Abstract
Introduction
Sternoclavicular joint tuberculosis is rare with non-specific signs and symptoms thus making correct clinical diagnosis difficult. Delay in diagnosis results in destruction of osteo-ligamentous structures, spread of abscess to deeper planes as well as bursting through skin resulting in joint instability and scar formation.
Material and methods
All the cases of sternoclavicular joint tuberculosis presented to the orthopaedic outdoor between 2004 and 2017 were evaluated clinico-radiologically along with cyto-histopathological and/or microbiological tests to ascertain the diagnosis before initiation of treatment.
Results
There were 11 males and 5 females patients aged 11–65 years (mean, 35 years). Aspiration or curettage of the swelling was performed, and the diagnosis was confirmed in 12 cases by cytology, AFB stain, TB polymerase chain reaction, culture or a combination of these. In 4 patients, anti-tubercular treatment was initiated on clinical suspicion.
Conclusion
Diagnosing sternoclavicular tuberculosis requires multimodal approach. A strong clinical suspicion is required as the presentation is often atypical. Early detection of disease and with conservative treatment resulted in complete remission and minimal long term disability.
Keywords: Sternoclavicular joint, Tuberculosis, TB, Conservative, Treatment, Diagnosis
1. Introduction
Sternoclavicular joint (SCJ) is a true diarthrodial synovial articulation between the upper limb and the axial skeleton. Sternoclavicular joint is infected by pyogenic organisms more often than by the tubercular bacillus. Skeletal tuberculosis comprises 10% of extra-pulmonary cases.1 Tuberculosis of SCJ (SCJ TB) is extremely rare and accounts for 1–2% of tubercular arthritis.2 There is limited information on SCJ TB even in developing countries and is largely based on case reports and a few clinical studies.
SCJ TB is mostly misdiagnosed leading to chronic disability, increased morbidity and delay in proper treatment. The most common clinical presentation of SCJ TB is swelling, pain in the area of the SCJ with mild fever.3 The localization of the symptoms to the joint is usually clinically obvious, but due to the lack of knowledge about the differential diagnosis, nonspecific symptoms, difficulty in interpreting early stage radiographs; the diagnosis of SCJ TB is usually delayed or, at times, even missed. The extensive osteo-cartilaginous destruction caused at the SCJ can result in joint instability. The surgical treatment of SCJ TB is associated with poor results and the potentially catastrophic complications due to the proximity of great vessels, phrenic nerve, and superior mediastinal structures to the joint.4 The worldwide resurgence of extrapulmonary tuberculosis has made this a topic of interest for orthopaedic surgeons from developing and developed nations. In this retrospective study, we sought to determine the clinico-radiological findings and role of nonoperative management in patients with SCJ tuberculosis.
2. Material and methods
From January 2004 to December 2017, we have treated 16 patients with tubercular arthritis of SCJ (Fig. 1, Fig. 2, Fig. 3, Fig. 4). There were 11 male and 5 female patients aged 11–65 years (mean, 35 years) who presented with tuberculosis of the right (n = 11) or left (n = 3) and two cases with bilateral SCJ were reviewed.
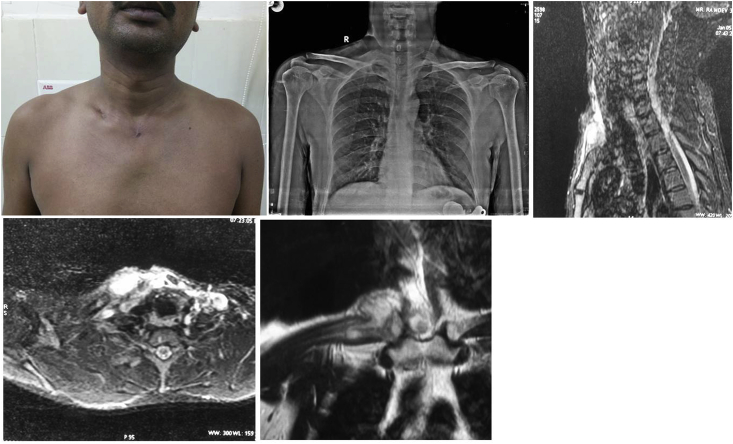
Fig. 1.
A: Clinical picture showing healed scar. 1B: Chest radiograph with lucency in medial end of clavicle on right side. 1C: Axial section of MRI showing abscess. 1D: Sagittal section of MRI showing collection at medial end of clavicle. 1E: Coronal MRI section showing abscess.
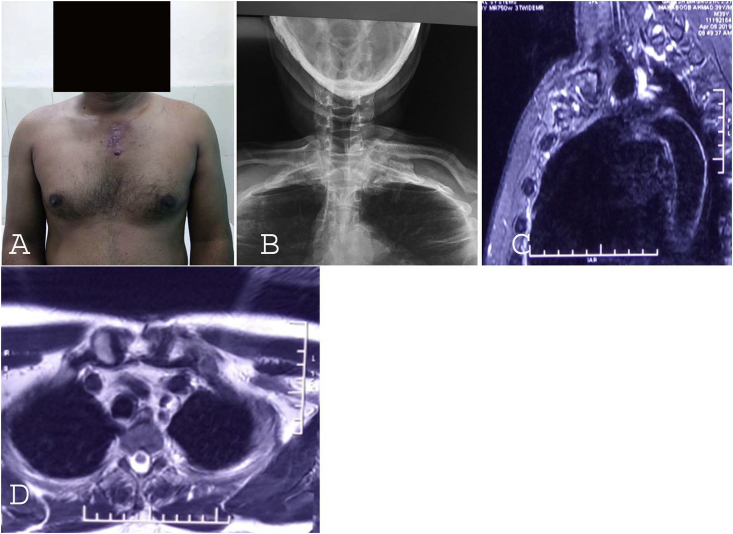
Fig. 2.
A: Clinical picture showing healed scar. 2B: Chest radiograph with destruction of left sternoclavicular joint. 2C&2D: Sagittal and axial section of MRI showing joint destruction.
