Abstract
Background
Since January 2020, novel coronavirus (SARS-Cov-2) – infected pneumonia (COVID-19) rapidly spread in Korea. This study aimed to introduce the Korean Medicine (KM) telemedicine center for treatment of COVID patients in Korea.
Methods
This work was a retrospective review of medical records on patients who received at least one telemedicine session from March 9, 2020 to April 12, 2020 provided by the COVID-19 telemedicine center of Korean Medicine. Data on demographic characteristics, treatment frequency, number of consultation were collected. A descriptive statistical analysis was conducted to report characteristics of patients.
Results
A total of 1742 patients underwent consultation through KM telemedicine centers. Despite the rapid increase in the number of patients, the telemedicine center provided treatments to an average of 192 patients per day by about an average of 15 doctors. Furthermore, 4552 herbal medicines were prescribed through telemedicine center, among which 1366 cases (30%) being Qing-Fei-Pai-Du-tang. Telemedicine care also has shown that even with patient's residence transition, medical care can be continued without pause.
Conclusion
These results show some advantages of the telemedicine center's implementation in terms of the effective use of medical resources and continuous treatment for patients.
Keywords: Telemedicine, Korean Medicine Center, COVID-19, Pandemic outbreaks
1. Introduction
Due to the COVID-19 Pandemic, each country around the world deliberate method of medical resources protection and efficient usage of medical resources. In the case of South Korea, the spread of infectious disease is prevented effectively by early detection and isolation through mass testing.1 Nevertheless, South Korea was one of the early hardest-hit countries with COVID-19 largely owing to a mass infection after an infected person visited a single church, which led to an increase of infected people localized in Daegu-Gyeongbuk region according to the Korea Centers for Disease Control and Prevention (KCDC).2 With this sudden increase in the number of infected people, the Korean government temporarily allowed “untact” (a term coined by a research team in Korea for non-face-to-face contact. And now widely used in terms of social distancing; also known as no-contact, zero contact, or non-contact) medical telephone counseling.
In particular, the explosive increase in the number of patients in a specific region, Daegu-Gyeongbuk for instance, has caused depletion of medical resources such as hospital beds and medical staff. For that reason, the Association of Korean Medicine opened the telemedicine center in Daegu on March 9, 2020, and started to operate another telemedicine center in Seoul on April 21, 2020.
The drive-through screening center and the community treatment centers in Korea efficiently managed medical resources.3, 4 Likewise, the telemedicine is also expected to increase the efficiency of using medical resources and managing patients overall. The purpose of this study was to introduce the telemedicine center as a treatment option for COVID-19 patients. In this regard, the researchers intended to report on the current status of medical treatment at the telemedicine center in Korea and the number of treatments up to date.
2. Method
2.1. Study design
This study was a retrospective review of the medical charts of patients who had received treatment at least one session for treating or managing COVID-19 in the Telemedicine Center of Korean Medicine from March 3, 2020 to April 12, 2020.
2.2. Participants and recruitment
Diagnosis on patients classified to be isolated under the standard of government, was preceded at the telemedicine center at Daegu, which opened on March 9. Promotion of the telemedicine center with its representative phone number was carried out through web portals and newspaper articles. When a patient was referred to the telemedicine center, the volunteer checked the status of the patient through an electronic chart. The quarantine rules were being enforced to the confirmed and suspected patients and the patients were deployed to self-isolating or admission to community centers or hospitalization. In this telemedicine center, treatments were done not only to the confirmed case but also the patients recovering from COVID-19 after having tested negative. The researchers analyzed the data of patients undergoing telemedicine from the opening of the COVID-19 Telemedicine center in Daegu on March 9 to April 12.
