Abstract
Introduction
Management of the complex non union of tibia is a challenging task due to infection, bony gap, deformity, poor bone quality and poor soft tissue cover at fracture site. The limb reconstruction system (LRS) or Rail fixator has emerged as a viable option for the treatment of the same as it can address most of all above problems. It is more patient friendly and easier to apply in comparison to Ilizarov ring fixator.
Material and methods
Twenty two patients (17 males and 5 females) with complex non union of tibia underwent thorough debridement and resection of non viable bone followed by bone transport to fill the gap and then lengthening (8 patients) or acute docking & lengthening (14 patients) by the use of rail fixator. The average time to union, bone gap filled, lengthening achieved, treatment index were measured. The bone and functional outcome assessment was done by ASAMI score. The complications were classified according to Paley’s classification.
Results
Union without residual infection was achieved in 20 (90.1%) patients while 2 patients had failure. As per ASAMI criteria bone results were excellent in 12 (54.5%), good in 5 (22.7%), fair in 3 (13.6%) and poor in 2 (9.1%). Functional results were excellent in 11 (50%), good in 5 (22.72%), fair in 4 (18.18%) and failure in 2 (9%). Mean treatment duration was 8.2 months (range 7–19 months). Mean follow up duration was 11.3 months (range - 8.3 to 22 months). Average lengthening achieved was 4 cm (0–9 cm). Treatment index was 2.1 month/cm
Conclusion
The monolateral rail fixator is simple, effective, easier to apply and more patient compliant with acceptable functional and radiological outcome.
Keywords: Complex non-union, Tibia, Limb reconstruction system, Rail fixator, Corticotomy, Bone transport
1. Introduction
The complex non union of tibia has been defined as an established non union (of at least 6 months) with one or more of the following criteria: a) infection at non union site, b) a bone gap > 4 cm, c) an attempt to achieve union that failed to heal after at least one supplementary intervention for example bone grafting or exchange nailing.1 The incidence of complex non union has increased in last few years due to increased incidence of road traffic accidents due high velocity. Patients of complex non union already have undergone multiple surgeries in form of stabilization to achieve union and/or control infection thereby leading to scarred soft tissues and devitalized bone at the fracture site. The problem is further exacerbated by the deformity, persistent infection, limb length discrepancy, disuse osteoporosis, atrophy of muscles and stiffness of adjacent joints.
The common method of doing soft tissue coverage followed by bone grafting although serves to achieve bony union but the functional outcome may be poor because of residual limb length discrepancy, deformity, long and repeated treatment. And also donor site morbidity and failure to use bone graft in presence of infection are other disadvantages.2, 3, 4
The Ilizarov ring fixator addresses the above problems in one go by addressing limb length discrepancy, gap at non union site, deformity. Weight bearing and joint movement can be allowed thereby preventing disuse osteoporosis and joint stiffness. However the tensioned wires of ring fixator can lead to soft tissue transfixation leading to neurovascular compromise and distort the local anatomy.5,6 They are also less tolerated and difficult to apply. In contrast to the ring fixator the rail fixator is less bulky and has lighter frame, easy to apply and is acceptable to the patients also. So this study has been undertaken with the aim to evaluate the role of monolateral rail fixator in the management of complex non union of tibia.
2. Materials and methods
We conducted a prospective study on 22 patients (17 males & 5 females) with established gap non union of the tibia who were managed by using monolateral rail fixator device between January 2014 to December 2016. The patients included in the study were those presenting with fracture tibia without any neurovascular compromise along with any of the following:
a) Infection at the site of non union, b) Bone defect of more than 4 cm, c) An attempt to achieve union that failed to heal after at least one supplementary intervention, for example bone grafting or exchange nailing. Non unions fracture due to congenital disorders, complex non union following pathological fractures (except due to infection), patients not medically fit, and those not willing to cooperate with long follow up were excluded from the study. A total of 22 patients (17 male and 5 females) with average age 31 years (range 16–55 years) were included in the study. All the patients demographic data and detailed history and examination for sinus, pus discharge, skin condition, shortening, deformity, and function and neurovascular status of the limb were recorded on a preformed Performa. The study was approved by local institutional review committee. All patients were explained completely about the nature and type of surgical procedures as per the protocol and other supplementary procedures that can be performed if needed. Full informed consent was taken from each patient.
