Abstract
Background
Obesity (OB) is a serious epidemic in the United States.
Methods
We examined OB patterns and time trends across socio-economic and geographic parameters and projected the future situation. Large national databases were used. Overweight (OW), OB and severe obesity (SOB) were defined using body mass index cut-points/percentiles; central obesity (CO), waist circumference cut-point in adults and waist:height ratio cutoff in youth. Various meta-regression analysis models were fit for projection analyses.
Results
OB prevalence had consistently risen since 1999 and considerable differences existed across groups and regions. Among adults, men’s OB (33.7%) and OW (71.6%) levelled off in 2009–2012, resuming the increase to 38.0 and 74.7% in 2015–2016, respectively. Women showed an uninterrupted increase in OB/OW prevalence since 1999, reaching 41.5% (OB) and 68.9% (OW) in 2015–2016. SOB levelled off in 2013–2016 (men: 5.5–5.6%; women: 9.7–9.5%), after annual increases of 0.2% between 1999 and 2012. Non-Hispanic Blacks had the highest prevalence in women’s OB/SOB and men’s SOB. OB prevalence in boys rose continuously to 20.6% and SOB to 7.5% in 2015–2016, but not in girls. By 2030, most Americans will be OB/OW and nearly 50% of adults OB, whereas ∼33% of children aged 6–11 and ∼50% of adolescents aged 12–19 will be OB/OW. Since 1999, CO has risen steadily, and by 2030 is projected to reach 55.6% in men, 80.0% in women, 47.6% among girls and 38.9% among boys. Regional differences exist in adult OB prevalence (2011–2016) and across ethnicities; South (32.0%) and Midwest (31.4%) had the highest rates.
Conclusions
US obesity prevalence has been rising, despite a temporary pause in 2009–2012. Wide disparities across groups and geographical regions persist. Effective, sustainable, culturally-tailored interventions are needed.
Keywords: Obesity, overweight, central obesity, body mass index, trend, projection
Key Messages
The prevalence of obesity in the USA has been heralded as having levelled off in the early 2010s. However, obesity prevalence has consistently risen since 1999, despite a temporary pause in 2009–2012.
Considerable differences in obesity/overweight rates existed across sex, race/ethnicity, socio-economic status and regions in the USA.
By 2030, 78% of American adults are projected to be overweight or obese.
Continuous effective intervention efforts are needed to fight the obesity epidemic and reduce disparities in obesity across socio-demographic groups and geographical regions.
Introduction
The global obesity (OB) epidemic stems from lifestyle, health-related and environmental factor changes, including poor eating and sedentary behaviours.1,2 Following cigarette smoking, it is the second leading cause of preventable deaths in the USA.3 Fighting the US OB epidemic has entailed over a decade’s worth of efforts and programmes.4
Twelve years ago in 2007, using national data we described time trends in obesity and overweight (OB/OW) prevalence, and highlighted disparities across sex, age, racial/ethnic groups, socio-economic status (SES) and US geographic regions.5 We also projected a continuous increase in OB, and by 2015, 75% of US adults would have OB/OW and 41% would have OB. Notwithstanding effective interventions, we expected by 2015, OB/OW might contribute to 17% of total health-care costs.6 Indeed, our 2007 projection of OB/OW and OB matched closely with the recently observed prevalence for 2015–2016 (75 vs 72% for OB/OW; 41 vs 40% for OB).
There are some controversies around whether in recent years US OB/OW prevalence has levelled off or not,7–11 whereas an upward decade-long trend in both OB and SOB prevalence has been reported.12 Also, existing research has mainly relied on using body mass index (BMI) to describe the trends of OB/OW and failed to project future trends of OB,12 whereas waist circumference (WC) [used to classify central obesity (CO)] reflects visceral adipose tissue and is a better predictor of obesity related health risks than BMI. Given significant time passing, lingering controversies and limited research in our field, updating our prediction published in 20075 with recent data is necessary. Such findings will be useful for helping develop better-targeted future interventions.
Our study comprehensively examines the US OB/OW epidemic based on recent, nationally-representative data collected since 1999. It describes the current situation, time trends and disparities across sex, age, racial/ethnic groups, SES and US geographic regions. The study also includes projections up to the year 2030, that are then contrasted to findings from our 2007 published study.5
Methods
Nationally-representative data
We used biennial data of the National Health and Nutrition Examination Survey (NHANES) in 1999–2016, which is a series of cross-sectional, nationally representative surveys conducted by the National Center for Health Statistics. Anthropometrics were measured through direct physical examination in a mobile examination centre and analysed in this study.13
The Behavioral Risk Factor Surveillance System (BRFSS) is an ongoing series of national telephone surveys collecting behavioural and health-related data since 1984. BRFSS data through 2016 provided us state-specific information on OB/OW using self-reported weight and height and enabled geographic difference analysis on OB/OW.14,15
Definitions of overweight and obesity
The World Health Organization (WHO) currently defines adult OB/OW, and the National Health, Lung, and Blood Institute classifies severe obesity (SOB), by using BMI (weight/height-squared, kg/m2) cut-points of 25, 30 and 40, respectively.1,16 Among youth (2–19 years), the 2000 CDC Growth Charts specifying age-sex-specific BMI percentiles17 define OW, OB and SOB by 85th, 95th17–20 and 120% of the 95th percentile, or BMI ≥ 35 kg/m2, whichever is lower.20
The American Heart Association/National Heart, Lung, and Blood Institute defines CO at WC cut-points of >40 inches (>102 cm) for men and >35 inches (>88 cm) for women.21 With no standard recommendations, CO for youth was defined as a WC:height ratio (WhtR) >0.5.22,23 Reflecting visceral fat stores, WC is a better predictor of OB-related metabolic disorders than BMI.24
Statistical analysis
Using regression-based analyses, patterns and trends in key adiposity measures among adults and youth were examined. NHANES 1999–2014 were used for most projections and 2015–2016 data for currently-observed rates.
First, we estimated means of adult WC and youth WhtR, and prevalence of OB, OW, SOB and CO across all available years. The primary stratifying variables were sex and age group (adults: 20 years+; youth: 2–5 years, 6–11 years and 12–19 years). The next level stratification was made by ethnicity [non-Hispanic (NH) White, NH Black, Mexican-American, and Other), educational attainment (<high school, high school, >high school) and poverty-income ratio (PIR) category (<100%, 100–200%, >200%). Survey sampling complexity was accounted for with wave-specific primary sampling units, strata and 2-year weights.
Second, after compiling wave-specific estimates for 1999–2016, we selected years up to 2014 (8 data-points) to project overall and stratum-specific estimates for the years 2015, 2020 and 2030, using linear meta-regression models,25 with study year (mid-wave) as the sole predictor. The underlying assumption was that means and proportion would continue to increase or decrease at the annual rate without any non-linear components over time. Thus, in the main analysis, beta coefficients reflected average annual changes in binary outcome prevalence (OB, OB/OW, SOB, CO), and annual changes in BMI, WC and WhtR. Projections accounted for the standard error around each wave-specific point estimate.25 For validation purposes, we compared the model projections with those from our previous study using 1978–2004 NHANES data5 and with actual NHANES 2015–16 data.
In addition for sensitivity analysis, we fit new non-linear models by adding a squared term for year to the linear model (centering year at 2000) and re-projected the years 2015–30 for all outcomes of interest and all strata. Model fit comparison between the linear and non-linear model was assessed using the Bayesian information criterion (BIC: the lower, the better the fit), which penalizes the model for the number of terms included, using the ordinary least square version of the model (rather than meta-regression). Specifically, for models with a significant quadratic term at a type I error of 0.10, BIC was compared with the linear model within each socio-demographic group (among both adults and the youth) and outcome of interest, with >2 points reduction in BIC between linear and non-linear models indicating significant improvement in model fit.26 For models whereby the quadratic term was not statistically significant, no model comparison was made and the linear model seemed to fit better.