2.3. Guidance on COVID-19 Telemedicine of Korean Medicine
Association of Korean Medicine developed ‘Guidance on COVID-19 Telemedicine of Korean Medicine’ based on the Chinese Clinical Guidance for COVID-19 Pneumonia Diagnosis and Treatment (7th edition)5, 6, 7, 8, 9 and referred to the data from Centers for Disease Control (CDC) and National Institutes of Health (NIH) of the United States and the recommendations from the KCDC and expert advice in Korean medicine. As a result, medical staffs at the telemedicine center were able to verify the patient's symptoms and recommend herbal medicine through telemedicine.6, 10, 11 The telemedicine center was initially installed at Daegu Haany University Korean Medicine Hospital during the outbreak in Daegu-Gyeongbuk area (Supplement 1A), which is later continued at the hall of the Association of Korean Medicine (AKOM) in Seoul since April 21 (Supplement 1B). The medical staffs of the telemedicine center were doctors who voluntarily applied to the center after coming across the announcement or the public service advertisement by the AKOM. The entire consultation process was managed by the AKOM's advisory group, consisting of doctors with wide experiences in respiratory diseases.
2.4. Telemedicine management
The Telemedicine Center of Korean Medicine used herbal medicine mainly for relieving COVID-19 symptoms and provided mindfulness meditation for improving mental health of COVID-19 patients.12 Herbal medicines were prescribed by Korean Medicine doctors according to established protocols made by expert advisory panels and by foreign guidance or data on COVID-19.6 In regards to mental health management, the ‘Korean Medicine Doctor's Mental Health Introduction Manual’ was developed by the Oriental neuropsychiatry specialists group, for patients who reported to suffer from psychological problems such as depression, anxiety and fear. COVID-19 patients consulted the telemedicine center doctors via telephone and the doctors prescribed herbal medicine such as Qing-Fei-Pai-Du-Tang, Yin-Qiao-San and Huo-Xiang-Zhengqi-San.11 When herbal medicine was prescribed to the patient, it was delivered directly to the patient's residence by volunteers of telemedicine center or through courier services. Follow up calls were made to patients every 3 days to check for changes in symptoms.
In order to standardize the treatment of doctors, they were trained by the AKOM's medical advisory group before assigning them to the center. The training consisted of various on-site response manuals related to the use of electronic charts during the treatment and prescriptions of available herbal medicine at the telephone treatment center.
2.5. Collected variables through telemedicine center
When patients contacted the telemedicine center for the first time, volunteers checked their gender, age, address, and date of initial diagnosis. Then a Korean Medicine doctor classified a patient's condition as one of the following: ‘Confirmed with COVID-19 and in quarantine’, ‘Confirmed with COVID-19 but released from quarantine after recovery and tested negative’, ‘Unconfirmed but in quarantine’, ‘Unconfirmed and released from quarantine’ and ‘Unknown’.
The doctor subsequently checked the medication and baseline disease of patients, such as hypertension, diabetes, hyperlipidemia, cancer, and chronic respiratory disease. After the medical background check, the patients were asked about possible symptoms caused by COVID-19 including fever, cough, sputum, sore throat, fatigue, nausea, diarrhea, anorexia, rhinorrhea, chest pain or discomfort, difficulty breathing, headache, and myalgia. Among these symptoms, the doctor recorded 3 representative symptoms of the patient. When the consultation finished, the doctor prescribed medicine to the patient. In the following up calls, the doctor checked for changes in the representative symptoms and recorded as ‘Severely worsening’, ‘Worsening’, ‘No changes’, ‘Improvement’, and ‘Great improvement’.
2.6. Data source/measurement
All data were collected through electric medical charts and managed by AKOM. Data extracted from the patient's medical chart was entered into the spreadsheet with the participant's identification code, used in creating statistical content, and provided to researchers.
2.7. Statistical analysis
A descriptive statistical analysis was conducted. Continuous data were analyzed with mean and standards deviation. Categorical data were presented by frequency and percentage. All statistical data were analyzed using SPSS for the Windows (ver 20.0) after data coding.
2.8. Ethical considerations
In this study, we could not access an original individual medical chart. However, the medical activities data reported by AKOM were received. An institutional review board approval for this study was exempted for full review at the Korea Institute of Oriental Medicine (number I-2004/003-003) for the use of medicinal records.
3. Result
3.1. Demographic characteristic of patients who underwent treatment through telemedicine center
A total of 1742 patients used Korean Telemedicine Center. The data of Daegu Korean Medicine Center from the opening to 12 April, was compared to the national statistics on April 13 at 00:00. Confirmed patients who underwent treatment through telemedicine center were 16.53% (Table 1).
Table 1.
