Abstract
Multiple organ failure in COVID-19 patients is a serious problem which can result in a fatal outcome. Damage to organs and tissues, including general lung dysfunction, develops as a consequence of ischemia, which, in turn, is caused by thrombosis in small blood vessels and hypoxia, leading to oxidative stress and inflammation. Currently, research is underway to screen existing drugs for antioxidant, antiplatelet and anti-inflammatory properties. Having studied the available publications concerning the mechanisms of damage to tissues and organs of patients with COVID-19, as well as the available treatment strategies, we propose to investigate salicyl-carnosine as a potential drug for treating COVID-19 patients. In a recent study, we described the drug’s synthesis procedure, and showed that salicyl-carnosine possesses antioxidant, anti-inflammatory, and antiplatelet effects. Therefore, it can simultaneously act on the three pathogenetic factors involved in tissue and organ damage in COVID-19. Thus, we propose to consider salicyl-carnosine as a potential drug for the treatment of patients with severe cases of COVID-19 infection.
Keywords: COVID-19, Salicyl-carnosine, Inflammation, Oxidative stress, Thrombosis, Aspirin
1. Introduction
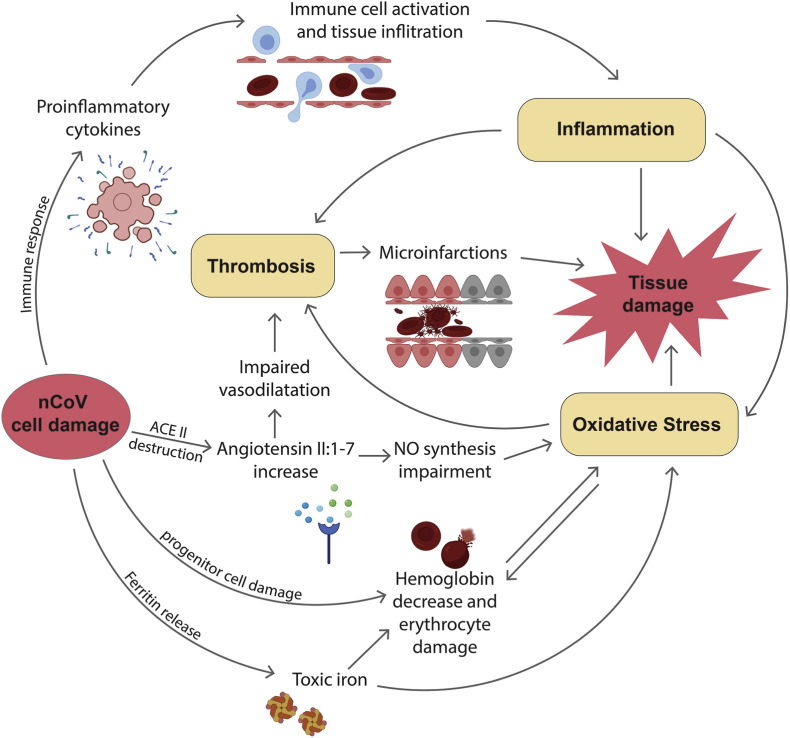
Recent studies show that mortality from COVID-19 is associated with multiple organ failure, especially pulmonary and cardiovascular dysfunction (Zaim et al., 2020). Tissue damage is associated with the development of strong systemic inflammation (Zaim et al., 2020), accompanied by oxidative stress (Delgado-Roche and Mesta, 2020). A key role in lung tissue damage is played by microinfarcts caused by small vessel thrombosis. At the present moment, our understanding of the mechanisms underlying tissue damage observed over the course of a COVID-19 infection is largely incomplete. However, a number of facts have already been established that indicate the involvement of oxidative stress, inflammation, and dysregulated platelet aggregation (Leisman et al., 2020). These three factors are closely interconnected - heightened immune response can cause infiltration of immune cells into small vessels, which leads to endothelium activation and thrombosis (Leisman et al., 2020). At the same time, the secreted proinflammatory cytokines cause oxidative stress (Yang et al., 2007) (Fig. 1 ).
Fig. 1.
