Abstract
Background:
Cerebral aneurysm rupture is a distinct entity among various causes of cerebrovascular accident. Despite the current concept of early surgical clipping to prevent consequences of ruptured aneurysm in good grade subarachnoid hemorrhage patients, 40–50% have postoperative cognitive dysfunction (POCD) on a long- term basis. Here, we compared the effect of two commonly used anesthetic agents on cognitive function following cerebral aneurysmal surgery, i.e., propofol and desflurane.
Methods:
We conducted a prospective double-blind clinical study in 70 patients who were randomized to receive maintenance anesthetic agents either propofol or desflurane. The cognitive functions of patients were studied at the time of the discharge from a hospital or at 2 weeks following surgery whichever was early using the Hindi version of the Montreal Cognitive Assessment scale. The hemodynamic parameters, brain relaxation score at the different time intervals, were also studied.
Results:
There was no difference between the two anesthetic agents in terms of incidence of POCD (65.4% vs. 82.6%, P > 0.05) at the time of discharge or at 2 weeks following surgery. The mean POCD score in propofol and desflurane group was 22.81 ± 4.45 and 19.09 ± 5.66 which was statistically significant (P-value-0.01). The scores for domains of executive function, attention, and orientation were better with propofol group than desflurane group. Intraoperative hemodynamics and brain relaxation scores were similar in both groups.
Conclusion:
A significant number of patients undergoing aneurysmal neck surgery experienced POCD although incidence remained similar in both groups. However, it appears that mean cognitive score and certain domains of cognitive functions especially the executive function, attention, and orientation were better preserved with the use of propofol when compared to desflurane at the time of discharge or on 2 weeks following surgery whichever was early.
Keywords: Aneurysmal subarachnoid hemorrhage, Desflurane, Postoperative cognitive dysfunction, Propofol

INTRODUCTION
The concept of postoperative cognitive dysfunction (POCD) has its origin in the1950s.[3] In the present era, due to easy accessibility to the medical facilities and availability of early surgical interventions, mortality following aneurysmal subarachnoid hemorrhage (aSAH) over a period of time has comparatively decreased. However, the incidence of POCD after craniotomy for aneurysmal neck clipping has been found to be varying between 40% and 55% and survivors continue to experience difficulty in day to day activity, recalling recent events, and easy forgetfulness.[12]
Over the past two decades, concern has been raised regarding the impact and role of used anesthetic agents during the perioperative period in POCD. Multiple human and nonhuman studies have found to prove both neuroprotective and neurotoxic action of various anesthetic agents used.[6,7,13,25]
Propofol along with remifentanil has shown to improve cognitive outcomes by rapid recovery and early return to normal activities. However, results with this anesthesia technique were heterogeneous.[8,11] Some studies failed to show any improvement in emergence time whereas others reported a faster emergence and return of cognitive functions in comparison to desflurane and sevoflurane.[9,14] Patients also showed speedy extubation, wakefulness, and orientation using desflurane as compared to propofol/remifentanil regimen.[1,10]
Propofol and desflurane both share common properties. They have rapid onset and rapid offset of action. In addition, both agents cause reduction of cerebral metabolism, cerebral oxygen consumption, and intracranial pressure (ICP).[16,17,20,23] Hence, both agents are favored in neurosurgical procedures. However, it is not sure whether these anesthetic agents have any impact on POCD in patients undergoing aneurysmal neck clipping following a ruptured cerebral aneurysm. Hence, this study was designed to prospectively evaluate the effects of propofol and desflurane on POCD in patients of aneurysmal SAH undergoing craniotomy and clipping of a ruptured aneurysm. In addition, intraoperative hemodynamics in terms of heart rate (HR), systolic blood pressure, and mean arterial blood pressure and intraoperative brain relaxation with the use of both these agents were also compared.