Finally, a second sensitivity analysis was conducted whereby logistic regression models were fit using machine learning techniques, mainly adaptive least absolute shrinkage and selection operator (LASSO), to select the best fitting model taking into account year, year2 and the interaction terms between year, sex and other covariates (age, race/ethnicity, education and poverty income ratio groups). From selected models for each outcome of interest, stratum-specific projected values of prevalence for each of 2015, 2020 and 2030, adjusting for key covariates, were obtained along with 95% confidence intervals (CIs). Detailed description of the methodology is provided in Supplementary Method 1, available as Supplementary data at IJE online. Sample sizes for each stratum and year are presented in Supplementary Table S4, available as Supplementary data at IJE online.
Geographic and ethnic differences in OB were described using BRFSS data. All analyses were conducted using Stata release 16.0 software.16
Results
Secular trends in US adult obesity/adiposity, with 2030 projections
Table 1 and Fig. 1 display key findings for adults, in terms of secular trends and projections of OB and other related outcomes based on NHANES1999–2015. A levelling off in OB rates among men between 2009–2010 (35.3%) and 2011–2012 (33.7%) was observed, followed by a resumption of increase beyond 2013. In contrast, women’s OB rates showed a steady increase since 1999, reaching 41.5% in 2015–2016. Despite men experiencing a faster annual rate of increase (ß±SE = 0.61 ± 0.10, P < 0.001 vs ß±SE = 0.47 ± 0.11, P < 0.01: 1999–2014), women consistently exhibited higher OB and SOB prevalence than men.
Table 1.
Trends in the observed 1999–2014 and projected 2020 and 2030 prevalence (%) of obesity, severe obesity and combined overweight and obesitya among US adults, by gender, ethnicity, level of education and poverty to income ratio: based on data from National Health and Nutrition Examination Survey (NHANES) 1999–2014b. PIR indicates ratio of income to the family’s appropriate poverty threshold set by the US Census Bureau in a given calendar year. The Census Bureau, working in accordance with the Statistical Policy Directive of the Office of Management and Budget, use a set of money income thresholds that vary by family size and composition to determine who is poor. Thresholds were updated annually for inflation by using the consumer price index
| Men |
Women |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Annual increase rateb |
Projected prevalence in 2020 (95% CI) | Projected prevalence in 2030 (95% CI) | Annual increase rateb |
Projected prevalence in 2020 (95% CI) | Projected prevalence in 2030 (95% CI) | |||||||||||||
| β | SE | P | β | SE | P | |||||||||||||
| Obesity (BMI ≥30 kg/m2) | ||||||||||||||||||
| All (Age≥ 20) | 0.61 | 0.10 | *** | 39.6 | 36.4 | 42.8 | 45.7 | 40.2 | 51.2 | 0.47 | 0.11 | ** | 41.8 | 38.1 | 45.4 | 46.5 | 40.1 | 52.8 |
| By ethnicity | ||||||||||||||||||
| NH White | 0.53 | 0.12 | ** | 38.9 | 34.8 | 43.0 | 44.2 | 37.3 | 51.1 | 0.53 | 0.13 | ** | 40.3 | 35.7 | 45.0 | 45.6 | 37.8 | 53.4 |
| NH Black | 0.90 | 0.20 | ** | 46.1 | 39.1 | 53.2 | 55.1 | 43.4 | 66.8 | 0.59 | 0.23 | * | 60.4 | 52.7 | 68.1 | 66.3 | 53.2 | 79.4 |
| Mexican- American | 1.30 | 0.36 | * | 51.0 | 38.0 | 63.8 | 64.1 | 42.6 | 85.7 | 1.00 | 0.26 | ** | 56.0 | 47.5 | 64.5 | 66.0 | 51.2 | 80.8 |
| Others | 0.46 | 0.28 | 31.3 | 21.9 | 40.7 | 35.9 | 19.9 | 51.8 | −0.15 | 0.29 | 25.7 | 16.5 | 34.8 | 24.2 | 8.2 | 40.1 | ||
| By education | ||||||||||||||||||
| <High school | 0.70 | 0.26 | * | 38.3 | 29.2 | 47.4 | 45.3 | 29.9 | 60.6 | 0.81 | 0.30 | * | 48.6 | 38.7 | 58.5 | 56.8 | 39.8 | 73.7 |
| High school | 0.82 | 0.32 | * | 42.2 | 30.6 | 53.8 | 50.4 | 31.1 | 69.6 | 0.17 | 0.24 | 45.3 | 37.5 | 53.2 | 47.0 | 33.4 | 60.6 | |
| >High school | 0.59 | 0.12 | ** | 39.7 | 35.8 | 43.7 | 45.7 | 39.0 | 52.4 | 0.54 | 0.13 | ** | 41.5 | 37.4 | 45.5 | 46.9 | 39.8 | 54.0 |
| By PIR | ||||||||||||||||||
| <100%PIR | 0.43 | 0.21 | 33.3 | 26.0 | 40.6 | 37.6 | 25.4 | 49.8 | 0.49 | 0.18 | * | 48.3 | 42.1 | 54.4 | 53.2 | 42.6 | 63.7 | |
