Abstract
Background:
transarticular screw (TAS) fixation without a supplementary posterior construct, even in rheumatoid arthritis (RA) patients, provides sufficient stability with acceptable clinical results. Here, we present our experience with 15 RA patients who underwent atlantoaxial (AA) TAS fixation without utilizing a supplementary posterior fusion.
Methods:
To treat AA instability, all 15 RA patients underwent C1–C2 TAS fixation without a supplementary posterior construct. Patients were followed for at least 24 months. Pre- and postoperative sagittal measures of C1– C2, C2–C7, and C1–C7 angles, atlanto-dens interval (ADI), posterior atlanto-dens interval (PADI), and adjacent segment (i.e., C2–C3) anterior disc height (ADH) were retrospectively recorded from lateral X-ray imaging. The presence or absence of superior migration of the odontoid (SMO), cervical subaxial subluxation, C1–C2 bony fusion, screw pull-out, and screw breakage were also noted.
Results:
There was little difference between the pre- and postoperative studies regarding angles measured. Following TAS fixation, the mean ADI shortened, and mean PADI lengthened. There was no difference in the mean measures of C2–C3 ADH. There was no evidence of SMO pre- or postoperatively. Two patients developed anterior subluxation at C5–C6; one of the two also developed anterior subluxation at C2–C3. All patients subsequently showed C1–C2 bony fusion without screw pull-out or breakage.
Conclusion:
In RA patients who have undergone C1–C2 TAS fixation, eliminating a supplementary posterior fusion resulted in adequate stability.
Keywords: Atlantoaxial, C1–C2, Rheumatoid arthritis, Transarticular screw fixation

INTRODUCTION
The instability of the atlantoaxial (AA) joint can result from aplasia or hypoplasia of the odontoid process, laxity of the transverse ligament, and assimilation of the atlas. AA can be associated with various conditions including Down’s syndrome, Klippel-Feil syndrome, osteogenesis imperfecta, neurofibromatosis, and rheumatoid arthritis (RA).[2] RA in the cervical spine may result in three principal deformities which may occur alone or in various combinations; AA instability, superior migration of the odontoid (SMO), and/or subaxial subluxation. The most common cervical spine abnormality observed in patients with RA is AA instability; it accounts for approximately two- thirds of rheumatoid cervical subluxations.[3]
Many spinal surgeons feel the current gold standard for posterior AA arthrodesis which is transarticular screw (TAS) fixation classically, achieved by the placement of a TAS screw from C2 to the anterior surface of C1 (across the facets, bilaterally).[1] This is typically followed by a Gallie-type block bone-wire posterior construct.[5] Here, we evaluated whether TAS fixation alone in 15 RA patients would provide sufficient stability, allowing for elimination of the additional posterior fusion.
MATERIALS AND METHODS
We retrospectively evaluated the radiographs of 15 consecutive patients (13 females and 2 males), averaging 52 years of age (33–78 years) who underwent bilateral C1– C2 TAS fixation for the treatment of RA-associated AA instability.
Surgical technique
Preoperative planning for screw placement utilized CT-based StealthStation® image guidance (Medtronic Sofamor Danek, Memphis, TN). Parallel caudal stab incisions allowed for delivery of all instruments percutaneously to the posterior arch of C2; we used cannulated 3.5 mm diameter titanium screws (UCSS, Medtronic Sofamor Danek, Memphis, TN). The screw trajectory was confirmed intraoperatively under StealthStation® image guidance and fluoroscopy. Before operative closure, the C1–C2 facet joints were curetted and packed with morselized autologous iliac crest bone graft; no supplementary posterior construct was performed.
Follow-up
Patients were followed an average of 26 months (range 24– 39 months). Pre- and postoperative sagittal cervical X-rays measured; C1–C2, C2–C7, and C1–C7 angles [Figure 1], the atlanto-dens interval (ADI), the posterior atlanto-dens interval (PADI), and adjacent segment (i.e., C2-C3) anterior disc height (ADH). Statistical analysis utilized SAS® software (SAS Institute, Cary, NC).