The patients were prepared for either regional or general anaesthesia. Preoperative assessment of soft tissue defect and planning for subsequent reconstruction was done. Any implant, such as a plate or an intramedullary nail, present in situ was removed first. Adequate debridement of all the dead and necrotic bone as well as scarred soft tissues and sinus tracts was done. The end point of bony debridement was considered when there was punctate bleeding from cortical margins. Tissue after debridement was sent for culture and sensitivity. Empirical intravenous antibiotic- Cefoperazone and Amikacin were started. Most common organism grown in culture was Staphylococcus aureus in 7 patients, Staphylococcus epidermidis in 2 patients, E. coli in 3 patients, mixed aerobic and anaerobic growth were seen in 2 patients and no growth in 8 patients. Monolateral external fixator or rail external fixator was used to stabilize the fracture. We used the Rail External Fixator System from SH Pitkar Orthotools, Pune, India, Newlife Surgical Works, New Delhi, India, and Kaushik Orthopaedic Pvt. Ltd. Delhi, India. A single-level corticotomy and distraction was performed through healthy tissue when the gap or shortening was more than 2 cm. The wound was closed in layers after thorough lavage. Fibulectomy was done in all the patients in whom acute docking was done by resecting fibula of size 1 cm larger than the gap created after resection of tibia at the same level and in two patients of bone transport and lengthening. Plastic cover was done in 8 cases prior to application of rail fixator to close soft tissue defect, no plastic opinion was sought intraoperatively or after rail fixator application.
In the post operative period, IV antibiotics were given for initial 4 days and there after oral antibiotics were given till stitch removal as per the culture and sensitivity report. If infection persisted in form of wet stitch line or continuous soakage from wounds then I.V. antibiotics were continued up to 2 weeks then switched to oral antibiotics. Distraction was started on 7th post-operative day. Physiotherapy of the adjacent joints and partial weight bearing walk was started with the help of crutches from the next postoperative day as tolerated by the patient. Daily pin tract cleaning and dressing was done with povidone iodine soaked gauze piece.
Patients were followed up regularly in OPD every two weeks for the first two months and thereafter every month till docking of the fracture fragments was achieved. Patients were allowed to walk bearing full weight once docking of the bone fragments was achieved to enhance union. Patients were reviewed thereafter every two months till there was union (Fig. 1, Fig. 2). At each visit patient were enquired and examined for pain, limp, level of activity, stiffness of adjacent joint, pin tract infection, loosening of pins, local skin condition, shortening, reflex sympathetic dystrophy. Patients were asked whether they resumed their job or were unemployed. Radiological outcome was measured where formation of regenerate, union, any signs of osteomyelitis, deformity were assessed. The infected non union was classified as per criteria given by Jain et al.7 and non union of tibia was classified as per Paley’s classification8 (Table 1). Patients were said to be having a quiescent infection if the wounds which they had, did not show any discharge for 3 months.7 The patients who were classified as A1 (quiescent infection with defect less than 4 cm) later qualified to be cases of complex gap non union because after debridement they had developed defect >4 cm. The fracture was considered united when 3 cortices were visible in two orthogonal views of X-ray image. The complications were graded into problem, obstacle, or true complication as per Paley’s classification.9 Problem comprised of those issues which required no operative intervention while obstacles required operative intervention. While the true complications were those which remain unresolved during or at the end of the treatment. Results were calculated and graded as excellent, good, fair and poor based on ASAMI Scoring System (Table 2).
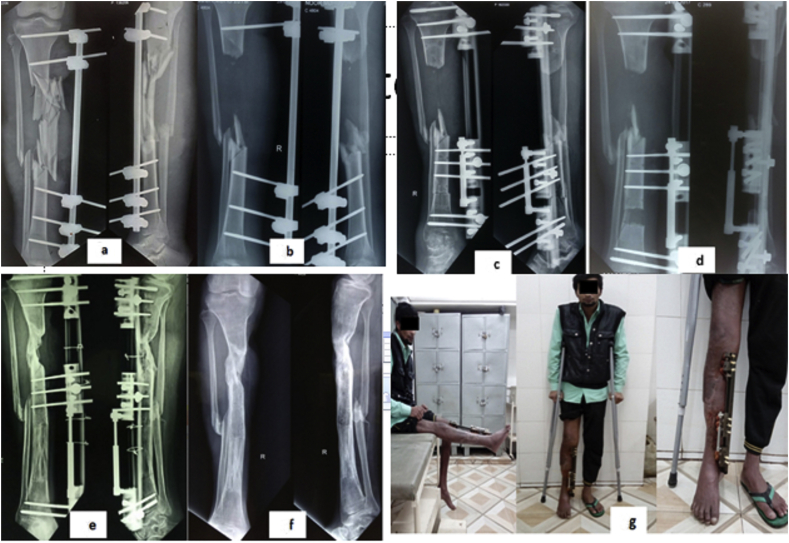
Fig. 1.