| 100–200% PIR | 0.80 | 0.20 | ** | 42.1 | 35.3 | 48.9 | 50.1 | 38.6 | 61.6 | 0.76 | 0.31 | * | 50.5 | 40.0 | 61.0 | 58.1 | 40.3 | 75.9 |
| >200% PIR | 0.63 | 0.16 | ** | 40.9 | 35.2 | 46.5 | 47.2 | 37.6 | 56.7 | 0.39 | 0.15 | * | 37.5 | 32.3 | 42.7 | 41.4 | 32.6 | 50.2 |
| Severe obesity (BMI ≥40 kg/m2) | ||||||||||||||||||
| All (Age ≥20) | 0.17 | 0.04 | ** | 6.2 | 4.7 | 7.7 | 7.9 | 5.4 | 10.5 | 0.22 | 0.06 | ** | 10.5 | 8.3 | 12.6 | 12.7 | 9.1 | 16.2 |
| By ethnicity | ||||||||||||||||||
| NH White | 0.15 | 0.06 | * | 5.8 | 3.8 | 7.9 | 7.3 | 3.9 | 10.7 | 0.23 | 0.06 | * | 9.8 | 7.4 | 12.1 | 12.1 | 8.2 | 15.9 |
| NH Black | 0.31 | 0.08 | ** | 10.1 | 7.3 | 12.8 | 13.2 | 8.6 | 17.7 | 0.31 | 0.13 | 19.1 | 14.5 | 23.7 | 22.2 | 14.4 | 30.0 | |
| Mexican-American | 0.24 | 0.09 | * | 6.8 | 3.4 | 10.2 | 9.3 | 3.8 | 14.8 | 0.20 | 0.10 | 9.8 | 6.1 | 13.6 | 11.9 | 5.7 | 18.0 | |
| Others | 0.08 | 0.11 | 3.4 | 0.0 | 6.8 | 4.2 | 0c | 10.1 | 0.05 | 0.11 | 5.7 | 2.3 | 9.1 | 6.2 | 0.1 | 12.3 | ||
| By education | ||||||||||||||||||
| <High school | 0.16 | 0.12 | 4.5 | 0.1 | 8.9 | 6.1 | 0.0c | 13.3 | 0.39 | 0.11 | ** | 10.3 | 6.3 | 14.4 | 14.2 | 7.6 | 20.8 | |
| High school | 0.08 | 0.13 | 5.2 | 0.8 | 9.7 | 6.0 | 0.0c | 13.5 | 0.09 | 0.13 | 9.8 | 5.3 | 14.2 | 10.7 | 3.2 | 18.2 | ||
| >High school | 0.17 | 0.05 | * | 6.3 | 4.7 | 7.9 | 8.1 | 5.3 | 10.8 | 0.20 | 0.06 | * | 10.0 | 7.9 | 12.2 | 12.1 | 8.4 | 15.7 |
| By PIR | ||||||||||||||||||
| <100%PIR | −0.004 | 0.14 | 3.3 | 0.0c | 7.8 | 3.2 | 0.0c | 11.0 | 0.29 | 0.14 | 14.2 | 9.6 | 18.7 | 17.1 | 9.3 | 25.0 | ||
| 100–200% PIR | 0.36 | 0.10 | ** | 10.2 | 6.4 | 14.1 | 13.8 | 7.6 | 20.0 | 0.36 | 0.13 | * | 13.5 | 8.8 | 18.2 | 17.1 | 9.2 | 24.9 |
| >200% PIR | 0.15 | 0.06 | * | 5.7 | 3.7 | 7.8 | 7.3 | 3.9 | 10.7 | 0.19 | 0.08 | * | 8.9 | 6.2 | 11.6 | 10.8 | 6.3 | 15.3 |
| Combined overweight and obesity (BMI ≥ 25 kg/m2) | ||||||||||||||||||
| All (Age≥ 20) | 0.40 | 0.09 | ** | 76.9 | 73.6 | 80.2 | 81.0 | 75.4 | 86.5 | 0.48 | 0.11 | ** | 70.2 | 66.5 | 73.9 | 74.9 | 68.6 | 81.2 |
| By ethnicity | ||||||||||||||||||
| NH Whitec | 0.40 | 0.11 | ** | 78.1 | 74.2 | 82.0 | 82.1 | 75.7 | 88.6 | 0.64 | 0.14 | ** | 69.6 | 64.9 | 74.2 | 76.0 | 67.9 | 84.0 |
| NH Blackc | 0.63 | 0.26 | 75.4 | 66.4 | 84.5 | 81.7 | 66.4 | 97.1 | 0.35 | 0.15 | 84.0 | 78.7 | 89.3 | 87.5 | 78.6 | 96.3 | ||
| Mexican-American | 1.10 | 0.20 | ** | 90.8 | 84.2 | 97.3 | 100c | 90.2 | 100c | 0.98 | 0.21 | ** | 88.2 | 81.4 | 95.0 | 98.0 | 86.2 | 100c |
| Others | −0.12 | 0.24 | 63.1 | 55.4 | 70.7 | 61.9 | 48.7 | 75.1 | −0.67 | 0.40 | 48.7 | 35.2 | 62.3 | 42.1 | 18.9 | 65.2 | ||
| By education | ||||||||||||||||||
| <High school | 0.69 | 0.29 | 80.9 | 71.1 | 90.7 | 87.8 | 71.1 | 100c | 0.51 | 0.27 | 80.9 | 71.5 | 90.4 | 86.0 | 70.2 | 100c | ||
| High school | 0.51 | 0.37 | 74.9 | 62.4 | 87.5 | 80.0 | 58.7 | 100c | 0.17 | 0.25 | 73.7 | 65.2 | 82.1 | 75.3 | 61.1 | 89.6 | ||
| >High school | 0.35 | 0.13 | * | 77.0 | 72.3 | 81.6 | 80.5 | 72.7 | 88.2 | 0.60 | 0.12 | ** | 69.8 | 66.0 | 73.7 | 75.8 | 69.2 | 82.5 |
| By poverty income ratio | ||||||||||||||||||
| <100%PIR | 0.21 | 0.35 | 65.5 | 53.2 | 77.8 | 67.6 | 46.9 | 88.3 | 0.70 | 0.16 | ** | 76.9 | 71.2 | 82.6 | 83.9 | 74.3 | 93.5 | |
| 100–200% PIR | 0.71 | 0.21 | * | 77.1 | 70.2 | 83.9 | 84.1 | 72.3 | 95.9 | 0.76 | 0.15 | ** | 79.1 | 73.9 | 84.3 | 86.7 | 77.9 | 95.5 |
| >200% PIR | 0.45 | 0.13 | * | 80.3 | 75.5 | 85.1 | 84.8 | 76.8 | 92.7 | 0.36 | 0.16 | 65.5 | 60.3 | 70.8 | 69.1 | 60.2 | 78.0 | |
P < 0.001, **P < 0.01, *P < 0.05.
We used the World Health Organization (WHO) BMI cut points for overweight and obesity and the US National Health, Lung, and Blood Institute BMI cut point for extreme obesity, BMI ≥25, 30 and 40 kg/m2, respectively.
Linear meta-regression models with year as the sole predictor was used to estimate annual increase rate and to project prevalence for the years of 2020 and 2030, overall and for each stratum by gender and ethnic groups based on the NHANES 1999–2014 data.
We truncated the prevalence and their 95% CI at 100 if they were >100%, and at 0 if they were <0, and indicated imprecise projection for those numbers.
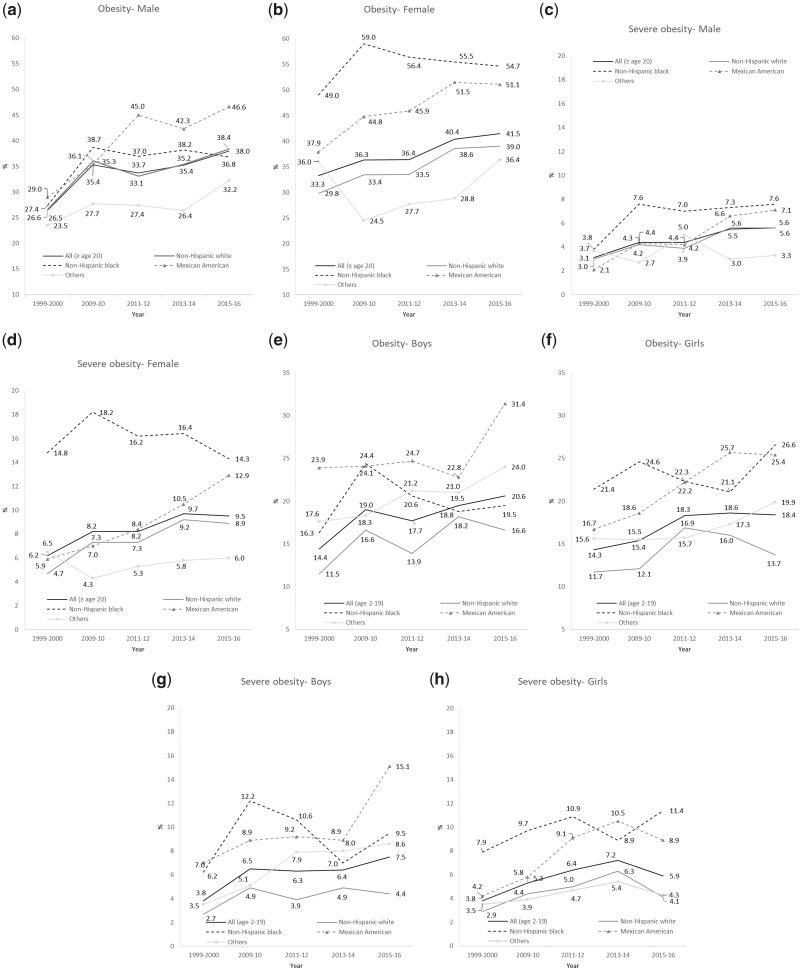
Figure 1.