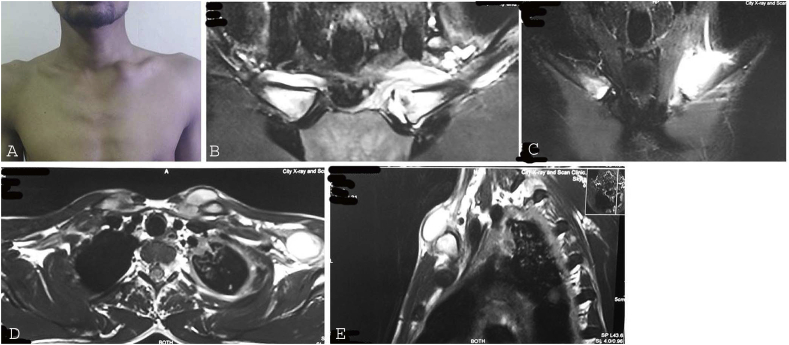
Fig. 3.
A: Clinical picture showing swelling at left sternoclavicular joint. 3B & 3C: Coronal section of MRI showing collection on left side. 3D & 3E: Axial and Sagittal sections of MRI showing abscess.
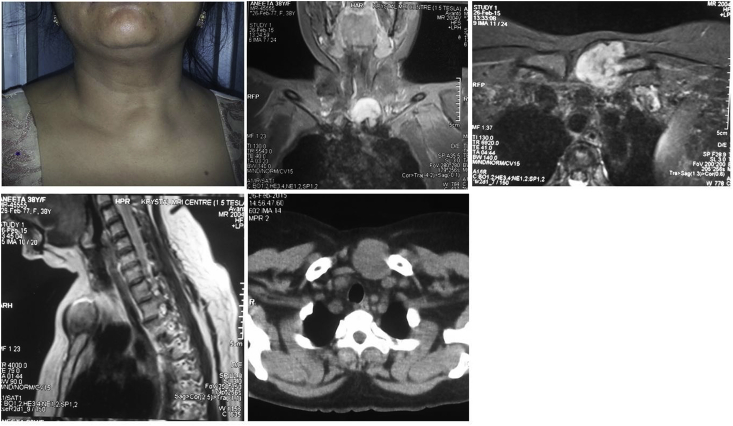
Fig. 4.
A: Clinical picture showing swelling at left sternoclavicular joint. 3B: Coronal section of MRI showing collection on left side. 3C: Axial section of MRI. 3D: Sagittal MRI section showing abscess. 4E: NCCT axial section showing affected side with soft tissue component.
Patients included in this series had histopathological and/or aspiration cytology and/or microbiological findings suggestive of tuberculosis and those suspected to have TB with improvement on anti-tubercular treatment (ATT) despite negative pathology and/or microbiology results. Radiological studies included chest radiograph and magnetic resonance imaging (MRI). Computed tomography (CT) scan was performed in some cases in which the MRI was inconclusive. Contrast material was not used in any of the patients. Chest x-ray was evaluated for the site of involvement, rarefaction, lytic changes, bony destruction and changes in the joint space and joint margins. Ultrasonography (USG) was also done in few cases to see the collection and for subsequent guided aspiration. Magnetic resonance imaging (MRI) was evaluated for site involved, marrow changes, bony destruction, joint effusion and soft tissue changes. Bone scan was done in one patient with multifocal disease. Aspiration was done in all cases, either blindly or under USG guidedence and samples were sent for gram stain, Zeihl-Neelsen (ZN) stain, culture, TB polymerase chain reaction (TB-PCR) and cytological evaluation. Samples were sent for histopathological evaluation in the case where debridement was done. Antitubercular treatment (ATT) was started and continued till 12 months wherever possible. MRI was again done at 12 months, which if did not show complete resolution, the ATT was continued for longer duration with maximum of up to 18 months.
3. Results
Local symptoms included pain (n = 16) swelling (n = 14) and discharging sinus (n = 1). The mean duration of symptoms was 14 (range, 3–36) weeks. Nine patients presented with systemic symptoms including malaise, fever, or loss of weight/appetite. Six patients had multifocal involvement of the lung (n = 4), and lymph node (n = 2), with pleural effusion (n = 3). All 16 patients had a raised erythrocyte sedimentation rate (ESR) or C-reactive protein(CRP) at presentation. Fifteen patients were evaluated by MRI. Aspiration (in all cases), curettage (in 1 out of 16 cases) of the swelling was performed, and the diagnosis was confirmed by cytology, AFB stain, TB-PCR or culture. In one case, where debridement was done, histopathology was suggestive of tuberculosis. To aggregate, 4 cases were diagnosed with a combination of cytological and microbiological findings, 6 with microbiological findings only (AFB, culture or TB-PCR) and 2 with cytological findings only. In 4 cases, diagnosis was based on clinical suspicion even when the diagnostic tests were negative. All patients received a standard regimen of ATT. In one patient, SCJ was surgically debrided as it was not responding to conservative management after 4 months of ATT. Post operatively ATT also was given in this patient. In all the cases, the total duration of ATT was 4–18 months and at final follow-up all lesions healed. Observations have been compiled in Table 1.
Table 1.
Compilation of all the cases of tuberculosis of sternoclavicular joint.
