Abstract
Background
The current COVID-19 pandemic has implications on the morbidities of orthopedic patients due to lack of routine follow-ups, and inpatient and outpatient-based interventions. Telemedicine has recently emerged as an alternative for healthcare delivery to the patients and providing them with important information about orthopedic self-care and medications that can be followed without a hospital visit. However, due to lack of physical assessment, telemedicine is bound to have some limitations as well. The aim of this study is to analyze the effectiveness of proactive telemedicine in maintaining follow-up of orthopedic patients, and their satisfaction with telemedicine as an alternative mode of treatment delivery.
Methods
This one-month cross-sectional study enrolled the follow-up patients that visited the orthopedic outpatient-department in February 2020. The patients were sequentially called according to the order of their registration, on a daily basis. Consenting patients were provided with telemedicine-based consultations, and those requiring physical evaluation were called for outpatient visits after documenting the valid reasons. The response-rates and the volume of patients requiring physical visits were measured for different diagnosis-based groups. Patients were asked to complete a questionnaire that included overall patient satisfaction with telemedicine, its effectiveness, and ease in following the telemedicine-based treatment.
Results
The response rate to telemedicine was 88.67%. Among the patients availing telemedicine, 71.43% were managed without needing physical visits to the outpatient-department. The need for physical examination and failed patient-doctor communication were the most common reasons for advising physical outpatient visits. The overall satisfaction-rate to telemedicine was 92%, and only 7.2% of patients had difficulty in understanding or following telemedicine-based advice.
Conclusions
Telemedicine can effectively reduce the need for physical visits to outpatient-departments for follow up of orthopedic patients. The response-rate and overall patient-satisfaction rates to telemedicine are high. Further efforts in expanding the use of telemedicine and addressing its limitations, especially those related to the failed communications, are needed to develop it as an alternative to physical orthopedic consultations in the current situation.
Keywords: COVID-19, Orthopaedics, Patient care, Patient satisfaction, Telemedicine
Introduction
The current COVID-19 pandemic has disrupted the health care services around the world.1 The pandemic has disabled some of the most advanced healthcare systems and will have long term sequelae. The elective surgical procedures and the outpatient-services have been deferred considering the high infectivity rate and transmission of the SARS-Cov-2 virus. However, a longer delay in these services carries an added risk of morbidity to the patients. Moreover, a sudden resumption of these services can result in an abrupt overburdening of the already compromised healthcare services in the coming time foreseeable. As WHO suspects that the COVID-19 risk may remain forever, it may be anticipated that healthcare systems will now have to function with a calculated risk of disease transmission. The crowded outpatient-departments (OPDs) are usual in our country and pose a major challenge in the regularization of the OPD services. A major proportion of the patients attending the outpatient services are follow-up patients, those have been previously clinically evaluated or examined.2 Alternative measures to maintain follow-up of such patients can reduce the overcrowding in the OPDs and help in the maintenance of physical distancing to prevent disease transmission.3 Telemedicine is a potential alternative that has already been used for health care services delivery to rural and remote areas with a lack of transport facilities, for those with socioeconomic limitations and vulnerable patients for whom physical follow-up is inconvenient.4 Telemedicine has been defined by the WHO as the remote delivery of health care services by health care professionals using information and communication technologies for the exchange of valid information for the diagnosis, treatment, and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.5 Telemedicine can be facilitated by various modes of communication like telephone calls, video conferencing, text messages, online chat services often supplemented by internet-based exchange of records based information. However, telemedicine has only been used focally in our country and its effectiveness in maintaining the follow-up of orthopedic patients in India has not been previously analyzed.6 The Medical Council of India (MCI) has recently released the guidelines for practicing telemedicine.7 While it is important to know whether the patients can adjust to the change in practice from physical consultation to telemedicine-based consultations, patient satisfaction is equally important.
The aim of this study is to analyze the effectiveness of proactive telemedicine in maintaining follow-up of orthopedic patients, and their satisfaction with telemedicine as an alternative mode of treatment delivery.
Materials and methods
This cross-sectional observational study was conducted at a tertiary care center after obtaining the clearance from the institutional review board. The orthopedic department of this institute has been providing telemedicine-based services since the announcement of nationwide lockdown due to the current COVID-19 pandemic. At least twenty follow-up patients were called on a daily basis (excluding holidays) between 10:00 a.m. to 2:00 p.m. All follow-up patients that attended orthopedic OPDs during the month of February 2020 were called for telemedicine consultation from April 1, 2020 to April 31, 2020 in the sequence of their registration numbers. Patients not consenting for telemedicine that included those who found the timing of the call or the call itself to be inappropriate, those who were uncontactable, those without internet access for the delivery of the telemedicine prescription, and those who had recently visited or planned a visit to the hospital were excluded. All telemedicine consultations were provided as per national guidelines and were provided free of cost during the aforestated period. All follow-up patients who underwent telemedicine consultations were encouraged to answer a questionnaire-based survey, a week after their telemedicine consultation. The telemedicine consultations and the feedback survey questionnaire were provided to the patients in the language of their choice. Further telemedicine consultations were provided to the patients during the questionnaire-based survey, wherever required.