Secular trends in the prevalence (%) of obesity and severe obesity in US adults (≥20 years old) and youth (2–19 years old) by sex and ethnicity, National Health and Nutrition Examination Survey 1999–2016. The World Health Organization (WHO) defines adult obesity and the National Health, Lung, and Blood Institute classified extreme obesity by using BMI cut points of 30 and 40 kg/m2, respectively. Childhood obesity [(BMI ≥95th percentile), and severe obesity (BMI ≥120% of the 95th percentile, or BMI ≥35kg/m2, whichever was lower] were defined by the age-sex-specific BMI percentile in the 2000 Centers for Disease Control and Prevention growth charts. Analysis was stratified by sex and ethnicity for each age group, without adjusting for other socio-demographic groups, taking into account sampling design complexity.
This sharp OB increase was restricted to NH Whites and Mexican-American women, unlike NH Blacks whose OB prevalence may have reached saturation earlier (58.5% in 2009–10). Projecting 1999–2014 estimates into the future, 46–47% of US adults overall will be obese by 2030 without interventions.
SOB showed interesting patterns, whereby its annual rate of increase was about 0.2% between 1999 and 2014, although its prevalence has levelled off between 2013–14 and 2015–16 (men: 5.5% and 5.6%; women: 9.7% and 9.5%), following that linear increase. Women experienced substantially higher SOB prevalence than men, reaching 9.5% in 2015–2016 (Fig. 1). It is expected that by 2030, 10% of all adults will have SOB (95% CI: 7.7–12.4%), with a women:men ratio of 1.6. NH Black adults had the highest SOB prevalence.
Since 1999, over two-thirds of US adults have been OB/OW, though the OB/OW prevalence trend may have levelled off between 2009 and 2014 among men (74.0%), unlike women whose OB/OW increasing trend remained linear (annual increase rate: women: ß±SE = +0.48 ± 0.11 vs men: +0.40 ± 0.09, all P < 0.01). Further, 81.0% of men and 74.9% of women, and almost all Mexican-Americans (100% of men and 98% of women), are projected to become OB/OW by 2030.
Demographic and socio-economic disparities in US adult adiposity, with 2030 projections
As Table 1 indicates, continuous increases were seen in all binary adiposity measures. Mexican men (ß±SE = 1.30 ± 0.36, P < 0.01) and women (ß±SE = 1.00 ± 0.26, P < 0.01) had the highest annual rate of increase in OB. Furthermore, Mexican-American men (46.6%) and NH Black women (54.7%) exhibited the highest recent OB prevalence in 2015–2016 (Fig. 1). NH Black adults continued to have an exceptionally high prevalence of SOB compared with other ethnic groups since 2009–2010, although NH Black women’s SOB prevalence dropped by 3.9% between 2009–2010 and 2015–2016 (Fig. 1). As stated earlier, Mexican-American men had the fastest annual increase in OB with OB prevalence projected to reach 64.1% by 2030 (Table 1). Despite this, the highest projected 2030 OB prevalence was found among NH Black women (66.3%) (Table 1).
Moreover, most binary adiposity measures were lowest in the >200% PIR group, despite a consistently high annual rate of increase for the 100–200% PIR category. In 2030, SOB prevalence in men within the 100–200% PIR category is projected to reach 13.8%, a major disparity with other income groups (vs <100% PIR: 3.2%, >200% PIR: 7.3%). The annual rate of increase in OB among women was highest within the <high school education category (ß±SE = 0.81 ± 0.30, P < 0.05), a pattern noted for SOB as well (ß±SE = 0.39 ± 0.11, P = 0.01), compared with women in higher educational groups.
The results of the first sensitivity analysis indicated that for most outcomes and strata, there was no added benefit to including a squared year term to the linear year term in our models. In fact, for the outcome of obesity prevalence among adults of all ages and other socio-demographic groups combined, adding a squared year term to the model lead to a higher BIC. On the other hand, when the quadratic term (year2) was statistically significant at a type I error of 0.10 (∼21 models), the non-linear model had for the most part a better fit than its linear counterpart, except for 3 models whereby added benefit was not significant. For the remaining 18 models, non-linearity was assumed and detailed results were shown in Supplementary Table S1, available as Supplementary data at IJE online. For most socio-demographic groups, most consistently NH Black men, year > 0 was combined with year2 < 0 and thus, the non-linear pattern manifested itself with an increasing trend that was levelling off with time. This was not the case among women of other racial/ethnic groups (year < 0, year2 > 0),
In the second sensitivity analysis with logistic regression models selected using adaptive LASSO techniques, confidence bounds were restricted to 0–100% and most of the findings were more conservative in terms of projected prevalence of binary outcomes (Supplementary Table S2, available as Supplementary data at IJE online), even though general patterns were preserved. In fact, the highest prevalence of OB, OB/OW, SOB and CO were found among minority groups, lower SES categories and among women. Most notably, NH Black women are expected to have the highest OB and SOB by 2030 with non-overlapping 95% CI compared with NH White women.
Youth adiposity trends during 1999–2016 in the US, with 2030 projections
Overall, youth OB and SOB prevalence were similar across sexes (1999–2014). Whereas OB and SOB prevalence proportions have continued to increase among boys (Fig. 1), for girls, prevalence reached a plateau between 2013–14 and 2015–16 (OB: 18.4%, SOB: 5.9%, 2015–16). Among boys, the highest OB/SOB prevalence proportions were found among NH Blacks between 2009 and 2012, though this distinction went to Mexican-American boys by 2015–16. For girls, NH Blacks generally had the highest OB/SOB prevalence proportions (OB: 26.6%; SOB: 11.4%: 2015–2016).
Compared with children (aged 6–11), adolescents (aged 12–19) had consistently higher prevalence proportions and rates of increase in OB, SOB and OB/OW. Among children, girls had a greater annual increase in OB (0.45 vs 0.25), SOB (0.17 vs 0.13) and OB/OW (0.61 vs 0.05) than boys. Among adolescents (aged 12–19), boys had higher rates of increase than girls in OB (0.46 vs 0.35) and OB/OW (0.61 vs 0.45; Table 2). The highest rate of annual increase was among younger girls (aged 6–11 years: β±SE = 0.61 ± 0.28) and adolescent boys (aged 12–19 years: β±SE = 0.61 ± 0.17) for OB/OW. About 39% of children and 46% of adolescents were projected to become OB/OW by 2030.
Table 2.
