Abstract
Health and healthcare disparities are variances in the health of a population or the care rendered to a population. Disparities result in a disproportionately higher prevalence of disease or lower standard of care provided to the index group. Multiple theories exist regarding the genesis of this disturbing finding. The COVID-19 pandemic has had the unfortunate effect of amplifying health inequity in vulnerable populations. African Americans, who make up approximately 12% of the US population are reportedly being diagnosed with COVID-19 and dying at disproportionately higher rates. Viewed holistically, multiple factors are contributing to the perfect storm: 1) Limited availability of public testing, 2) A dramatic increase in low wage worker unemployment/health insurance loss especially in the service sector of the economy, 3) High rates of preexisting chronic disease states/reduced access to early healthcare and 4) Individual provider and structural healthcare system bias. Indeed, COVID-19 represents a pandemic superimposed on a historic epidemic of racial health inequity and healthcare disparities. Therapeutic solutions are not expected in the near term. Thus, identifying the genesis and magnitude of COVID-19's impact on African American communities is the requisite first step toward crafting an immediate well designed response. The mid and long term approach should incorporate population health based tactics and strategies.
Introduction
Health and healthcare disparities are variances in the health of a population or the care rendered to a population. Disparities result in a disproportionately higher prevalence of disease or a lower standard of care provided to the index group. Multiple theories exist regarding the genesis of this disturbing finding.
Structural societal issues such as historical redlining policies affecting residential housing and neighborhood safety, public school quality, access to healthy foods and livable wage employment opportunities directly impact health from birth. The impact of these environmental challenges may dramatically influence an affected individual's health over the course of their life.1 In metropolitan areas, the difference of several miles and a change of zip codes may be associated with an increase in the prevalence of chronic disease and consequent shortened lifespans amongst the residents of poorer communities.2
In the best of times, chronic diseases such as diabetes, hypertension, coronary artery disease, kidney disease, cancer, stroke and other conditions occur with higher prevalence in Blacks.3 Consequently, on either end of life, Blacks experience both higher rates of infant mortality and shorter life expectancies relative to their White counterparts.4
Structural Racism's impact on COVID-19
SARS-CoV-2 is responsible for COVID-19, a contagious respiratory illness. The first reported case is believed to have originated in Wuhan, China. The World Health Organization has designated the COVID-19 Pandemic a Public Health Emergency of International Concern.5 Two factors are associated with increased susceptibility to COVID-19: advanced age and underlying chronic medical conditions.6 , 7
The COVID-19 pandemic has had the unfortunate effect of amplifying health inequity in vulnerable populations. African Americans, who make up approximately 12% of the US population are reportedly being diagnosed with COVID-19 and dying at disproportionately higher rates. The early data reveals this alarming trend to be occurring in various parts of the country ( Table 1 ).8, 9, 10, 11
Table 1.
Demonstrates African Americans as a percentage of the population, the percentage of COVID-19 confirmed cases in African Americans, and fatalities as a percentage of all residents in 4 states of the United States of America.
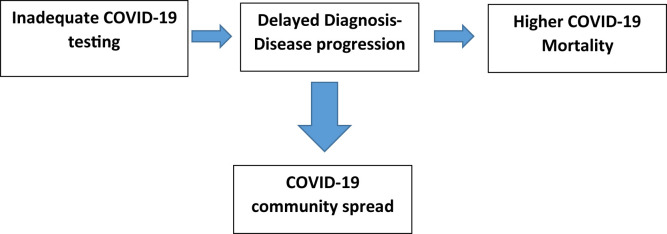
The lack of definitive data on testing rates, confirmed cases and mortality highlight issues around COVID-19 race/ethnic data collection and reporting process at the local, state and federal level through the CDC.12 , 13 Indeed, the CDC's data collection form for patients under investigation and confirmed case reports requests ethnic demographics.14 However, in some states, racial and ethnic data has been reported to be unavailable in up to 40% of confirmed cases.14 Unfortunately, the fact that not all local, state and federal public health agencies are collecting race and ethnic data points will contribute to delays in reaching a complete understanding of the magnitude of this pandemic's impact on Black communities (Figure 1 ). However, it is clear that the finding that COVID-19 is disproportionately afflicting and killing more African Americans is more than a statistical aberrancy. Accurate public reporting of tests administered, confirmed positive results and patient outcomes for Blacks will allow strategic planning and public health efforts to be effectively and equitably deployed and implemented.
Figure 1.
Limited/delayed access to COVID-19 testing results in progression to advanced disease presentation-worse outcomes or asymptomatic or mild disease states transmitting within the Black community.