The mode of communication for telemedicine consultations was the telephonic conversations between the patient and the doctor supplemented by the transfer of photographic-videographic data and document records through internet-based services like email and Whatsapp with a real-time interaction solely between the patient and the doctor and only for the non-emergent purposes. The consultations were provided to the guardians or parents when the patients were minor. Audio consents were sought from all patients (guardians/parents for minor patients) prior to the telemedicine consultation. The doctors delivering telemedicine were orthopedic senior residents and faculties with at least one year of experience in orthopedic practice following completion of their post-graduation. The patient’s presenting complaints and clinical history were enquired and the data was supplemented with the previous clinical records, investigations, and treatment that was saved in electronic records of our hospital. Our institute has been running electronic prescription services and outpatient management information has been stored in the hospital server. Additional records were sought over internet-based services whenever required. Based on these, the patients’ concerns were addressed through health education, rehabilitation via pictorial or video description over the internet, and pharmacological therapy, on an individual basis. A picture of the telemedicine prescription was sent to the patient through email or Whatsapp. In select cases where a need for physical interaction was felt, after documenting the valid reasons, the patients were advised to visit our hospital OPD or any available orthopedic facility in their vicinity, for further evaluation and management. We tried to limit the telephonic conversations to up to 10 min duration for each patient. Based on their past management, the types of follow-up were recorded as: postoperative follow-ups and non-operated follow-ups.
The diagnoses were broadly classified under following umbrella terms based on the major symptoms for which the treatment was sought: back pain and radicular symptoms, cervical disorders, large joint degenerative disorders, treated fracture and dislocations, inflammatory arthropathies, instability, soft tissue injuries, non traumatic soft tissue disorders, osteonecrosis, chronic infection, musculoskeletal tumors, deformities, and others. The indications for the physical presence in OPD were grouped as a) failed communication between the patient and the doctor, where either the doctor or the patient found it difficult to interpret the information given b) need for a physical examination that was needed for further treatment advice, c) insufficient records or those with difficult interpretation, for example physically damaged reports, unclear pictures of records and incomplete records, and d) alarming symptoms where intervention or evaluation needs to be prioritized considering the worsening of the symptoms. The proportions of the patients required physical visits were measured for the reason for the physical visit, for different diagnosis-based categories and for the types of follow-up.
The questionnaire by Acharya et al.8 was used to seek the effectiveness of telemedicine consultations. This questionnaire has been prevalidated and reliability-tested in the Indian population. The questionnaire evaluated the patient’s perspective of the quality of telemedicine service, patient satisfaction, and its shortcomings (Table 1). The questionnaire was translated into the patient’s language of understanding. Patients were given options of verbal (telephonic) mode, email, and WhatsApp for answering the questions. The response rate to telemedicine was recorded as the percentage of patients consenting for telemedicine out of the total patients contacted during the study. The frequency distribution of the binary data of the questionnaire (in the form of ‘yes’ or ‘no’) and overall satisfaction rates of patients in different categories of diagnoses and type of follow-up were measured.
Table 1.
Questionnaire for the patients’ perception of the telemedicine.8
| S.No. | Question | Response |
|---|---|---|
| 1. | Was scheduling of the appointment appropriate? | Yes/No |
| 2. | Was detailed medical history taken? | Yes/No |
| 3. | Are you satisfied with treatment advice through telemedicine? | Yes/No |
| 4. | Did you find telemedicine: a) Feasible b) Convenient c) Both d) No response |
Feasible/Convenient/Both/No response |
| 5 | Would you recommend this service to your friends? | Yes/No |
| 6. | Did you find any difficulty in understanding the process of telemedicine? | Yes/No |
Results
A total of 620 follow-up patients were called for telemedicine consultation between April 1, 2020 and April 30, 2020. One hundred and fourteen patients (18.38%) couldn’t be contacted due to failed connections or non-availability of the patient for attending the phone call. Twenty-nine patients (4.67%) had a lack of access to the internet facility. Twenty-six patients (4.19%) had recently visited or planned a visit to the hospital on their day of calling. One patient has passed away during this follow-up.
