Abstract
Traumatic brain injury (TBI) is a major public health issue worldwide. A portable near-infrared spectroscopy (NIRS) is a non-invasive device to detect intracranial hematoma. The advantages of the NIRS include real time results and non-radiation exposure. However, sensitivity and specificity of the NIRS for intracranial hematoma are varied. This study aimed to evaluate the diagnostic properties of the NIRS in TBI patients to detect intracranial hematoma. This study was a diagnostic and prospective study conducted at the Emergency Department. The inclusion criteria were adult patients (age of 18 years or over) with moderate to high risk of all degrees of traumatic brain injury within 24 h after the injury. The primary endpoint of the study was a description of diagnostic properties of the NIRS compared with the CT brain. There were 47 patients enrolled in the study. Most of patients had Glasgow Coma Scale of 15 (44 patients; 93.62 %). Of those, 11 patients (23.40 %) had intracranial hematoma: subdural hematoma (n = 9), epidural hematoma (n = 1), intracerebral hematoma (n = 1), and subarachnoid hemorrhage (n = 3). One patient had subdural hematoma, epidural hematoma, intracerebral hematoma and subarachnoid hemorrhage. There were 31 patients had abnormal findings by the NIRS but only 11 patients had bleeding detected by the CT brain. There were 16 patients had negative results on both the NIRS and the CT brain. The sensitivity and specificity of the NIRS compared with the CT brain was 100 % and 44.4 %, respectively. The area under the ROC curve of the NIRS was 0.722. The median time to complete the NIRS examination was 3 min. In conclusion, the NIRS has high sensitivity and negative predictive value for intracranial hematoma detection in mild TBI patients with extra-axial hematomas.
Keywords: Sensitivity, Specificity, Predictive value, Likelihood ratio
1. Introduction
Traumatic brain injury (TBI) is a major public health issue worldwide. The incidence of TBI from a meta-analysis conducted on 28 epidemiological studies from 16 European countries was 262 per 100,000 for admitted TBI [1]. Road traffic, one of the causes of TBI, may cause injury in at least 50 million persons and kill 1.2 million persons annually [2]. Intracranial hematoma is a major cause of morbidity and mortality in TBI patients and required prompt treatment [3]. A non-contrast computed tomography (CT) of the brain is the main investigation for TBI individuals.
Even though CT scan of the brain is the gold standard for detecting intracranial abnormalities in TBI patients, it has several disadvantages including cost, radiation exposure, and availability. In developing countries [4], CT scan may not be available in all health care facilities and may need a referral to secondary or tertiary care hospitals. A portable near-infrared spectroscopy (NIRS) is a non-invasive device to detect intracranial hematoma [[5], [6], [7], [8]]. The advantages of the NIRS include real time results and non-radiation exposure.
The NIRS is a spectroscopy using the near-infrared region of the electromagnetic spectrum on molecular vibrations of various substances such as O—H in water, C—H in organics/oils and N—H in proteins. To detect intracranial hemorrhage, different light absorption in hemoglobin molecules in the brain is used to show hematoma [5]. The extravascular blood has a greater concentration of hemoglobin than intravascular blood resulting in more absorption of light and being an indicator of hematoma by the NIRS. The NIRS is a rapid, non-invasive, handheld device (Fig. 1). Typically, the brain scan by the NIRS can be performed completely in 3 min. Several studies showed that sensitivity and specificity of the NIRS for intracranial hematoma are varied [[5], [6], [7], [8]]. The sensitivity ranges from 68.70 % to 95.6 %, while the specificity varies from 78.60 % to 92.5 %. This study aimed to evaluate the diagnostic properties of the NIRS in TBI patients to detect intracranial hematoma.
Fig. 1.
A portable near-infrared spectroscopy (NIRS) components (A) and usage (B). Source: https://infrascanner.com/.
2. Methods
This study was a diagnostic and prospective study conducted at the Emergency Department. The inclusion criteria were adult patients (age of 18 years or over) with moderate to high risk of all degrees of traumatic brain injury within 24 h after the injury and willing to participate in the study. We excluded patients who had scalp lacerations or contusions or blood over the areas for the NIRS examination (Fig. 2), previous history of cranial surgery, shock or cardiac arrest. The study period was between January and October 2018.
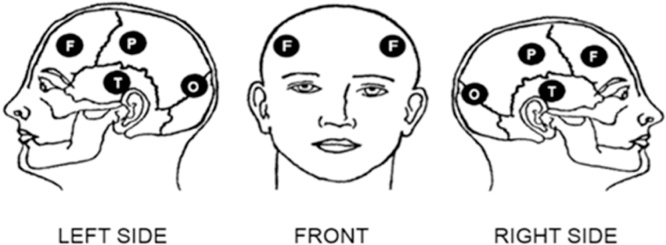
Fig. 2.