| Cases | Age sex | Site | Clinical features | Duration of symptoms | Radiology | Histology/cytology/ESR/CRP | AFB | Culture | TB-PCR | Treatment | Follow-up | Associated TB | Remark |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 21/M | B/L | Painful swelling, wt loss, loss of appetite | 6 months | MRI- bilateral lytic area with bone marrow edema with collection Lt SCJ; Chest xray- left pleural effusion; Bone scan- multifocal disease |
USG guided aspiration showed pus ESR-30 |
+ | + | NA | ATT for 8 months | 8 months, symptoms improved and then lost to follow-up | Lung, Spine D5 and D7, Left sided pleural effusion |
Multifocal TB |
| 2 | 38/F | Lt | Painful swelling, fever | 9 months | MRI- bone marrow edema and cortical erosion with collection; USG- collection in Lt SCJ |
Cytology -Chronic Granulomatous pathology; Histopath- Chronic Granulomatous patholgy; Mantoux- ESR 28 |
+ | – | NA | ATT for 4 months, surgical debridement and ATT continued for 4 months | 8 months, symptom free | None | Misdiagnosed as strain of SCJ and treated conservatively |
| 3 | 64/F | Rt | Pain | 4 months | MRI- bone marrow edema Rt SCJ | ESR-25 | – | NA | – | ATT for 12 months | 1 year | None | Initially diagnosed as SCJ osteoarthritis |
| 4 | 29/M | Rt | Painful swelling | 4 months | MRI- erosion of articular margin with synovial thickening and collections with mild subluxation and widening of space | USG guided aspiration; ESR-23 |
– | – | + | ATT for 18 months | 2 years | TB lymphadenitis for 5 months ATT | Conservative treatment from quack |
| 5 | 56/F | Rt | Painful swelling | 5 months | MRI- marrow edema with periarticular collection | USG guided FNA- granulomatous pathology; ESR-40 |
NA | – | + | ATT for 12 months | 16 months | None | Initially diagnosed as SCJ osteoarthritis |
| 6 | 30/M | Rt | Painful swelling; history of indirect trauma |
5 months | MRI- marrow edema in medial aspect of clavicle with collection in Lt SCJ | Aspiration-granulomatous pathology; ESR-34 |
– | – | NA | ATT for 12 months | 2 year, then lost to follow-up | None | Traumatic SCJ |
| 7 | 40/M | Rt | Pain, weight loss, cough, fever | 2 months | Discovered incidentally on chest CT | Cytology -chronic granulomatous pathology; ESR-22 |
NA | + | NA | ATT for 6 months | 6 months | chest TB, pleural effusion, TB lymphadenitis | Multifocal |
| 8 | 27/F | Rt | Painful swelling | 3 months | MRI- marrow edema with periarticular collection | ESR-31 | + | + | NA | ATT for 12 months | 13 years | None | With pregnancy |
| 9 | 42/F | B/L | Painful swelling | 6 months | MRI- bone marrow edema and cortical erosion with collection | Cytology -chronic granulomatous pathology; ESR-29 |
NA | NA | + | ATT for 12 months | 2.5 years | None | Recurrent Rheumatoid arthritis |
| 10 | 11/M | Lt | Painful swelling | 2 months | MRI- marrow edema in medial aspect of clavicle with collection in left SCJ | ESR-17; CRP-9 |
NA | NA | + | ATT for 6 months | 6 months | Pleural effusion | |
| 11 | 65/M | Rt | Painful swelling | 3 weeks | CT chest - erosion over both SCJ | Cytology -chronic granulomatous pathology; ESR-37 |
– | – | NA | ATT for 4 months | Lost to follow-up after 4 months | Known c/o CKD | |
| 12 | 30/M | Lt | Painful swelling, discharging sinus | 2 months | MRI- erosion in left SCJ with collection; CT scan- showed destruction involving Lt SCJ |
ESR-70; CRP-49 Montoux - |
– | NA | – | ATT for 5 months | 5 months | Cough and on and off fever with history of weight loss | |
| 13 | 38/M | Rt | Painful swelling | 1 month | MRI- signal intensity changes over medial aspect of clavicle with erosions and small collections | Aspiration; ESR-17 CRP>10. |
NA | + | + | ATT for 12 months | 19 months | None | |
| 14 | 19/M | Rt | Painful swelling | 1 month | MRI- collection in SCJ with bone marrow edema | ESR-41; CRP-20 |
NA | – | + | ATT for 12 months | 18 months | None | |
| 15 | 20/M | Rt | Painful swelling | 2 months | MRI- bilateral SCJ marrow edema With Rt effusion |
ESR-32 | – | – | – | ATT for 9 months | 9 months | None | |
| 16 | 30/M | Rt | Painful swelling | 6 weeks | MRI- collection in SCJ with bone marrow edema | ESR-29 | – | – | – | ATT for 12 months | 12 months | None |
Abbreviations: M-Male, F-Female, Rt- Right side, Lt- Left side, NA- Not available, ATT- Anti-tubercular therapy, CKD- Chronic kidney disease, SCJ- Sternoclavicular joint, ‘+’ is positive, ‘-’ is negative.
4. Discussion
SCJ is a plane synovial joint between medial end of clavicle and manubrium sterni. It is the only joint through which the upper limb is attached to the axial skeleton. It has no isolated movements but it moves secondary to movements of scapula and glenohumeral joint. The SCJ is vulnerable to the same pathological conditions as other synovial joints; the most common of these are subluxation or dislocation due to injury, age related osteoarthritis, infections and inflammatory arthritis. Osteoarthritis is the most common cause of pain in SCJ. Septic arthritis of the sternoclavicular joint is infrequent in healthy adults, accounts for less than 0.5% of bone and joint infections. Staphylococcus aureus accounts for 49% cases, pseudomonas aeruginosa for 10% and mycobacterium tuberculosis for 3%. Pseudomonas infection most frequently affects immunocompromised hosts. SCJ TB accounts for 1–2% of all the peripheral tubercular arthritis.2 SCJ TB is insidious in onset; therefore, a high degree of suspicion is necessary to make the diagnosis. We have extensively searched the literature for all the reported cases from search engines such as Google, PubMed using the terms, “tuberculosis AND sternoclavicular”. References from these results were also screened and found 29 publications in various journals, published from 1982 to 2019. Twenty six papers were in English, 2, 3, 4, 5, 6, 7, 8, 10, 11, 12, 13, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 one in French9 and two in Japanese 14, 16 (Table 2). About half of these reports were from India, which is an endemic region for tuberculosis. These case series were much larger than any other parts of the world. A total number of 86 patients were reported in which more than half of the patients were males. All, but the two cases had unilateral involvement of the joint. There was no specific predilection for a particular age group. On review, the chief presenting complaints were swelling, pain, fever, discharging sinuses or a combination of these. Swelling was the most common complaint with 25 patients presenting with swelling over the SCJ. Clinically, patients with SCJ TB presented with cystic and globular swelling. Because of a subcutaneous position of SCJ; the swelling of the joint was apparent at an early stage of the disease. The swelling was not just localized to SCJ but was diffuse in many patients. Pain was the second most common complaint. Pain was not significant in early stages of the disease. On examination, the joint is usually minimally tender in early stages with non-pulsatile swelling without raised temperature of the skin. Fever was present in 7 cases which was much less than the expected. Discharging sinuses were an uncommon symptom with only two cases presented with it.
Table 2.