An overview of the processes discussed in this review, the sum of which leads to secondary tissue damage during a COVID-19 infection.
In previous publications, a variety of drugs targeting different aspects of the COVID-19 infection have been proposed. Many authors suggest using anti-inflammatory drugs, such as blockers of the different proinflammatory cytokines, including IL-1, IL-6, and TNF (Moore and June 2020; Ye et al., 2020). Other authors suggest the use of anti-aggregation therapy to combat thrombosis in COVID-19 treatment (Cattaneo et al., 2020). A number of antioxidants were suggested to ameliorate oxidative stress (Carr, 2020; Wang et al., 2020). Thus, most of the drugs currently suggested for the treatment of COVID-19 act upon only one of the three listed factors.
Low oxygen levels in the blood can also lead to multiple organ failure. Hemoglobin levels in patients with severe COVID-19 cases are significantly lower than in patients with mild symptoms (Lippi and Mattiuzzi, 2020). Researchers suggest that non-structural coronavirus proteins penetrate red blood cells and displace iron ions from hemoglobin, which leads to both the loss of hemoglobin function and the release of toxic iron, the presence of which in the blood leads to an increase in oxidative stress levels (Liu and Li, 2020). Currently, erythropoiesis inducers are being studied as potential drugs for treating COVID-19 (Geier and Geier, 2020). At the same time, the search for drugs which can stabilize red blood cells remains relevant (Fig. 1).
A promising drug in this case is aspirin, as it possesses both anti-inflammatory and anti-aggregation effects, and suppresses the development of oxidative stress (van Gijn et al., 1993). However, aspirin has a number of side effects which makes it potentially dangerous to use for treatment of COVID-19 patients (Adam et al., 2016).
We propose to investigate salicyl-carnosine as a potential drug for treating COVID-19, due to its anti-oxidative, anti-aggregational, and anti-inflammatory actions, as well as its ability to inhibit erythrocyte hemolysis and lack of detrimental side effects (Kulikova et al., 2020).
2. Inflammation
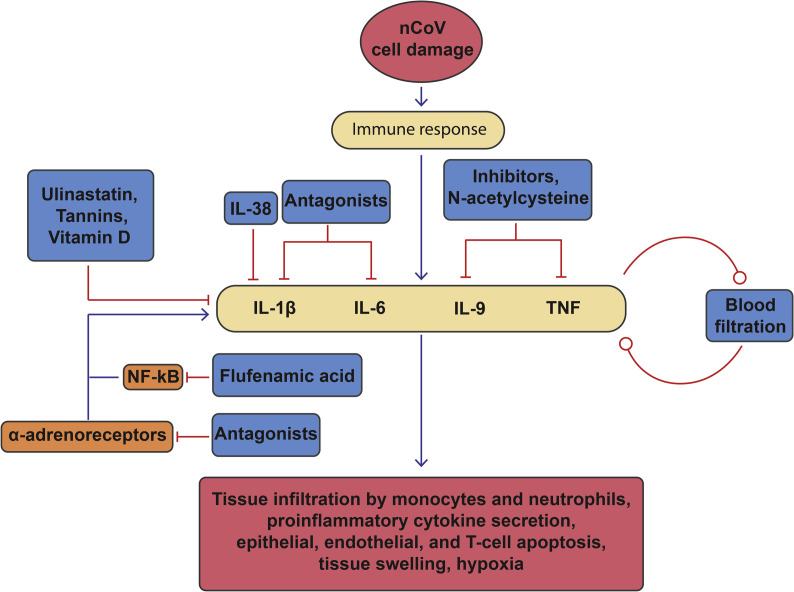
It was shown that the interleukin-mediated inflammatory response observed in patients with COVID-19 is significantly less pronounced than in those with acute respiratory syndrome (ARDS) or the so-called “cytokine release syndrome” (CRS). During hyperinflammatory ARDS, interleukin-6 (IL-6) plasma levels can reach 517–3205 pg/ml (at a rate of <5.9 pg/ml.) (Sinha et al., 2020), and in patients with CRS, IL-6 plasma levels increase to 10,000 pg/ml (Maude et al., 2014). Meanwhile, in COVID-19, reported IL-6 levels reach only 125 pg/ml, with the mean bening 25 (SD: 10–55) pg/ml. Other proinflammatory interleukins exhibit similar dynamics. The use of IL-6 inhibitors (Moore and June 2020) or monoclonal antibodies against the IL-6 receptor (tocilizumab) (Xu et al., 2020) has previously been proposed; however, the inflammatory response observed in COVID-19 is weaker than in typical ARDS or CRS, and as such the use of IL-6 inhibitors to relieve the inflammation in COVID-19 patients does not seem entirely justified (Leisman et al., 2020) (Fig. 2 ).