The remaining 450 patients (72.58%) were considered for telemedicine consultation. There were 228 female patients and 222 male patients. The mean age was 38.03 ± 16.23 (mean ± standard deviation). Among these, 399 patients (88.67%) gave their consents for telemedicine and 51 (11.33%) opted out of it. Three hundred and ninety-one patients (86.89%) belonged to non-operated follow-up patients. The proportion of patients that required a physical visit to the hospital OPD or any orthopedic facility in their vicinity was 28.57%. The need for physical re-evaluation was least for patients with back pain (10.57%) and cervical pain (9.7%) which together formed diagnoses of 34% of all the patients receiving telemedicine (Table 2). The follow-up patients of fracture and dislocations, large joint degenerative disorders, inflammatory arthropathies, non traumatic soft tissue disorders, chronic infections, and deformities were the ones with a higher need for a physical visit to the OPDs (Table 2). Among the patients requiring outpatient visits, a need for physical examination (70.17%) was the most common indication followed by the failed communication between the doctor and the patients (15.78%) (Table 3). The worsening of the symptoms (alarming symptoms) and difficulty in interpretation or availability of records was observed in 12.28% and 1.7% of the patients receiving the telemedicine consultations, respectively. The detailed results of the telemedicine feedback survey are presented in Table 4. While all those receiving the telemedicine consultation were satisfied with the timing of calls, a major proportion of the patients (103 out of 399, 25.81%) felt that a detailed clinical history was not asked. Thirty-two patients (8.64%) were not satisfied with the telemedicine consultation they received and twenty-nine patients (7.83%) found difficulty in following the same. The overall patient satisfaction rates were high with exceptions in a few groups (Table 5).
Table 2.
Patients response rates and need for physical visit to outpatient departments based on their diagnoses.
| Diagnosis | Number of patients contacted (n = 450) | Patient that opted for telemedicine consultation (n = 399) | Response rate (patients availing telemedicine/patients contacted x 100 | Proportion of the patients receiving telemedicine that required a physical visit to OPD %(n) |
|---|---|---|---|---|
| Back pain and radicular symptoms | 116 (25.7%) | 104 (26.0%) | 89.65% | 10.57% (n = 11, 1 with alarming symptoms) |
| Fracture and dislocations | 87 (19.3%) | 77 (19.2%) | 88.50% | 36.36% (n = 28) |
| Soft tissue injuries | 67 (14.8%) | 59 (14.7%) | 88.05% | 22.03% (n = 13, 3 with alarming symptoms) |
| Large joint degenerative disorders | 51 (11.3%) | 48 (12.0%) | 94.11% | 39.58% (n = 19, 7 with alarming symptoms) |
| Inflammatory arthropathies | 33 (7.3%) | 32 (8.0%) | 96.96% | 40.06% (n = 13, 1 with alarming symptoms) |
| Cervical disorders | 31 (6.8%) | 31 (7.7%) | 100% | 9.67% (n = 3, 1 with alarming symptoms) |
| Non traumatic soft tissue disorders | 30 (6.6%) | 24 (6.0%) | 80% | 54.16% (n = 13, 1 with alarming symptoms) |
| Chronic infection | 15 (3.3%) | 13 (3.2%) | 86.66% | 53.84% (n = 7) |
| Deformities | 10 (2.2%) | 7 (1.7%) | 70% | 71.42% (n = 5) |
| Other conditions | 5 (1.1%) | 1 (0.2%) | 20% | 100% (n = 1) |
| Tumors | 3 (0.6%) | 1 (0.2%) | 33.33 | None |
| Instability | 2 (0.4%) | 2 (0.5%) | 100% | 50% (n = 1) |
| Total | 450 (100%) | 399 (100%) | 88.66% | 28.57% (n = 114, 14 with alarming symptoms) |
Table 3.
Reasons for physical visit to the outpatient department or other orthopaedic facility.
| Reason for advising physical visit to OPD | Number of patients requiring physical visit (n = 114) |
|---|---|
| Failed communications | 15.78% (n = 18) |
| Unclear records or difficult interpretation | 1.7% (n = 2) |
| Need for physical evaluation | 70.17% (n = 80) |
| Alarming symptoms | 12.28% (n = 14) |
Table 4.
Responses from the patients for the telemedicine feedback survey.
| Question/Group | Postoperative (n = 48) | Nonoperative (n = 351) | Total (Yes: No) |
|---|---|---|---|
| Was scheduling of the appointment appropriate? | Yes 48 (100%) No 0 | Yes 351 (100%) No 0 | Yes 399 (100%) No 0 |
| Was detailed medical history taken? | Yes 45 (93.7%) No 3 | Yes 251 (71.5%) No 100 | Yes 296 (74.2%) No 103 |
| Are you satisfied with treatment advice through telemedicine? | Yes 45 (93.7%) No 3 | Yes 322 (91.7%) No 29 | Yes 367 (92%) No 32 |
| Did you find telemedicine: Feasible, Convenient, Both, Not responded | Feasible 13 (27.1%) Convenient 7 (14.6%) Both 28 (58.3) | Feasible 16 (4.6%) Convenient 82 (23.4%) Both 253 (72.0%) | Feasible 29 (7.3%) Convenient 89 (22.3%) Both 281 (70.4%) |
| Would you recommend this service to your friends? | Yes 48 (100%) No 0 | Yes 348 (99.1%) No 3 | Yes 396 (99.2%) No 3 |
| Did you find any difficulty in understanding the process of telemedicine? | Yes 2 (4.2%) No 46 | Yes 27 (7.7%) No 324 | Yes 29 (7.3%) No 370 |
Table 5.
