Abstract
Background
The aim of this study was to evaluate the impact of clinical closure and delayed orthodontic care delivery in terms of types of emergencies, pain intensity, and disability experienced by orthodontic patients during the COVID-19 pandemic.
Methods
This was a descriptive cross-sectional study using an electronic survey that was distributed to orthodontic patients who were not seen in clinic for 2 to 3 months due to clinic closure. The survey included demographics, types of orthodontic emergencies, Numerical Rating Scale, and Manchester Orofacial Pain Disability Scale.
Results
There were a total of 150 respondents with mean age of 20 years; 57.33% were female patients. The most common reported orthodontic emergencies were poking wire 30%, debonded brackets 27.3%, bad odor 24%, sharp ligature tie 20%, inflammation and bleeding 9.3%, ulcer 8.7%, and problematic palatal device 8%. Pain was significantly associated with poking wire (P < 0.001), sharp ligature tie (P < 0.01), ulcer (P < 0.05), and problematic palatal device (P < 0.01). Poking wire, sharp ligature tie, and problematic palatal device were found to be significant predictors of pain intensity. Median pain intensity was 3, similar to the median disability score. There was a significant association between pain intensity and disability score (P < 0.01). With each unit increase in pain intensity, the disability score increased by 1.18.
Conclusions
Delay in receiving orthodontic care could result in an orthodontic emergency, yet pain and disability resulting from these events are minimal. The decision to resume clinical service should be evaluated considering risks and benefits in case of the pandemic. Further studies are required.
Keywords: Disability, Disease outbreak, Emergency, Orthodontics, Pain
1. Introduction
The novel coronavirus disease 2019 (COVID-19) was announced as a public health emergency of international concern by the World Health Organization (WHO) on March 13, 2020 [1]. Since the emergence of the disease in late December 2019, it became a pandemic and spread out widely affecting more than 200 countries and territories [2,3]. Number of global confirmed cases reached (13,378,853) with total deaths exceeding half a million by July 17, 2020. The highest reported cases were in the United States (3,405,494) followed by Brazil (1,926,824) and India (968,876), respectively [3]. This disease has a high transmissibility rate that can spread by fomite, aerosol, and droplet [4]. Symptoms can vary from asymptomatic, mild, moderate, severe, to critical [5]. Asymptomatic carriers, including children, were reported in several studies [6,7]. Incubation period was reported as high as 14 days that could reach up to 24 days [8,9]. Furthermore, this virus could remain viable in aerosol for up to 3 hours with half-life of more than 5 hours on stainless steel and plastic surfaces [10]. This presents a potential risk of treating patients during their latency yet contagious period or asymptotic carriers. This is especially alarming for orthodontists who tend to see high volumes of patients in a short period of time.
To control transmission of this highly infectious disease, strict infection control measures were recommended. Personal protective equipment, including eye and face protection, aspirator mask, and reduction of aerosol-producing procedures were advised [9,11]. Several orthodontic procedures produce a significant amount of aerosol, including preparation for bonding, debonding, scaling, and adjustment of appliance [12]. Even more, any procedure that elicits the gag reflex, such as impression taking, could provoke coughing or vomiting, which could spread infection [13].
Efforts to contain COVID-19 and minimize the risk of cross-transmission have been implemented by multiple countries [14]. This includes quarantine measures, dusk-to-dawn curfew, and 24-hour lockdown, with particular emphasis on social distancing [15]. Among these measures are country-level closure of dental services except for emergency treatment [11]. Pulpitis, abscess, and dental trauma were reported to be the main dental emergencies presented to clinics during the pandemic [16]. Orthodontic emergencies occasionally occur and they represent urgencies rather than emergencies. Pain and discomfort are the main reported emergencies experienced during orthodontic treatment [17,18].
In orthodontic practice, patients present to clinic regularly for activation of appliance and continuity of care. Between visits, patients could experience adverse events, including pocking wire, irritation, pain, or appliance breakage [19]. These adverse events are not considered true emergencies yet require prompt action to assure the patient and alleviate discomfort [19].
As a result of the clinical closure implemented during the COVID-19 crisis, access to orthodontic facilities and care delivery to active patients were restricted. The aim of this study was to evaluate the impact of clinical closure and delayed orthodontic care delivery in terms of types of emergencies, pain intensity, and disability experienced by orthodontic patients during the COVID-19 pandemic.