MATERIALS AND METHODS
This prospective randomized study was conducted in our institution over a period of 1½ years after obtaining ethical clearance from the institutional board. The patients with clinical and radiological evidence of ruptured cerebral aneurysm aged between 18 and 65 years, Hunt and Hess (H&H) grade 1, 2 and American Society of Anesthesiology (ASA) physical status I, II, and III scheduled for aneurysm neck clipping were included in the study. A previous history of multiple surgeries, low level of education (illiterate), known psychiatric disease or drug abuse, comorbidities other than hypertension, and diabetes mellitus, were excluded in the study. Postoperatively, patients who were intubated or tracheostomized even after 2 weeks following exposure to anesthesia were not assessed for cognitive functions.
Randomization and blinding
A total of 70 patients were randomized equally into two groups, the propofol group and desflurane group. The randomization was done using a computer-generated random numbers algorithm. The neurosurgical team and the clinical psychologist were blinded to the anesthesia protocol.
Anesthetic technique
All the surgeries were conducted by experienced neurosurgeons. Written informed consent was obtained beforehand. Fasting status as per ASA guidelines was confirmed before shifting the patient inside the OT. Preinduction noninvasive monitors were attached. These were 5-lead electrocardiography, noninvasive automated blood pressure, pulse oximetry, capnography, and entropy. Propofol was used as an induction agent in both groups. For intraoperative analgesia, 1–2 μg/kg bolus fentanyl followed by infusion at 0.5–2 μg/kg/h used. Vecuronium 0.1 mg/kg was given for muscle relaxation. For continuous blood pressure monitoring, an arterial catheter was inserted. Subsequently, they were maintained on either propofol or desflurane as per the randomization along with 100% oxygen (due to nonavailability of air). For maintaining a comparable depth of anesthesia in both groups, state entropy (SE) was targeted between 40 and 60. Partial arterial pressure of carbon dioxide (PaCO2) was maintained in the range of 32–35 mmHg but if the brain swelling persisted despite osmotic therapy then PaCO2 was brought down to 28–32 mmHg. Fentanyl infusion was stopped at the beginning of scalp closure whereas the maintenance anesthetic agents were stopped at the time of application of skin staples for skin closure. Neuromuscular blockade was reversed with iv neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg. Subsequently, patients were extubated if they met extubation criteria. Intraoperatively, hemodynamic monitoring, temporary clipping time, and any incidence of aneurysm rupture were noted. Brain bulge at the time of dura reflection and dura closure was noted. Patient status was assessed at the end of surgery, i.e., GCS was noted. The postoperative ventilation days were noted as well.
Cognitive function assessment
The cognitive functions were assessed using a modified Hindi version of the Montreal Cognitive Assessment (MOCA) scale.[18,24] The MOCA test is a thirty-point scale and includes six subsets: visuospatial/executive functions, naming, attention, abstraction, recall (delayed), and orientation. The maximum score is 30 while the minimum possible is 0 in the MOCA scale. A score of ≥26 is considered as normal.
The cognitive impairment is considered if the score is either 25 or <25. One point is added for participants with <12 years of education. Few changes were made by us in the original version considering the Indian population. The changes were:
The naming of rhinoceros was done by only one of aneurysmal surgery patients postoperatively out of ten and was replaced with an elephant which was easier and familiar in the Indian population.
In reading, a list of letters in place of English word A, Hindi word d was used.
In the language section, sentences in the Hindi language were used for the convenience of patients as most patients found it difficult to remember and repeat sentences in the English language.
Fluency/naming maximum number of words in 1 min that begin with F was changed to e.
In delayed recall, words face, velvet, church, daisy, and red was changed to Hindi words.
An assessment was carried out in a single session at the time of discharge of patients from hospital or 2 weeks following surgery (whichever was earlier) by an independent clinical psychologist who was unaware of study drug.
Sample size calculation
The sample size was estimated based on the mean difference of cerebral metabolic rate (CMR) (with the use of propofol when compared to desflurane) as 17%, with a standard deviation (SD) of 2.0 between two groups.[16,20] The sample size was calculated having 30 subjects per group with a power of 80% and Type I error of 5%. For possible dropouts and mortality, it was decided to include 35 patients per group.
