Abstract
Background
Interposition arthroplasty (IA) is one of the oldest reconstructive options for elbow arthritis and is an alternative to total elbow arthroplasty in young active patients with moderate to severe elbow arthritis. In literature there is very little, if any, mention about relationship of post-operative functional recovery and time. In this study we assess the clinical and functional outcome of interposition arthroplasty using abdominal dermal graft.
Methods
Study was conducted retrospective and prospectively during 2014-15 on 18 elbows of 17 patients (10 females and 7 male) which were operated between 2010 and 2015 for elbow arthritis by interposition arthroplasty using abdominal dermal graft by a single surgeon. Etiologically 10 cases were post-traumatic, 4 cases inflammatory joint disease and 4 cases were post-tubercular. All patients were operated using standard kochers approach and above elbow Plaster of Paris were applied in 90° flexion and mid prone position till suture removal i.e. 2 weeks and range of motion (ROM) exercises started. Post-operatively patients were reviewed on 1, 3, 6, 9, 12 months and then yearly. Functional assessments were done using Mayo Elbow Performance Score (MEPS).
Results
The mean age of the patients were 34.33 years (16 years–50 years) and follow-up duration of median 22 months (minimum 12 months and maximum 50 months). Pre-operative the ROM of the patients were 0°–75° with median value of 25° which were significantly improved to 55°–135° with median value of 120° which was statistically significant with p-value of less than 0.01. Preoperative MEPS were 15–70 with median value of 45 which was improved to 85 to 100 with median value of 95 with p-value less than 0.01. Post-operatively 14 elbows (77.8%) has excellent and 4 elbows (22.2%) has good result. 5 (27.7%) elbow has mild instability and in 3 patients has hypertrophic scar over donor site.
Conclusion
It's a very cost effective treatment as compared to total elbow arthroplasty. It provides superior functional outcome than other kind of salvageable procedure like arthrodesis and patient's satisfaction is very high after surgery as pain subsided and range of motion improved. Most of the patients returned to their previous occupation by 6 months after surgery.
Keywords: Elbow arthritis, MEPS, Interposition arthroplasty, TEA
1. Introduction
Elbow arthritis is a very debilitating condition presenting with pain, stiffness and loss of function. Rheumatoid arthritis is the most common cause followed by post-traumatic, primary osteoarthritis, post infection, crystalline arthropathy, haemophillia, and ochronosis etc.1,2
The non-operative treatment may provide symptomatic relief in majority of the patients in early stage of the disease. It includes oral analgesics, intra-articular injections, physical therapy, and hinged braces.1,2
Surgical treatment is guided by disease etiology and severity, patient age, and functional demands.1 The primary aim of the treatment is to reduce pain and improve function without compromising future surgical option. Sears et al. (2012) suggest that this requires accurate assessment of the primary patient complaint. Patients with pain and stiffness at the extremes of motion may benefit from osteocapsular debridement, arthroscopic or open. Those with advanced degeneration and symptoms throughout their arc of motion may require joint resurfacing or replacement.3 Arthroscopic or open synovectomy, debridement arthroplasty, and interposition arthroplasty are generally recommended for the young and active patient population, whereas for low-demand and elderly patients with end-stage painful arthritis, total elbow arthroplasty is considered a more suitable surgical option and resection arthroplasty and arthrodesis considered as salvage option, even though it is poorly tolerated.1
Although total elbow arthroplasty is considered the first choice in the treatment of severe elbow arthritis but in young adults with high demands it is generally avoided due to its complications like longevity issue, infection, fracture, aseptic loosening, restriction of weight lifting etc.4, 5, 6, 7
Interposition arthroplasty (IA) is one of the oldest reconstructive options for elbow arthritis described for a variety of indications. It is an alternative to total elbow arthroplasty in young active patients with moderate to severe elbow arthritis. Historically it was first introduced by Sir Defontaine in 1887.10 It attempts to create a painless pseudoarthrosis of the elbow by resecting and resurfacing the articular surfaces by inserting various interposition material.2 Interposition arthroplasty preserves bone stock, and if needed total elbow arthroplasty can be done successfully later on.11
Various interposition materials have been used till now. But the most commonly used materials are dermal graft, allogenic Achilles tendon graft, tensor fascia lata and others are bovine collagen membrane, gelfoam, allograft cadaveric dura matter etc.2,9
In literature there is very little, if any, mention about the time required for functional outcome after surgery. This study was conducted to assess the clinical and functional outcome of interposition arthroplasty using abdominal dermal graft and to know the relationship between functional outcome and recovery time after surgery.