2. Material and methods
This study was reviewed and approved by the Research Ethical Committee at the Faculty of Dentistry, King Abdulaziz University (KAUFD). This is a descriptive cross-sectional study that was performed in 2020, after 2 months of clinical closure because of the COVID-19 outbreak. A convenient sampling method was implemented to include patients who visited orthodontic screening clinic at KAUFD and University Dental Hospital. An anonymous electronic survey in the Arabic language was created and sent out to registered contacts of patients and patients’ guardians.
The first part of the survey included an outline describing aim of the research with a consent form. Participation was voluntary and anonymous with no patient identifiers required. Confirmation for willingness to participate in the research was mandatory to proceed to survey content. Any patient who selected “No, I am not willing to participate” was automatically directed out of the survey. Next, a confirmation statement of current active treatment or retention was necessary to proceed. Patients who were not undergoing active orthodontic treatment or orthodontic retention were excluded.
The second part of the survey was dedicated to demographic questions, including age, gender, and educational background. This was followed by questions related to participants’ orthodontic treatment, including type of orthodontic appliance (fixed, removable, clear aligner, retainer), when was their last orthodontic visit, and any current orthodontic problem. A list of the most common orthodontic emergencies was provided as a checklist and participants were required to select all answers that applied to him or her, including debonded bracket, long poking wire, sharp end of ligature tie, broken fixed retainer, broken or loose expander, lost or broken removable retainer, oral ulcer, inflammation, swelling, exudate, bleeding, bad odor, or others. Each item in the list was accompanied by an illustrative image for simplification purposes.
The third part of the survey used the translated Arabic version of the validated Manchester Orofacial Pain Disability Scale (MOPDS) [20]. This is a self-administered specific measure for disability and intensity of pain related to the orofacial region within the past month. It consists of a 26-item questionnaire covering 2 components: 7-item physical and 19-item psychological disabilities. Scoring of each item uses a 3-item Likert scale: 0 = none of the time, 1 = on some days, 2 = on most/every day. This questionnaire was developed for all age groups and was found to be valid among the UK population. A final score is then derived from the sum of scores for each disability item ranging from 0 to 52, with the highest score of 52 indicating worst pain-related disability, 26 is moderate, and 0 indicates no pain-related disability. The questionnaire has 2 binary yes/no questions related to history of pain in the face, mouth, or jaws for more than 24 hours in the past month, and if any professional advice was sought for this pain.
Because there was no validated translated Arabic version of MOPDS, translation of the scale was done following the process of translation and adaptation of instruments recommended by WHO [21]. This process included forward-translations and bilingual expert panel back-translations. Comparison of the original and back-translated versions was performed and discussed by the author, to ensure accuracy and equivalence. Last, the average pain intensity was measured using the Numerical Rating Scale (NRS-11) [22]. It is a segmented numerical scale on a horizontal line with numbers from 0 to 10, with 0 representing no pain, and 10 representing the worst pain imaginable. The higher the score, the greater the pain.
2.1. Statistical analysis
NRS-11 and MOPDS scores were recorded. Descriptive statistics were reported in mean, median, and range. Wilcoxon's rank-sum test and linear regression were used to measure association between emergency type with pain intensity. Linear regression was used to determine the association between levels of pain intensity and disability score. The level of statistical significance was set at P < 0.05. All analyses were performed using STATA Version 16.0 (StataCorp, College Station, TX) statistical software package.
3. Results
A total of 259 responses to the electronic survey were received. Of those, 150 patients were undergoing orthodontic treatment at KAUFD and agreed to participate, comprising 57.9% of total respondents. The remaining 109 respondents did not agree to participate or were not currently undergoing any orthodontic treatment.
Characteristics of the study population are presented in Table 1 . The mean age of the study sample was 20 years, and 57.33% of the respondents were female. Adolescents comprised most respondents, 54.7%, compared with adults, 45.3%, and approximately 35% were enrolled in secondary school. A total of 130 individuals had fixed orthodontic appliance (86.67%) followed by removable appliance (6%), retainers (6%), and aligners (1.33%). Approximately 64% of patients had not seen an orthodontist for more than 2 months, and almost 59% of them reported having current orthodontic problem.
Table 1.