Cases of sternoclavicular joint tuberculosis reported in world literature.
| Author,Year, Language, number of SCJ TB patients | Presentation | Radiology | Biopsy/FNAC | TB-PCR | Treatment | Follow-up | Outcome | Comment/Co-morbidities |
|---|---|---|---|---|---|---|---|---|
| Simon GL, Worthington MG5 1982 English 1 patient |
46/M Soft tissue mass adherent to the medial aspect of the left clavicle for 3 months |
Xray- defect at the medial end of the left clavicle; CT- defect involving the medial clavicle and SCJ with diffuse sclerosis of the adjoining bone |
Necrotic material with caseating granuloma; AFB+; culture + | NA | Isoniazid and Ethambutol | Lost to follow-up | Not known | Past history of alcoholic hepatitis, TB epididymitis |
| Martini M6 (out of 74 cases of TB, one was SCJ TB) 1986 English 1 patient |
Lt SCJ involvement | NA | NA | NA | NA | NA | NA | NA |
| Bezza et al.2 1998 English 2 patients |
38/M Swelling |
Erosion on CT | Histopathology + | NA | 6 months ATT | 8 months | Favourable | |
| 46/F Swelling |
Erosion on CT | Histopathology + | NA | 9 months ATT | 6 months | Favourable | ||
| Yasuda et al.7 1995 English 3 patients |
71/M Painless swelling Rt SCJ for 9 months |
Xray- lytic lesion clavicle; CT and MRI- soft tissue mass; Gallium scan-abnormal isotope accumulation |
Open biopsy showed MTB | 2 year | Pulmonary TB | |||
| 54/M Painless swelling Rt SCJ for 9 months |
Xray- erosion clavicle and first rib; Arthogram- communication between lung and SCJ |
ATT with debridement with excision of Clavicle, rib, sterum | 3 years | Pulmonary TB | ||||
| Painless swelling Lt SCJ with discharging sinus, decreased shoulder movement | Xray- partial destruction clavicle and sternum; CT- soft tissue swelling and erosion clavicle; Tc99- abnormal uptake Fistulogram- track to SCJ |
Fistula excision; clavicle resection and medical debridement |
2 year | Pulmonary TB | ||||
| Fang et al.8 1997 English 1 patient |
34/F painless mass Lt SCJ 3 months | Xray chest- resorption of proximal clavicle; CT- heterogeneous enhanced tumor with erosion of clavicle and sternum; Bone scan- a focal area of increased uptake |
Biopsy- caseating grauloma | – | Total resection of mass with ATT |
NA | NA | On hemodialysis, anaemic |
| Shah J3 2000 English 8 patients |
36/F Lt SCJ Swelling, fever |
Xray- Normal; MRI- destruction with signal intensity in clavicle and soft tissue mass |
Biopsy confirmed TB | NA | NA | NA | NA | |
| 28/F Rt SCJ Painless swelling, fever |
Xray- articular erosion clavicle; MRI- destruction with signal intensity in clavicle and soft tissue mass |
Sputum for AFB +; Biopsy + | NA | NA | NA | NA | Pulmonary TB | |
| 78/M Rt SCJ Painful swelling, fever |
Xray- articular erosion clavicle; MRI and CT- destruction with signal intensity over clavicle and soft tissue mass |
Culture for MTB +; Biopsy + | NA | NA | NA | NA | Diabetic hypertensive | |
| 60/M Lt SCJ Painful swelling, fever |
Xray- articular destruction of clavicle; MRI- signal intensity of clavicle and sternum, soft tissue mass |
sputum AFB+; Culture for MTB +; Biopsy + |
NA | NA | NA | NA | Diabetic; H/O Pulmonary TB | |
| 62/M Lt SCJ Painless swelling, fever |
Xray- normal CT- soft tissue mass extension |
Histopathology + | NA | NA | NA | NA | Cirrhosis of liver, TB of wrist and L2 vertebra | |
| 66/M Lt SCJ Painless swelling, fever, |
CT- SCJ, clavicular destruction, normal sternum, large extrapleural abscess |
Culture for MTB +; Biopsy + | NA | NA | NA | NA | ||
| 53/M Rt SCJ Painful swelling, fever |
Xray- normal; CT- Rt SCJ, clavicular, manubrium and body of sternum (ant. and post. cortex) destruction, soft tissue mass extension |
Culture for MTB +; Biopsy + | NA | NA | NA | NA | Gall bladder calculi; HIV+; Pulmonary and mediastinal TB | |
| 58/F Rt SCJ Painful swelling |
CT- Rt SCJ shows increased joint space, minimal sternal destruction, soft tissue mass extension | Culture for MTB +; Biopsy + | NA | NA | NA | NA | ||
| Sy et al.9 2000 French 1 patient |
Painless swelling, 4 months | Xray- Increased joint space with lytic lesion of sternum | Aspiration- AFB+ | 9 month healing, died after 2 month (unrelated cause) | HIV + | |||
| Dhillon et al.10 2000 English 1 patient |
28/M Painful either side, 3 months | Xray- normal; CT- destruction of sternum, clavicle and first rib | Rt side open biopsy- grauloma | NA | 16 months ATT | NA | Healed | |
| Fukasawa et al.11 2001 English 1 patient |
Lt SCJ Painless mass, 10 months |
CT- heterogenously enhanced mass lesion, which expanded over the Lt SCJ and the surrounding soft tissues |
FNAC -granulomatous; Culture + |
1 year; symptoms improved | Malignancy or metastatic tumor; diabetes mellitus; hemodialysis; no response to antibiotics | |||
| Dhillon et al.12 2001 English 8 cases |
28/M Bilateral pain and swelling |
Xray- normal | FNAC/Biopsy- granulomatous pathology | NA | 18months ATT | 48 months | Healed | |
| 18/M Lt Pain and swelling for 9 months |
Xray- cystic lesion | FNAC/Biopsy- granulomatous pathology | NA | 16 months ATT | 90 months | Healed | ||
| 41/M Rt, Painful swelling with constitutional symptoms for 11 months |
Xray- normal | FNAC/Biopsy- granulomatous pathology | NA | 15 months ATT | 78 months | Healed | ||
| 29/F Rt Discharging sinus, 10 months |
Xray- normal | FNAC/Biopsy- granulomatous pathology | NA | 16 months ATT | 72 months | Healed | ||
| 39/M 32 month, Rt Pain and swelling |
Xray- normal | FNAC/Biopsy- granulomatous pathology | NA | 16 months ATT | 50 months | Healed | ||
| 50/F 8 month, Lt Swelling |
Xray- normal | FNAC/Biopsy- granulomatous pathology | NA | 14 months ATT | 35 months | Healed | ||
| 37/M 12 month, Lt Pain and swelling |