2. Material and methods
The study was conducted during the period of 2014–2015 on eighteen elbows of 17 patients, 10 female and 7 male were included for the study. All the patients operated for elbow arthritis with interposition arthroplasty using abdominal dermal graft from 2010 to 2013 were included and reviewed and cases operated from 2014 to 2015 were included and followed up prospectively.
2.1. Inclusion Criteria:
Patient up to 50 years of age with Stiff and painful elbow due to intrinsic cause.
2.2. Exclusion Criteria:
-
1.
Active Infection
-
2.
Gross elbow instability
-
3.
Congenital ankylosis
-
4.
Noncompliant patient
2.3. Study design
All the patients based on inclusion and exclusion criteria, were taken for study. Detailed demography of every patient and clinical history and thorough physical examination were done with special attention given for any ulnar nerve involvement and stability was assessed. The functional score were calculated according using Mayo Elbow Performance Score (MEPS16) and range of motion noted.
Every patients were investigated thoroughly with routine blood investigations which would include Haemoglobin, TLC, DLC, PCV, platelet count, ESR, RBS, Blood urea, S.creatinine, Virology markers and in case of polyarthritis CRP and RA factor were done and if the patient's age is above 30 yrs then he/she were investigated for x-ray chest PA view and electrocardiography as a part of pre-anaesthetic investigation. Informed written consent was duly taken from all patients before surgical intervention.
Proper evaluation of the Cases of post-infective tubercular arthritis was done with history of Anti tubercular medication, minimum 1 year of free from constitutional symptoms and normal ESR and CRP level.
Plain radiograph of elbow includes AP view and Lateral views were done.
2.4. Operation technique
The standard Extensile Kocher deep lateral approach was used.9
Anaesthesia was given in the form general anaesthesia with/without regional block. The patient was placed supine on the operating table with a large pillow or bolster under the ipsilateral shoulder, allowing the operated extremity to rest across the trunk for the procedure. Pneumatic tourniquet was applied as proximally as possible on the upper arm. The upper extremity as well as donor site was painted and draped under aseptic precautions as per standard hospital protocol.
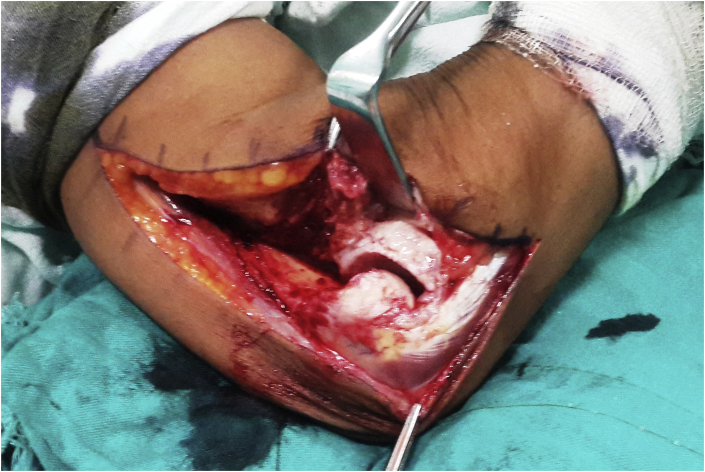
A posterior lateral skin incision was given (Fig. 1). Subcutaneous tissue dissected and flaps elevated to identify Kocher's interval (Fig. 2). It proceeds down the supracondyler ridge of the humerus between Extensor carpi ulnaris and Anconeus muscle. The common extensor origin, lateral collateral ligament and periosteum are dissected off of the lateral condyle and distal humerus. Further release of the capsule exposed the medial collateral ligaments (Fig. 3). Applying a varus stress allows the joint to dislocate and exposes the distal humerus and proximal ulna, radius (Fig. 4).
Fig. 1.
Postero-lateral skin incision.
Fig. 2.
Kocher's interval identified between extensor carpi ulnaris and anconeus muscle.