Fig. 2.
A diagram of inflammation development during the course of a COVID-19 infection. Blue arrows represent positive regulation between the interacting elements, red arrows ending in a dash represent negative regulation, or drug action.
Viral invasion can lead to an overly expressed immune reaction, which, in turn, can worsen the patient’s condition. Proinflammatory cytokines IL-1β, IL-6, TNF and chemokines C–C motif chemokine ligand (CCL)-2, CCL-3, and CCL-5 cause the infiltration of tissues (for example, lung tissues) by neutrophils and monocytes, leading to tissue damage. In response to the activation of interferon receptors, neutrophils and monocytes produce additional pro-inflammatory cytokines, which facilitates the apoptosis of T-cells, as well as epithelial and endothelial lung cells, leading to lung tissue swelling and hypoxia (Ye et al., 2020). Ye and co-authors suggest using inhibitors of interferons, TNF inhibitors, IL-1 and IL-6 antagonists, ulinastatin, which normalises the pro- and anti-inflammatory cytokine levels, as well as a number of other drugs used to suppress CRS during other viral infections (Fig. 2).
Most of the proposed drugs possess anti-inflammatory effects. For example, it has been proposed to use IL-38 in treating COVID-19 patients, as it suppresses IL-1β and other proinflammatory members of the IL family (Conti et al., 2020). Another suggested anti-inflammatory drug is hydroxychloroquine, which is often used to treat and prevent malaria. Clinical trials have already been conducted with this drug, resulting in significantly reduced viral load in patients with COVID-19 (Sinha and Balayla, 2020). However, its emergency use authorization was revoked by FDA (Food & Drug Administration; https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-revokes-emergency-use-authorization-chloroquine-and) because its potential side effects (for example, cardiac adverse) do not overweight its potential benefits. N-acetylcysteine in doses of ≥1200 mg reduces the formation of pro-inflammatory cytokines such as IL-9 and TNF-α, possesses a vasodilatory effect as consequence of increased cGMP levels, and promotes regeneration of the endothelial relaxation factor (van Hecke and Lee, 2020).
Vitamin D has been suggested for COVID-19 treatment as an immunomodulatory drug due to its ability to suppress pro-inflammatory cytokines. It can also bind to the ACE II receptor, preventing the virus from entering the cell. However, vitamin D increases the level of extracellular calcium, which can activate TRPM2, which can lead to an increase in intracellular calcium, and as a result, apoptosis or necrosis (Kouhpayeh et al., 2020). These authors also suggest using substances with anti-inflammatory properties, such as tannins (which can inhibit cytokine expression) and flufenamic acid (activates AMPKα-P and inhibits NFkB expression).
A more complex proposed treatment consists of filtering pro-inflammatory cytokines from the blood, utilizing antibodies in a special column, after which the purified blood is returned to the patient's body (Tay et al., 2020).
Another approach to anti-inflammatory therapy is the use of α1 adrenoceptor antagonists, which are thought to prevent the “cytokine storm”. Catecholamines lead to stronger inflammation by increasing the production of IL-6 and other cytokines through a positive feedback loop in immune cells, that requires signaling from α1 adrenoceptor (Konig et al., 2020). Thus, blocking the receptor in question would lead to a decrease in inflammation.