Characteristics of the study population
| Variables | Male, n (%) | Female, n (%) | Total |
|---|---|---|---|
| Age, y | |||
| 8–12 | 3 (33.33) | 6 (66.67) | 9 |
| 13–18 | 31 (42.47) | 42 (57.53) | 73 |
| >18 | 30 (44.12) | 38 (55.53) | 68 |
| Gender | 64 (42.67) | 86 (57.33) | 150 |
| Education | |||
| Elementary | 6 (46.15) | 7 (53.85) | 13 |
| Intermediate | 15 (46.88) | 17 (53.13) | 32 |
| Secondary | 19 (35.85) | 34 (64.15) | 53 |
| Graduate | 23 (46.94) | 26 (53.06) | 49 |
| Postgraduate | 1 (33.33) | 2 (66.67) | 3 |
| Type of orthodontic appliance | |||
| Fixed | 56 (43.08) | 74 (56.92) | 130 |
| Removable | 5 (55.56) | 4 (44.44) | 9 |
| Aligner | 1 (50) | 1 (50) | 2 |
| Retainer | 2 (22.22) | 7 (77.78) | 9 |
| Last orthodontic visit, d | |||
| ≤30 | 0 | 2 (100) | 2 |
| 31–60 | 23 (44.23) | 29 (55.77) | 52 |
| 61–90 | 25 (49.02) | 26 (50.98) | 51 |
| >90 | 16 (35.56) | 29 (64.44) | 45 |
| Current orthodontic problem | |||
| Yes | 41 (46.59) | 47 (53.41) | 88 |
| No | 23 (37.10) | 39 (62.90) | 62 |
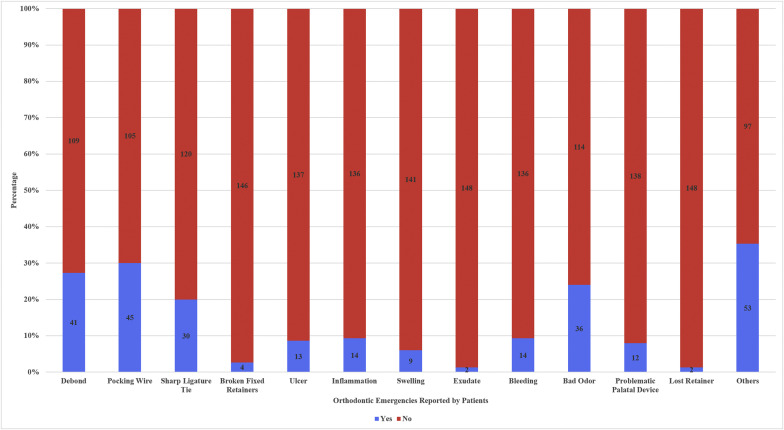
Figure 1 presents the most common emergencies reported by respondents. The most common orthodontic emergency was poking wire, which was reported by 30% of the respondents. This was followed by debonded bracket (27.3%), bad odor (24.0%), and sharp ligature tie (20.0%), respectively. Inflammation and bleeding were reported by 9.3%, ulcer was reported by 8.7%, and problematic palatal device by 8% of respondents. Nine respondents reported swelling, and 2 respondents reported exudate and lost retainers. Four of the 150 respondents reported broken fixed retainers. Other reported complications included loose elastomeric chain, loose molar bands, pain related to molar bands, teeth are moving in a wrong direction, spaces between teeth, ran out of elastics, cheek biting, and remaining sutures related to impacted canine exposure.
Fig. 1.
Orthodontic emergencies as reported by patients.
Based on the type of orthodontic appliance used, the main emergencies reported with aligners were inflammation and swelling, whereas ulcer, bad odor, problematic palatal device, and lost retainer were reported by patients undergoing retention. Ulcer, inflammation, bleeding, bad odor, and problematic palatal device were reported with removable appliances, whereas the remaining emergencies were reported with fixed appliances, as displayed in Figure 1.
No significant difference was found in intensity of pain between male and female patients, and among different age groups. Patients who reported poking wires had significantly higher pain scores compared with those who did not (P < 0.001). Similar findings were observed in pain scores between those who reported sharp ligature tie, ulcer, and problematic palatal device than those who did not (Table 2 ). Confounding factors in these correlations were studied using linear regression models. After adjustment of confounders, poking wire, sharp ligature tie, and problematic palatal device were found to be significant predictors of pain intensity. On the other hand, the presence of ulcer was not found to be a significant predictor for pain intensity.