Areas of examinations for intracranial hematoma by a portable near-infrared spectroscopy (NIRS); F: frontal, P: parietal, T: temporal, O: occipital.
Study procedure. After the eligible patients gave an informed consent, the NIRS examination was performed and followed by the computed tomography of the brain. The NIRS was performed by the Infrascanner 2000 (Infrascan Inc., Philadelphia, USA), which was provided by the Supreme Products Co., LTd, Thailand. The Infrascanner measurements were performed in eight symmetrical anatomical points (frontal, temporal, parietal, and occipital) on the patient’s head (Fig. 2). The landmark of each area were as follows: frontal site: above the frontal sinus, below the hair line; temporal site: temporal fossa in front of the top of the ear; parietal site: midway between top of the ear and top of the skull; and occipital site: midway between top of the ear and the occipital protuberance. The NIRS is able to detect intracranial hematoma with volume of 3.5 mL and 3.5 cm from the skin surface. If the hematoma is present, the monitor will be red spot (Fig. 2). The NIRS in this study was performed by a trained emergency physician (CY). The CT brain was performed with a 128-slice scanner (Aquillon CX) at the ED using a conventional technique. The CT scans were a non-contrast study with 0.5 × 64 mm scan thickness from scalp to top of the C1 vertebrae. Both NIRS and CT brain results were blind to both the NIRS examiner and the radiologist. An example of the positive NIRS and CT brain was shown in Fig. 3.
Fig. 3.
Positive intracranial hemorrhage by a portable near-infrared spectroscopy (NIRS) confirmed by the CT brain.
Data collection. Baseline characteristics of all eligible patients were recorded. The Infrascanner exam data were collected on the results of the presence or absence hematoma, location of the hematoma, the difference in optical density (ΔOD) and time to complete the Infrascanner exam in minute. The CT brain results were recorded on type of hematoma (subdural hematoma, epidural hematoma, intracerebral hematoma; and subarachnoid hemorrhage), and the location of the hematoma.
Statistical analysis. The primary endpoint of the study was a description of diagnostic properties of the NIRS compared with the CT brain including sensitivity, specificity, positive predictive values (PPV), negative predictive values (NPV), likelihood ratio, area under the receiver operating characteristic (ROC) curve.
3. Results
There were 47 patients enrolled in the study. Of those, 11 patients (23.40 %) had abnormal CT brain findings; subdural hematoma (n = 9), epidural hematoma (n = 1), intracerebral hematoma (n = 1), and subarachnoid hemorrhage (n = 3). Note that one patient had subdural hematoma, epidural hematoma, intracerebral hematoma and subarachnoid hemorrhage. Those with positive and negative findings on CT brain were comparable in terms of age, hair thickness, mechanism of injury, and Glasgow Coma Scale (Table 1). Only the proportion of male sex was significantly higher in the positive CT brain group than the negative group (90.91 % vs 30.56 %; p value 0.001).
Table 1.
Baseline characteristics of patients with traumatic head injury categorized by CT brain results (n = 47).
| Factors | CT positive (n = 11) | CT negative (n = 36) | p value |
|---|---|---|---|
| Mean age (SD) | 64.36 (15.93) | 72.11 (19.63) | 0.240 |
| Male sex | 10 (90.91) | 11 (30.56) | 0.001 |
| Hair thickness | 0.290 | ||
| Normal | 5 (45.45) | 22 (61.11) | |
| Thin | 5 (45.45) | 14 (38.89) | |
| Thick | 1 (9.09) | 0 | |
| Mechanism of injury | 0.246 | ||
| Traffic accident | 2 (18.18) | 5 (13.89) | |
| Fall | 4 (36.36) | 23 (63.89) | |
| Others | 5 (45.45) | 8 (22.22) | |
| Glasgow Coma Scale | 0.275 | ||
| 15 | 10 (90.91) | 34 (94.44) | |
| 14 | 0 | 2 (5.56) | |
| <13 | 1 (9.09) | 0 |
The 2 × 2 table between the NIRS and CT brain was shown in Table 2. There were 31 patients had abnormal findings by the NIRS but only 11 patients had bleeding detected by the CT brain. There were 16 patients had negative results on both the NIRS and the CT brain. The sensitivity and specificity of the NIRS compared with the CT brain was 100 % and 44.4 %, respectively. Other diagnostic properties of the NIRS were shown in Table 3. The area under the ROC curve of the NIRS was 0.722 (Fig. 4). The median time to complete the NIRS examination was 3 min. The difference in optical density (ΔOD) in case of the NIRS positive was between 0.203 and 2.145.