Xray- normal | FNAC/Biopsy- granulomatous pathology | NA | 15 months ATT | 28 months | Healed | ||
| 22/M 14 month, Rt Swelling |
Xray- normal | FNAC/Biopsy- granulomatous pathology | NA | 16 months ATT | 64 months | Healed | ||
| 34/M 12 month, Rt Pain and swelling |
Xray- normal | FNAC/Biopsy- granulomatous pathology | NA | 16 months ATT | 18 months | Healed | ||
| Khan et al.13 2003 English 1 patient |
13/F Lt SCJ pain and swelling for 11 months |
Xray- well defined lytic area in medial end of clavicle | FNAC- granuloma; AFB+; Culture+ | NA | 12 months ATT | 18 months | Healed | |
| Kawasaki et al.14 2007 Japanese 1 patient |
70/F Rt SCJ swelling |
CT- destruction of Rt SCJ | Biopsy+ | + | ATT and debridement when not healed at 3 months | NA | Healed | Past history of pulmonary TB |
| Sahu S15 2008 English 1 patient |
38/M Pain and swelling for 2 months |
Xray- moth-eaten appearance on medial end of clavicle, mild sclerosis of articular surface of manubrium; CT scan- lytic lesion involving Lt SCJ | FNAC- tubercular abscess | NA | 12 months ATT | NA | Healed | |
| Amano et al.16 2009 Japanese 1 patient |
79/M Lt precordial swelling |
CT- destruction of Lt SCJ | Needle biopsy- AFB seen | NA | ATT | NA | Improved | Renal failure due to rifampicin |
| Aggarwal et al.17 2009 English 1 patient |
22/M Rt Painful, swelling 4 month |
Xray- lytic lesion on Rt medial clavicle CT scan- erosion and fragmentation of medial clavicle |
FNAC- tubercular abscess | NA | 12 months ATT | 12 months | Healed | TB of wrist and bilateral sacroiliac joint. |
| Pandita et al.18 2010 English 1 patient |
62/F Swelling of both SCJ |
CT- fluid collections with erosion both ends | FNAC granuloma | NA | 12 months ATT | NA | Healed | Pleural effusion. |
| Shrivastav et al.19 2010 English 1 patient |
12/M Swelling Lt SCJ for 2 months |
Normal radiograph | FNAC- tubercular abscess; Culture- negative |
NA | NA | NA | Healed | |
| Grover et al.20 2011 English 2 patients |
53/M Pain and swelling Rt SCJ for 6 months |
Xray- osteolytic lesion; CT scan- expansion of clavicle with multiple erosions |
Curettage- granulomas | NA | NA | NA | NA | Pulmonary TB |
| 23/F Pain and swelling Lt SCJ for 2 months |
Xray- Lt SCJ dense sclerosis; CT -erosions of its articular surface with dense sclerosis |
CT guided aspiration-granulomas |
NA | NA | NA | NA | Sputum for AFB+; Pulmonary TB |
|
| Khare et al.21 2011 English 1 patient |
32/M Pain and swelling Lt SCJ |
Chest Xray- lytic lesion with sclerosis over medial aspect of clavicle | AFB + | NA | 12 months ATT | NA | Healed | |
| Kelderman et al.22 2012 English 1 patient |
24/F Swelling on medial aspect of Rt clavicle |
Normal radiograph | NA | + | ATT | NA | Healed | |
| Metanat M, Alavi-Naeini R23 2012 English 1 patient |
63Y/F Pain and swelling Lt SCJ for 7 months |
Xray- destruction of SCJ | FNAC- tubercular abscess; Culture- negative |
NA | ATT | NA | Healed | |
| Koshy S24 2014 English 1 patient |
28/F Pain Rt SCJ 10 months with multiple sinuses |
MRI - periosteal inflammatory condition | Culture + Resistance for INH |
NA | ATT | NA | At fifth month of ATT her sinuses reduced from 7 to 1 | Initially treated as bacterial infection |
| Saibaba et al.25 2014 English 1 patient |
24/F Painful swelling Rt SCJ of 2 months |
Xray- destruction and sclerosis of medial end of Rt clavicle | FNAC - caseating granuloma; AFB + | NA | 18 months ATT | 2 years | Healed | Pulmonary TB and spine TB |
| Walid et al.26 2015 English 1 patient |
63/M Swelling over Rt SCJ for 3 months |
Normal radiograph; CT-heterogeneously enhanced mass over Rt SCJ with widening of joint space and subchondral sclerosis of sternum | Histopathology+; Culture- |
NA | 12 months ATT | 4 years | Healed | |
| Jain et al.27 2015 English 13 patients |
29/F Swelling for 2 months |
Xray- normal | Histopathology +; Culture - |
+ | 12 months ATT | 17 months | Healed | 4 out of 13 patients had other site involvement(not specified which ones) |
| 34/F Painful swelling for 1 month |
Xray- normal | Histopathology +; Culture - |
– | 12 months ATT | 13 months | Healed | ||
| 44/M Discharging sinus for 3 months |
Xray- lytic lesion at clavicle | Histopathology -; Culture - |
+ | 18 months ATT | 21 months | Healed | Required immunomodulation; CD4:CD8 ratio-low | |
| 47/M Swelling for 7 months |
Xray- normal | Histopathology +; Culture - |
– | 12 months ATT | 12 month | Healed | ||
| 29/M Painful swelling for 4 months |
Xray- normal | Histopathology +; Culture - |
– | 12 months ATT | 14 months | Healed | ||
| 37/M Discharging sinus for 3 months |
Xray- normal | Histopathology -; Culture - |
– | 12 months ATT | 14 months | Healed | ||
| 41/M Swelling for 1 month |
Xray- normal | Histopathology +; Culture + |
– | 12 months ATT | 19 months | Healed | ||
| 33/F Painful swelling for 2 month |
Xray- normal | Histopathology -; Culture - |
– | 12 months ATT | 23 months | Healed | ||
| 39/M Swelling for 2 months |
Xray- normal | Histopathology -; Culture - |
+ | 12 months ATT | 18 months | Healed | ||
| 26/F Discharging sinus |
Xray- normal | Histopathology +; Culture - |
– | 18 months ATT | 22 months | Healed | Required immunomodulation; CD4:CD8 ratio-low | |
| 38/M Painful swelling for 2 months |
Xray- normal | Histopathology +; Culture - |
– | 12 months ATT | 16 months | Healed | ||
| 42/M Swelling for 1 month |
Xray- normal | Histopathology -; Culture - |
+ | 12 months ATT | 15 months | Healed | ||
| 36/M Discharging sinus for 3 months |
Xray- normal | Histopathology -; Culture - |
+ | 12 months ATT | 17 months | Healed | ||
| Akhtar et al.28 2015 English 1 patient |
41/F Painful swelling Rt SCJ |
Xray- normal; CT scan- sclerotic lesion on medial end of clavicle |