Table 2.
Association between pain/disability and reported emergency
| Emergency | NRS-11 |
|
|---|---|---|
| Median | P value | |
| Debonded bracket | ||
| Yes | 4 | 0.094 |
| No | 2 | |
| Poking wire | ||
| Yes | 4 | 0.001c |
| No | 2 | |
| Sharp ligature tie | ||
| Yes | 4 | 0.005b |
| No | 2 | |
| Broken fixed retainer | ||
| Yes | 4 | 0.633 |
| No | 3 | |
| Ulcer | ||
| Yes | 5 | 0.013a |
| No | 3 | |
| Inflammation | ||
| Yes | 3 | 0.368 |
| No | 3 | |
| Swelling | ||
| Yes | 1 | 0.077 |
| No | 3 | |
| Exudate | ||
| Yes | 1 | 0.356 |
| No | 3 | |
| Bleeding | ||
| Yes | 3 | 0.694 |
| No | 3 | |
| Bad odor | ||
| Yes | 3 | 0.241 |
| No | 2 | |
| Problematic palatal device | ||
| Yes | 5 | 0.008b |
| No | 2.5 | |
| Lost retainer | ||
| Yes | 1.5 | 0.517 |
| No | 3 | |
NRS, Numerical Rating Scale.
Wilcoxon rank-sum test.
P < 0.05.
P < 0.01.
P < 0.001.
From the study sample, 21.3% reported pain for more than 24 hours in their face, jaws, or mouth. Of those, 53% were male patients with mean age of 22 years (range: 13–45). From all 150 respondents, approximately 9.3% reported seeking professional consultations for their pain. The median reported pain intensity of the whole group on the NRS-11 was 3 (range: 0–9).
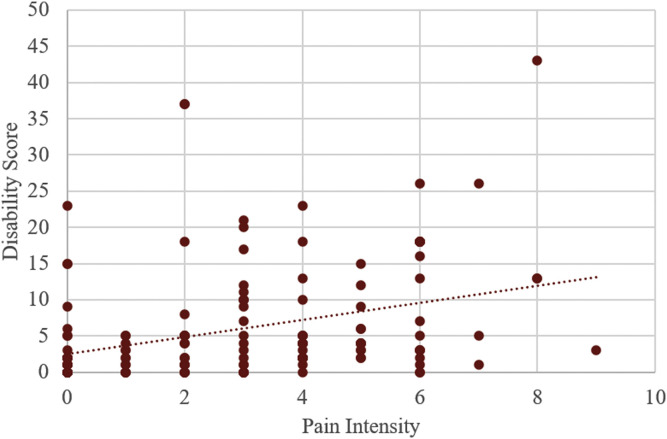
Table 3 presents respondents’ reported disability on each MOPDS item. The greatest reported physical disabilities were “I cannot eat hard foods” (51.3%), “I take longer to finish my meals” (46%), and “I no longer enjoy my food” (36.7%). The highest reported psychosocial disabilities were “I find it difficult to talk for long periods of time” (30.7%) followed by “I am irritable, angry, and easily frustrated” (26.7%). The median disability score was 3 (range: 0–43). Linear regression model revealed a significant association between intensity of pain and disability score (P < 0.01) (Fig. 2 ). With each unit increase in pain intensity, the disability score increased by 1.18 (95% confidence interval 0.67–1.69).
Table 3.