Statistical analysis
Normality of quantitative data was checked by measures of Kolmogorov–Smirnov tests of normality. The normally distributed data means have been compared using unpaired t-test and presented as mean ± SD. Categorical variables were analyzed using Chi-square test and presented as number and percentages. All calculations are two sided and were performed using Statistical Package for the Social Sciences (SPSS Inc. 2013, version 22.0 for Windows, Armonk, NY, USA). A P < 0.05 has been considered statistically significant.
RESULTS
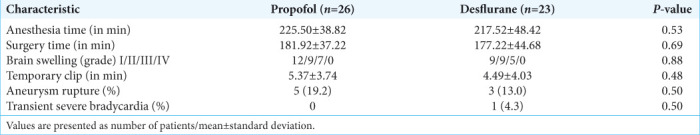
A total of 70 patients were enrolled in the study with 35 patients in each group. After exclusion, only 26 patients in the propofol group and 23 patients in the desflurane group were considered a part of the study and the data obtained from them were used for statistical analysis [Figure 1]. The baseline characteristics (age, sex, educational status, ASA grading, site of the aneurysm, H&H grade, and WFNS grades) were comparable in both drug groups. Intraoperatively, both the groups were comparable with respect to the following parameters: duration of anesthesia, duration of surgery, brain swelling grades, temporary clipping time, significant hemodynamic changes, and intraoperative aneurysm rupture requiring pharmacological intervention [Tables 1 and 2].
Figure 1:
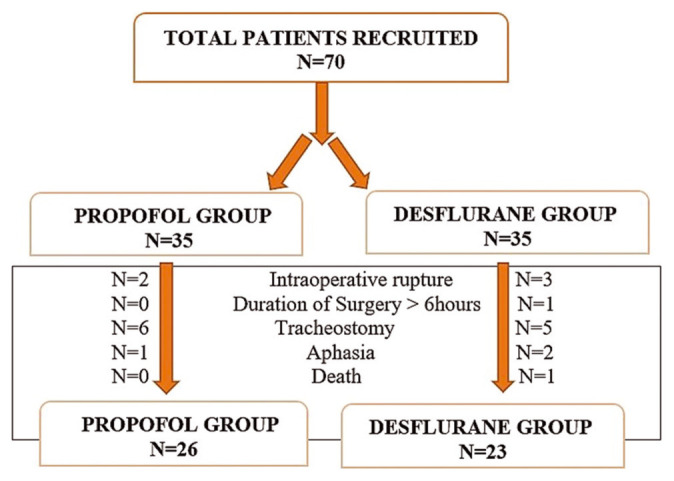
Patient Recruitment
Table 1:
Demographic characteristics.
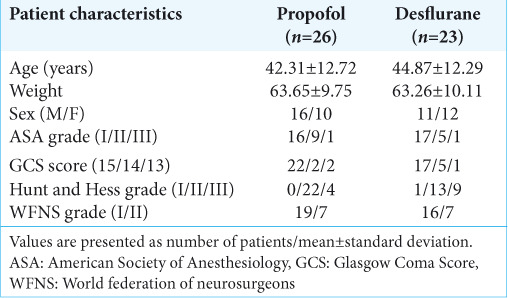
Table 2:
Intraoperative characteristics.
Cognitive function assessment
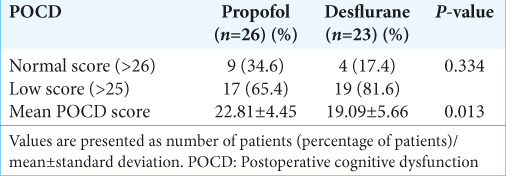
Cognitive functions assessed at the time of discharge of patients from hospital or 2 weeks following surgery and we found that the incidence of POCD in propofol group was 65.4% and in desflurane group was 82.6%. The incidence of POCD appears to be higher in desflurane group compared to propofol group but it was not statistically significant (P = 0.33).
A significant difference emerged between the two groups with regard to mean POCD score. The mean POCD score in propofol group was 22.81 ± 4 which was significantly higher than that of desflurane group (19.09 ± 5.66) (P = 0.01) [Table 3].
Table 3:
Intergroup POCD incidence and mean POCD score.