Table 2.
A 2 × 2 table compared the results between a portable near-infrared spectroscopy (NIRS) and CT brain.
| CT |
Total | |||
|---|---|---|---|---|
| Positive | Negative | |||
| NIRS | Positive | 11 | 20 | 31 |
| Negative | 0 | 16 | 16 | |
| Total | 11 | 36 | 47 | |
Table 3.
Diagnostic properties of a portable near-infrared spectroscopy (NIRS) compared with the CT brain in patients with traumatic brain injury (n = 47).
| Factors | Values | 95 % confidence interval |
|---|---|---|
| Sensitivity | 100 | 71.90–100 |
| Specificity | 44.40 | 35.80–44.40 |
| Positive predictive value | 35.50 | 25.50–35.50 |
| Negative predictive value | 100 | 80.70–100 |
| Positive likelihood ratio | 1.80 | 1.12–1.80 |
| Negative likelihood ratio | 0 | 0–0.79 |
Fig. 4.
An ROC curve of a portable near-infrared spectroscopy (NIRS) compared with the CT brain.
4. Discussion
This study showed that the NIRS can be used to detect intracranial hematoma in TBI patients. The main advantage of the NIRS in this study is that if the negative NIRS, it has a low risk for intracranial hematoma and the CT brain may not be needed. As in this study, the majority of the TBI patients had GCS of 15 (93.61 %). The results of this study may imply that TBI patients with the GCS of 15 and require clinical observation may have advantages from the NIRS. Another situation that may be used the NIRS is the pre-hospital evaluation for the TBI patients.
Even though the sensitivity of the NIRS in this study is perfectly 100 %, it has the false positive of 20 patients. In other words, the positive predictive value was only 35.50 %. Therefore, there are 64.50 % of patients who have positive test on the NIRS do not have intracranial hematoma. However, due to the very high sensitivity (100 %) which was higher than previous studies [[5], [6], [7], [8]], the intracranial hematoma lesions would be detected by the NIRS. The majority of intracranial hematoma in this study were extra-axial hematoma (90.9 %; 9 patients with subdural hematoma and 1 patient with epidural hematoma).
The previous study showed that GCS is one important factor to detect intracranial hematoma in TBI patients [7]. All 13 patients with blunt or penetrating head injury who had the GCS of 3–12 had intracranial hematoma. Similarly, one patient in this study had the GCS of lower than or equal to 13 had intracranial hematoma (Table 1). For those with the GCS of 15 in this study, the intracranial hematoma was found in 90.91 % (Table 1). This number was quite higher than the previous report: only 44.44 % (32/72 patients) with the GCS of 13–15 had intracranial hematoma [8]. The different rates of intracranial hematoma of both studies may be from different study population. This current study had higher mean age (64.36 vs 55.5 years), and more proportion of male (90.91 % vs 69 %) than the previous study in those with intracranial hematoma. Additionally, the mechanism of injury is different: the majority of patients in this study had TBI from fall (36.36 %), while assualt was the main mechanism of injury in the previous study. Even though there are different rate of intracranial hematoma in TBI patients with the GCS of 15, the rate is quite high (44.44–90.91 %). These results may imply that those TBI should be investigated for intracranial hematoma even with the 15 GCS. And, the non-invasive NIRS may be a good option for this setting.
Even though the NIRS is a rapid, portable device for intracranial hemorrhage detection, it cannot report on size and exact location of the bleeding. Small sample size and characters of the study population are other limitations in this study. Even though the 95 % confidence interval are quite wide from small sample size (Table 3), the lower values are quite high for sensitivity and negative predictive value (71.90 % and 80.70 %). As previously discussed, the majority of the patients in this study had GCS of 15 and unilateral extra-axial hematoma. Therefore, further studies stratified by GCS and intracranial type with large sample size are needed. Note that the results of this study may not be applied for bilateral hematomas or chronic subdural hematomas. However, the results of this study may be useful for those mild TBI with required clinical observation. The NIRS may be a tool to save costs and times particularly in resource-limited setting to reduce numbers of referral patients to the higher-level health care facilities. Some factors were not evaluated [[9], [10], [11], [12]].
In conclusion, the NIRS has high sensitivity and negative predictive value for intracranial hematoma detection in mild TBI patients with extra-axial hematomas. The TBI patients may be screened for intracranial hematoma with the NIRS even with normal GCS. Those with negative results on the NIRS may do not require further CT brain imaging, while the positive NIRS is highly suggestive for intracranial hematoma. The NIRS may be useful particularly in the pre-hospital setting in well-trained emergency technicians.