FNAC- inconclusive; Culture-; AFB- |
NA | 9 months ATT | 2 year | Healed | |
| Meena et al.29 2017 English 9 patient |
53/M Painful swelling Rt SCJ for 5 months |
Xray was normal in all except one who had doubtful cystic lesion at medial end clavicle and another had active disease in lung and spine | Biopsy- caseating granuloma | + | 16 months ATT | NA | Healed | 1 out of 9 patients had pulmonary and spine involvement |
| 24/M Painful swelling Rt SCJ for 2 months |
AFB + | + | 14 months ATT | NA | Healed | HIV+ | ||
| 51/M Discharging sinus Lt SCJ for 4 months |
AFB + | NA | 18 months ATT with immunomodulation for HIV | NA | Healed | |||
| 32/M Painful swelling for 7 months |
Biopsy- caseating granuloma | + | Second line ATT for 18 months with immunomodulation for HIV | NA | Healed | HIV+ | ||
| 58/F Painless swelling for 13 months |
Biopsy- caseating granuloma | NA | 18 months ATT | NA | Healed | Rheumatoid arthritis | ||
| 45/M Painful swelling for 6 months |
Biopsy- caseating granuloma | NA | 16 months ATT | NA | Healed | |||
| 65/M Discharging sinus for 6 months |
Biopsy- caseating granuloma | NA | 12 months ATT | NA | Healed | |||
| 33/F Painful swelling for 8 months |
Biopsy- caseating granuloma | + | 15 months ATT | NA | Healed | |||
| 54/M Painful swelling for 5 months |
AFB + | NA | 18 months ATT | NA | Healed | |||
| Jha et al.30 2018 English 3 cases |
49/M Swelling in Lt SCJ and fever |
CECT thorax- inflammatory lesion involving left SCJ with extension to mediastinum | NA | NA | 9 months ATT | NA | Healed | |
| 45/F Swelling in Rt SCJ and fever |
CECT thorax- cold abscess of Rt SCJ |
FNAC- grauloma; AFB+ | NA | 9 months ATT | NA | Healed | ||
| 36/F Swelling in Rt SCJ and fever |
CECT thorax- necrotic soft tissue swelling of Lt SCJ |
NA | NA | ATT | NA | NA | Pott’s spine at D6- D8 | |
| Prakash et al. 2019 English 19 cases |
14 of 19 were females. Pain in all patients |
Xray- varied appearances including diffused thickening and honeycombing, eccentric expansile lytic lesions with osteopenia, or sequestration at medial end of clavicle not unlike pyogenic infection. MRI- signal intensity changes, distended joint, granulation/abscess in the soft tissue. Few areas of cortical destruction |
Biopsy - caseating grauloma (all patients) | + in 16 out of 19 patients | 18 months ATT Curettage and debridement in 3 patients |
NA | Healed | 7 of 19 had past h/o pulmonary tuberculosis |
Abbreviations: ATT- Anti-tubercular therapy; AFB- Acid fast bacilli; CT-computed tomography; FNAC- Fine needle aspiration cytology; F- female; Lt- Left; M-male; MRI - magnetic resonance imaging; MTB- Mycobacterium tuberculosis; NA-not available; Rt- Right; SCJ-sternoclavicular joint; TB-PCR- Tuberculosis polymerase chain reaction; - denotes negative; + denotes positive.
In the present study also, it was observed that pain and swelling are the most common symptoms. Only one of our patients had swelling without pain and two patients had pain without any obvious swelling. Shah et al.3 reported 8 cases of SCJ TB, in which they noticed pain, swelling and fever to be the most common symptom combination (6 out of 8). Dhillon et al.,12 in their study of 9 cases, also reported pain and swelling as common symptoms. Jain et al.,27 reported fever and swelling as the most common constellation. The review of literature showed; the concomitant TB in other organs, commonly of the lung, was present in 15 patients. These cases may mimic metastatic bone disease in some patients leading to a diagnostic dilemma. 32 Past history of TB was present in 8 cases. HIV was found in 4 patients. Other foci of TB were noticed in four of our patients. (Table 2) Shows the observations made by various authors on SCJ TB.
Radiological investigations mentioned in literature were plain radiographs, CT scans, MRI, Tc99 scan, arthrogram and fistulogram. On compilation of review finding, 45% patients in previous studies had findings in a plain radiograph which ranged from localized osteopenia to the gross destruction of medial end of clavicle and sternum, although most authors are of the opinion that plain radiographs are not helpful unless there is marked destruction or subluxation of the joint, which also, could be missed because of the confluence of many structures. CT scan is better than plain radiographs for identifying bony lesions around the sternum as it precisely picks up bony erosions. CT scans better delineate damaged osteoarticular parts of the joint with the extent of the disease.23 Over one-third of patients had notable changes in CT scan, including bone and cartilage destruction, diffuse enhancement and calcification, soft tissue masses crossing anatomical planes with involvement of underlying viscera.2,3 An MRI was done in 29% cases which had changed such as signal intensity alterations, soft tissue mass, abscess, distended joint and areas of cortical destruction. There was communication between the lung and sternoclavicular joint in the arthrogram that was done in only one case.7 Abnormal uptake was noted in Tc99 scan, performed in two cases.7 Other features of SCJ TB include soft tissue masses crossing fascial planes, with abscess and calcification as well as underlying pleuro-parenchymal tubercular involvement.3 MRI gives effective soft tissue delineation with sensitivity of 88% and a sensitivity of 93%. It shows bone marrow edema and collection in the vicinity of the joint. Ultrasonography also detects collection around SCJ. The USG can be used for aspiration; as many vital structures are in the vicinity of the joint. Shah et al.3 suggested that all modalities complement each other though MRI is better in detecting marrow and soft tissue involvement.