3. Oxidative stress
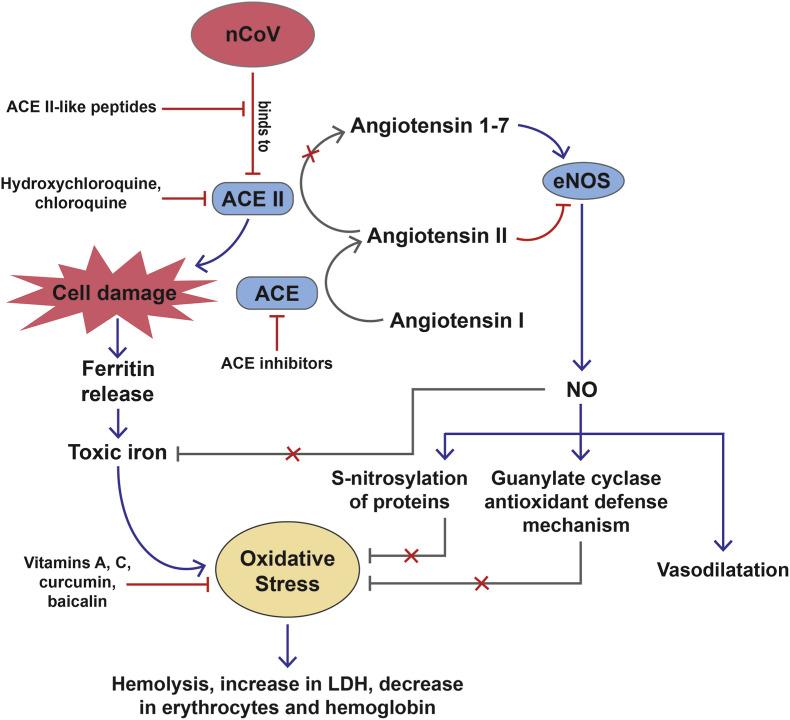
It was shown that the development of inflammation, accompanied by oxidative stress, is augmented by the ability of the virus to block the organism’s antioxidant defense mechanism (Delgado-Roche and Mesta, 2020) (Fig. 1). A unique feature of COVID-19 is that the virus binds to the angiotensin-converting protein-2 (ACE2), and the ACE2-virus complex enters the epithelial cells of the pulmonary alveoli, where ACE2 is destroyed (Buinitskaya et al., 2020). The virus can also bind to vascular endothelial ACE2. ACE2 converts Angiotensin (Ang) II to Angiotensin 1-7. Ang II decreases the amount of active forms of endothelial nitric oxide synthase (eNOS), while Ang 1–7 has the opposite effect (Xiao et al., 2015). Therefore, ACE2 inactivation leads to impaired NO synthesis due to the dysfunction of the ACE2/eNOS/NO cascade (Xiao et al., 2015) and impaired vascular dilatation (Buinitskaya et al., 2020) (Fig. 3 ). Although large amounts of NO lead to the formation of toxic peroxynitrite (Forstermann, 2010), a decrease in the amount of cellular NO leads to the development of oxidative damage. It is also known that during a COVID-19 infection, ferritin, along with free iron radicals, is released from ruptured cells. As a consequence, concentrations of the respective substances are increased in the blood of patients (Colafrancesco et al., 2020). NO, binding to Fe2+, prevents the formation of OH radicals (Sahni et al., 2018), and triggers the guanylate cyclase antioxidant defense mechanism and S-nitrosylation of proteins, which protects them from oxidative damage (Otani, 2009). The decrease in NO levels which occurs during a COVID-19 infection leads to impaired vasodilation, which the body is forced to compensate via an increase in heart rate and respiratory rate (Buinitskaya et al., 2020). To prevent the virus from entering cells, the use of ACE2 blockers, such as hydroxychloroquine and chloroquine phosphate, has previously been proposed (McKee et al., 2020). However, the suggestion was later withdrawn. At the same time, other researchers propose to inhibit ACE rather than ACE2 (South et al., 2020), which, in the context of data regarding the role of ACE2, is a convincing approach. The use of short peptides the structure of which mimics ACE2 and blocks the viral S protein that binds to ACE2 has also been proposed (Li et al., 2020). Clinical data has shown an increase in LDH concentration and decrease in erythrocytes and hemoglobin in the blood of COVID-19 patients, which indicates the presence of hemolysis (Cavezzi et al., 2020). Damage and break-down of erythrocytes may be linked to the above mentioned mechanisms of oxidative stress development (Fig. 3). Erythropoietin has been suggested for restoring erythrocyte level in the blood (Soliz et al., 2020). The most often suggested antioxidant treatment for COVID-19 is intravenous administration of vitamin C. Clinical trials of its effectiveness are already underway, with an approximate end date in September 2020 (Carr, 2020). During a viral infection, the blood level of vitamin C can drop significantly, to counteract which in the abovementioned study, large doses of vitamin C are administered to patients intravenously: 24 g/day for 7 days (Carr, 2020). Wang et al. suggest using vitamins C and E as antioxidant therapy for patients with COVID-19, and imply that molecules such as Curcumin and Baicalin may also be effective (Wang et al., 2020) (Fig. 3).