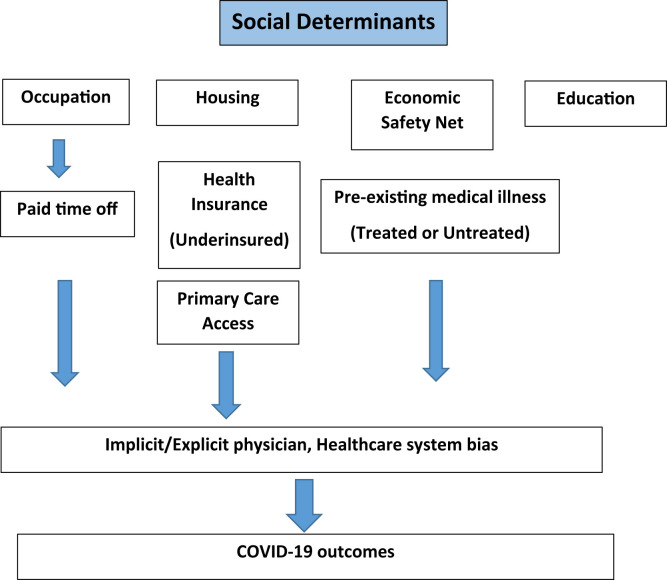
The finding of disparate health outcomes in African Americans is not a novel concept. For years it has been scientifically validated and accepted that where we live, where we learn, work and play all fundamentally affect our personal health including the prevalence of chronic health conditions (Figure 2 ).15
Figure 2.
Social determinant of illness model.
Of all measures of socioeconomic status (SES), educational attainment is perhaps the single best indicator that has the most consistent association with metrics of health including all cause and cause specific mortality.16 Low SES is associated with the earlier onset of chronic medical conditions, on average 10–15 years sooner than high SES communities.17
Minorities including African Americans disproportionately represent service industry workers including early care and education, restaurant workers, food processors. These individuals experience disproportionately higher levels of COVID-19 exposure as a result of high rates of public interaction. Defying public health recommendations during the COVID-19 pandemic, where “physical distancing” has been mandated legislatively is not an option for these “essential worker” groups.
Stratifying across economic levels, 93% of highest wage earners (top 10%) were able to earn paid sick days whereas only 30% of lowest earners (bottom 10%) were able to earn sick days.18 , 19 This fundamental shortcoming in worker benefits denies minorities, including Blacks, the privilege of sheltering in place and working from home. Additionally, in metropolitan areas like Chicago, Detroit and New Orleans, lower income workers disproportionally rely upon mass public transportation at a greater rate.
Currently up to 27 million Americans are uninsured.20 However, health insurance coverage is not the sole determinant of healthcare outcomes.21 Insurance status notwithstanding, African Americans are more likely to have a Medicaid health insurance product which may provide them with limited access to primary care physicians and no broad-based healthcare benefits portfolio. Moreover, low wage service workers are less likely to have uninterrupted healthcare insurance due to job transitions rendering them “underinsured”.21
Viewed holistically multiple factors are contributing to the perfect storm: 1) Limited availability of public testing, 2) A dramatic increase in low wage worker unemployment/health insurance loss especially in the service sector of the economy, 3) High rates of pre-existing chronic disease states/reduced access to early healthcare and 4) Individual and structural healthcare system bias.
Once hospitalized, Black patients are vulnerable to the impact of implicit and explicit healthcare provider bias. Stereotypes and biases are more likely to affect decision making in times of emotional stress and anxiety-both of which are more likely in the COVID-19 surge and peak phase when providers and the healthcare system are stretched to capacity. All human beings harbor bias of some sort and it is only with the acknowledgment of this fact that we can effectively manage ourselves.22
Bias may occur from the time when decisions regarding the “selective” offering of COVID-19 testing to individuals are made all the way across the care spectrum to the point of deciding who will be intubated and in whom care is going to be withdrawn because of perceived “futility of further care”. Bias can be mitigated by the application of evidence based protocols that provide guidance with enough leeway for judicious application of prudent physician clinical judgment. Triage teams which employ a team of clinicians including a bio-ethicist may be helpful to mitigate the ‘moral burden’ of a single physician making critical decisions on their own.
Accurate and timely documentation of the exact number of tests performed, confirmed COVID-19 cases and fatalities within the Black population is the essential first step. This must occur at the municipal, state and federal level and mandates should be issued to private testing laboratories as more testing is relegated to private entities. This should be extended to new testing methods, like plasma antibody serology testing, as they come online. In the interest of transparency, these data should be reported to the public at all levels including by the CDC.
Discussion and next steps
With the detrimental impact of social determinants of health in mind, testing that is available to the public, but not accessible to some communities is ineffective for identifying problematic areas and performing contact tracing and other public health initiatives to mitigate the spread of COVID-19 infection. Until therapeutics are available in the form of vaccinations, a strategic and broad-based public health approach will continue to be the centerpiece approach to COVID-19.
To overcome limiting geographic factors such as a dependence on public transportation, as public testing is accelerated, efforts should be focused on locating the testing centers within underserved neighborhoods. Effective advertising campaigns will be needed to overcome the historic distrust associated with population testing and perceived stigma of positive test results. Media reports have documented the circulation of “urban myths” that young blacks are not susceptible to COVID-19 and that only the elderly are effected. Instead, in a population where a disproportionate number of individuals suffer from diabetes, hypertension and other chronic conditions earlier in life; campaigns should focus on dispelling such myths. Faith based organizations should play a role in disseminating this information. Visible community leaders should be called upon. African American health providers who are known to the community and have established trusting relationships should be active in disseminating important, timely and accurate healthcare messaging.