Fig. 3.
Common extensor origin, lateral collateral ligament, and periosteum dissected off of lateral supracondyler ridge.
Fig. 4.
Elbow joint dislocated by varus stress force.
After dislocating the elbow, synovectomy done and the distal humerus was prepared by excising osteophytes, removing all damaged and remaining articular cartilages and un-united bone fragments and fibrous debris, that should yield a smooth, rounded surface 4 or 5 cm wide and approximately 2 cm from anterior to posterior. On an average, only about 1–1.5 cm of the distal humerus was resected. Articular surfaces of the proximal radius and ulna were disturbed as little as possible and if these joints are irregular, they simply smoothened down with bur or bone rasp before reducing the elbow (Fig. 5).
Fig. 5.

Removal of damaged articular surface and osteophytes and subchondral bone exposed and smoothened.
After completing the preparatory stage of the elbow procedure, depending upon how large the Dermal graft is needed, a very thin split thickness skin graft was taken from donor site using hand held Humby's knife, the skin graft was taken in such a way so that its one side is still attached and was flipped over to expose the dermis which has the typical whitish appearance with minute punctate bleeding. The deep dermal layer was harvested with the help of hand held humby's knife. After securing haemostasis with electrocautery, the split-thickness skin graft is then replaced over the donor site and held in places with sutures/stapler and a bolster dressing done (Fig. 6, Fig. 9).
Fig. 6.
Dermal Graft harvested from lower abdomen.
Fig. 9.
Superficial split skin graft returned back to its previous place and su.
Trimming of the Dermal graft is done to remove residual epidermal portions which are sometimes present at the margins. Drilling of several small holes through the medial and lateral epicondylar ridges is done. The graft is then draped over the prepared distal end of humerus, applying the superficial cut surface of dermis to bone and graft is sutured with non absorbent Polyester (Ethibond™) suture. The deep surface of the Dermal graft which may containing some adipose tissue faces the new joint space (Fig. 7).
Fig. 7.
Graft applied and fixed with non-absorbable suture.
The elbow joint is then reduced again (Fig. 8), and the extensor muscles, lateral collateral ligament are re-sutured with Polygalactin (Vicryl™) suture, and wound closed in layers. A compression dressing is applied followed by above elbow POP (plaster of Paris) cast at 90° of flexion.
Fig. 8.
Elbow joint reduced back.
2.5. Post-operative rehabilitation protocol
Post operatively slab and dressing were not disturbed for 2 weeks till suture removal, only shoulder ROM, active finger exercises advised and for next 2 weeks only flexion and extension movements (protecting lateral and medial stress) advised on elbow ROM brace and after 1 month resistive flexion and extension exercise were started and after 6 weeks extensor strengthening exercises were added to it.
2.6. Follow-up protocols
Patients were called up for follow on 1 month, 3 month, 6 month, 9 month and 12 months and yearly. At each visit clinical evaluation including the range of motion, and MEPS were calculated and recorded.
2.7. Statistical analysis
To know the comparison of repeated measure of MEPS and ROM we have applied Wilcoxon signed rank test. The P < 0.05 is considered to be significant. The statistical analysis is done by SPSS software™ (IBM Corp).
3. Results
Age of the patients was between 16 years and 50 years with mean age of 34.33 years and follow-up duration was minimum 12 months and maximum 50 months with median of 22 months. In this study post-traumatic cause were most common as seen in 10 cases (55.6%) out of 18 elbows followed by inflammatory arthritis (RA) in 4 elbows (22.3%) and post-infection arthritis (tubercular) in 4 elbows (22.3%). Pre-operatively the ROM of the patients were from 0° to 75° with median value of 25° which was significantly improved post-operatively to from 55° to 135° with median value of 120° and found to be statistically significant with p-value of less than 0.01(Fig. 10).
Fig. 10.
Box-Whisker plot for Range of motion of the patients.
The pre-operative functional score MEPS of the patient were from 15 to 70 with median value of 45 which was improved post-operatively to from 85 to 100 with median value of 95 and found to statistically significant with p-value less than 0.01 (see Table 1) (Fig. 11).
Table 1.