Fig. 3.
A diagram of processes leading to oxidative stress and tissue damage during a COVID-19 infection. Blue arrows represent positive regulation between the interacting elements, red arrows ending in a dash represent negative regulation, or drug action.
4. Thrombosis
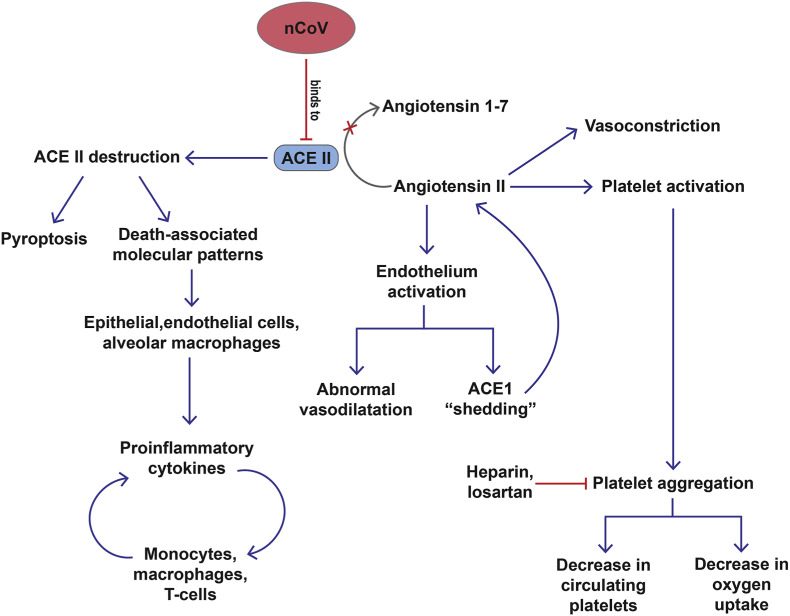
Multiple pulmonary thrombosis, accompanied by damage to blood vessel walls, leads to a severe course of the infection, and is in most cases lethal. To understand the development of thrombosis, it is necessary to turn to the mechanism of action of the SARS-CoV-2 in the early stages of infection. As mentioned above, the virus binds to ACE2 on the cell surface, which leads to pyroptosis and the chaotic release of death-associated molecular patterns (Fehr and Perlman, 2015), which are recognized by neighboring epithelial cells, endothelial cells and alveolar macrophages, which respond with the generation of pro-inflammatory cytokines that attract monocytes, macrophages and T-cells, which, in turn, contributes to further inflammation (Vénéreau et al., 2015). This can lead to the accumulation of immune cells and the overproduction of proinflammatory cytokines that circulate in the bloodstream and enter other organs, leading to their damage. Viral invasion of endothelial cells leads to localized foci of inflammation in small vessels, which, in turn, causes the activation of the endothelium, leading to abnormal vasodilation and the formation of blood clots (Leisman et al., 2020) (Fig. 4 ). The binding of the viral S protein to ACE2 causes Angiotensin II, which possesses a vasoconstrictor effect, to no longer be metabolized. Normally, it is metabolized by endothelial ACE2 to produce angiotensin, which has vasodilatory and anti-inflammatory effects. The localized increase in angiotensin II concentration (in patients with COVID-19, the level of angiotensin II is two times higher than in healthy individuals (Liu et al., 2020) also contributes to the activation of the endothelium and the release of pro-inflammatory cytokines. Angiotensin II can also activate platelets, contributing to their aggregation in the area of inflammation (Duprez, 2004). At the same time, activation of the endothelium leads to the so-called “shedding” of ACE1 and a subsequent temporary sharp increase in concentration of angiotensin II, thus forming a positive feedback loop which further promotes local inflammation and coagulation (Verdecchia et al., 2020). The specific mechanism of the occurrence of coagulation and spontaneous sedimentation of cells, as well as the occurrence of platelet aggregates in the blood of patients observed in severe