward elevation; IR: internal rotation.
Fig. 1.
Antero-inferior paralabral cyst (25 × 10mm) shown on MRI Coronal view PD SPAIR.
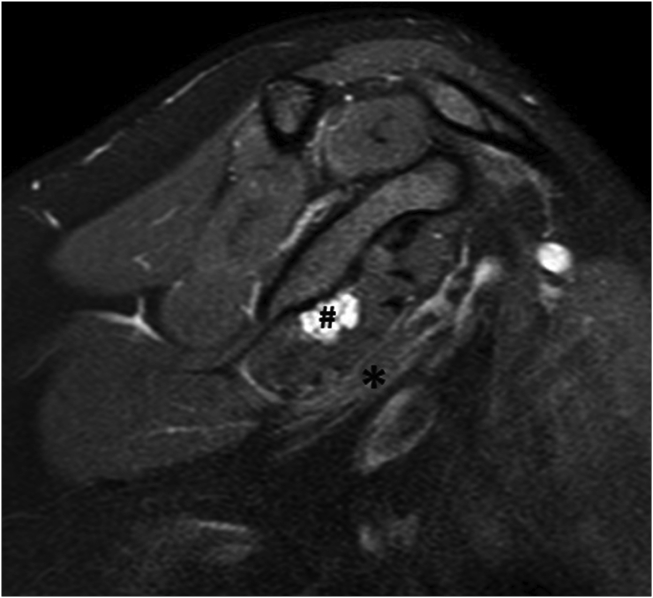
Fig. 2.
Relationship between the cyst (#) and the terminal nerve roots (*) shown on MRI Sagittal view PD SPAIR.
Electromyography (EMG) showed a reduced amplitude of compound muscle action potential of the axillary nerve. Furthermore, profuse denervation and reduction of motor unit action potential of the deltoid, teres minor and biceps brachii muscles were recorded.
The patient was diagnosed with a compression neuropathy caused by the cyst at the level of the terminal branches of the plexus afflicting the axillary and musculocutaneous nerve. Due to the clinically relevant nervous impairment, shoulder arthroscopy was performed in mid-December 2017 with the goal of decompressing the cyst and explore the terminal branches of the brachial plexus endoscopically.
3. Description of the procedure
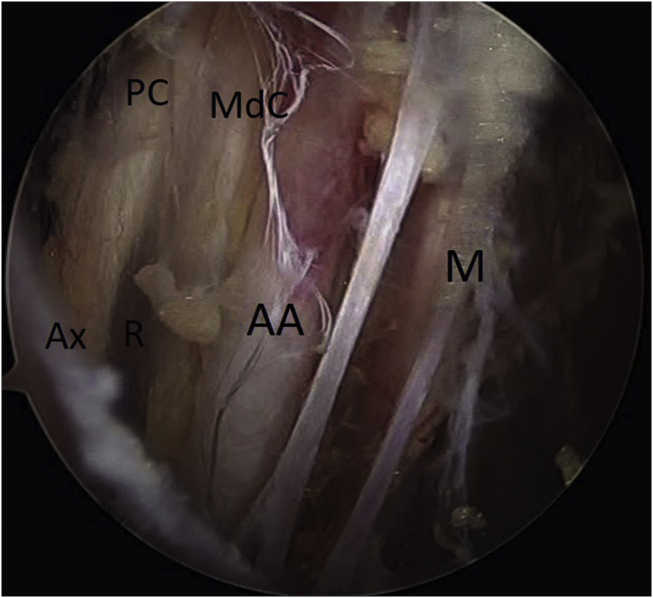
The patient was placed in a beach-chair position in general anesthesia. Arthroscopic findings showed a partial detachment of the antero-inferior labrum at the 4:30 o'clock position. The capsular-labral complex was surgically detached using a Liberator device followed by drainage of cystic fluid and resection of the cyst walls with an arthroscopic shaver. The labrum was then repaired with 3 all-suture anchors (Iconix 1, Stryker, Mahwah, NJ, USA). Subsequently, an endoscopic retrocoracoid dissection of the brachial plexus was performed. While staying in the space limited by the anterior border of the subscapularis tendon and the posterior border of the coracoid and conjoint tendon, the retrocoracoid bursa was bluntly divided giving access to the terminal branches of the plexus. Once visualized, the terminal nerve branches were surrounded by dense fibrotic tissue and were released using the blunt tip of an electrocautery device (Fig. 3.
Fig. 3.
After retrocoracoid plexus release.
AA: axillary artery
Ax: axillary nerve
M: median nerve
MdC: medial cord
PC: posterior cord
R: radial nerve.
4. Postoperative rehabilitation and outcome
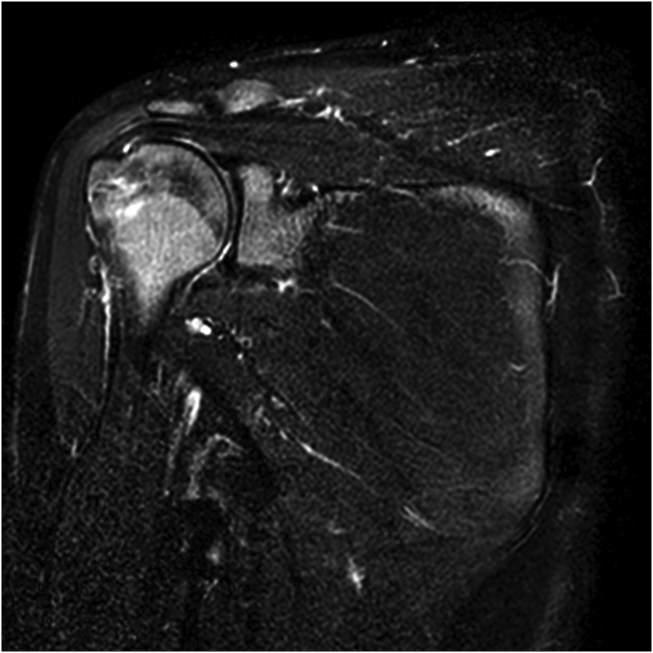
There were no post-operative complications. After surgery, the patient immediately reported complete disappearance of the posterior shoulder pain. The shoulder was positioned in a sling for 30 days, followed by standard rehabilitation program for Bankart repair. A clinical evaluation 5 months after surgery showed complete recovery of active function with no pain and equal muscle force between right and left shoulder with MRI showing complete resolution of the cyst (Fig. 4) and EMG revealing overall normal nerve function.