CRediT authorship contribution statement
Chaiyaporn Yuksen: Conceptualization, Methodology, Formal analysis. Pungkawa Sricharoen: Data curation, Investigation. Nipa Puengsamran: Data curation, Investigation. Nitima Saksobhavivat: Data curation, Investigation. Yuwares Sittichanbuncha: Supervision. Kittisak Sawanyawisuth: Formal analysis, Writing - original draft, Writing - review & editing.
Declaration of Competing Interest
The authors have declared no conflict of interest.
Contributor Information
Chaiyaporn Yuksen, Email: chaipool0634@hotmail.com.
Pungkawa Sricharoen, Email: pungkawa@hotmail.com.
Nipa Puengsamran, Email: beau_friends@hotmail.com.
Nitima Saksobhavivat, Email: nitimasak@gmail.com.
Yuwares Sittichanbuncha, Email: yuwares.sit@mahidol.ac.th.
Kittisak Sawanyawisuth, Email: kittisak@kku.ac.th.
References
- 1.Peeters W., van den Brande R., Polinder S., Brazinova A., Steyerberg E.W., Lingsma H.F., Maas A.I. Epidemiology of traumatic brain injury in Europe. Acta. Neurochir (Wien) 2015;157:1683–1696. doi: 10.1007/s00701-015-2512-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cole T.B. Global road safety crisis remedy sought: 1.2 million killed, 50 million injured annually. JAMA. 2004;291:2531–2532. doi: 10.1001/jama.291.21.2531. [DOI] [PubMed] [Google Scholar]
- 3.Liang C.Y., Yang Y., Shen C.S., Wang H.J., Liu N.M., Wang Z.W., Zhu F.L., Xu R.X. Chinese military evaluation of a portable near-infrared detector of traumatic intracranial hematomas. Mil. Med. 2018;183:e318–e323. doi: 10.1093/milmed/usx088. [DOI] [PubMed] [Google Scholar]
- 4.Yuksen C., Sittichanbuncha Y., Patumanond J., Muengtaweepongsa S., Sawanyawisuth K. Clinical predictive score of intracranial hemorrhage in mild traumatic brain injury. Ther. Clin. Risk Manag. 2018;14:213–218. doi: 10.2147/TCRM.S147079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leon-Carrion J., Dominguez-Roldan J.M., Leon-Dominguez U., Murillo-Cabezas F., Infrascanner The. A handheld device for screening in situ for the presence of brain haematomas. Brain Inj. 2010;24:1193–1201. doi: 10.3109/02699052.2010.506636. [DOI] [PubMed] [Google Scholar]
- 6.Robertson C.S., Zager E.L., Narayan R.K., Handly N., Sharma A., Hanley D.F., Garza H., Maloney-Wilensky E., Plaum J.M., Koenig C.H., Johnson A., Morgan T. Clinical evaluation of a portable near-infrared device for detection of traumatic intracranial hematomas. J. Neurotrauma. 2010;27:1597–1604. doi: 10.1089/neu.2010.1340. PMID: 20568959. [DOI] [PubMed] [Google Scholar]
- 7.Xu L., Tao X., Liu W., Li Y., Ma J., Lu T., Han B., Liu B., Zhao Y., Li J., Zhao J. Portable near-infrared rapid detection of intracranial hemorrhage in Chinese population. J. Clin. Neurosci. 2017;40:136–146. doi: 10.1016/j.jocn.2017.02.056. [DOI] [PubMed] [Google Scholar]
- 8.Peters J., Van Wageningen B., Hoogerwerf N., Tan E. Near-infrared spectroscopy: a promising prehospital tool for management of traumatic brain injury. Prehosp. Disaster Med. 2017;32:414–418. doi: 10.1017/S1049023X17006367. [DOI] [PubMed] [Google Scholar]
- 9.Osakwe O., Owoh U.E., Oke S.A. An accident prevention model: case study of a small-scale wood workshop in a developing country. Asia. Pac. J. Sci. Technol. 2017;22 APST-22-03-01. [Google Scholar]
- 10.Albertsson P., Falkmer T. Is there a pattern in European bus and coach incidents? A literature analysis with special focus on injury causation and injury mechanisms. Accid. Anal. Prev. 2005;37:225–233. doi: 10.1016/j.aap.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 11.Wongwiriya P., Nakamura F., Tanaka S., Miura S., Ariyoshi R. User perception of paratransit in Thailand: case study of traveling to work in Khon Kaen city. Asia. Pac. J. Sci. Technol. 2017;22 APST-22-02-05. [Google Scholar]
- 12.Ohmori S., Yoshimoto K., Kuriyama S., Arunyanart S. Vehicle routing problem for freight forwarding. Asia. Pac. J. Sci. Technol. 2017;22 APST-22-02-02. [Google Scholar]