Twenty year old male with infected non union left Tibia proximal 1/3rd (10 months old) with tubular external fixator and discharging sinus, a)Preop xray; b)Post op Xray after thorough debridement, resection of all infected bone with gap and rail fixator in situ; c) 6 month follow up x ray shows mal alignment of middle segment for which it was manipulated and docking site freshened also; d) At 8 months follow up; e) At 15 months follow up with solid union of fracture site so fixator was removed; f) After rail fixator removal; g) clinical photograph of patient after rail fixator removal with full flexion and 1 cm residual shortening so shoe raise given; h) patient standing full weight bearing.
Fig. 2.
a) A twenty two years male presented to us infected comminuted fracture of right tibia in proximal half with skin defect and external fixator in situ 4 ½ months after sustaining injury; b) All the infected and devitalized bone and tissues were debrided and flap was applied by plastic surgeons to cover the wound; c) Six weeks after plastic surgery rail fixator was applied and distal corticotomy was done; d) 5 weeks after rail fixator application; e) 7.5 months after rail fixator application; f) After 11 months rail fixator was removed with solid union at docking site; g) clinical photograph of patient with full extension and patient standing partial weight bearing with crutches.
Table 1.
| Infected non union grading | Number of patients (%) | |
|---|---|---|
| A1-Quiescent infection with defect <4 cm | 6 (27.3) | |
| A2- Quiescent infection with defect >4 cm | 4 (18.1) | |
| B1- Actively discharging sinus with defect <4 cm | 7 (31.8) | |
| B2- Actively discharging sinus with defect >4 cm | 5 (22.7) | |
| Classification of non union of tibia (Paley et al.8) | ||
| Type A- Nonunions with bone loss of <1 cm | ||
| A1-Lax/mobile non-union | 0 | |
| A2- Stiff/non-mobile | A2-1 With no deformity | 0 |
| A2-2 With fixed deformity | 0 | |
| Type B - Nonunions with bone loss of >1 cm | ||
| B1- Bony defect, no shortening | 4 (18.2) | |
| B2- Shortening, no bony defect | 5 (22.7) | |
| B3- Bony defect and shortening | 13 (59.1) | |
Table 2.
Association for the Study and Application of the Methods of Ilizarov (ASAMI) scoring system and number of patients in each group.
| Bone results | Functional result | Number of patients (Bone result/Functional result) | |
|---|---|---|---|
| Excellent | Union, no infection, deformity<7°, limb length Discrepancy<2.5 cm |
Active, no limp, minimum stiffness (loss of <15°knee extension/<15° dorsiflexion of ankle), No reflex sympathetic dystrophy, insignificant Pain |
12/11 |
| Good | Union + any two of the following: No infection, deformity<7°, limb length discrepancy< 2.5 cm |
Active with one or two of the following: Limp, Stiffness, RSD, significant pain. |
5/5 |
| Fair | Union + only one of the following: No infection, deformity<7°, limb length discrepancy< 2.5 cm |
Active with three or all of the following: Limp, Stiffness, RSD, significant pain |
3/4 |
| Poor | Non-union/refracture/union + infection + Deformity>7° + limb length discrepancy>2.5 Cm |
Inactive (unemployment or inability to return to Daily activities because of injury) | 2/2 |
| Failure | Amputation | 2 |
3. Results
Most of the patients presented to us with complex non-union after sustaining road traffic accidents with majority being males. The details of the patients are given in Table 3.
Table 3.
Patients details.
| Total number of patients included in study | 22 | |
|---|---|---|
| Fracture side | Right | 15 |
| Left | 7 | |
| Gender | Male | 17 |
| Female | 5 | |
| Mechanism of injury | Road traffic accident | 18 (81.8%) |
| Fall from height | 1 (4.5%) | |
| Machinery injury | 1 (4.5) | |
| Complex gap non union following chronic osteomyelitis | 2 | |
| Number patients with external fixator in situ | 08 (36.4%) | |
| Number of patients with infected nail in situ | 05 (22.7%) | |
| Number of patients with infected plate in situ | 03 (13.6%) | |
| Number of patients who had prior plastic surgery | 08 (36.4%) | |
| Number of patients with raised ESR | 22 | |
| Number of patients with raised CRP | 22 | |
| Mean number of previous surgery | 02.43 (range 1–5) | |
| Mean time from injury to presentation | 1.8 years (range 6 months–19 years) | |
Mean duration from trauma to presentation was 1.8 years (range 6 months–19 years). Twelve patients had discharging sinus at presentation. Mean bone defect after adequate debridement was 4.7 cm (range 2–9 cm). Average shortening was 4.38 cm (0 cm–15 cm). Bone transport to fill the gap followed by lengthening was done in 8 patients and acute docking & lengthening in 14 patients. Out of the 22 patients treated union was achieved in 20 patients (90.9%) and 2 went into failure due to intractable infection. Infection was eradicated in 20 (90.2%) patients. Average lengthening achieved was 4 cm (0–9 cm). Mean shortening after treatment was 1.5 cm (Range 0–4.5 cm). Mean treatment index (number of months for which external fixator is kept in situ/total length gained in centimetres) was 2.1 months per cm (Table 4).