Fig. 4.
MRI 5 months after surgery showing no cyst recurrence. Coronal view T2 weighted DIXON.
5. Discussion
Inferior paralabral cysts are a rare condition with an estimated incidence of 0,6%.1 These cysts are highly related to labral tears and usually afflict young active male patients.1 Associations between anterior or inferior paralabral cysts with anterior/multidirectional shoulder instability and axillary compression neuropathy in the context of a quadrilateral space syndrome have been reported.3,4
Park et al.5 reported a case of compression neuropathy of the axillary nerve caused by an antero-inferior paralabral cyst in a young elite baseball player. In that case, the shoulder had no history of trauma nor signs of instability. As activity modification by physical rest relieved symptoms temporarily, the authors hypothized that the axillary nerve was dynamically compressed by the cyst during repetitive overhead throwing.
In our case a traumatic etiology that could give rise to the cyst was not identified. The presence of neurological symptoms regarding both axillary and musculocutaneous nerve were not activity related. Indeed, neurological symptoms may have been caused by static compression of the cyst on the nerves.
Cases of paralabral cysts with associated neurological symptoms are extremely rare and treatment should be aggressive in order to prevent nerve and muscle degeneration to an irreversible level. Authors' approach was to remove the paralabral cyst and repair the labral lesion. We believe anatomic repair of the labrum is mandatoy to prevent shoulder instability and avoid cyst recurrence. At present, the main application of exposing the brachial plexus endoscopically is during arthroscopic Latarjet procedure,6 massive subscapularis tears7 and neurogenic thoracic outlet syndrome.8 In our case an exploration of the plexus was performed due to the rapidly evolving nerve palsy. This evidenced diffuse fibrous adhesions around all terminal branches of the plexus that may have limited physiological gliding of the nerves during upper limb movement contributing to clinical symptoms. However, endoscopic brachial plexus exploration may seem hazardous but represents a precious surgical option in selected cases. Concerning safety of this procedure Lafosse7 stated that infraclavicular plexus dissection is feasible and reproducible. In our case, the nerve release was limited to the terminal roots because authors’ interest was to benefit from the advantages of exposing the compressed nerve roots arthroscopically thus minimizing scar tissue formation.
Concluding results of this case report suggest an accurate clinical evaluation and MRI execution in patients with shoulder pain associated with neurological symptoms. Symptoms related to paralabral cysts, when correctly identified, can be successfully treated by shoulder arthroscopy.
Conflicts of interest
Raymond Klumpp, Gianluca Gallinari, Riccardo Compagnoni and Carlo Trevisan declare that they have no conflict of interest.
Financial support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2019.09.003.
Contributor Information
Raymond Klumpp, Email: rayklu@gmail.com.
Gianluca Gallinari, Email: gianlucagallinari@hotmail.it.
Riccardo Compagnoni, Email: riccardo.compagnoni@gmail.com.
Carlo Trevisan, Email: carlo.trevisan@tiscali.it.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Jeong J.J., Panchal K., Park S.E. Outcome after arthroscopic decompression of inferior labral cysts combined with labral repair. Arthroscopy. 2015 Jun;31(6):1060–1068. doi: 10.1016/j.arthro.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Kibler W.B., McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003;11(2):142–151. doi: 10.5435/00124635-200303000-00008. Mar-Apr. [DOI] [PubMed] [Google Scholar]
- 3.Sanders T.G., Tirman P.F. Paralabral cyst: an unusual cause of quadrilateral space syndrome. Arthroscopy. 1999 Sep;15(6):632–637. doi: 10.1053/ar.1999.v15.015063. [DOI] [PubMed] [Google Scholar]
- 4.Gregory T., Sangha H., Bleakney R. Spontaneous resolution of quadrilateral space syndrome: a case report. Am J Phys Med Rehabil. 2015 Jan;94(1):e1–e5. doi: 10.1097/PHM.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 5.Park J.Y., Jeon S.H., Oh K.S., Chung S.W., Lim J.J., Bang J.Y. Compressive partial neuropathy of axillary nerve resulting from antero-inferior paralabral cyst in an adolescent overhead athlete. Korean J Sports Med. 2015 Jun;33(1):34–39. doi: 10.5763/kjsm.2015.33.1.34. [DOI] [Google Scholar]
- 6.Lafosse L., Boyle S. Arthroscopic Latarjet procedure. J Shoulder Elb Surg. 2010 Mar;19(2 Suppl):2–12. doi: 10.1016/j.jse.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 7.Lafosse T., Masmejean E., Bihel T., Lafosse L. Brachial plexus endoscopic dissection and correlation with open dissection. Chir Main. 2015 Dec;34(6):286–293. doi: 10.1016/j.main.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 8.Lafosse T., LeHanneur M., Lafosse L. All-endoscopic brachial plexus complete neurolysis for idiopathic neurogenic thoracic outlet syndrome: a prospective case series. Arthroscopy. 2017 Aug;33(8):1449–1457. doi: 10.1016/j.arthro.2017.01.050. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.