Number of respondents reporting disability on each item of the Manchester Orofacial Pain Disability Scale
| Disability | Because of pain in my face, jaws, or mouth | None of the time, n (%) | On some days, n (%) | On most/everyday(s), n (%) |
|---|---|---|---|---|
| Physical | I cannot open my mouth as wide as I could | 123 (82) | 24 (16) | 3 (2) |
| I cannot touch my face | 141 (94) | 9 (6) | 0 | |
| I cannot eat hard foods like apples or toast | 73 (48.7) | 50 (33.3) | 27 (18) | |
| I take longer to finish my meals | 81 (54) | 53 (35.3) | 16 (10.7) | |
| I no longer enjoy my food | 95 (63.3) | 47 (31.3) | 8 (5.4) | |
| I find it sore to kiss | 132 (88) | 12 (8) | 6 (4) | |
| I find it difficult to smile or laugh | 109 (72.7) | 29 (19.3) | 12 (8) | |
| Psychosocial | I have difficulty falling asleep | 125 (83.3) | 24 (16) | 1 (0.7) |
| I wake up at night in pain | 134 (89.3) | 16 (10.7) | 0 | |
| I cannot find a comfortable position in which to sleep | 123 (82) | 26 (17.3) | 1 (0.7) | |
| People find me difficult to live with | 135 (90) | 12 (8) | 3 (2) | |
| I have had to take time off work | 138 (92) | 10 (6.7) | 2 (1.3) | |
| I have lost earnings | 139 (92.7) | 7 (4.7) | 4 (2.6) | |
| I have found it difficult to concentrate | 127 (84.7) | 16 (10.7) | 7 (4.6) | |
| I have problems performing normal household tasks | 133 (88.7) | 13 (8.7) | 4 (2.6) | |
| I would rather be by myself | 124 (82.7) | 18 (12) | 8 (5.3) | |
| I find it difficult to talk for long periods of time | 104 (69.3) | 38 (25.3) | 8 (5.4) | |
| I have canceled social activities and holidays | 134 (89.3) | 13 (8.7) | 3 (2) | |
| I am unable to eat out in restaurants | 137 (91.3) | 10 (6.7) | 3 (2) | |
| I feel weary/tired | 123 (82) | 24 (16) | 3 (2) | |
| I am irritable, angry, and easily frustrated | 110 (73.3) | 35 (23.3) | 5 (3.4) | |
| I cannot stop crying | 135 (90) | 14 (9.3) | 1 (0.7) | |
| I am worried that I may have a serious illness | 141 (94) | 6 (4) | 3 (2) | |
| I feel embarrassed and self-conscious | 116 (77.3) | 26 (17.3) | 8 (5.4) | |
| I feel depressed | 124 (82.7) | 20 (13.3) | 6 (4) | |
| I feel I no longer take any pleasure in life | 126 (84) | 18 (12) | 6 (4) |
Fig. 2.
Association between pain intensity and disability score.
4. Discussion
Implications of the coronavirus pandemic (COVID-19) had extended beyond affecting only infected individuals to reach everyone globally, causing a huge disruption on peoples' lives. The risk management plans and containment measures enforced by several countries to halt the spread of COVID-19 had affected individuals' daily activities and their access to routine care. Orthodontics was not an exception, where national dental clinic closure and restricting clinical visits to emergency treatment only had affected patients undergoing active treatment in these clinics. In many cases, the sudden clinical closure did not provide an opportunity for orthodontists to stabilize their cases and communicate well with their patients and prepare them for an extended period of no treatment. This could negatively influence patients' experience and treatment outcome [23]. More importantly, the definition of what would be considered a true emergency in orthodontics is not clear. They are usually adverse events related to the orthodontic appliance that requires an unscheduled appointment to relieve patients' discomfort and maintain continuity of care. The types and severity of adverse events that are considered emergencies could be different from patients' perspectives than orthodontists. In this research, we provided a list of the most common adverse events related to orthodontics that could necessitate an unscheduled appointment or result in patients’ discomfort [19].
Most patients included in this study had not been seen by their treating orthodontist for more than 2 months. During this prolonged period, patients could experience discomfort due to a problem arising from the orthodontic appliance requiring an emergency appointment or at least a consultation and reassurance. Furthermore, patients could lose motivation and trust, and stop wearing their elastics or appliances that are critical and time sensitive [17]. They could experience anxiety, fear, and abandonment, which could exacerbate their discomfort [24,25]. For this, assuring patients using virtual assistance through teleorthodontics and maintaining appropriate communication channels is advised [17].