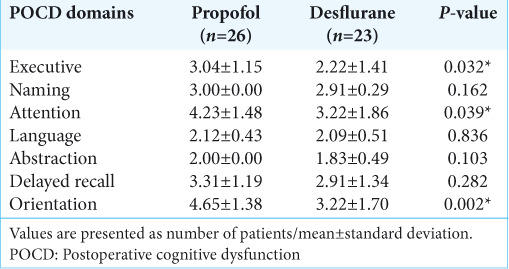
Further subgroup analysis of individual domains of cognition was performed. We found a significant difference between both groups in the domains of executive functions, attention, and orientation with P = 0.032, 0.039, and 0.002, respectively. However, there was no significant difference in the following domains- naming, language, abstraction, and delayed recall [Table 4].
Table 4:
Individual cognitive domains.
DISCUSSION
POCD is commonly seen in good grade aSAH patients despite early surgical clipping of aneurysmal neck. Both inhalational and intravenous agents have been used for the maintenance of anesthesia during neurosurgery. However, the data comparing various agents for aneurysm neck clipping surgery are lacking. The only study which we could find for this particular surgery was carried out by Cheng et al. wherein they compared desflurane and propofol for brain relaxation after achieving burst suppression.[5] Our search did not come across any study evaluating the influence of the anesthetic drug on the POCD following aneurysmal neck clipping surgery.
An early postoperative assessment should be conducted during the 1st week, at its end if at all possible. Surgery-related factors may affect test performance if performed too early. Pain, fatigue, nausea, and vomiting, the effects of opioids, and sedative medications and possible early complications would impair function and motivation and make it difficult to distinguish normal performance from deterioration. If testing is done within the first 3 postoperative days, it is advisable to test the patients for possible delirium. Some patients develop persistent delirium lasting more than 3 months.[19] With the possibility of minimizing confounding factors, we conducted the test for POCD at 2 weeks or at the time of discharge of the patient (whichever was earlier) after surgery.
In our study, we found that 34.6% of patients in propofol group and 17.4% of patients in desflurane group had normal cognitive functions postoperatively. Seventeen (65.4%) patients in propofol group and 19 (82.6%) patients in desflurane group had cognitive dysfunction postoperatively. Both groups had a comparable incidence of POCD. A significant difference emerged between the two groups with regard to mean POCD score. The mean POCD score in propofol was 22.81 ± 4 which was significantly higher than that of desflurane (19.09 ± 5.66).
To date, none of the studies has compared propofol with desflurane for POCD in aneurysmal neck clipping surgery. In non- neurosurgical settings few studies have found higher incidence of POCD with use of propofol as compared to desflurane.[14,15,21] Royse et al. found significantly higher incidence of early-onset POCD with propofol as compared to desflurane (56/84 [67.5%] vs. 41/83 (49.4%), respectively, P = 0.018) in patients who underwent coronary artery bypass grafting and 3 months later no difference was found (10/87 [11.2%] vs. 9/90 [10%], respectively.[21] Hence, they concluded decreased early cognitive impairment with desflurane. Larsen et al. conducted a study in 2000 in which authors compared remifentanil-propofol with desflurane and sevoflurane anesthesia in elective operations for emergence time and return of cognitive function.[14] They found a significantly faster emergence and return of cognitive function with a remifentanil-propofol group than desflurane. Lebenbom et al. conducted a study comparing recovery times with desflurane and propofol with and without nitrous oxide.[15] They divided the patients into four groups, namely, propofol induction followed by desflurane and nitrous oxide maintenance (Group 1), propofol and nitrous oxide (Group 2), desflurane induction followed by desflurane and nitrous oxide (Group 3), and desflurane induction and maintenance (Group 4). They found Group 4 patients were able to communicate earlier than Groups 1, 2, and 3. Furthermore, immediate recovery was better in Groups 2 and 4 as compared to 1 and 3 numerically but that finding was not statistically significant.