Comparisons of observed actual prevalence (%) in 2015–2016 vs our 2007 study projected prevalence for 2015, and projections for 2015, 2020 and 2030 prevalence (%) of obesity, severe obesity and combined overweight and obesity among adults (age ≥20 years), children (age 6–11 years) and adolescents (age 12–19 years) in the US by gender using the National Health and Nutrition Examination Survey (NHANES) 1999–2016 dataa,b
| Gender | Actual prevalence in 2015–16 | Our 2007 study projection for 2015c | Annual increase rated |
Projected 2015d |
Projected 2020d |
Projected 2030d |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | P | Prevalence (95% CI) | Prevalence (95% CI) | Prevalence (95% CI) | ||||||||||
| Adults (age ≥20) | |||||||||||||||
| Obesity (BMI≥30kg/m2) | All | 39.8 | 40.8 | 0.57 | 0.09 | *** | 38.5 | 36.6 | 40.4 | 40.3 | 38.5 | 44.2 | 47.1 | 42.1 | 52.0 |
| Men | 38.0 | 37.3 | 0.61 | 0.10 | *** | 36.6 | 34.4 | 38.7 | 39.6 | 36.4 | 42.8 | 45.7 | 40.3 | 51.2 | |
| Women | 41.5 | 46.4 | 0.47 | 0.11 | ** | 39.4 | 37.0 | 41.8 | 41.8 | 38.1 | 45.4 | 46.5 | 40.1 | 52.9 | |
| Severe obesity (BMI≥40kg/m2) | All | 7.6 | 7.4 | 0.18 | 0.04 | ** | 7.3 | 6.4 | 8.2 | 8.2 | 6.8 | 9.6 | 10.0 | 7.7 | 12.4 |
| Men | 5.6 | 5.3 | 0.17 | 0.04 | ** | 5.4 | 4.4 | 6.4 | 6.2 | 4.7 | 7.7 | 7.9 | 5.4 | 10.5 | |
| Women | 9.5 | 9.5 | 0.22 | 0.06 | ** | 9.4 | 7.9 | 10.8 | 10.5 | 8.3 | 12.6 | 12.7 | 9.1 | 16.2 | |
| Combined overweight & obesity (BMI≥25kg/m2) | All | 71.7 | 74.7 | 0.45 | 0.08 | *** | 71.3 | 69.4 | 73.1 | 73.5 | 70.8 | 76.2 | 78.0 | 73.5 | 82.4 |
| Men | 74.7 | 76.8 | 0.40 | 0.09 | ** | 74.9 | 72.6 | 77.2 | 76.9 | 73.6 | 80.3 | 81.0 | 75.4 | 86.5 | |
| Women | 68.9 | 73.6 | 0.48 | 0.11 | ** | 67.8 | 65.3 | 70.3 | 70.2 | 66.5 | 73.9 | 74.9 | 68.6 | 81.3 | |
| Children (Age 6–11) | |||||||||||||||
| Obesity (BMI ≥95th percentile) | All | 20.4 | 22.7 | 0.27 | 0.11 | 19.8 | 17.7 | 22.0 | 21.2 | 18.0 | 24.4 | 23.9 | 18.5 | 29.3 | |
| Boys | 22.8 | 23.3 | 0.25 | 0.18 | 20.9 | 17.7 | 24.1 | 22.2 | 17.4 | 27.0 | 24.6 | 16.5 | 32.8 | ||
| Girls | 17.9 | 21.8 | 0.45 | 0.24 | 20.4 | 16.0 | 24.9 | 22.7 | 16.1 | 29.3 | 27.2 | 16.1 | 38.3 | ||
| Severe obesityb | All | 7.1 | – | 0.15 | 0.10 | 6.3 | 4.4 | 8.2 | 7.1 | 4.3 | 9.9 | 8.6 | 3.9 | 13.4 | |
| Boys | 7.9 | – | 0.13 | 0.11 | 6.5 | 4.4 | 8.5 | 7.1 | 4.1 | 10.1 | 8.4 | 3.4 | 13.4 | ||
| Girls | 6.3 | – | 0.17 | 0.09 | 5.7 | 3.5 | 8.0 | 6.6 | 3.3 | 9.8 | 8.3 | 2.8 | 13.7 | ||
| Combined overweight & obesity (BMI ≥ 85th percentile) | All | 36.5 | – | 0.24 | 0.21 | 35.3 | 31.7 | 38.9 | 36.5 | 31.0 | 42.0 | 38.8 | 29.4 | 48.3 | |
| Boys | 38.2 | – | 0.05 | 0.23 | 33.8 | 30.0 | 37.6 | 34.1 | 28.1 | 40.0 | 34.6 | 24.2 | 45.0 | ||
| Girls | 34.8 | – | 0.61 | 0.28 | 38.3 | 33.1 | 43.5 | 41.4 | 33.7 | 49.1 | 47.5 | 34.5 | 64.4 | ||
| Adolescents (age 12–19) | |||||||||||||||
| Obesity (BMI ≥95th percentile) | All | 21.8 | 23.6 | 0.42 | 0.11 | ** | 22.3 | 19.3 | 25.3 | 24.4 | 20.2 | 28.6 | 28.6 | 21.8 | 35.4 |
| Boys | 21.8 | 23.7 | 0.46 | 0.14 | * | 23.2 | 19.3 | 27.2 | 25.5 | 19.9 | 31.1 | 30.1 | 21.1 | 39.1 | |
| Girls | 21.7 | 21.0 | 0.35 | 0.14 | * | 20.9 | 17.2 | 24.6 | 22.6 | 17.3 | 28.0 | 26.2 | 17.6 | 34.7 | |
| Severe obesityb | All | 8.9 | – | 0.28 | 0.07 | ** | 9.6 | 7.7 | 11.4 | 10.9 | 8.3 | 13.6 | 13.7 | 9.4 | 18.0 |
| Boys | 10.3 | – | 0.24 | 0.09 | * | 9.4 | 7.0 | 11.8 | 10.6 | 7.2 | 14.0 | 13.0 | 7.4 | 18.6 | |
| Girls | 7.4 | – | 0.26 | 0.09 | * | 9.1 | 6.7 | 11.5 | 10.4 | 7.1 | 13.8 | 13.1 | 7.7 | 18.5 | |
| Combined overweight and obesity (BMI ≥85th percentile) | All | 41.3 | – | 0.49 | 0.13 | ** | 38.1 | 34.8 | 41.5 | 40.6 | 35.8 | 45.4 | 45.5 | 37.5 | 53.5 |
| Boys | 37.9 | – | 0.61 | 0.17 | ** | 40.2 | 36.2 | 44.2 | 43.2 | 37.4 | 49.1 | 49.3 | 39.6 | 59.1 | |
| Girls | 44.9 | – | 0.45 | 0.20 | 37.6 | 32.5 | 42.8 | 39.9 | 32.4 | 47.4 | 44.4 | 32.1 | 56.7 | ||
P < 0.001, **P < 0.01, *P < 0.05.
The World Health Organization (WHO) defines adult overweight and obesity and the National Health, Lung, and Blood Institute classified extreme obesity by using BMI cut points of 25, 30 and 40 kg/m2, respectively.
Childhood overweight (BMI ≥ 85th percentile), obesity (BMI ≥ 95th percentile) and severe obesity (BMI ≥ 120% of the 95th percentile, or BMI ≥ 35 kg/m2, whichever was lower) were defined by the age-sex-specific BMI percentile in the 2000 CDC growth charts.
Our old estimation in obesity, overweight and severe obesity in 2015 were from our previous projection in 2007 (Wang and Beydoun5 which used NHANES 1976 to 2004 data and linear regression models with year per age, gender, ethnic stratum as a function of time as the independent variable.
Linear meta-regression models with year as the sole predictor was used to estimate annual increase rate and project prevalence proportions for the years 2020 and 2030 overall and for each stratum by gender and ethnic groups based on NHANES 1999–2014 data.
In our first sensitivity conducted for the youth, only one model fit the description whereby year < 0 and year2 > 0 (SOB, Mexican-Americans, 12–19 years), though the linear pattern was assumed due to no appreciable difference in BIC between the alternative models. In the second sensitivity analysis (Supplementary Table S3, available as Supplementary data at IJE online), Mexican-American girls of all ages combined (2–19 years) appear to have the largest projected prevalence of OB (35.6, 95% CI: 24.3–48.7), OB/OW (52.0, 95% CI: 43.6–60.3) and SOB (20.9, 95% CI: 11.1–35.7) in 2030 with little overlap in terms of 95% CI compared with NH White girls in the same age group. No significant differences were observed by gender within each of the age groups 6–11 or 12–19 years. This was consistent with the findings from the linear meta-regression analysis.
Central adiposity in US adults and youth; with 2030 projections
Table 3 indicates that among adults, CO has increased over time (annual increase rate: 0.56% in men and 0.75% in women) reaching 46.1 and 67.8% in 2013–2014 among men and women, respectively. By 2030, ∼55.6% of men and 80.0% of women are projected to have CO.
Table 3.