The understanding of clinical immunity following COVID-19 infection and the role, if any, that accurate serum plasma testing plays will be a critical step. Communicating that those who have suffered and resolved the disease, sometimes with mild or no symptoms, will have the ability to return to work more easily and to resume daily life is crucial to family economic viability and stimulating the local economic community. Wide scale COVID-19 testing, contact tracing of those found positive for infection and timely quarantining of contacts will require equitable distribution of Federal funding to build out a robust public health tracing program.
On the behalf of healthcare institutions servicing disproportionately impacted Black communities, motivation exists beyond the fact that there is a “moral imperative” to treat all populations with equal care. A profound business case can be made that improving care within underserved groups will reduce emergency department visits, hospitalizations for costly advanced stage COVID-19 presentations and allow healthcare facilities to emerge from the COVID-19 fog and resume a more normal business pattern.
Indeed, COVID-19 represents a pandemic superimposed on a historic epidemic of health and healthcare disparities. Given the fact that therapeutics solutions are not expected in the near term-identifying the genesis and magnitude of COVID-19's impact on African American communities is the requisite first step toward crafting and immediate response. The mid and long term approach should incorporate population health based tactics and strategies.
Disclosures
None
Acknowledgment
This study was supported by Walter W Buckley Endowment.
Acknowledgements
The authors declare no relevant industry financial disclosures or conflicts of interest.
References
- 1.Jones N.L., Gilman S.E., Cheng T.L., Drury S.S., Hill C.V., Geronimus A.T. Life course approaches to the causes of health disparities. Am J Publ Health. 2019;109(S1):S48–S55. doi: 10.2105/AJPH.2018.304738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.https://www.rwjf.org/en/library/interactives/whereyouliveaffectshowlongyoulive.html. Last accessed 23 April 2020.
- 3.Thorpe R.J., Wynn A.J., Walker J.L. Relationship between chronic conditions and disability in African American men and women. J Natl Med Assoc. 2016;108(1):90–98. doi: 10.1016/j.jnma.2015.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bond M Jermane, Herman Allen A. Lagging life expectancy for black men: a public health imperative. Am J Publ Health. 2016;106(7):1167–1169. doi: 10.2105/AJPH.2016.303251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO director-general's statement on IHR emergency committee on novel Coronavirus (2019-nCoV) 2019. https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov
- 6.Munster V.J., Koopmans M., van Doremalen N., van Riel D., de Wit E. A Novel Coronavirus Emerging in China – Key Questions for Impact Assessment. N Engl J Med. 2020;382:692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- 7.https://www.cdc.gov/mmwr/volumes/69/wr/mm6913e2.htm?s_cid=mm6913e2_x. Last accessed 23 April 2020.
- 8.https://www.dph.illinois.gov/covid19/covid19-statistics. Last accessed 23 April 2020.
- 9.https://www.michigan.gov/coronavirus/0,9753,7-406-98163_98173---,00.html. Last accessed 23 April 2020.
- 10.https://www.census.gov/quickfacts/fact/table/LA/PST045219. Last accessed 23 April 2020.
- 11.http://ldh.la.gov/Coronavirus/. Last accessed 23 April 2020.
- 12.https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/testing-in-us.html. Last accessed 23 April 2020.
- 13.https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html#investigation. Last accessed 23 April 2020.
- 14.https://www.cdc.gov/coronavirus/2019-ncov/downloads/pui-form.pdf. Last accessed 23 April 2020.
- 15.Hales C.M., Fryar C.D., Carroll M.D., Freedman D.S., Aoki Y., Ogden C.L. Differences in obesity prevalence by demographic characteristics and urbanization level among adults in the United States, 2013-2016. J Am Med Assoc. 2018;319(23):2419–2429. doi: 10.1001/jama.2018.7270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elo I. Social Class Differentials in health and mortality: patterns and explanations in comparative perspective. Annu Rev Sociol. 2009;35(1):553–572. [Google Scholar]
- 17.Crimmins E.M., Hayward M.D., Seeman T.E. Race/ethnicity, socioeconomic status and health. In: Anderson N.B., Bulatao R.A., Cohen B., editors. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Natl. Acad. Press; Washington, DC: 2001. pp. 310–352. [Google Scholar]
- 18.Bureau of Labor and Statistics . March 2019. Employee Benefits in the US. (Bls.gov) [Google Scholar]
- 19.Census.gov. Last accessed 23 April 2020.
- 20.Heeju S. Racial and ethnic disparities in health insurance coverage: dynamics of gaining and losing coverage over the life-course. Popul Res Pol Rev. 2017 April;36(2):181–201. doi: 10.1007/s11113-016-9416-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Woolhandler S., Himmelstein D.U. Life or debt: underinsurance in America. J Gen Intern Med. 2013;28(9):1122–1124. doi: 10.1007/s11606-013-2460-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams David R., Cooper Lisa A. Reducing racial inequities in health: using what we already know to take action. Int J Environ Res Publ Health. 19 Feb. 2019;16(4):606. doi: 10.3390/ijerph16040606. [DOI] [PMC free article] [PubMed] [Google Scholar]