As compared to nonneurosurgical studies, our study showed better results with propofol group than desflurane group. This could be due to the favorable effects of propofol on cerebrovascular physiology.[20] Propofol has an intrinsic cerebral vasoconstrictive property and it decreases CMR by 48–58% and cerebral blood flow (CBF) by 53–79%.[20,23] Volatile anesthetic agents have vasodilatory properties. Desflurane decreases CMR by 35% and CBF by 22%. Desflurane may cause an increase in CBF more so if used at a concentration >1.0 MAC.[16,17] This might have contributed to the better cognitive function propofol group compared to desflurane group.
When individual domains of cognitive function were compared between two drug groups, we found a significant difference in the domains of executive functions, attention, and orientation with P = 0.032, 0.039, and 0.002, respectively. In the present study, it was found that patients in propofol group have higher scores as compared to desflurane group. However, there were no statistically significant differences in naming, language, abstraction, and delayed recall.
Surgery for clipping of aneurysm neck after SAH requires strict control on the intraoperative hemodynamics. Both groups had comparable intraoperative hemodynamics. Our results were comparable to those seen in the intraoperative hypothermia for aneurysm surgery trial for aneurysm clipping conducted by Todd et al. wherein the incidence of hypotension in the hypothermia and normothermia group was 2% and 3%, respectively (P = 0.24).[22] Similarly, Bastola et al. in their study on supratentorial lesions found comparable hemodynamics with propofol, sevoflurane, and desflurane.[2] In our study, we also found that intraoperative hemodynamics with respect to HR was comparable in both groups except at dura closure, skin closure, and removal of headpins. Although the difference in results of HR was statistically significant, the difference was clinically not important.
We also compared intraoperative brain relaxation with the use of both these agents. Our results did not show any difference in the grades of brain swelling in both groups (P = 0.884). The majority of patients in both groups had either a relaxed brain or mild brain swelling (Grade I and II). Five patients each in both the groups (19.2% for propofol vs. 21.8% for desflurane) had moderate (Grade III) brain swelling. None of the patients in either group had Grade IV swelling. Only 2 patients (8.69%) in desflurane group required additional measures for reduction in brain swelling (P = 0.88). In desflurane group, one patient received thiopentone boluses along with moderate hyperventilation while another patient was given furosemide. The only study which we could find for this particular surgery was carried out by Cheng et al. wherein they compared desflurane and propofol for brain relaxation after achieving burst suppression.[5] This study revealed that all the patients in both groups had Grade I brain relaxation. The difference in the result between our study and that of Cheng et al. was probably due to the fact that they used a burst suppression dose of anesthetics and we used maintenance dose to achieve adequate depth of anesthesia as guided by entropy values.[5] At target SE of 40–60, it is not possible to achieve burst suppression. Despite this both anesthetic agents provided similar brain conditions in our study. Bhardwaj et al. also found identical brain relaxation scores using entropy guided maintenance dose of propofol and desflurane in patients undergoing surgery for aSAH.[4] However, it would be interesting to study the effect of burst suppression induced at the time of clipping of aneurysm on POCD.
Our results were similar to the trial conducted by Bastola et al. where they compared propofol, sevoflurane, and desflurane as a choice of anesthetic agent in patients undergoing elective supratentorial craniotomy.[2] In their trial in which each group had 25 patients, they did not find any appreciable difference in the relaxation of the brain with the use of any of the three agents (P = 0.70).
Limitations
It is preliminary study and has limitations of its own. First, we have assessed cognitive function at the time of discharge or at 2 weeks period only. Neither preoperative baseline cognitive functions nor long-term cognitive consequences were assessed. Second, we included only those patients in our study who had good SAH grades and excluded poor grade patients. Poor grade patients are more likely to have much more raised ICP and the use of these two agents with different actions on cerebral physiology might show different results from what we observed in the good grade patients. Thus, large studies including poor grade SAH as well, are required in the future to establish the superiority of one anesthetic agent over another in terms of POCD. Moreover, we also need further studies to assess the long-term effects of anesthetic agents on POCD.
CONCLUSION
This preliminary study concludes that both propofol and desflurane are comparable in terms of incidence of postoperative cognitive dysfunction at two weeks. The mean postoperative cognitive scores as well as the executive functions, attention and orientation are better with the use of propofol when compared to desflurane.