Comparison of pre-operatuve and post-operative MEPS.
| MEPS | No. of patients | Median | Interquartile Range |
Min.-max. | p-value |
|---|---|---|---|---|---|
| Pre-op | 18 | 45 | 16.25 | 15–70 | <0.01 |
| Post-op | 18 | 95 | 1.25 | 85–100 |
Fig. 11.
Box- Whisker plot for MEPS of the patients.
The pain score as per MEPS of patients pre-operatively were from 0 (severe) to 45 (none) with median value of 15 which was improved post-operatively to pain score from 30 (mild) to 45 (none) with median value of 45 and found to be statistically significant with p-value less than 0.01. Out of 18 elbows in 14 (77.8%) cases excellent result and in 4 (22.2%) cases good result were observed.(see Table 2).
Table 2.
Final outcome.
| Outcome | MEPS score | Frequency | % |
|---|---|---|---|
| Excellent | 90–100 | 14 | 77.8 |
| Good | 75–89 | 4 | 22.2 |
| Fair | 60–74 | 0 | 0 |
| Poor | <60 | 0 | 0 |
It is found that out of 18 elbows in 5 patients (27.7%) mild instability found while in 3 patient (16.7%) hypertrophic scar over donor site was seen. No post-operative surgical site infection found out of 18 operated elbows (see Fig. 12, Fig. 13, Fig. 14, Fig. 15, Fig. 16, Fig. 17, Fig. 18).
Fig. 12.
Pre-op flexion.
Fig. 13.
Pre-op extension.
Fig. 14.
Pre-op x-rays AP and lateral view.
Fig. 15.
Post-op flexion.
Fig. 16.
Post-op extension.
Fig. 17.

Post-op x-ray AP view.
Fig. 18.
Post-op x-ray lateral view.
4. Discussion
Elbow joint is prone to stiffness due to various causes. Stiffness due to intrinsic cause like post-traumatic arthritis, inflammatory arthritis and post-infection arthritis are difficult to manage specially in young adults. Management of the elbow arthritis depends upon disease etiology, severity, age of the patient and functional demands. Total elbow replacement is considered the first choice in the treatment of severe elbow arthritis, but in young adult with high demand patients it is generally avoided due some serious limitations like restrictions of weight lifting of 5 kgs, longevity issue, aseptic loosening, infection etc. Interposition arthroplasty is a viable alternative option in such cases as other options like resection arthroplasty and arthrodesis are not well tolerated.4, 5, 6, 7
In this study post-traumatic cause were most common as in 10 cases (55.6%) out of 18 elbows followed by inflammatory arthritis (RA) in 4 elbows (22.3%) and post-infection arthritis (tubercular) in 4 elbows (22.3%). This correlates well with previous study done by Larson and Morrey6 in 2008, in their study of 45 elbows, 34 were due to post-traumatic and 11 were due to inflammatory arthritis and AI Froimson et al.13 in 1976 reported a study 5 patients where 3 patient (60%) were post-traumatic and 1 patient (20%) of RA and 1 patient (20%) of birth injury to the brachial plexus. But no previous studies had inclusion of post-tubercular cause, it may be due to those studies were conducted in developed countries where tuberculosis prevalence is very low.
In our study all the patients operated with interposition arthroplasty with lower abdominal dermal graft. The dermal graft was taken with the help of hand held Humby's knife. Post-operatively no distractor was applied and only POP slab was applied for 2 weeks and physiotherapy initiated thereafter.
We observed that the pre-operative functional score MEPS of the patients were ranged 15 to 70 with median value of 45 which is significantly increased inpost-operative to the score of 85–100 with median value of 95. Out 18 elbows excellent result seen in 14 (77.8%) elbows where good result seen in 4 (22.2%) elbows. All the patients in the study group are satisfied with the procedure. Out of 18 elbows 15 elbows became painless while other 3 has complaints of mild pain.
Significant improvement of the ROMs seen during post-operative time in all patients and attains functional arc of motion (100°, Morrey et al., 1981) except one patient which was a case of 13 year old post-traumatic bony ankylosis of elbow fixed in 90° flexion deformity where only 45° of range of motion could achieve. The pre-operative range of motion of the patients was 0°–75° with median value of 25° which is increased to 45°–135° with median value of 120.