Figure 1:
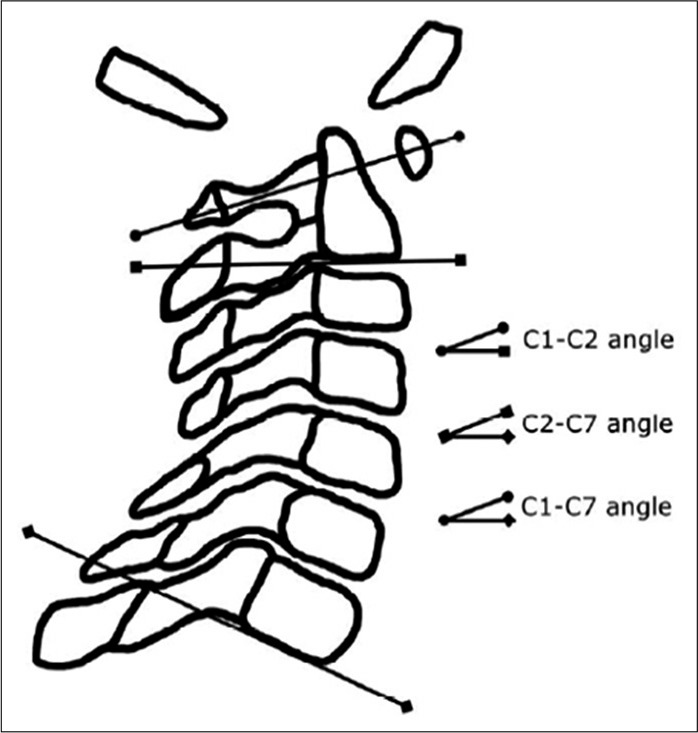
Sagittal C1–C2, C2–C7, and C1–C7 angles were measured between the lines, as shown in this figure.
RESULTS
Compared to the preoperative mean measures, there were no remarkable differences noted in the postoperative fixation, subaxial, and C-spine angles (i.e., the C1–C2, C2–C7, and C1–C7 angles, respectively) [Table 1]. Following C1–C2 TAS fixation, the mean distance for the ADI was shorter, and the mean distance for the PADI was longer. No patient had evidence pre- or postoperatively of SMO nor significant evidence of cervical subaxial subluxation. Two patients developed anterior subluxation at C5–C6, for example, at 27 months and 36 months, respectively (e.g., the latter was associated anterior subluxation at C2–C3). Although immediate corrective surgical intervention was not required in either case, this prompted increased clinical imaging/ surveillance. The final C1–C2 bony fusion rate was 100%, and there were no instances of instrumentation failure.
Table 1:
Pre- and postoperative (n=15) mean angle (degrees) ± standard error of the mean for C1–C2, C2–C7, and C1–C7.

DISCUSSION
Satisfactory clinical outcomes are reported utilizing C1–C2 TAS fixation alone with RA.[4,8] Naderi et al. suggested that the overall stability of the AA segment was increased utilizing as many fixation points as possible.[7] Yoshimoto et al. have reported that for various posterior AA fixation techniques (all of which involved posterior bone-wire or clamp constructs), the C1–C2 fusion angle became somewhat more hyperlordotic leading to subaxial cervical kyphosis.[10] Mukai et al. suggested various biomechanical compensatory changes after C1–C2 TAS fixation in RA; increased C1–C2 lordosis, anterior shift of C2, decreased C2–C7 lordosis, and a tendency of C1 to return to the preoperative angulation.[6] Another study in 38 cases most with posttraumatic AA instability, using a two-point, modified Magerl technique consisting of bilateral TAS fixation with block bone graft, but without a supplementary posterior construct; the fusion rate was comparable fusion to that achieved with a traditional Magerl operation.[1] Further, Wang et al. have reported 100% C1– C2 fusion rate in 57 cases of C1–C2 TAS fixation using morselized autologous bone graft without a supplementary posterior construct in AA patients in with instability (e.g., due to congenital malformations or trauma) rate.[9]
CONCLUSION
Technically satisfactory outcomes of AA segment arthrodesis can be achieved in RA patients using the TAS fixation technique without a supplementary posterior construct.