Table 4.
Details of treatment related result.
| Treatment variables | |
|---|---|
| Mean bone defect | 4.7 cm (range 2–9 cm) |
| Mean shortening before treatment | 4.38 cm (0 cm–13.5 cm) |
| Number of patients who underwent bone transport followed by lengthening (gradual closure of bone defect) | 08 |
| Number of patients who underwent Acute docking and lengthening | 14 |
| Number of patients in whom Bony union was achieved | 20 |
| Number of patients who required fibulectomy | 16 |
| Mean lengthening achieved | 4 cm (0–9 cm) |
| Mean shortening after treatment | 1.5 cm (Range 0–4.5 cm) |
| Mean treatment index | 2.1 months per cm |
| Mean follow up | 11.3 months (8.3–22 months) |
| Mean treatment duration | 8.2 months (7–19 months) |
Results were calculated according to ASAMI scoring system which includes various clinical and radiological parameters. Bone results were excellent in 12 (54.5%), good in 5 (22.7%), fair in 3 (13.6%) and poor in 2 (9.1%). Functional results were excellent in 11 (50%), good in 5 (22.72%), fair in 4 (18.18%), poor in 2 (9%). Two cases were declared failure. Mean treatment duration was 8.2 months (range 7–19 months). Mean follow up duration was 11.3 months (range - 8.3 to 22 months). Two patients developed intractable infection with extensive soft tissue devitalisation so had to undergo below knee amputation and were categorised as failure as per ASAMI criteria (Table 2).
Complications were classified as per Paley’s classification.7Pin tract infection was seen in 13 (59.1%) patients (most common problem) and pain during distraction in 15 (68.1%) patients. Pin loosening (n = 4, 18.18%) was the most common obstacle and joint stiffness (n = 2, 9.1%) was most common true complication. In our study at completion of treatment, there was no significant angular deviation (>15°) in any case. Only one case (4.54%) had angulation of 5⁰. Neurovascular complications, joint subluxation or fracture of regenerate or docking site was not seen in any of the cases. Problem of union at the docking site was encountered in 5 cases. In 3 (13.6%) cases secondary procedures were done. In 1 patient (4.54%) only freshening of bone ends was done to achieve union as intraoperatively fracture site had good punctate bleed and adequate compression achieved so we decided not to do bone grafting and the fracture united uneventfully. Freshening of bone ends with bone grafting was done in 2 patients (9.1%) to achieve union. Delayed maturation of regenerate was dealt with slowing or stopping the distraction for 1–2 weeks.
4. Discussion
The goal of treating a complex non-union is to achieve a fully functional limb without any deformity, with union at fracture site and no residual infection or limb length discrepancy.8Achieving the above goal is a challenge to the treating orthopaedician. The concept of distraction histogenesis given by Ilizarov10 whereby the bone and soft tissue regeneration occurs when subjected to tensile stress is a boon for treatment of these complex non-union. But the technique and procedure of application of the Ilizarov ring fixator is complex, difficult, time taking and fraught with potential for numerous complications.9 Limb reconstruction system (LRS) or rail fixator is another implant that tends to work on the same principle as that of Ilizarov ring fixator. It is uniplaner external fixator device which is light, easy to construct and apply and has a short learning curve. Also the sliding clamps can be adjusted easily to alter the spread of the pins across the fracture site unlike the need to alter the nut bolts over the threaded rods in Ilizarov ring fixator.11 However being uniplaner rail fixator is not suitable for fracture with deformity in three dimensions.11 To achieve the desired limb length without any bone defect either the defect can be docked acutely and then lengthening is done or gradual distraction of osteotomy site and transport to fill the defect and continued distraction to take care of shortening of limb is done. Acute docking and lengthening is suitable for defect of ≤3 cm for tibia and ≤5 cm for femur.12 Gradual distraction and filling of bone defect is done in cases where defect is larger. The major advantages of acute docking and lengthening are immediate full contact between the bone ends can be achieved, immediate stimulation of the docking site for union without transporting difficulties through the soft tissues there by leading to lesser incidence of delayed or non-union of docking site.