Time trends in the observed estimated annual increase during 1999–2014 and projected 2020 and 2030 prevalence (%) of central obesitya and means of waist circumference (cm) in US adults (>20 years old), children and adolescents (2–19 years old), by gender and ethnicity, based on the National Health and Nutrition Examination Survey (NHANES) 1999–2014 datab. PIR indicates ratio of income to the family’s appropriate poverty threshold set by the US Census Bureau in a given calendar year. The Census Bureau, working in accordance with the Statistical Policy Directive of the Office of Management and Budget, uses a set of money income thresholds that vary by family size and composition to determine who is poor. Thresholds are updated annually for inflation by using the Consumer Price Index6
| Men |
Women |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Annual increase ratea |
Projected for 2020 | Projected for 2030 | Annual increase ratea |
Projected for 2020 | Projected for 2030 | ||||||
| β | SE | P | β | SE | P | ||||||
| Adults (age≥ 20) | |||||||||||
| Waist circumference (cm; mean) | |||||||||||
| All | 0.20 | 0.04 | ** | 103.2 | 105.1 | 0.34 | 0.04 | *** | 99.5 | 102.8 | |
| By ethnicity | |||||||||||
| NH White | 0.21 | 0.04 | ** | 104.8 | 106.9 | 0.39 | 0.05 | *** | 99.6 | 103.5 | |
| NH Black | 0.32 | 0.09 | * | 101.7 | 104.9 | 0.34 | 0.07 | ** | 104.6 | 108.0 | |
| Mexican-American | 0.43 | 0.09 | ** | 104.7 | 109.0 | 0.49 | 0.09 | *** | 102.9 | 107.8 | |
| Others | 0.08 | 0.09 | 97.2 | 98.0 | 0.07 | 0.10 | 91.9 | 92.6 | |||
| By education | |||||||||||
| <High school | 0.22 | 0.09 | * | 102.8 | 105.0 | 0.42 | 0.09 | ** | 102.6 | 106.8 | |
| High school | 0.28 | 0.11 | * | 103.4 | 106.2 | 0.10 | 0.08 | 99.2 | 100.1 | ||
| >High school | 0.19 | 0.05 | * | 103.3 | 105.2 | 0.38 | 0.05 | *** | 99.3 | 103.1 | |
| By poverty income ratio | |||||||||||
| <100%PIR | 0.08 | 0.12 | 98.3 | 99.1 | 0.35 | 0.07 | ** | 101.9 | 105.4 | ||
| 100–200% PIR | 0.29 | 0.08 | ** | 104.1 | 107.0 | 0.38 | 0.07 | *** | 102.0 | 105.8 | |
| >200% PIR | 0.22 | 0.06 | * | 104.3 | 106.5 | 0.33 | 0.06 | *** | 98.0 | 101.3 | |
| Central obesity (%)d | |||||||||||
| All | 0.56 | 0.12 | ** | 50.1 | 55.6 | 0.75 | 0.12 | *** | 72.5 | 80.0 | |
| By ethnicity | |||||||||||
| NH White | 0.56 | 0.13 | ** | 54.2 | 59.8 | 0.87 | 0.15 | *** | 72.7 | 81.4 | |
| NH Black | 0.92 | 0.12 | ** | 48.1 | 57.3 | 0.69 | 0.17 | ** | 83.5 | 90.3 | |
| Mexican-American | 1.20 | 0.32 | ** | 53.4 | 65.6 | 1.30 | 0.27 | ** | 86.6 | 99.4 | |
| Others | 0.31 | 0.49 | 33.0 | 36.2 | 0.04 | 0.33 | 54.1 | 54.4 | |||
| By Education | |||||||||||
| <High School | 0.46 | 0.29 | 46.3 | 50.9 | 0.79 | 0.27 | * | 83.9 | 91.8 | ||
| High School | 0.57 | 0.37 | 48.3 | 54.0 | 0.35 | 0.19 | 76.2 | 79.7 | |||
| >High School | 0.57 | 0.17 | * | 50.8 | 56.5 | 0.87 | 0.14 | *** | 72.0 | 80.7 | |
| By Poverty income ratio | |||||||||||
| <100%PIR | 0.49 | 0.25 | 40.7 | 45.7 | 0.68 | 0.21 | * | 75.8 | 82.6 | ||
| 100–200% PIR | 0.85 | 0.22 | ** | 53.0 | 61.6 | 0.76 | 0.20 | ** | 78.9 | 86.5 | |
| >200% PIR | 0.55 | 0.19 | * | 52.4 | 57.9 | 0.72 | 0.16 | ** | 69.1 | 76.3 | |
| Youth (Age 2–19) | |||||||||||
| Waist circumference (cm; mean) | 0.06 | 0.05 | 70.7 | 71.3 | 0.13 | 0.05 | * | 71.1 | 72.4 | ||
| Waist-to-height ratio (WhtR)c | 0.00 | 0.00 | 0.49 | 0.49 | 0.00 | 0.00 | 0.51 | 0.51 | |||
| WhtR ≥ 0.5 (%)d | 0.24 | 0.13 | 36.5 | 38.9 | 0.36 | 0.16 | 44.0 | 47.6 | |||
P < 0.001, **P < 0.01, *P < 0.05.
The American Health Association/ National Heart, Lung, and Blood Institute defined central obesity as waist circumference > 102 cm in men and > 88 cm in women.
Linear meta-regression models with year as the sole predictor was used to estimate annual increase rate and project prevalence proportions for the years 2020 and 2030 overall and for each stratum by gender and ethnic groups. Projections are based on four datapoints: 1999–00, 2009–2010, 2013–14 and 2015–16. For consistency with Table 1, all other projections are based on 1999–00 to 2013–14 (8 data-points).
Mexican-American adults exhibited the highest annual increase in WC (men: 0.43 cm, women: 0.49 cm) and CO (men: 1.20%; women: 1.30%). Our projections indicated that 99.4% of Mexican-American women would have CO by 2030. There was a gender difference across SES: men had higher WC with higher SES, while the reverse was true among women.
Among the youth (Table 3), WC and WhtR ≥0.5 increased steadily, reaching 46.1 cm and 31.5% in boys and 67.8 cm and 38.2% in girls by 2013–2014. Girls were projected to maintain a higher WhtR ≥0.5 prevalence than boys (47.6% vs 38.9%) in 2030.
Geographic differences in adult obesity
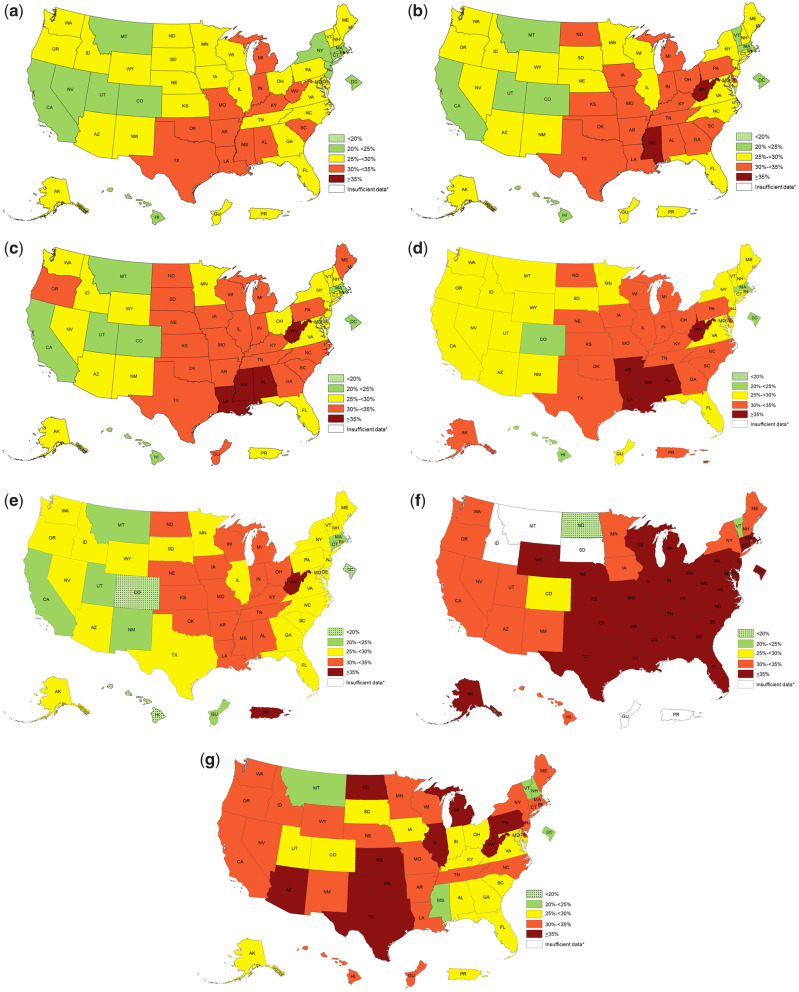
Figure 2 shows the regional differences in adult OB prevalence between 2011 and 2016 and across ethnicities based on state-specific BRFSS data.14,15 Generally, higher OB prevalence was observed in the South (32.0%) and the Midwest (31.4%). In 2016, all states had OB prevalence ≥20%; with five exceeding 35% (West Virginia: 37.7%, Mississippi: 37.3%, Arkansas: 35.7%, Alabama: 35.7% and Louisiana: 35.5).