Patient satisfaction rates to telemedicine under different diagnosis based categories.
| Diagnosis | Satisfaction rates to telemedicine |
|---|---|
| Back pain and radicular symptoms | 92.30% (96 out of 104) |
| Cervical disorders | 96.7 (30 out of 31) |
| Large joint degenerative disorders | 87.50% (42 out of 48) |
| Fracture and dislocations | 94.80% (73 out of 77) |
| Inflammatory arthropathies | 87.50% (28 out of 32) |
| Instability | None |
| Soft tissue injuries | 94.91% (56 out of 59) |
| Chronic infection | 100% (13 out of 13) |
| Non traumatic soft tissue disorders | 87.50% (21 out of 24) |
| Tumors | 100% (1 out of 1) |
| Deformities | 71.42% (5 out of 7) |
Discussion
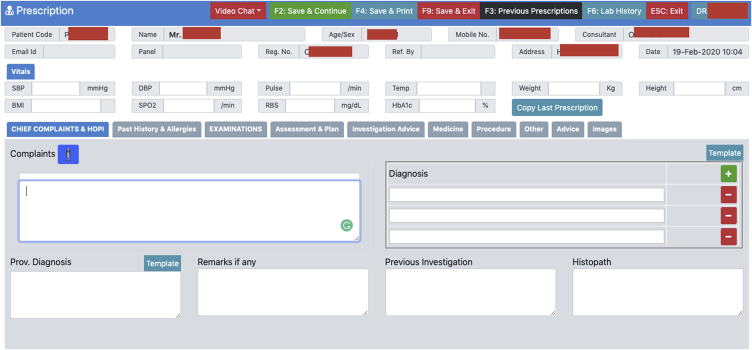
In the current pandemic situation, telemedicine has been emerging as a viable mode of communication between doctors and patients for the clinical assessment as well as for the treatment. The MCI has only recently permitted telemedicine as an alternative mode for treatment advice.7 The basic requirement for the feasibility of telemedicine is access to the telecommunication services that can allow the information transfer between the patient and doctor. While the limitations of telemedicine related to the lack of physical examination and assessment of records are well justifiable for newly presenting patients, the same may not be always applicable to the follow-up patients. A simple knowledge of the progression of the symptoms and general condition of the patient can guide further treatment. Further access to the patient’s previous assessment records, investigations, and previous treatment, which is often available in OPDs maintaining computerized records, can help in an effective telemedicine practice (Fig. 1). This ultimately reduces the physical patient burden in OPDs without affecting the overall reach of patient care.
Fig. 1.
A representative image of a template for the maintenance of electronic records of patients that can help in easy clinical assessment and consultations through telemedicine.
With the widespread use of smartphone and mobile-based internet services, telecommunications have greatly advanced in India.9 While video conferencing applications and video call services have been available, there are limitations due to network coverage, the patients’ unfamiliarity to video calls, and the suitability of their mobile devices for the same.
Our results suggest that telephonic call-based telemedicine in orthopedics can be effectively used as a medium for maintaining the patient follow-up with patient satisfaction rates as high as 92%. Patients with back pain and cervical symptoms which form more than one-third of the follow-up patients can be satisfactorily managed with telemedicine and with minimal need for physical visits. Besides this major proportion of patients with degenerative disorders can also be managed with minimal physical follow-up visits. The overall response rates were high (88.67%) suggesting the interest of patients towards telemedicine. The highest rate of patients requiring physical visits belonged to the patients with deformities, chronic infections, large joint degenerative disorders, and inflammatory arthropathies. The deformity assessment needs physical evaluation to document the progression and correction. It is better to increase the width of follow-up intervals as an effective measure for the convenience of both the doctor and the patients. The chronic infection patients often have chronic wounds that require regular wound dressings and may have a pending surgical intervention. Such patients should be given options for wound management in their vicinity and should be educated regarding the tell-tale signs of acute exacerbations to avoid delay in intervention. The degenerative arthritis of large joints mainly affects the vulnerable elderly patients and it may be difficult for them to understand the telemedicine advice, especially the rehabilitation part and the access to physiotherapy. For these patients as well, the width of follow-up intervals should be increased to reduce their follow-up visits and their attendees should be explained regarding home-based exercises and local therapies to reduce dependency on hospital.10 The probable issue with the inflammatory arthropathy patients requiring physical OPD visits may also be related to a lack of access to physiotherapy and overlapping treatment regimens with rheumatologists. These patients should be advised to consult their rheumatologists for appropriate long duration medical regimen. Home-based exercises should be explained to them and their attendees to reduce dependency on hospital for minor change in symptoms.11 The numbers of patients in other diagnosis based categories were too less to make any inferences.