In our study 20 out of 22 patients developed union without any residual infection. As per ASAMI criteria bone results were excellent in 12 (54.5%), good in 5 (22.7%), fair in 3 (13.6%) and poor in 2 (9.1%). Functional results were excellent in 10 (45.45%), good in 5 (22.72%), fair in 4 (18.18%). Our results were similar to those of other studies (Table 5).
Table 5.
Comparision of bone and functional result of various studies.
| Author and year of publication | Method of fixation (bones fixed) | No. of patients of tibial complex non union | Functional result as per ASAMI criteria (Excellent/good/fair/poor/failure) In percentage |
Bone results as per ASAMI criteria Excellent/good/fair/poor In percentage |
Percentage of patients who achieved bony union |
|---|---|---|---|---|---|
| Patil and Montgomery et al.13 2006 | IRF (tibia and femur) | 78 | 41/41/6/6/6 | 41/34/10/15 | 85 |
| Yin et al. 201414 | IRF (Tibia & femur) | 66 | 66/22/8/4 | 73/25/8/3 | 97 |
| Harshwal et al.15 2014 |
REF (Tibia & femur) | 37 | 73/16/3/8/0 | 65/24/3/8 | 92 |
| Ajmera et al.16 2015 |
REF (Tibia only) | 30 | 84/8/8/0/0 | 76/12/4/8 | 92 |
| Tetsworth et al.17 2017 |
IRF (Tibia only) | 21 | 67/28/5/0 | 71/24/5/0 | 100 |
| Zhang et al. 201818 | IRF (Tibia only) | 16 | 62.5/0/0/37.5 | 75/25/0/0 | 100 |
| Bhardwaj et al.19 2019 |
IRF (Tibia & femur) | 25 | 32/32/36/0/0 | 28/32/40/0 | 100 |
| Bhardwaj et al.19 2019 |
REF (Tibia & femur) | 25 | 32/52/16/0/0 | 32/52/16/0 | 100 |
| Present study | REF (Tibia only) | 22 | 50/23/18/9 | 54/23/14/9 | 91 |
Aktuglu et al.20 performed a review of the outcome of Ilizarov ring fixator in infected non union of tibia and evaluated results of 27 studies published between 2008 and 2018 that consisted of a total of 619 patients and found combined bone result (excellent + good) to be 88.6% and functional result (excellent + good) to be 82.6%. Similarly Yin et14 al performed a review of 13 studies published between 1995 and 2013 which consisted of results of 303 patients of infected non union tibia and had combined (excellent + good) bone result of 87% and functional result of 76%.
Bhardwaj et al.19 in their comparative study between role rail and Ilizarov ring fixator in infected non union of long bones had good to excellent functional result in 84% patients in rail fixator group while 64% in Ilizarov ring fixator group although both group had 100% bony union. So they recommended Ilizarov ring fixator to be used in highly comminuted fracture that too near to joints otherwise rail fixator was equally good and had was associated with lesser complication, more acceptable to the patient and easier to apply.
Mean treatment index (number of months for which external fixator is kept in situ/total length gained in centimetres) in our study was 2.1 months per cm, which is comparable to other studies. Marais et al.,21 Pirwani et al.,22 Khan et al.23 and Aktuglu et20 al had a treatment index of 2.7, 3, 4.2 and 1.73 months per cm respectively after Ilizarov ring fixator application. Comparable treatment indices strengthened our belief that rail fixator gives equally good results and in equally acceptable time period as that of Ilizarov. The duration or treatment index mainly depends on the size of gap, shortening and type of distraction whether monofocal, bifocal or trifocal. The average bone gap and mean shortening in our study were 4.7 cm (range 2–9 cm) and 4.38 cm (0 cm–13.5 cm) respectively. Saleh et al.12 had an external fixation index or treatment index of 2.04 months/cm (mean bone defect 4.7 cm) in the bifocal compression distraction group while in bone transport group treatment index was 2.5 months/cm (mean bone defect - 6.5 cm). Paley et al.27 similarly had mean external fixation index of 2.1 months/cm in single level and 1.2 months/cm in a double-level bone transport (mean bone loss 10.7 cm).