Figure 2.
Secular trends and ethnic disparities in the regional differences in prevalence (%) of obesity in US adults, Behavioral Risk Factor Surveillance System (BRFSS) 2011–2016. Secular trends (a) 2011, (b) 2013, (c) 2015, (d) 2016. Ethnic disparities using combined BRFSS 2014-2016 (e) non-Hispanic Whites, (f) non-Hispanic Blacks, (g) Hispanics. BMI of study participants was calculated based on reported weight and height. The improvement changes to the BRFSS affect obesity prevalence estimates, and mean that estimates from data collected in 2010 and before cannot be compared estimates from data collected in 2011 and thereafter. The World Health Organization (WHO) defines obesity as BMI ≥30 kg/m2. Data source: Centers for Disease Control and Prevention (CDC). Prevalence of self-reported obesity among US adults by state and territory. Behavioral Risk Factor Surveillance System (BRFSS), 2017.14
The 2016 estimates also indicated that Blacks had ≥30% of OB prevalence in 44 states; Hispanics in 32 states; and Whites in 18 states. During 2011–2016, Blacks ranked highest in OB prevalence, followed by Hispanics and Whites, with a few exceptions (e.g. Guam, Idaho, Montana, Puerto Rico and Wyoming).
2007 study vs current study projections compared
Using NHANES 1999–2014 data, we projected OB/OW/SOB prevalence in 2015, then compared it with two other estimates: (i) the 2007 study projected prevalence in 2015 (based on NHANES 1976–2004) and (ii) the observed prevalence in NHANES 2015–2016 (Table 2). Overall, differences between estimates were small: 1.6%age points (%p) on average (range from −0.7 to 4.9%p). Women had 4.7–4.9%p higher prevalence of OB and OB/OW in our 2007 projection than the actual, which reflected their continuously-increasing trends since 1999, while men’s OB plateaued between 2009–10 and 2011–12, as did men’s SOB between 2013–14 and 2015–16. The newly-projected prevalence in 2015 was lower by 0.6%p on average (range: −7.3 to 1.7%p for adolescent girls) than the actual prevalence in 2015–16.
Discussion
Using nationally representative data, we estimated the prevalence of OB, SOB, OB/OW and CO among adults and the youth in the US. We further examined differences across population groups (sex, age, ethnicity, SES) and geographic regions. Projected adiposity means and prevalence proportions for 2020 and 2030 were also calculated.
To our knowledge, this is the most comprehensive, nationally-representative study of the US OB epidemic using recent data. Prior studies using 2013–14 NHANES data reported that the age-adjusted prevalence of OB was 35.0% among men and 40.4% among women,10 with estimates among youth 2–19 years approaching 17.0%.11 Whether US OB rate has reached a plateau is still controversial.7–11,27,28
Our findings highlight some novel aspects of the US OB epidemic not previously reported, which have implications for future intervention efforts. First, the prevalence of OW, OB and CO in the US has continuously risen to alarming levels. The OB prevalence briefly plateaued or declined in men between 2009–10 (35.5%) and 2011–12 (33.7%), but resumed its rise beyond 2013 (35.0–38.0%). In contrast, women’s OB prevalence proportions have steadily increased since 1999, reaching 41.5% in 2015–16. A similar sex pattern was observed for OB/OW prevalence. By 2030, 81.0% of men and 74.9% of women are projected to be OB/OW. Thus, despite inherent complexity within these time trends, it is safe to say that OB has not levelled off and remains an epidemic, especially CO. Effective intervention efforts to prevent and treat OB thus remain an urgent need.
Second, due to various factors (e.g. policies, interventions, environmental changes, etc.), past data may not reliably predict future trends. Our previous projection models, nevertheless, showed high accuracy,5 with the 2015 prevalence matching well with the recently-observed rate in NHANES 2015–16. This may also indicate that nationwide intervention efforts have not been very successful, and thus more intensive efforts are needed.
Third, ethnic and socio-economic disparities in OB/OW remain large. Notably, the difference of annual increase rate in OB were highest between Mexican-American men vs other men (0.36 vs 0.12) and Mexican-American women vs other women (1.00 vs. −0.15). Across ethnic groups, Mexican-American men (46.6%) and NH Black women (54.7%) had the highest OB prevalence in 2015–16. Mexican-American men had the highest annual increase rate (1.30%p) in OB prevalence, with a 2030 projection of 64.1%. Our new projection indicates that Mexican-Americans are projected to reach 100% OB/OW prevalence by 2030, thus earlier than NH Blacks, even though our 2007 published study projected that Black women would reach a 100% OB/OW prevalence first by 2034.5 In contrast, NH Black women had the highest 2030 projected OB prevalence among all sex-ethnic groups (66.3%).
Importantly, OB, SOB, OB/OW are less prevalent in higher income groups, particularly when PIR > 200%. Nevertheless, those indicators had consistently the highest annual increase rates within the 100–200% of PIR group. US child OB patterns differed markedly from those of adults. In fact, while the prevalence of OB (20.6% in 2015–16) and SOB (7.5%: 2015–16) have continued to increase in boys, their prevalence among girls has levelled off between 2013–14 and 2015–16, as reflected by an estimate of 18.4% in OB and 5.9% in SOB by 2015–16. To stop the OB epidemic in the US, multidisciplinary intervention strategies are needed which consider individual, familial, economic, environmental, social and cultural barriers for promoting healthy lifestyles.