Inappropriate timing of the phone calls could be a potential cause for lack of interest in telemedicine and could be a contributing factor in some patients opting out of telemedicine in the first instance. It would be more convenient for them if a prior intimation is sent through text, WhatsApp, or an email and they are asked to respond with a convenient time slot. Secondly, around one-fourth of the patients felt that their detailed history was not taken. A preset time-limit assigned for our calls could have probably resulted in this incomplete history recording. Thus, it is important for the treating doctor to anticipate the approximate time allotment for various patients depending on their diagnosis and other available clinical information. Previously, several studies outside India have found telemedicine to be an effective method of administering healthcare services for orthopedic patients.12, 13, 14 It reduces the inconvenience of long travel distance, costs, and added discomfort to the patient. In the current COVID-19 pandemic, telemedicine can help in reducing the physical load on already overburdened orthopedic OPDs and reduce the risk of disease transmission to the patient as well as the doctor. Currently, the estimated patient satisfaction rate with teleconsultations is approximately 70%.14
Both telephonic conversations and videoconference based services have been used previously for delivering telemedicine.14 However, with limited resources and easy access to telephone calls compared to videoconferencing for the patients, the telephonic conversation supplemented by internet-based transfer of pictures and other records can be a cost-effective measure in an Indian scenario. Our results compared well with the patient satisfaction rates in previous studies that analyzed the feasibility of telemedicine in maintaining follow up of orthopaedic patients (Table 6). The need for physical visit was higher in our study which could probably be explained by the diverse group of diagnoses included in our study, telephonic conversations rather than video conferencing, and regional differences in patient understanding and interactions.
Table 6.
Major studies analysing the feasibility of telemedicine in orthopaedic disorders and associated patient satisfaction rates.
| Study and year | Region | Mode of telemedicine | Sample size | Patient satisfaction | Diagnosis or symptoms of patients | Need for physical visit |
|---|---|---|---|---|---|---|
| Couturier P et al. (1998)15 | France | Videoconference | 15 | 80% reported telemedicine as excellent or good | Geriatric orthopaedic rehabilitation | 13% |
| Aarnio P et al. (1999)16 | Finland | Videoconference with document images | 29 | 87% reported telemedicine as good or very good | Mostly back symptoms and joint disorders | NR |
| Wan AC et al. (1999)17 | UK | Videoconference | 146 | 92% - score 8–10 (out of 10) | Pain management, orthopedic disorders, general surgery | NR |
| Haukipuro K et al. (2000)18 | Finland | Videoconference | 76 | 95% patients reported telemedicine as good or very good | Mostly knee and hip arthrosis | NR |
| Williams M et al. (2008)19 | UK | Telephone | 598 | 93% patients were satisfied | Carpal tunnel syndrome | 6.8% |
| Sharareh B et al. (2014)20 | USA | Videoconference | 34 | Mean satisfaction of 9.44 out of 10 | Follow-up after total joint arthroplasty | Nil |
| Sathiyakumar V et al. (2015)21 | USA | Videoconference | 12 | 89% patients satisfied | Trauma follow up | NR |
| Bini SA et al. (2017)22 | USA | Videoconference | 14 | Satisfaction was high and comparable to physical visit | Physical therapy following total knee arthroplasty | 20% |
| Tsvyakh AI et al. (2017)23 | Ukraine | Smartphone application | 48 | 83.1% patients were satisfied | Orthopaedic rehabilitation in lower extremity injuries | NR |
| Shem K et al. (2017)24 | USA | Videoconference | 10 | 100% patients were satisfied | Spinal Cord Injuries follow up | NR |
| Waibel KH et al. (2017)25 | Germany | Smartphone application | 5 | Average satisfaction score of 4.7 out of 5 | Frozen shoulder | NR |
| Buvik A et al. (2019)26 | Norway | Videoconference | 199 | 99% patients were satisfied | Orthopaedic new referred, follow-up after surgery, trauma or chronic disorders | NR |
| Sinha N et al. (2019)27 | Pennsylvania | Videoconference | 101 | Medial satisfaction rate 5 out of 5 | Pediatric fractures | NR |
| Silva M et al. (2019)28 | USA | Videoconference | 26 | 97.8% | nondisplaced pediatric elbow fractures | NR |
| Coronado RA et al. (2020)29 | USA | Telephone | 8 | 100% | Cognitive-behavioral-based physical therapy | NR |
| Kane LT et al. (2020)30 | USA | Videoconference | 33 | 94.1% very satisfied or satisfied | Post operative followup of rotator cuff repair | NR |
| Cheng O et al. (2020)31 | Canada | Videoconference | 32 | 100% patients rated excellent or good | Musculoskeletal issues | NR |
| Gilbert AW et al. (2020)32 | UK | Telephone and video both | 1359∗ - telephone 133∗ - videoconference |
90% patients satisfied with telephone 85% for video |
Orthopedic patients with varying issues | NR |
| Bailey JF et al. (2020)33 | USA | Digital program with an app, videoconference and phone calls | 6468 back pain 3796 knee pain |
Final satisfaction score - 8.97 out of 10 | Followup patients with knee and back pain | NR |
| Current study | India | Telephone | 450 | 92% patient satisfied with telemedicine | Multiple orthopedic issues | 28.57% |
NR = not reported, ∗ Final assessment.