Footnotes
How to cite this article: Thomas P, Amoo M, Horan J, Husien MB, Cawley D, Nagaria J, et al. Technical outcome of atlantoaxial transarticular screw fixation without supplementary posterior construct for rheumatoid arthritis. Surg Neurol Int 2020;11:188.
Contributor Information
Philip Thomas, Email: philip.thomas@belfasttrust.hscni.net.
Michael Amoo, Email: michaelamoo@rcsi.ie.
Jack Horan, Email: jack.horan@ucdconnect.ie.
Mohammed Ben Husien, Email: mohammenbenhusien@beaumont.ie.
Derek Cawley, Email: derekcawley@hotmail.com.
Jabir Nagaria, Email: jnagaria@gmail.com.
Ciaran Bolger, Email: ciaranbolger@beaumont.ie.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bahadur R, Goyal T, Dhatt SS, Tripathy SK. Transarticular screw fixation for atlantoaxial instability-modified Magerl’s technique in 38 patients. J Orthop Surg Res. 2010;5:87. doi: 10.1186/1749-799X-5-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crockard HA, Stevens JM. Craniovertebral junction anomalies in inherited disorders: Part of the syndrome or caused by the disorder? Eur J Pediatr. 1995;154:504–12. doi: 10.1007/BF02074823. [DOI] [PubMed] [Google Scholar]
- 3.Dreyer SJ, Boden SD. Natural history of rheumatoid arthritis of the cervical spine. Clin Orthop Relat Res. 1999;366:98–106. doi: 10.1097/00003086-199909000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Haid RW, Jr, Subach BR, McLaughlin MR, Rodts GE, Jr, Wahlig JB., Jr C1-C2 transarticular screw fixation for atlantoaxial instability: A 6-year experience. Neurosurgery. 2001;49:65–8. doi: 10.1097/00006123-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Magerl F, Seemann P. Stable posterior fusion of the atlas and axis by trans-articular screw fixation. In: Kehr P, Weidner A, editors. Cervical Spine. Vol. 1. Vienna: Springer-Verlag; 1987. pp. 322–7. [Google Scholar]
- 6.Mukai Y, Hosono N, Sakaura H, Fujii R, Iwasaki M, Fuchiya T, et al. Sagittal alignment of the subaxial cervical spine after C1-C2 transarticular screw fixation in rheumatoid arthritis. J Spinal Disord Tech. 2007;20:436–41. doi: 10.1097/bsd.0b013e318030ca3b. [DOI] [PubMed] [Google Scholar]
- 7.Naderi S, Crawford NR, Song GS, Sonntag VK, Dickman CA. Biomechanical comparison of C1-C2 posterior fixations. Cable, graft, and screw combinations. Spine (Phila Pa 1976) 1998;23:1946–55. doi: 10.1097/00007632-199809150-00005. [DOI] [PubMed] [Google Scholar]
- 8.Nagaria J, Kelleher MO, McEvoy L, Edwards R, Kamel MH, Bolger C. C1-C2 transarticular screw fixation for atlantoaxial instability due to rheumatoid arthritis: A seven-year analysis of outcome. Spine (Phila Pa 1976) 2009;34:2880–5. doi: 10.1097/BRS.0b013e3181b4e218. [DOI] [PubMed] [Google Scholar]
- 9.Wang C, Yan M, Zhou H, Wang S, Dang G. Atlantoaxial transarticular screw fixation with morselized autograft and without additional internal fixation: Technical description and report of 57 cases. Spine (Phila Pa 1976) 2007;32:643–6. doi: 10.1097/01.brs.0000257539.75693.cc. [DOI] [PubMed] [Google Scholar]
- 10.Yoshimoto H, Ito M, Abumi K, Kotani Y, Shono Y, Takada T, et al. A retrospective radiographic analysis of subaxial sagittal alignment after posterior C1-C2 fusion. Spine (Phila Pa 1976) 2004;29:175–81. doi: 10.1097/01.BRS.0000107225.97653.CA. [DOI] [PubMed] [Google Scholar]