Fourth, WC and CO revealed patterns that were distinctive from those of BMI and OB/OW, particularly with respect to time trends. Adult CO has increased over time and reached 46.1% among men and 67.8% among women in 2013–14. We projected that by 2030, over half of the men (55.6%) and 80.0% of women would have CO. Even among youth, 47.6% of girls and 38.9% of boys are estimated to have the same condition. As CO is a better indicator of OB-related health risks than OB based on BMI, such findings provide useful insights into important targets when preventing and treating OB.24
Finally, large regional differences exist in the US in adult OB prevalence. Although NHANES cannot assess regional differences, BRFSS data can.13–15 They confirmed that regional differences exist, and that they varied over time and across ethnic groups. Generally, OB was most prevalent in the South (32.0%) and the Midwest (31.4%). These regional differences in OB could be related to multiple factors, including economics, race/ethnicity, unemployment rates and governmental policies unique to those regions.29
Our 2007 published study projected that total health-care costs attributable to OW/OB would double every decade to 860.7–956.9 billion US dollars by 2030, accounting for 16–18% of total US health-care costs.6 However, efforts to combat the OB epidemic in the US, including those from federal agencies such as the Center for Disease Control and Prevention (CDC), the US Department of Agriculture (USDA), the Childhood Obesity Task Force, and the National Collaborative on Childhood Obesity Research (NCCOR) during the 8-year Obama administration have resulted in some desirable changes in public awareness of the problem and actions, possibly containing the epidemic growth.30 Otherwise, the problem could have grown worse.6,30
This study has several limitations. First, OB prevalence data from BRFSS were based on self-reported weight and height, which might suffer from report errors. However, such reported data are widely used in obesity-related epidemiological research;31,32 and these are the only available national data to show the geographic distribution of OB rates. Second, our projections were based on the last 15 years of data and recent public health policy changes may impact the trend of OB in the USA. Third, projections among certain groups was limited to the data points available and comparability across waves was an issue with respect to classification of race/ethnicity. This may bias certain estimates and increase uncertainty around projected values. However, the use of meta-regression analysis taking into account the estimated standard error of the means and prevalence proportions was an improvement over our 2007 projections.5 Finally, whereas the projections that are presented consistently used linear models, it is worth noting that for some groups and outcomes, our sensitivity analysis indicated non-linear changes over time. Those were listed comprehensively among our findings. Nevertheless, only a few indicated significant change in model fit between linear and non-linear models (see also the Supplementary Tables, available as Supplementary data at IJE online).
In summary, this study provides a comprehensive description of the obesity epidemic in the USA, related time trends, patterns and disparities across population groups (across sex, age, socio-economic status, racial/ethnic groups and geographic regions) based on recent national survey data. The USA continues to move away from the Healthy People 2010 objectives,33 and obesity has continued rising. We project that the prevalence of OB will continue to increase if effective interventions are not implemented. There is an urgent need to intensify efforts to implement effective interventions to fight the obesity epidemic. Our findings and the projections highlighted are important to help guide future intervention efforts. Because the associations of obesity with key socio-demographic and economic factors are complex and dynamic, population-specific obesity prevention and treatment programmes and policies are needed.
Supplementary Material
Acknowledgements
The content of the paper is solely the responsibility of the authors and does not represent the official views of the funders. The authors also thank Hailee Goodale from Ball State University for her assistance in collecting some data and Shuo-Yu Lin from Virginia Commonwealth University for quality-checking part of the data.
Conflict of interest: None declared.
Supplementary Data
Supplementary data are available at IJE online.
Funding
This work was supported in part by research grants from the National Institutes of Health (NIH), the Eunice Kennedy Shriver National Institute of Child Health & Human Development [U54HD070725 and 1R01HD064685-01A1], the US National Aeronautics and Space Administration (NASA) Mission X program and the Intramural Program of the NIH National Institute on Aging (NIA).
References
- 1. Jensen MD, Ryan DH, Apovian CM. et al. AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol 2014;63:2985–3023. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization Technical Report Series, 2000;1–253;i–xii. [PubMed]
- 3.National Institutes of Health, National Heart, Lung, and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Executive summary, 1998.
- 4. Chriqui JF. Obesity prevention policies in U.S. States and Localities: lessons from the field. Curr Obes Rep 2013;2:200–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang Y, Beydoun MA.. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 2007;29:6–28. [DOI] [PubMed] [Google Scholar]
- 6. Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK.. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring, Md) 2008;16:2323–330. [DOI] [PubMed] [Google Scholar]
- 7. Flegal KM, Carroll MD, Kit BK, Ogden CL.. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491–97. [DOI] [PubMed] [Google Scholar]
- 8. Ogden CL, Carroll MD, Kit BK, Flegal KM.. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA 2012;307:483–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ogden CL, Carroll MD, Kit BK, Flegal KM.. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL.. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016;315:2284–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ogden CL, Carroll MD, Lawman HG. et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA 2016;315:2292–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL.. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA 2018;319:1723–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Center for Disease Control and Prevention (CDC). National Health and Nutrition Examination Survey. Atlanta, GA: CDC, 2016. http://www.cdc.gov/nchs/nhanes.htm (25 October 2016, date last accessed). [Google Scholar]
- 14.Centers for Disease Control and Prevention (CDC). Prevalence of Self-Reported Obesity Among U.S. Adults by State and Territory, BRFSS, 2017. https://www.cdc.gov/obesity/data/prevalence-maps.html (10 October 2017, date last accessed).
- 15.Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System: Turning Information into Health http://www.cdc.gov/brfss (25 October 2016, date last accessed).
- 16.Stata Corporation. Statistics/Data Analysis: Release 16.0 [Computer Program]. Texas: Stata Corporation, 2019. [Google Scholar]
- 17.Kuczmarski RJ, Ogden CL, Guo SS et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11 2002;(246):1–190. [PubMed] [Google Scholar]
- 18.National Health Lung, and Blood Institute. Classification of Overweight and Obesity by BMI, Waist Circumference, and Associated Disease Risks. Bethesda: National Health Lung, and Blood Institute, 2000. [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC). Defining childhood obesity https://www.cdc.gov/obesity/childhood/defining.html (20 October 2017, date last accessed).
- 20. Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR.. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr 2009;90:1314–320. [DOI] [PubMed] [Google Scholar]
- 21.National Institutes of Health (NIH) National Heart L, and Blood Institute’s (NHLBI) North American Association for the Study of Obesity (NAASO). The practical guide: identification, evaluation, and treatment of overweight and obesity in adults In. National Institutes of Health ,2000. Vol Publication no. 00-4084. Rockville, MD. [Google Scholar]
- 22. Li C, Ford ES, Mokdad AH, Cook S.. Recent trends in waist circumference and waist-height ratio among US children and adolescents. Pediatrics 2006;118:e1390–1398. [DOI] [PubMed] [Google Scholar]
- 23. McCarthy HD, Ashwell M.. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message--'keep your waist circumference to less than half your height'. Int J Obes 2006;30:988–92. [DOI] [PubMed] [Google Scholar]
- 24. Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB.. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am J Clin Nutr 2005;81:555–63. [DOI] [PubMed] [Google Scholar]
- 25. Sharp S. sbe23: Meta-Analysis Regression. College Station, TX: Stata Press, 1998. [Google Scholar]
- 26. Singer JD, Willett JB.. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press, 2003. [Google Scholar]
- 27. Skinner AC, Perrin EM, Skelton JA.. Prevalence of obesity and severe obesity in US children, 1999-2014. Obesity (Silver Spring, Md) 2016;24:1116–123. [DOI] [PubMed] [Google Scholar]
- 28. Wang Y, Baker JL, Hill JO, Dietz WH.. Controversies regarding reported trends: has the obesity epidemic leveled off in the United States? Adv Nutr (Bethesda, MD) 2012;3:751–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Myers CA, Slack T, Martin CK, Broyles ST, Heymsfield SB.. Regional disparities in obesity prevalence in the United States: a spatial regime analysis. Obesity (Silver Spring, Md) 2015;23:481–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.White House Task Force on Childhood Obesity. American's move to raise a healthier generation of kids. https://letsmove.obamawhitehouse.archives.gov/white-house-task-force-childhood-obesity-report-president (26 October 2017, date last accessed).
- 31. Nelson DE, Powell-Griner E, Town M, Kovar MG.. A comparison of national estimates from the national health interview survey and the behavioral risk factor surveillance system. Am J Public Health 2003;93:1335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pierannunzi C, Hu SS, Balluz L.. A systematic review of publications assessing reliability and validity of the behavioral risk factor surveillance system (BRFSS), 2004-2011. BMC Med Res Methodol 2013;13:49.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention, National Center for Health Statistics. Healthy People 2010 https://www.cdc.gov/nchs/healthy_people/hp2010.htm (8 January 2020, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.