Most respondents in the current study were female patients; however, there was no difference in the median pain intensity experienced by male compared with female patients, which is in line with the findings of Zheng et al. [26]. This might indicate that female patients could have a higher tendency to seek treatment when experiencing pain. In addition, the most common reported orthodontic emergency was poking wire (30%) followed by debonded bracket (27.3%), and ulcer (8.7%), which contradicts the findings of Dyke and Sandler [27] who reported most unscheduled orthodontic appointments to be resulting from detached bracket (28.2%) followed by an extended arch wire 8.2%. Moreover, Popat et al. [28] reported debonded bracket (37%) to be the most common orthodontic emergency followed by protruding wire 25%, whereas ulcer was 4%. In their study, Popat et al. [28] distributed electronic surveys to general dental practitioners to assess the number of orthodontic emergencies they encounter and were confident to treat. In the current study, we measured the outcomes reported from the patients themselves. Also, patients in the study by Popat et al. [28] would usually present to general dentists for an emergency treatment appointment that could occur between their regular orthodontic visits. Whereas in this study, patients had not been seen for an extended period of time, which could explain the difference in the findings favoring a higher percentage of adverse events, including poking wires, which was found to be significantly associated with pain. Popat et al. [28] reported that emergency treatment was significantly associated with pain, which goes along with our findings that poking wire, sharp ligature tie, and problematic palatal device were significant pain predictors. Although ulcer in the current study was found to be significantly associated with pain initially, further analysis using the regression model revealed that this was influenced by the confounding effect of other predictors. This could be explained by the low incidence of ulcer (13 only) among the study sample, which could dilute the effect of the variable, given that true emergencies in orthodontics are not very common.
In this study, we used MOPDS, which is an orofacial pain–specific disability measure. Previous studies reported significant association between orofacial pain symptoms and psychological distress [29]. Wan et al. [30] reported strong association between severity of pain and disability score using MOPDS, which is in line with the findings of the current study. Although median pain intensity and disability score were not significantly high, future implications of such delay in receiving care in addition to other physical and mental effects of the COVID-19 pandemic are still questions to be answered.
In general, any delay in orthodontic treatment would result in the emergencies reported in this study. However, the current study highlighted the association between these emergencies and pain and disability experienced by patients especially in the event of a pandemic, which were not very high as normally reported by the patients. This should help decision makers evaluate risks versus benefits when it comes to resumption of clinical operation in case of a future disease outbreak.
Limitations of the study were the sample size and convenience sampling method that was used on patients from one city, which could affect the generalizability of the findings. Furthermore, the validated scales measured outcomes experienced by the patients within the past month, which rely on patients’ recall memories that could influence their answers. Last, findings present the situation within 3 months of no treatment during this unprecedented situation of pandemic lockdown, yet it might be different in other situations or if the patients were not seen by their orthodontist for a longer duration than what was addressed here. Given these limitations, to our knowledge, this is the first study to report orthodontic emergency, pain, and disability experienced by patients during clinical lockdown in time of the COVID-19 pandemic. Findings of this study could enhance further studies in this area.
5. Conclusion
In summary, delay in receiving orthodontic care could give rise to orthodontic emergencies experienced by patients, yet pain and disability resulting from these events are minimal. Poking wires, sharp ligature ties, and problematic palatal device were the significant predictors of pain. The higher the intensity of pain, the more disability was noted. Finally, the decision to resume clinical service should be evaluated considering risks and benefits during an infectious outbreak. Further research to complement or contradict these study findings is required.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interest: Authors have completed and submitted the ICMJE Form for Disclosure of potential conflicts of interest. None disclosed.
Provenance and peer review: Not commissioned, Externally peer reviewed.
References
- 1.World Health Organization Coronavirus disease 2019 (COVID-19): situation report-11. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4 Available at:
- 2.World Health Organization Coronavirus disease 2019 (COVID-19): situation report-51. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10 Available at:
- 3.World Health Organization Coronavirus disease 2019 (COVID-19): situation report-178. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200716-covid-19-sitrep-178.pdf?sfvrsn=28ee165b_2 Available at:
- 4.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:1–6. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hassan S., Sheikh F.N., Jamal S., Ezeh J.K., Akhtar A. Coronavirus (COVID-19): a review of clinical features, diagnosis, and treatment. Cureus. 2020;12:e7355. doi: 10.7759/cureus.7355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rothe C., Schunk M., Sothmann P. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu X., Zhang L., Du H. SARS-CoV-2 infection in children. N Engl J Med. 2020;382:1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guan W-j, Ni Z-y, Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Eng J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turkistani K.A. Precautions and recommendations for orthodontic settings during the COVID-19 outbreak: A review. Am J Orthod Dentofacial Orthop. 2020;158:175–181. doi: 10.1016/j.ajodo.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Doremalen N., Bushmaker T., Morris D.H. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meng L., Hua F., Bian Z. Coronavirus Disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Micik R.E., Miller R.L., Mazzarella M.A., Ryge G. Studies on dental aerobiology. I. Bacterial aerosols generated during dental procedures. J Dent Res. 1969;48:49–56. doi: 10.1177/00220345690480012401. [DOI] [PubMed] [Google Scholar]
- 13.Ge Z-y, Yang L-m, Xia J-j, Fu X-h, Zhang Y-z. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J Zhejiang Univ Sci B. 2020;21:361–368. doi: 10.1631/jzus.B2010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koh D. COVID-19 lockdowns throughout the world. Occup Med. 2020;70:322. [Google Scholar]
- 15.Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27 doi: 10.1093/jtm/taaa020. taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guo H., Zhou Y., Liu X., Tan J. The impact of the COVID-19 epidemic on the utilization of emergency dental services [published online ahead of print March 16, 2020] J Dent Sci. 2020 doi: 10.1016/j.jds.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caprioglio A., Pizzetti G.B., Zecca P.A., Fastuca R., Maino G., Nanda R. Springer; Berlin/Heidelberg, Germany: 2020. Management of orthodontic emergencies during 2019-NCOV. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dowsing P., Murray A., Sandler J. Emergencies in orthodontics part 1: management of general orthodontic problems as well as common problems with fixed appliances. Dent Update. 2015;42:131–140. doi: 10.12968/denu.2015.42.2.131. [DOI] [PubMed] [Google Scholar]
- 19.Sodipo I., Birdsall J. Orthodontic first aid for general dental practitioners. Dent Update. 2016;43:461–471. doi: 10.12968/denu.2016.43.5.461. [DOI] [PubMed] [Google Scholar]
- 20.Aggarwal V.R., Lunt M., Zakrzewska J.M., Macfarlane G.J., Macfarlane T.V. Development and validation of the Manchester orofacial pain disability scale. Community Dent Oral Epidemiol. 2005;33:141–149. doi: 10.1111/j.1600-0528.2004.00193.x. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization . 2013. Process of translation and adaptation of Instruments.https://www.who.int/substance_abuse/research_tools/translation/en/ Available at: [Google Scholar]
- 22.Hawker G.A., Mian S., Kendzerska T., French M. Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP) Arthritis Care Res. 2011;63:S240–S252. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 23.Lahti S., Tuutti H., Hausen H., Kääriäinen R. Comparison of ideal and actual behavior of patients and dentists during dental treatment. Community Dent Oral Epidemiol. 1995;23:374–378. doi: 10.1111/j.1600-0528.1995.tb00266.x. [DOI] [PubMed] [Google Scholar]
- 24.Firestone A.R., Scheurer P.A., Bürgin W.B. Patients' anticipation of pain and pain-related side effects, and their perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1999;21:387–396. doi: 10.1093/ejo/21.4.387. [DOI] [PubMed] [Google Scholar]
- 25.Vassend O. Anxiety, pain and discomfort associated with dental treatment. Behav Res Ther. 1993;31:659–666. doi: 10.1016/0005-7967(93)90119-f. [DOI] [PubMed] [Google Scholar]
- 26.Zheng B., Ren M., Lin F., Yao L. Prediction of pain in orthodontic patients based on preoperative pain assessment. Patient Prefer Adherence. 2016;10:251. doi: 10.2147/PPA.S101391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dyke A., Sandler J. Audit of unscheduled orthodontic appointments at Chesterfield Royal Hospital. Br Orthod Soc Clin Effect Bull. 2015;35:8–10. [Google Scholar]
- 28.Popat H., Thomas K., Farnell D.J. Management of orthodontic emergencies in primary care—self-reported confidence of general dental practitioners. Braz Dent J. 2016;221:21–24. doi: 10.1038/sj.bdj.2016.495. [DOI] [PubMed] [Google Scholar]
- 29.Grönblad M., Järvinen E., Hurri H., Hupli M., Karaharju E.O. Relationship of the Pain Disability Index (PDI) and the Oswestry Disability Questionnaire (ODQ) with three dynamic physical tests in a group of patients with chronic low-back and leg pain. Clin J Pain. 1994;10:197–203. doi: 10.1097/00002508-199409000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Wan K., McMillan A., Wong M. Orofacial pain symptoms and associated disability and psychosocial impact in community-dwelling and institutionalized elderly in Hong Kong. Community Dent Health. 2012;29:110–116. [PubMed] [Google Scholar]