The automated mobile text response based tools can be helpful in grading patient symptoms and administering the modified treatment.34 Patients can be asked to perform maneuvers based on the pictorial information and the patient can “store and forward” their performance in the form of pictures. This forms the basis of virtual clinical examination.35
Telemedicine may sound as promising, but it may be difficult to solely rely upon telemedicine for patient care and the only purpose of telemedicine should be to prioritize patient care when the physical consultation is difficult or needs to be avoided, as in the current pandemic situation. Besides this, patient age, intelligence, lack of supporting devices, poor connectivity limit the applicability of the telemedicine.36 As evident in our results and advocated by the previous studies, a major portion of patients avoided teleconsultation. Privacy issues, trust factors, lack of awareness, difficulty in comprehension can all be implicated and need to be further investigated in the Indian scenario.
There had been some limitations of this study. Firstly, the study is of preliminary nature representing a cross-sectional analysis of patients in one tertiary care center during a month period. The variability of response and the effectiveness of telemedicine can vary from region to region and from time to time. Its effectiveness and patient preferences may change once the current pandemic situation is over. Further long term data is still needed. Secondly, the study discusses the effectiveness and feasibility of one basic mode of telemedicine delivery i.e, proactive telephonic calls supplemented by internet based transfer of information. The other modes may have different outcomes. Thirdly, the effectiveness of telemedicine in new patients cannot be determined, as this study included only follow-up patients. Fourth, since the patients were not charged for the teleconsultations, the cost-effectiveness beyond this study is difficult to determine. Also, the easy availability of patient previous clinical records and investigations which were stored in the hospital data server might have played a major role in easing the telemedicine consultation. Without such a facility, it may be really difficult to address the patient concerns. Lastly, the study does not provide a comparative analysis due to the lack of a control group. Nevertheless, the study provides an insight into the role of telemedicine in the effective maintenance of orthopedic follow-up in these times of unexpected necessity and which may further evolve as a major mode of medical care.
The pattern of the orthopedic disorders and their response to telemedicine can help the orthopedicians in prioritizing outpatient-care. The basic minimum requirement of a phone and internet can be used in the efficient delivery of telemedicine in orthopedic patients.
Conclusion
The telemedicine-based consultations can effectively reduce the need for physical visits to outpatient departments for the follow-up of orthopaedic patients, especially when patients’ previous clinical information has been available to the treating doctor. The response rate and overall patient satisfaction rates to telemedicine are high. Efforts should be made to strengthen and facilitate telemedicine-based medical care by spreading awareness, computerization of patient records, and maximize the use of technology in patient care to reduce the physical burden on outpatient departments, and to minimize the risk of disease transmission in current COVID-19 pandemic.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Declaration of competing interest
None of the authors have any conflicts to declare.
Contributor Information
Sandeep Kumar, Email: drsandeepkumar20@gmail.com.
Arvind Kumar, Email: arvindmamc@gmail.com.
Mukesh Kumar, Email: drmukesh1.pmch@gmail.com.
Ashok Kumar, Email: drashok.sgpgims@gmail.com.
Rajesh Arora, Email: rajeshmamc@gmail.com.
Rakesh Sehrawat, Email: drrsehrawat@gmail.com.
References
- 1.WHO Coronavirus disease 2019 (COVID-19) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Date accessed: May 24, 2020.