Demographic Characteristics of Patients Who Used Telemedicine Center and Their Proportion to Total Confirmed Cases
| Patient using telemedicine center |
Total patients in Korea |
||||
|---|---|---|---|---|---|
| Number | Percentage (%) | Number and percentage (%) | Percentage of patients using telemedicine center to total confirmed cases (%) | ||
| Sex distribution | Female | 1325 | 76.1 | 6294 (59.73) | 21.05 |
| Male | 417 | 23.9 | 4243 (40.27) | 9.83 | |
| Age distribution | 0–19 | 73 | 4.2 | 694 (6.58) | 10.52 |
| 20–39 | 355 | 20.4 | 4001 (37.97) | 8.87 | |
| 40–59 | 890 | 51.1 | 3333 (31.64) | 26.70 | |
| +60 | 424 | 24.3 | 2509 (23.81) | 16.90 | |
| Termination status | Ongoing | 837 | 48.0 | 2873 (27.27) | Non-comparable |
| Termination | 905 | 52.0 | 7664 (72.73) (Including Death 217; 2.06%) | Non-comparable | |
| Diagnosis | Suspected | 47 | 2.70 | Non-comparable | Non-comparable |
| Confirmed & isolation | 250 | 14.35 | |||
| Recovering after Discharge | 1430 | 82.10 | |||
| Unknown and fail to follow up | 15 | 0.86 | |||
* The data of telemedicine center were based on statistics as of 12 April 2020, 18:00 Korea Standard Time (KST).
** The data of national statistics were based on statistics as of 13 April 2020, 00:00 KST.
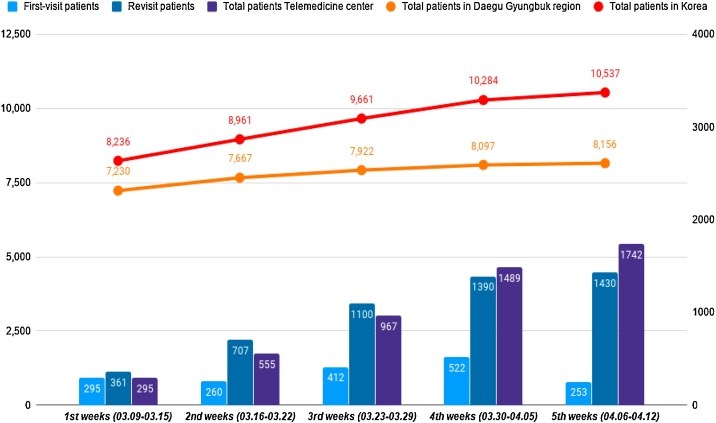
Among those who received treatment through telemedicine center (1742 patients in total), 1686 (96.79%) patients were from Daegu and Gyeongbuk region and 56 (3.2%) were from other areas (Supplement 1C). The characteristics of patients in Daegu-Gyeongbuk region who received telemedicine treatment is presented as Supplement 2. Cumulative cases in the telemedicine center of Korean medicine association as of 13 April, 2020 is presented on Fig. 1.
Fig. 1.
The number of COVID-19 patients in Korea and usage of Telemedicine center. The light blue bars were the number of first-visit patients, the dark blue bars were the number of revisit patients, the purple bars were total.
3.2. The number of treatment conducted through telemedicine center
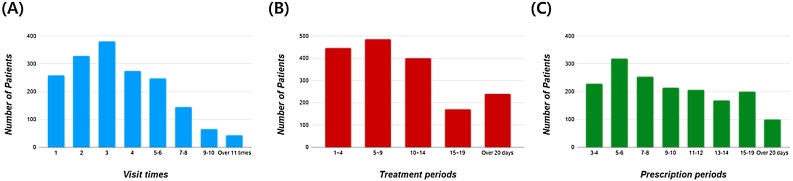
The patients who received over 5 times of the telemedicine treatment were 501, those who received 3 times were 381, and those who received 1 time were 258 patients (Fig. 2). Among the patients who received treatment at the telemedicine center, 232 (13.3%) patients were in quarantine after being confirmed with COVID-19. A total of 873 (50.1%) confirmed patients received treatment through telemedicine center after releasing from quarantine status. An average of 14.94 Korean Medicine doctors and 17.75 volunteers participated for medical treatment every day at each center. With only about 15 doctors, the telemedicine center provided treatments to an average of 192 patients per day. Out of 4552 herbal medicines prescribed through telemedicine center, 1366 (30%) cases were Qing-Fei-Pai-Du-tang.