ESR and CRP are usually elevated in every patient. The review suggests a biopsy showed caseous granulomas in 74.4% cases. AFB were seen in 12.7% cases and the same percentage of cases had a positive MTB culture. TB-PCR was positive in 30% cases. As osteoarticular TB is paucibacillary pathology hence microbiological evaluation is mostly negative. Histopathology can show chronic granulomatous inflammation. TB-PCR is a good tool as it can detect even traces of MTB DNA. Any single investigation is not sufficient for diagnosis. It is the combined approach which is required for the correct diagnosis. In 4 patients, we could not demonstrate MTB in ZN staining, culture or TB-PCR nor do there be any evidence of granulomatous inflammation on histopathological examination. In these patients, we started ATT on clinical suspicion and found clinical improvement in 4–6 months.
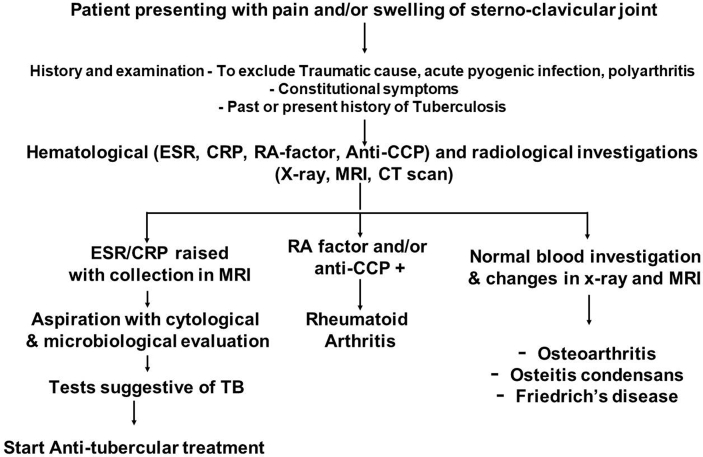
Differential diagnosis of SCJ TB includes osteoarthritis, low grade pyogenic infection, rheumatoid arthritis, Friedrich’s disease, secondary deposits and osteitis condensans. Osteoarthritis is typically present in elderly patients with sclerotic joint surfaces, osteophytes and reduced joint space. Rheumatoid arthritis is usually polyarticular with morning stiffness, affecting the small joints of hand and feet. Positive rheumatoid factor and anti-CCP clinches the diagnosis. Septic arthritis will have systemic signs of sepsis, elevated infection markers and purulent aspirate. On local examination, swelling with inflammation will be present. Osteitis condensans affects younger women and shows expansion of the medial end clavicle and medullary obliteration on radiographs. Friedrich’s disease is an aseptic osteonecrosis of the medial end of the clavicle which can have cystic changes on X-ray and often resembles osteomyelitis or tumor. Sometimes the symptoms and signs overlap between the above mentioned pathologies where histopathological and microbiological evaluation should be considered to reach an accurate diagnosis. Fig. 5 showed clinical decision making process for diagnosing sternoclavicular joint tuberculosis.
Fig. 5.
Diagnostic algorithm showing clinical decision making process for diagnosing sternoclavicular joint tuberculosis.
ATT was given in all reported patients in the literature. Debridement was done in 8 cases. The medical treatment usually was continued from 6 to 18 months. Long-term treatment for 12–18 months, usually resolves the problems of recurrence and relapse. 33ATT results in better outcome as pain and swelling subsided in all but one of our patients at 6 months. Dhillon et al.12 noted that there were better results when surgical debridement was done at the time of open biopsy. Sahu15 mentioned en-block resection in cases where infection extends beyond the joint on imaging. According to our opinion, surgery is not necessary in all the cases because the disease responds well to the anti-tubercular drugs. Moreover, surgery needs a bigger incision which is cosmetically unappealing at this exposed site of SCJ.
5. Conclusion
SCJ TB is commonly misdiagnosed as osteoarthritis or inflammatory arthritis or as a traumatic event. One should evaluate in a line of tuberculosis using modalities like MRI, cytology, histopathology, culture and TB-PCR, before labelling it as a non-tubercular arthritis. This leads to correct early diagnosis and commencement of ATT, reducing patient morbidity.
Contributor Information
Sanjeev Kumar, Email: sanjeevmamc88@gmail.com.
Vijay Kumar Jain, Email: drvijayortho@gmail.com.