Acute docking and lengthening was done in 14 patients whereas 8 patients had transport of middle segment and then lengthening was done to compensate for shortening. El Rosasy24 recommended maximum acute shortening in leg depends on the level of fracture exceeding the limit led to vascular compromise as confirmed by Doppler ultrasound and buckling of soft tissue that prevented further shortening. These safe limits are 3 cm proximal third leg, 3–5 cm in middle third leg and upto 6 cm in distal third. We adhered to above limits and eight patients who had large bone defect after debridement had to undergo gradual distraction 5 of which had problems of delayed union at docking site. Two united with compression alone and PTB calliper was given for 8 weeks, while 1 had to undergo freshening of bone ends, and the rest 2 had to undergo freshening of bone ends along with iliac crest grafting to achieve union. Harshwal et al.15 and Ajmera et al.16 in their study on 37 and 30 patients using rail fixator had to do bone grafting in 2 patients each. Bhardwaj et al.19 had to inject bone marrow aspirate at the docking in two patient fixed with Ilizarov and 4 patients treated by rail fixator to achieve union.
Pin tract infection was seen in 13 (59.1%) patients (most common problem) and pain during distraction in 15 (68.1%) patients. Pin loosening (n = 4, 18.18%) was the most common obstacle and joint stiffness (n = 2, 9.1%) was most common true complication. On comparing with the complications seen in other studies (using Ilizarov as well as rail fixator) we had similar incidence of various complications as listed in (Table 6).
Table 6.
Comparision of complications of various studies.
| Study (author and year) | Mode of fixation | Total number of patients | Pin tract infection | Joint stiffness (>15⁰ loss of Range of motion at knee or ankle) | Persistent infection No. | Shortening >2.5 cm at end of treatment | Delayed union requiring grafting or freshening of docking site | Deformity (>7⁰ malalighnment) | Amputation | others |
|---|---|---|---|---|---|---|---|---|---|---|
| Sen et al. 200425 | IRF | 24 | 9 | 3 | 1 | 1 | 0 | 1 | 0 | |
| Seenappa et al. (2013)26 | REF | 30 | 22 | 13 | 2 | 0 | 0 | 5 | 0 | Refracture- 01 Premature union of corticotomy- 1 |
| Harshwal et al. 201415 | REF | 37 | 11.7%a | 3 | 1 | 2 | 2 | 1 | 0 | Non union-03 |
| Ajmera et al.16 2015 |
REF | 30 | 5 | 9 | 1 | 2 | 2 | 0 | 0 | |
| Tetsworth et al.17 2017 | IRF | 21 | 8 | 5 | 0 | 0 | 7 | 1 | 0 | |
| Zhang et al. 201818 | IRF | 16 | 13 | 3 | Not available | 0 | 3 | 0 | 0 | |
| Bhardwaj R19 et al., 2019 | IRF | 25 | 18 | 5 | 0 | 5 | 1 | 0 | Pain in all patients | |
| Bhardwaj R19 et al., 2019 | REF | 25 | 14 | 2 | 0 | 8 | 0 | 0 | Pain in all patients | |
| Present study | REF | 22 | 13 | 2 | 2 | 0 | 3 | 0 | 2 |
Out of 162 pins 19 got infected; REF-rail external fixator, IRF- Ilizarov ring fixator.
Pin tract infection was the most common problem encountered which was managed by daily pin tract cleaning and dressing. Pain was mainly present during the distraction phase and was controlled on oral analgesics. We had 4 cases who developed pin loosening 2 had loosening of the proximal most pin in the tibial condyles and 2 patients in distal clamp which were replaced and new pin inserted in another position in the same clamps. Two of our patients developed equinus deformity at ankle joint which was corrected by tendo Achilles lengthening. There was no case of malalignment >7⁰ except one patient who had small middle fragment which developed displacement of the distal fragment medially with respect to transported middle segement (Fig. 1c) when ends apposed at docking site so it was aligned under short general anaesthesia after loosening the pins in the middle and distal clamps, the docking site united uneventfully. (Table 6).
Two of our patients had to undergo below knee amputation as they had intractable infection. The soft tissue in both the patients were severely scarred and adhered to underlying bone as the infected gap non union in both was in distal one third of tibia and had already under gone multiple previous surgeries. In one patient nailing was done initially which got infected with exposure of underlying bone in distal third tibia, nail was removed, external fixator was applied, plastic surgery was done to apply flap but discharging sinus persisted. So he underwent thorough debridement and rail fixator was applied but infection persisted leading to amputation. In second patient who had infected distal tibia locked plate had undergone plate removal, thorough debridement and rail fixator application. But distal fragment was small and after closure wound dehiscence occurred with frank pus discharge from pin tracts so we had to do a below knee amputation.