Froimson et al.13 in 1976 reported results of cutis interposition arthroplasty in a series of 5 patient, all the patients in their study group have satisfactory restoration of elbow motion and returned to their previous occupation.
Uuspaa et al.14 in 1987 reported outcome of interposition arthroplasty using dermal graft in a series of 51 elbows of RA. In their study ROM was improved from pre-operative 20°–150°, mean 90°, to post-operative 40°–145°, mean 109°.
Recent published studies are done on the use of fascia lata and Achilles tendon graft as interposition material with the use of post-operative temporary distractor.
Cheng and Morrey15 in 1990 in their study of 13 patients of distraction interposition arthroplasty (DIA) using fascia lata reported that out of 13 patients, three patients whose primary diagnosis was inflammatory arthritis, two had excellent results with an improvement of the MEPS from 30 to 97 points (p = 0.03). The third patient with Reiter's syndrome continued to have pain in the elbow and subsequently had a successful TEA. Of the ten patients with post-traumatic arthritis, two had an excellent result, four good and three fair or poor. 3 patients required subsequent TEA.
Larson and Morrey6 in 2008 reported the largest series of 38 patients of interposition arthroplasty elbow using Achilles tendon graft with distractor. In their study the mean flexion-extension arc improved from 51° preoperatively to 97° postoperatively. The mean Mayo Elbow Performance Score improved from 41 pointspreoperatively to 65 points postoperatively. Thirteen patients had a good or excellent result, fourteen had a fair result, and eleven had a poor result. The remaining seven had a revision. On the basis of the Mayo Elbow Performance Score, twelve patients rated the elbow as somewhat better and nineteen rated the elbow as much better following the interposition procedure.
In literature no study has been mentioned about the functional outcome and the relationship with the duration it takes. In our study we found that the functional outcome MEPS takes a increasing pattern upto 6 months of post-operative period, which persists almost rest of the follow up period and we found that most of our patients returned to their previous work by that time. The range of motion of the patients also achieved their maximum outcome by 6 months in most of the patients which persists rest of the post-operative period.
Pre-operative instability of the elbow does effects the outcome of interposition arthroplasty. So excluded the patients with pre-operative instability, none of the patients included in our study had complaints of instability. Post-operatively it is found that mild instability present in 5 patients. But it does not hamper the performance of the patient. Patients are ready to accept mild instability for mobile and painless elbow.
No intra-operative complications we encountered in any of the case. Among the post-operative complication, mild instability found in 5 (27.7%) patients and in 3 (16.7%) patients hypertrophic scar over donor site. If the split thickness skin graft take over the donor site was poor, hypertrophic scars were observed after healing. Scar hypertrophy later managed with triamcenolone acetate injection intralesionally and compression bandage. The post-operative instability was also mentioned in previous published studies which is relevant with our study. No post-operative infection reported among our study group. No complications like bone resorption, seroma formation etc were seen. In the previous studies of cutis arthroplasty Froimson et al.13 (1976) reported no serious complications after the procedure. Distraction arthroplasty using fascia lata as graft, Cheng and Morrey15 (2000) reported eight complications in six of the patients. Two with pre-existing paraesthesia of the ulnar nerve with sensory deficit experienced slight worsening of their symptoms; one had fresh symptoms after the operation, which was treated successfully by subcutaneous transposition of the nerve. One patient had temporary paraesthesia in the distribution of the superficial radial nerve. Two complained of burning or cramping discomfort at the donor site for the fascia lata graft. One had an uncomfortable muscle herniation in the thigh which required repair later on. Using Achilles tendon as graft material Larson and Morrey6 (2008) reported seven patients out of 38 required revision surgery for the treatment of complications, which were primarily related to infection (two cases) or instability (three cases). Two elbows were converted to a total elbow arthroplasty at 3.8 years and at 2.0 years postoperatively for unknown reasons.
The main drawback of our study is the small sample size of the patients and short follow-up duration. These patients are in regular follow-up and it will be worthwhile to study the long term results of this procedure.
5. Conclusion
Stiff elbow still remains a challenge to the reconstructive orthopaedic surgeon. Many techniques have been tried to overcome this problem with very little success. We revisited Interposition arthroplasty with dermal graft as a viable option for stiff elbows. It provides good range of motion and better functional outcome in the patients of stiff and arthritic elbow. It is a good alternative to total elbow arthroplasty and viable option in young adults as it does not impose any activity restriction after surgery and no serious complication is seen like infection, failure, loosening, and longevity issue. Most of the patients returned to their previous occupation by 6 months after surgery.