Fig. 2.
The statistics of telemedicine center treatments (A) The number of treatments (B) Treatment periods (C) Duration of medication prescribed through telemedicine center.
3.3. Classification of patients’ residence and transition of treatment
In Korea, patients with severe symptoms got treated in hospitals with negative-pressure isolation rooms, specialized in the COVID-19 intensive care and treatment. Patients with mild symptoms were treated at the community treatment centers or self-isolated at home. Residence status of 1715 (98.45%) patients out of 1742 total patients that received the telemedicine treatment, was identified during the treatment. During the follow up, 489 patients who transferred at least once, 94 patients (19.07%) have experience with admission to higher facilities such as from self-isolation to hospital and from community center to hospital. Notably, we observed some cases of hospitalization again after being discharged from the hospital (Supplement 3).13
4. Discussion
Recent research suggests that telemedicine intervention is an effective way in managing infectious diseases.14, 15 In particular, according to the review paper on the effectiveness of telemedicine, the use of the telemedicine helps patients’ satisfaction, privacy and time saving.16, 17 This study may show that the telemedicine center in Korea could be an example of managing mild patients and screening patients transitioning from mild to the severe stage in isolation facilities. COVID-19 telemedicine center of Korean Medicine is still in operation with the increasing number of new patients as the number of treatments per patient is distributed from 1 to over 10 times. Especially, it is suggestive that there are 145 cases who received treatment over 8 times and 44 cases with more than 10 times of treatment. 26.70% of confirmed patients in 40–50 s and 16.90% of confirmed patients in 60 s and above have underwent treatment through the telemedicine center. High participation and response of telemedicine in patients of these age groups suggest the possibility of using telemedicine in selectively high-risk groups in the treatment of infectious diseases. Moreover, it is noteworthy that these treatments were made to an average of 192 patients by an average of 15 doctors.
Based on the literature searching, this is the first report in Korea to record changes in the residence transition status of patients. Untact medical care system like telemedicine shows the probability of reducing waiting time of patients and solving hospital-bed shortage problems.18
However, there are several limitations of this study. First, this is a retrospective descriptive analysis and does not reflect the information on the improvement of symptoms in patients. Second, this is interim analysis and does not cover the whole results of telemedicine center. In these regard, further studies are needed to figure out the satisfaction and clinical outcomes of the patients who underwent treatment through the COVID-19 telemedicine center. Researchers may conduct and analyze a satisfaction survey with relevant data and changes on symptoms in the future.
In conclusion, the case of telemedicine operation in response to infectious diseases in Korea is considered to be meaningful for efficient use of medical resources, patient management and prevention of infection spread.
Acknowledgment
The authors are grateful for the support and cooperation with COVID-19 telemedicine center of Korean medicine and The Association of Korean Medicine.
Author contributions
Conceptualization: DK and EL, Methodology and Writing–Original Draft: HC, Data Curation: EL and BK, Writing–Review and Editing: YM and SP, Visualization: KK, S-HP and YK, Supervision: MS and GC, Project administration: EL. All authors read and approved the final version of the manuscript.
Conflict of interest
The authors declare no conflict of interest.
Funding
This research received no external funding.
Ethical statement
This study received an exemption determination by the Institutional Review Board (IRB) of the Korea Institute of Oriental Medicine (number I-2004/003-003) for the use of medical records.
Data availability
The datasets used for this study are available from the corresponding author on reasonable request.
Footnotes
Supplements associated with this article can be found in the online version, at doi:10.1016/j.imr.2020.100492.