- 2.Gani A., Bhat S., Gupta A. Pattern & prevalence of orthopaedic outdoor patients at a tertiary level care hospital in jammu, India. JK Sci. 2016;18(3):155–158. [Google Scholar]
- 3.Lal H., Sharma D.K., Patralekh M.K., Jain V.K., Maini L. Out Patient Department practices in orthopaedics amidst COVID-19: the evolving model. J Clin Orthop Trauma. 2020 doi: 10.1016/j.jcot.2020.05.009. [published online ahead of print, 2020 May 18] 10.1016/j.jcot.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Orlando J.F., Beard M., Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS One. 2019;14(8) doi: 10.1371/journal.pone.0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. 2009. https://www.who.int/goe/publications/goe_telemedicine_2010.pdf Date accessed: May 24, 2020.
- 6.Chellaiyan V.G., Nirupama A.Y., Taneja N. Telemedicine in India: where do we stand? J Fam Med Prim Care. 2019;8(6):1872–1876. doi: 10.4103/jfmpc.jfmpc_264_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Board Of Governors In supersession of the Medical Council of India Telemedicine practice guidelines. https://www.mohfw.gov.in/pdf/Telemedicine.pdf Date accessed: May 24, 2020.
- 8.Acharya R.V., Rai J.J. Evaluation of patient and doctor perception toward the use of telemedicine in Apollo Tele Health Services, India. J Fam Med Prim Care. 2016;5(4):798–803. doi: 10.4103/2249-4863.201174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Angrish S., Sharma M., Bashar M.A. How effective is the virtual primary healthcare centers? An experience from rural India. J Fam Med Prim Care. 2020;9(2):465–469. doi: 10.4103/jfmpc.jfmpc_1124_19. Published 2020 Feb 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Odole A.C., Ojo O.D. A telephone-based physiotherapy intervention for patients with osteoarthritis of theknee. Int J Telerehabilitation. 2013;5(2):11–20. doi: 10.5195/ijt.2013.6125. Published 2013 Dec 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Warmington K., Flewelling C., Kennedy C.A. Telemedicine delivery of patient education in remote Ontario communities: feasibility of an Advanced Clinician Practitioner in Arthritis Care (ACPAC)-led inflammatory arthritis education program. Open Access Rheumatol. 2017;9:11–19. doi: 10.2147/OARRR.S122015. Published 2017 Feb 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lamminen H., Nevalainen J., Alho A., Lindholm T.S., Tallroth K., Lepistö J. Experimental telemedicine in orthopaedics. J Telemed Telecare. 1996;2(3):170–173. doi: 10.1258/1357633961930013. [DOI] [PubMed] [Google Scholar]
- 13.Anthony C.A., Volkmar A., Shah A.S. Communication with orthopedic trauma patients via an automated mobile phone messaging robot. Telemed J e Health. 2018;24:504–509. doi: 10.1089/tmj.2017.0188. [DOI] [PubMed] [Google Scholar]
- 14.Behmanesh A., Sadoughi F., Mazhar F.N., Joghataei M.T., Yazdani S. Tele-orthopaedics: a systematic mapping study. J Telemed Telecare. 2020 doi: 10.1177/1357633X20919308. [published online ahead of print, 2020 May 11] 1357633X20919308. [DOI] [PubMed] [Google Scholar]
- 15.Couturier P., Tyrrell J., Tonetti J., Rhul C., Woodward C., Franco A. Feasibility of orthopaedic teleconsulting in a geriatric rehabilitation service. J Telemed Telecare. 1998;4(Suppl 1):85–87. doi: 10.1258/1357633981931597. [DOI] [PubMed] [Google Scholar]
- 16.Aarnio P., Lamminen H., Lepistö J., Alho A. A prospective study of teleconferencing for orthopaedic consultations. J Telemed Telecare. 1999;5(1):62–66. doi: 10.1258/1357633991932405. [DOI] [PubMed] [Google Scholar]
- 17.Wan A.C., Gul Y., Darzi A. Realtime remote consultation in the outpatient clinic--experience at a teaching hospital. J Telemed Telecare. 1999;5(Suppl 1):S70–S71. doi: 10.1258/1357633991932621. [DOI] [PubMed] [Google Scholar]
- 18.Haukipuro K., Ohinmaa A., Winblad I., Linden T., Vuolio S. The feasibility of telemedicine for orthopaedic outpatient clinics--a randomized controlled trial. J Telemed Telecare. 2000;6(4):193–198. doi: 10.1258/1357633001935347. [DOI] [PubMed] [Google Scholar]
- 19.Williams M., Amin A., Getgood A., Hallam P., Chojnowski A.J., Chapman P.G. Telephone clinic follow-up following carpal tunnel decompression. J Hand Surg Eur. 2008;33(5):641–644. doi: 10.1177/1753193408090124. [DOI] [PubMed] [Google Scholar]
- 20.Sharareh B., Schwarzkopf R. Effectiveness of telemedical applications in postoperative follow-up after total joint arthroplasty. J Arthroplasty. 2014;29(5):918–922. doi: 10.1016/j.arth.2013.09.019. e1. [DOI] [PubMed] [Google Scholar]