The main limitation of our study is lack of control group and small patient sample size. Majority of patients being males (17 males in comparison to 5 females only), average age 31 years (range 16–55 years) that is more young patients were included, both these factors may have favourably skewed the results towards better side as females and elderly have lower immunity28, 29, 30 and different inflammatory response due to different hormonal milieu in females.31
The studies we have included to compare our results vary in sample size, have been published in different geographic areas, the patients demographic data are also different, different fixators have been used. So we think that a multi centre randomized controlled trial on a large population and geographic area comparing rail fixator with Ilizarov ring fixator for management of complex non union of tibia is needed to confirm or negate that whether rail fixator a better device than Ilizarov ring fixator.
In conclusion rail fixator is a promising implant for the management of complex non union of tibia. Its main advantages are lighter yet robust frame, greater patient satisfaction, learning curve short, less complication and it addresses both the shortening and deformity. Although less stable, being monoplaner constrct unlike Ilizarov yet it serves the purpose with equally satisfactory functional and radiological results.
Declaration of competing interest
We have no conflict of interest to declare.
Contributor Information
Latif Zafar Jilani, Email: lzjilani@gmail.com.
Ziaul Hoda Shaan, Email: shaan.hoda007@gmail.com.
Rajesh Ranjan, Email: rajeshranjan@gmail.com.
Mohd Faizan, Email: mohdfaizan2002@gmail.com.
Sohail Ahmad, Email: drsohailahmad@rediffmail.com.
Naiyer Asif, Email: naiyerasif@gmail.com.
References
- 1.Patil S., Montgomery R. Management of complex tibial and femoral nonunion using the Ilizarov technique, and its cost implication. J Bone Jt Surg Br. 2006;88B:928–932. doi: 10.1302/0301-620X.88B7.17639. [DOI] [PubMed] [Google Scholar]
- 2.Cierny G., 3rd, Zorn K.E. Segmental tibial defect: comparing conventional and Ilizarov methodologies. Clin Orthop. 1994;301:118–123. [PubMed] [Google Scholar]
- 3.Marsh J.L., Prokuski L., Biermann J.S. Chronic infected tibial nonunions with bone loss: conventional techniques versus bone transport. Clin Orthop. 1994;301:139–146. [PubMed] [Google Scholar]
- 4.Watson J.T., Anders M., Moed B.R. Management strategies for bone loss in tibial shaft fractures. Clin Orthop. 1995;315:138–152. [PubMed] [Google Scholar]
- 5.Grivas T.B., Magnissalis E.A. The use of twin-ring Ilizarov external fixator constructs: application and biomechanical proof of principle with possible clinical indications. J Orthop Surg Res. 2011;6:41. doi: 10.1186/1749-799X-6-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mahran M.A., Elgebeily M.A., Ghaly N.A. Pelvic support osteotomy by Ilizarov’s concept: is it a valuable option in managing neglected hip problems in adolescents and young adults? Strat Trauma Limb Reconstr. 2011;6:13–20. doi: 10.1007/s11751-011-0104-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jain Anil K. Infected non-union of the long bones. Clin Orthop Relat Res. 2005;(431):57–65. doi: 10.1097/01.blo.0000152868.29134.92. saaNumber. [DOI] [PubMed] [Google Scholar]
- 8.Paley D., Catagni M.A., Argnani F., Villa A., Benedetti G.B. Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res. 1989;241:146–165. [PubMed] [Google Scholar]
- 9.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 10.Ilizarov G.A. The tension-stress effect on the genesis and growth of tissues: Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;238:249–281. [PubMed] [Google Scholar]
- 11.Agrawal H.K., Jaiman A., Khatkar V., Sharma V.K. Application of monorail fixator for femoral gap nonunion. Chin J Traumatol. 2014;17(4):239–241. [PubMed] [Google Scholar]
- 12.Saleh M., Rees A. Bifocal surgery for deformity and bone loss after lower-limb fractures: comparison of bone-transport and compression-distraction methods. J Bone Jt Surg [Br] 1995;77-B:429–434. [PubMed] [Google Scholar]
- 13.Patil S., Montgomery R. Management of complex tibial and femoral nonunion using the Ilizarov technique, and its cost implications. J Bone Jt Surg [Br] 2006;88– B:928–932. doi: 10.1302/0301-620X.88B7.17639. [DOI] [PubMed] [Google Scholar]