Supplementary material
The following are the supplementary data to this article:
References
- 1.Balilla J. SSRN; 2020. Assessment of COVID-19 mass testing: the case of South Korea. published online March 18 (preprint) [DOI] [Google Scholar]
- 2.Kang Y.J. Characteristics of COVID-19 infection in Korea from the mass infection perspective. J Prev Med Public Health. 2020;53 doi: 10.3961/jpmph.20.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwon K.T. JKMS; 2020. Drive-through screening center for COVID-19: a safe and efficient screening system against massive community outbreak. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park P.G., Kim C.H., Heo Y., Kim T.S., Park C.W., Kim C.H. Out-of-hospital cohort treatment of coronavirus disease 2019 patients with mild symptoms in Korea: an experience from a single community treatment center. J Korean Med Sci. 2020;35:e140. doi: 10.3346/jkms.2020.35.e140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.China National Health Commission . 7th ed. 2020. Chinese clinical guidance for COVID-19 pneumonia diagnosis and treatment. [Google Scholar]
- 6.The Association of Korean Medicine . 2nd ed. 2020. COVID-19 Korean medicine clinical guidance. https://www.kmcric.com/news/newspaper/view/41842. [Google Scholar]
- 7.Ho L.T.F., Chan K.K.H., Chung V.C.H., Leung T.H. Highlights of traditional Chinese medicine frontline expert advice in the China national guideline for COVID-19. Eur J Integr Med. 2020:101116. doi: 10.1016/j.eujim.2020.101116. [published online ahead of print, 2020 April 3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jin Y.H., Cai L., Cheng Z.S., Chung Z.S., Cheng H., Deng T. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Mil Med Res. 2020;7:4. doi: 10.1186/s40779-020-0233-6. Published 2020 Feb 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luo E., Zhang D., Luo H., Liu B., Zhao K., Zhao Y. Treatment efficacy analysis of traditional Chinese medicine for novel coronavirus pneumonia (COVID-19): an empirical study from Wuhan, Hubei Province, China. Chin Med. 2020;15:34. doi: 10.1186/s13020-020-00317-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang S.X., Wang Y., Lu Y.B., Li J.-y., Song Y.-j., Nyamgerelt M. Diagnosis and treatment of novel coronavirus pneumonia based on the theory of traditional Chinese medicine. J Integr Med. 2020 doi: 10.1016/j.joim.2020.04.001. [published online ahead of print, 2020 Apr 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ren J.L., Zhang A.H., Wang X.J. Traditional Chinese medicine for COVID-19 treatment. Pharmacol Res. 2020;155:104743. doi: 10.1016/j.phrs.2020.104743. [published correction appears in Pharmacol Res. 2020 Mar 25:104768] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kwon CY, Kwak HY, Kim JW. Using Mind-Body Modalities via Telemedicine during the COVID-19 Crisis: Cases in the Republic of Korea. [DOI] [PMC free article] [PubMed]
- 13.Ye G., Pan Z., Pan Y., Deng Q., Chen L., Li J. Clinical characteristics of severe acute respiratory syndrome coronavirus 2 reactivation. J Infect. 2020;80:e14–e17. doi: 10.1016/j.jinf.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coombes C.E., Gregory M.E. The current and future use of telemedicine in infectious diseases practice. Curr Infect Dis Rep. 2019;21:41. doi: 10.1007/s11908-019-0697-2. [DOI] [PubMed] [Google Scholar]
- 15.Eron L., King P., Marineau M., Yonehara C. Treating acute infections by telemedicine in the home. Clin Infect Dis. 2004;39:1175–1181. doi: 10.1086/424671. [DOI] [PubMed] [Google Scholar]
- 16.Parmar P., Mackie D., Varghese S., Cooper C. Use of telemedicine technologies in the management of infectious diseases: a review. Clin Infect Dis. 2015;60:1084–1094. doi: 10.1093/cid/ciu1143. [DOI] [PubMed] [Google Scholar]
- 17.Gras G. Use of telemedicine in the management of infectious diseases. Méd Maladies Infect. 2018;48:231–237. doi: 10.1016/j.medmal.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 18.Kim S.W., Lee K.S., Kim K., Lee J.J., Kim J.Y., Daegu Medical Association A brief telephone severity scoring system and therapeutic living centers solved acute hospital-bed shortage during the COVID-19 outbreak in Daegu, Korea. J Korean Med Sci. 2020;35:e152. doi: 10.3346/jkms.2020.35.e152. Published 2020 Apr 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used for this study are available from the corresponding author on reasonable request.