References
- 1.Tuli S.M. Jaypee; New Delhi, India: 1993. Tuberculosis of Skeletal System: Bones, Joints, Spine and Bursal Sheaths; pp. 121–123. [Google Scholar]
- 2.Bezza A., Niamane R., Benbouazza K., el Maghraoui A., Lazrak N. Tuberculosis of the sternoclavicular joint. Report of two cases. Rev Rhum Engl Ed. 1998;65(12):791–794. [PubMed] [Google Scholar]
- 3.Shah J. Tuberculosis of sternum and clavicle: imaging findings in 15 patients. Skeletal Radiol. 2000;29:447–453. doi: 10.1007/s002560000207. [DOI] [PubMed] [Google Scholar]
- 4.Robinson C.M., Jenkins P.J., Markham P.E., Beggs I. Disorders of the sternoclavicular joint. J Bone Joint Surg Br. 2008;90(6):685–696. doi: 10.1302/0301-620X.90B6.20391. [DOI] [PubMed] [Google Scholar]
- 5.Simon G.L., Worthington M.G. An unusual case of pleural, epididymal and sternoclavicular tuberculosis. J Infect. 1982;4(3):259–261. doi: 10.1016/s0163-4453(82)92605-6. [DOI] [PubMed] [Google Scholar]
- 6.Martini M. Springer; Berlin Heidelberg New York: 1988. Tuberculosis of the Bones and Joints; pp. 149–150. [Google Scholar]
- 7.Yasuda T., Trauma K., Fujiwara M. Tuberculous arthritis of the sternoclavicular joint – a report of three cases. J Bone Joint Surg Am. 1995;77:136–139. doi: 10.2106/00004623-199501000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Fang J.T., Huang C.C., Liu H.P. Apparent neoplasm of the clavicle of a dialysis patient, ultimately revealed as tuberculosis. Nephrol Dial Transplant. 1996;11:1380–1382. [PubMed] [Google Scholar]
- 9.Sy M.H., Konate I., Gassama A., Kane A., Seye S.I. Monoarticular/sternoclavicular arthritic tuberculosis: a proposal and an observation. Int 1 Tubevc Lung Dzs. 2000;4:486–487. [PubMed] [Google Scholar]
- 10.Dhillon M.S., Gupta R., Rao K.S., Nagi O.N. Bilateral sternoclavicular joint tuberculosis. Arch Orthop Trauma Surg. 2000;120:363–365. doi: 10.1007/s004020050486. [DOI] [PubMed] [Google Scholar]
- 11.Fukasawa H., Suzuki H., Kato A., Yamamoto T., Fuigaki Y., Yonemura K. Tuberculous arthritis mimicking neoplasm in a hemodialysis patient. Am J Med Sci. 2001;322(6):373–375. doi: 10.1097/00000441-200112000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Dhillon M.S., Gupta R.K., Bahadur R., Nagi O.N. Tuberculosis of the sternoclavicular joints. Acta Orthop Scand. 2001;72(5):514–517. doi: 10.1080/000164701753532862. [DOI] [PubMed] [Google Scholar]
- 13.Khan S.A., Zahid M., Asif N., Hasan A.S. Tuberculosis of the sternoclavicular joint. Indian J Chest Dis Allied Sci. 2002;44(4):271–273. [PubMed] [Google Scholar]
- 14.Kawasaki T., Sasaki Y., Shinozaki A. Tuberculosis of the sternoclavicular joint. Kekkaku. 2007;82(5):475–479. [PubMed] [Google Scholar]
- 15.Sahu S. Sternoclavicular Tuberculosis. Med J Armed Forces India. 2008;64(4):373–374. doi: 10.1016/S0377-1237(08)80031-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amano H., Takamori M., Fujita A., Sakashita K., Murata K. A case of sternoclavicular joint tuberculosis with renal failure due to rifampicin. Kekkaku. 2009;84(8):591–595. [PubMed] [Google Scholar]
- 17.Aggarwal A.N., Dhammi I.K., Singh A.P., Kumar S., Goyal M.K. Tubercular osteomyelitis of the clavicle: a report of four cases. J Orthop Surg. 2009;17(1):123–126. doi: 10.1177/230949900901700128. [DOI] [PubMed] [Google Scholar]
- 18.Pandita K.K., Sharma R., Dogra S., Pandita S. Bilateral sternoclavicular joint tubercular cold abscess. Ann Thorac Med. 2010;5(1):56–57. doi: 10.4103/1817-1737.58966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shrivastav A., Pal J., Karmakar P.S., Debnath N.B. Tuberculosis of sternoclavicular joint-uncommon manifestation of a common disease. J Med. 2010;11(1):102–104. [Google Scholar]
- 20.Grover S.B., Jain M., Dumeer S., Sirari N., Bansal M. Chest wall tuberculosis - a clinical and imaging experience. Indian J Radiol Imag. 2011;21(1):28–33. doi: 10.4103/0971-3026.76051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khare P., Sharma V., Khare S. Tuberculosis of the sternoclavicular joint. J Orthop Trauma Rehabil. 2013;17(2):96–98. [Google Scholar]
- 22.Kelderman S., Steenvoorde P., van der Valk P.D. Sternoclavicular joint tuberculosis. Ned Tijdschr Geneeskd. 2012;156(18):A3315. [PubMed] [Google Scholar]
- 23.Metanat M., Alavi-Naeini R. Sternoclavicular joint tuberculosis with cold abscess. Iran J Clin Infect Dis. 2012;1:29–31. [Google Scholar]
- 24.Koshy S. A rare case of sternoclavicular joint tubercular cold abscess. IntJ PrevTher Med. 2014;2:134–138. [Google Scholar]
- 25.Saibaba B., Meena U.K., Behera P., Meena R.K. Multicentric spinal tuberculosis with sternoclavicular joint involvement: a rare presentation. Case Rep Pulmonol. 2014;2014:685406. doi: 10.1155/2014/685406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walid O., Amine T.M., Hamdi K., Sonia J. Tuberculosis arthritis of the sternoclavicular joint. Open J Orthoped. 2015;5:135–139. [Google Scholar]
- 27.Jain A., Jajodia N., Aggarwal A., Singh J., Gupta S. Tuberculosis of the sternoclavicular joint. J Orthop Surg. 2015;23(3):315–318. doi: 10.1177/230949901502300311. [DOI] [PubMed] [Google Scholar]
- 28.Akhtar M.N., Agarwal S., Athar R. Clinico-radiological approach to a rare case of early clavicle tuberculosis: a case discussion based review of differential diagnosis. J Clin Diagn Res. 2015;9(6):RE01–RE05. doi: 10.7860/JCDR/2015/11971.6079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meena U.K., Saibaba B., Behera P., Meena R.K. Sternoclavicular joint tuberculosis: a series of 9 cases. Indian J Tubercul. 2017;64(3):221–224. doi: 10.1016/j.ijtb.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Jha A.K., Jha A.C., Mishra N. Tuberculosis of the sternoclavicular joint: report of three cases. J Assoc Phys India. 2018;66(10):96. [PubMed] [Google Scholar]
- 31.Prakash J., Sareen A., Arora P., Chopra R.K. Sternoclavicular tuberculosis: an atypical imitator of refractory shoulder pain. Int Orthop. 2020 Apr;44(4):693–698. doi: 10.1007/s00264-019-04400-3. [DOI] [PubMed] [Google Scholar]
- 32.Tsay M.H., Chen M.C., Jaung G.Y., Pang K.K., Chen B.F. Atypical skeletal tuberculosis mimicking tumor metastases: report of a case. J Formos Med Assoc. 1995;94:428–431. [PubMed] [Google Scholar]
- 33.Tuli S.M. Clinical features. In: Tuli S.M., editor. fourth ed. vols. 54–55. Jaypee Brothers; New Delhi, India: 2010. pp. 62–64. (Tuberculosis of Skeletal System (Bones, Joints, Spine and Bursal Sheaths)). [Google Scholar]