- 21.Sathiyakumar V., Apfeld J.C., Obremskey W.T., Thakore R.V., Sethi M.K. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J Orthop Trauma. 2015;29(3):e139–e145. doi: 10.1097/BOT.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 22.Bini S.A., Mahajan J. Clinical outcomes of remote asynchronous telerehabilitation are equivalent to traditional therapy following total knee arthroplasty: a randomized control study. J Telemed Telecare. 2017;23(2):239–247. doi: 10.1177/1357633X16634518. [DOI] [PubMed] [Google Scholar]
- 23.Tsvyakh A.I., Hospodarskyy A.J. Telerehabilitation of patients with injuries of the lower extremities. Telemed J e Health. 2017;23(12):1011–1015. doi: 10.1089/tmj.2016.0267. [DOI] [PubMed] [Google Scholar]
- 24.Shem K., Sechrist S.J., Loomis E., Isaac L. SCiPad: effective implementation of telemedicine using iPads with individuals with spinal cord injuries, a case series. Front Med. 2017;4(58) doi: 10.3389/fmed.2017.00058. Published 2017 May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waibel K.H., Cain S.M., Hall T.E., Keen R.S. Multispecialty synchronous telehealth utilization and patient satisfaction within regional health command Europe: a readiness and recapture system for health. Mil Med. 2017;182(7):e1693–e1697. doi: 10.7205/MILMED-D-16-00368. [DOI] [PubMed] [Google Scholar]
- 26.Buvik A., Bugge E., Knutsen G., Småbrekke A., Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare. 2019;25(8):451–459. doi: 10.1177/1357633X18783921. [DOI] [PubMed] [Google Scholar]
- 27.Sinha N., Cornell M., Wheatley B., Munley N., Seeley M. Looking through a different lens: patient satisfaction with telemedicine in delivering pediatric fracture care. J Am Acad Orthop Surg Glob Res Rev. 2019;3(9) doi: 10.5435/JAAOSGlobal-D-19-00100. Published 2019 Sep. 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silva M., Delfosse E.M., Aceves-Martin B., Scaduto A.A., Ebramzadeh E. Telehealth: a novel approach for the treatment of nondisplaced pediatric elbow fractures. J Pediatr Orthop B. 2019;28(6):542–548. doi: 10.1097/BPB.0000000000000576. [DOI] [PubMed] [Google Scholar]
- 29.Coronado R.A., Sterling E.K., Fenster D.E. Cognitive-behavioral-based physical therapy to enhance return to sport after anterior cruciate ligament reconstruction: an open pilot study. Phys Ther Sport. 2020;42:82–90. doi: 10.1016/j.ptsp.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 30.Kane L.T., Thakar O., Jamgochian G. The role of telehealth as a platform for postoperative visits following rotator cuff repair: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2020;29(4):775–783. doi: 10.1016/j.jse.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 31.Cheng O., Law N.H., Tulk J., Hunter M. Utilization of telemedicine in addressing musculoskeletal care gap in long-term care patients. J Am Acad Orthop Surg Glob Res Rev. 2020;4(4) doi: 10.5435/JAAOSGlobal-D-19-00128. e19.00128. Published 2020 Apr 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gilbert A.W., Billany J.C.T., Adam R. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual. 2020;9(2) doi: 10.1136/bmjoq-2020-000985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bailey J.F., Agarwal V., Zheng P. Digital care for chronic musculoskeletal pain: 10,000 participant longitudinal cohort study. J Med Internet Res. 2020;22(5) doi: 10.2196/18250. Published 2020 May 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martínez-Ramos C., Cerdán M.T., López R.S. Mobile phone-based telemedicine system for the home follow-up of patients undergoing ambulatory surgery. Telemed J e Health. 2009;15(6):531–537. doi: 10.1089/tmj.2009.0003. [DOI] [PubMed] [Google Scholar]
- 35.Tanaka M.J., Oh L.S., Martin S.D., Berkson E.M. Telemedicine in the era of COVID-19: the virtual orthopaedic examination [published online ahead of print, 2020 Apr 24] J Bone Joint Surg Am. 2020 doi: 10.2106/JBJS.20.00609. 10.2106/JBJS.20.00609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Board on Health Care Services; Institute of Medicine . Vol. 4. National Academies Press (US); Washington (DC): 2012 Nov 20. https://www.ncbi.nlm.nih.gov/books/NBK207146/ (The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary). Challenges in Telehealth. Available from: [PubMed] [Google Scholar]