Footnotes
How to cite this article: Sharma N, Wig J, Mahajan S, Chauhan R, Mohanty M, Bhagat H. Comparison of postoperative cognitive dysfunction with the use of propofol versus desflurane in patients undergoing surgery for clipping of aneurysm after subarachnoid hemorrhage. Surg Neurol Int 2020;11:174.
Contributor Information
Nanish Sharma, Email: nanish.sharma26@gmail.com.
Jyotsna Wig, Email: jyotsnawig23@googlemail.com.
Shalvi Mahajan, Email: drshalvimahajan@gmail.com.
Rajeev Chauhan, Email: drrajeevchauhan@gmail.com.
Manju Mohanty, Email: manjumohanty2011@gmail.com.
Hemant Bhagat, Email: bhagat.hemant@pgimer.edu.in.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Apfelbaum JL, Lichtor L, Lane BS, Coalson DW, Korttila KT. Awakening, clinical recovery, and psychomotor effects after desflurane and propofol anesthesia. Anesth Analg. 1996;83:721–5. doi: 10.1097/00000539-199610000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Bastola P, Bhagat H, Wig J. Comparative evaluation of propofol, sevoflurane and desflurane for neuroanaesthesia: A prospective randomised study in patients undergoing elective supratentorial craniotomy. Indian J Anaesth. 2015;59:287–4. doi: 10.4103/0019-5049.156868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bedford P. Adverse cerebral effects of anesthesia on old people. Lancet. 1995;2:758–861. doi: 10.1016/s0140-6736(55)92689-1. [DOI] [PubMed] [Google Scholar]
- 4.Bhardwaj A, Bhagat H, Grover VK, Panda NB, Jangra K, Sahu S, et al. Comparison of propofol and desflurane for postanaesthetic morbidity in patients undergoing surgery for aneurysmal SAH: A randomized clinical trial. J Anesth. 2018;32:252–8. doi: 10.1007/s00540-018-2474-z. [DOI] [PubMed] [Google Scholar]
- 5.Cheng MA, Ratnaraj J, McHugh TA. Burst suppression during surgery for cerebral aneurysm: Propofol vs. Desflurane. Anesthesiology. 2002;96:A25. [Google Scholar]
- 6.Engelhard K, Werner C, Reeker W, Lu H, Mollenbery O, Mielke L. Desflurane and isoflurane improve neurological outcome after incomplete cerebral ischaemia in rats. Br J Anaesth. 1999;83:415–21. doi: 10.1093/bja/83.3.415. [DOI] [PubMed] [Google Scholar]
- 7.Ergun R, Akdemir G, Sen S, Tasci A, Ergungor F. Neuroprotective effects of propofol following global cerebral ischemia in rats. Neurosurg Rev. 2000;25:95–8. doi: 10.1007/s101430100171. [DOI] [PubMed] [Google Scholar]
- 8.Glass PS, Gan TJ, Howell S. A review of the pharmacokinetics and pharmacodynamics of remifentanil. Anesth Analg. 1999;89:S7–14. doi: 10.1097/00000539-199910001-00003. [DOI] [PubMed] [Google Scholar]
- 9.Grundmann U, Silomon M, Bach F, Becker S, Bauer M, Larsen B, et al. Recovery profile and side effects of remifentanil-based anaesthesia with desflurane or propofol for laparoscopic cholecystectomy. Acta Anaesthesiol Scand. 2001;45:320–6. doi: 10.1034/j.1399-6576.2001.045003320.x. [DOI] [PubMed] [Google Scholar]
- 10.Gupta A, Stierer T, Zuckermann R, Sakima N, Parker SD, Fleisher LA. Comparison of recovery profile after ambulatory anesthesia with propofol, isoflurane, sevoflurane and desflurane: A systematic review. Anesth Analg. 2004;98:632–41. doi: 10.1213/01.ane.0000103187.70627.57. [DOI] [PubMed] [Google Scholar]