It's a very cost effective treatment as compared to total elbow arthroplasty. It provides superior functional outcome than other kind of salvageable procedure like arthrodesis and patient's satisfaction is very high after surgery as pain subsided and range of motion improved. Moreover, it maintains good bone stock so further procedure if any required in future can be carried out.
Further study and critical analysis is needed with a larger sample size and a longer follow up.
Conflicts of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the preparation of this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2019.08.019.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Gallo R.A., Payatakes A., Sotereanos D.G. Surgical options for the arthritic elbow. J Hand Surg Am. 2008 May-Jun;33(5):746–759. doi: 10.1016/j.jhsa.2007.12.022. [DOI] [PubMed] [Google Scholar]
- 2.Soojian Michael G., Kwon Young W. Elbow arthritis. Bull Hosp Joint Dis. 2007;65(1):61–71. [PubMed] [Google Scholar]
- 3.Sears B.W., Morrey M.E., Sanchez-Sotelo J., Morrey B.F. Posttraumatic elbow arthritis in the young adult: evaluation and management. J Am Acad Orthop Surg. 2012;20:704–714. doi: 10.5435/JAAOS-20-11-704. [DOI] [PubMed] [Google Scholar]
- 4.Gill D.R.J., Morrey B.F. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis: a ten to fifteen year follow up study. J Bone Joint Surg [Am] 1998;80-A:1327–1335. doi: 10.2106/00004623-199809000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Morrey B.F., Adams R., Bryan R.S. Total replacement for posttraumatic arthritis of the elbow. J Bone Joint Surg [Br] 1991;73-B:607–612. doi: 10.1302/0301-620X.73B4.2071644. [DOI] [PubMed] [Google Scholar]
- 6.Noelle Larson A., Morrey Bernard F. Interposition arthroplasty with an Achilles tendon allograft as a salvage procedure for the elbow. J Bone Joint Surg Am. 2008;90:2714–2723. doi: 10.2106/JBJS.G.00768. [DOI] [PubMed] [Google Scholar]
- 7.Celli Andrea, Morrey Bernard F. Total elbow arthroplasty in patients forty years of age or less. J Bone Joint Surg Am. 2009 Jun 01;91(6):1414–1418. doi: 10.2106/JBJS.G.00329. [DOI] [PubMed] [Google Scholar]
- 9.Froimson A.I., Morrey B.F. Interposition arthroplasty of the elbow. In: Morrey B.F., editor. Master Techniques in Orthopaedic Surgery: The Elbow. Lippincott Williams and Wilkins; Philadelphia: 2002. pp. 391–408. [Google Scholar]
- 10.Defontaine L. Osteotomietrochleiforme: Nouvelle methode pour la cure des ankylosisosseaus du coude. Rev Chir. 1887;7:716–726. [Google Scholar]
- 11.Blaine T.A., Adams R., Morrey B.F. Total elbow arthroplasty after interpositional arthroplasty for elbow arthritis. J Bone Joint Surg Am. 2005 Feb;87(2):286–292. doi: 10.2106/JBJS.03031pp. [DOI] [PubMed] [Google Scholar]
- 13.Froimson A.I., Silva J.E., Richey D. Cutis arthroplasty of the elbow. J Bone Jt. Surg. 1976;58A(863) [PubMed] [Google Scholar]
- 14.Uuspaa V. Anatomical interposition arthroplasty with dermal graft: a study of 51 elbow arthroplasties on 48 rheumatoid patients. Z Rheumatol. 1987;46(132) [PubMed] [Google Scholar]
- 15.Cheng S.L., Morrey B.F. Treatment of the mobile, painful arthritic elbow by distraction interposition arthroplasty. J. Bone Joint Surg. Br. 2000;82B:233. [PubMed] [Google Scholar]
- 16.Gill D.R., Morrey B.F. The coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. A ten to fifteen-year follow-up study. J Bone Joint Surg Am. 1998;80:1327–1335. doi: 10.2106/00004623-199809000-00012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.