- 14.Yin P., Ji Q., Li T. A systematic review and meta-analysis of Ilizarov methods in the treatment of infected nonunion of tibia and femur. PLoS One. 2015;10(11) doi: 10.1371/journal.pone.0141973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harshwal R.K., Sankhala S.S., Jalan D. Management of nonunion of lower-extremity long bones using mono-lateral external fixator--report of 37 cases. Injury. 2014;45:560–567. doi: 10.1016/j.injury.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 16.Ajmera A., Verma A., Agrawal M., Jain S., Mukherjee A. Outcome of limb reconstruction system in open tibial diaphyseal fractures. Indian J Orthop. 2015;49:429–435. doi: 10.4103/0019-5413.159638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tetsworth K., Paley D., Sen C. Bone transport versus acute shortening for the management of infected tibial non-unions with bone defects. Injury. 2017;48(10):2276–2284. doi: 10.1016/j.injury.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y., Wang Y., Di J., Peng A. Double-level bone transport for large post-traumatic tibial bone defects: a single centre experience of sixteen cases. Int Orthop. 2018;42:1157–1164. doi: 10.1007/s00264-017-3684-y. [DOI] [PubMed] [Google Scholar]
- 19.Bhardwaj R., Singh J., Kapila R., Boparai R.S. Comparision of Ilizarov ring fixator and rail fixator in infected nonunion of long bones: a retrospective followup study. Indian J Orthop. 2019;53:82–88. doi: 10.4103/ortho.IJOrtho_77_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aktuglu Kemal, Erol Kubilay, Vahabi Arman. Ilizarov bone transport and treatment of critical-sized tibial bone defects: a narrative review. J Orthop Traumatol. 2019;20:22. doi: 10.1186/s10195-019-0527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marais L.C., Ferreira N. Bone transport through an induced membrane in the management of tibial bone defects resulting from chronic osteomyelitis. Strat Trauma Limb Reconstr. 2015;10(1):27–33. doi: 10.1007/s11751-015-0221-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pirwani M.A., Siddiqui M.A., Soomro Y.H. Management of infected non-union tibia by intercalary bone transport. Pak J Surg. 2008;24:26–30. [Google Scholar]
- 23.Khan M.S., Rashid H., Umer M., Qadir I., Hafeez K., Iqbal A. Salvage of infected non-union of the tibia with an Ilizarov ring fixator. J Orthop Surg. 2015;23(1):52–55. doi: 10.1177/230949901502300112. [DOI] [PubMed] [Google Scholar]
- 24.El-Rosasy M.A. Acute shortening and re-lengthening in the management of bone and soft-tissue loss in complicated fractures of the tibia. J Bone Jt Surg [Br] 2005;89-B:80–88. doi: 10.1302/0301-620X.89B1.17595. 2007. [DOI] [PubMed] [Google Scholar]
- 25.Sen Cengiz, Kocaoglu Mehmet, Eralp Levent, Gulsen Mahir, Cinar Murat. Bifocal compression-distraction in the acute treatment of grade III open tibia fractures with bone and soft-tissue loss A report of 24 cases. J Orthop Trauma. 2004;18:150–157. doi: 10.1097/00005131-200403000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Seenappa H.K., Shukla M.K., Narasimhaiah M. Management of complex long bone nonunions using limb reconstruction system. Indian J Orthop. 2013;47:602–607. doi: 10.4103/0019-5413.121590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paley D., Maar D.C. Ilizarov bone transport treatment for tibial defects. J Orthop Trauma. 2000;14:76–85. doi: 10.1097/00005131-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Plowden J., Renshaw-Hoelscher M., Engleman C., Katz J., Sambhara S. Innate immunity in aging: impact on macrophase function. Aging Cell. 2004;3:161–167. doi: 10.1111/j.1474-9728.2004.00102.x. [DOI] [PubMed] [Google Scholar]
- 29.Plackett T.P., Boehmer E.D., Faunce D.E., Kovacs E.J. Aging and innate immune cells. J Leukoc Biol. 2004;76:291–299. doi: 10.1189/jlb.1103592. [DOI] [PubMed] [Google Scholar]
- 30.Linton P.J., Dorshkind K. Age related changes in lymphocyte development and function. Nat Immunol. 2004;5:133–139. doi: 10.1038/ni1033. [DOI] [PubMed] [Google Scholar]
- 31.Gee A.C., Sawai R.S., Differding J., Muller P., Underwood S., Schreiber M.A. The influence of sex hormone on coagulation and inflammation in the trauma patients. Shock. 2008;29:334–341. doi: 10.1097/shk.0b013e3181506ee5. [DOI] [PubMed] [Google Scholar]