- 11.Hogue CW, Jr, Bowdle TA, O’Leary C, Duncalf D, Miguil R, Pitts M, et al. A multicenter evaluation of total intravenous anesthesia with remifentanil and propofol for elective inpatient surgery. Anesth Analg. 1996;83:279–85. doi: 10.1097/00000539-199608000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Hutter BO, Kreitschmann-Andermahr I, Mayfrank L, Rohde V, Spetzger U, Gilsbach JM. Functional outcome after aneurysmal subarachnoid hemorrhage. Acta Neurochir Suppl. 1999;72:157–74. doi: 10.1007/978-3-7091-6377-1_13. [DOI] [PubMed] [Google Scholar]
- 13.Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K, Zorumski C, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23:876–82. doi: 10.1523/JNEUROSCI.23-03-00876.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Larsen B, Seitz A, Larsen R. Recovery of cognitive function after remifentanil-propofol anesthesia: A comparison with desflurane and sevoflurane anesthesia. Anesth Analg. 2000;90:168–74. doi: 10.1097/00000539-200001000-00035. [DOI] [PubMed] [Google Scholar]
- 15.Lebenbom-Mansour MH, Pandit SK, Kothary SP, Randel GI, Levy I. Desflurane versus propofol anesthesia: A comparative analysis in outpatients. Anesth Analg. 1993;76:936–41. doi: 10.1213/00000539-199305000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Mielck F, Stephan H, Buhre W, Weyland A, Sonntag H. Effects of 1 MAC desflurane on cerebral metabolism, blood flow and carbon dioxide reactivity in humans. Br J Anaesth. 1998;81:155–60. doi: 10.1093/bja/81.2.155. [DOI] [PubMed] [Google Scholar]
- 17.Muzzi DA, Lossaso TJ, Dietz NM. The effect of desflurane and isoflurane on cerebrospinal fluid pressure in humans with supratentorial mass lesions. Anaesthesiology. 1992;76:720–4. doi: 10.1097/00000542-199205000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collins I. The montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 19.Page V, Ely EW. USA, New York: Cambridge University Press; 2011. Delirium in Critical Care; pp. 94–108. [Google Scholar]
- 20.Patel PM, Drummond JC. Cerebral physiology and the effects of anesthetic drugs. In: Miller RD, editor. Miller’s Anesthesia. 7th ed. Vol. 1. Philadelphia, PA: Churchill Livingstone; 2009. pp. 305–40. [Google Scholar]
- 21.Royse CF, Andrews DT, Newman SN, Stygals J, Williams J, Pang J, et al. The influence of propofol or desflurane on postoperative cognitive dysfunction in patients undergoing coronary artery bypass surgery. Anaesthesia. 2011;66:455–64. doi: 10.1111/j.1365-2044.2011.06704.x. [DOI] [PubMed] [Google Scholar]
- 22.Todd MM, Hindman BJ, Clarke WR, Torner JC, Intraoperative Hypothermia for Aneurysm Surgery Trial (IHAST) Investigators. Mild intraoperative hypothermia during surgery for intracranial aneurysm. N Engl J Med. 2005;352:135–45. doi: 10.1056/NEJMoa040975. [DOI] [PubMed] [Google Scholar]
- 23.Vandesteene A, Trempont V, Engelman E. Effect of propofol on cerebral blood flow and metabolism in man. Anaesthesia. 1988;43:42–3. doi: 10.1111/j.1365-2044.1988.tb09067.x. [DOI] [PubMed] [Google Scholar]
- 24.Wong GK, Lam S, Ngai K, Wong A, Mok V, Poon WS, et al. Evaluation of cognitive impairment by the montreal cognitive assessment in patients with aneurysmal subarachnoid haemorrhage: Prevalence, risk factors and correlations with 3-month outcomes. J Neurol Neurosurg Psychiatry. 2012;83:1112–7. doi: 10.1136/jnnp-2012-302217. [DOI] [PubMed] [Google Scholar]
- 25.Yu D, Jiang Y, Gao J, Liu B, Chen P. Repeated exposure to propofol potentiates neuroapoptosis and long-term behavioral deficits in neonatal rats. Neurosci Lett. 2013;534:41–6. doi: 10.1016/j.neulet.2012.12.033. [DOI] [PubMed] [Google Scholar]