infections, is not fully understood. Nevertheless, there is reason to believe that coagulation activation and inhibition of anticoagulant factors are observed in patients with COVID-19, as evidenced by the increased D-dimer content in the blood of severe case patients (Violi et al., 2020). Interestingly, in severe COVID-19 cases, thrombocytopenia is also observed. One of the proposed mechanisms of its occurrence is based on the aggregation of platelets in the lungs, which leads to a decrease in oxygen uptake and circulating platelets (Xu et al., 2020). Antiplatelet drugs, such as heparin (Cattaneo et al., 2020), and losartan, which reduces platelet aggregation and has an antihypertensive effect, have been proposed as potential treatment strategies for COVID-19 (Kouhpayeh et al., 2020) (Fig. 4).
Fig. 4.
A diagram of processes leading to thrombosis and thrombocytopenia during a COVID-19 infection. Blue arrows represent positive regulation between the interacting elements, red arrows ending in a dash represent negative regulation, or drug action. Greyed out arrows represent processes which are inhibited by COVID-19.
5. Aspirin
Aspirin (acetylsalicylic acid) is the most widely used antiplatelet agent in clinical practice (Fiolaki et al., 2017). It can inhibit the pro-inflammatory cascade and the development of oxidative stress (van Gijn et al., 1993). These effects are due to the antioxidant properties of salicylates, which include the neutralization of OH radicals, chelation of transition metals, activation of nitric oxide, and inhibition of the “oxidative explosion” of neutrophils (Dinis-Oliveira et al., 2007). Aspirin is rapidly absorbed from the human gastrointestinal tract, and within 20 min is deacetylated by esterases to form salicylic acid. Its half-life in plasma depends on the dose, ranging from 2 to 30 h (Needs and Brooks, 1985). Thus, most of the biological activity of aspirin can be attributed to its primary metabolite, salicylic acid.
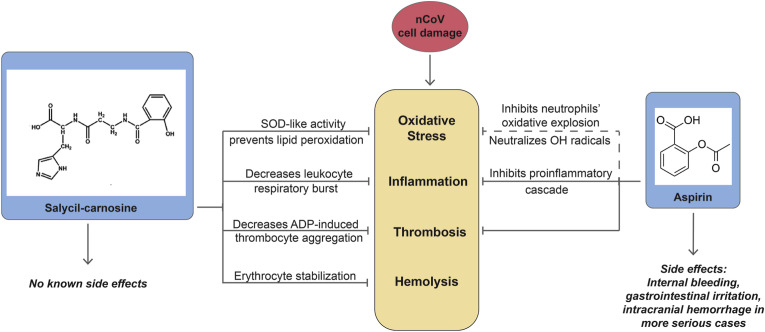
Currently, aspirin is proposed for use as an antithrombotic drug for the treatment of COVID-19, but only if the patient has confirmed hypercoagulation, with markers such as soluble P-selectin or Iib/IIIa used to evaluate it (Violi et al., 2020). Data on the use of low doses of aspirin for the prevention of preeclampsia in pregnant women with COVID-19 is contradictory: one group (Mathilde et al., 2020) suggests canceling the treatment if a coronavirus infection is detected due to the risk of bleeding during cesarean section, the other group (Kwiatkowski et al., 2020) suggests continuing administration of low doses of aspirin due to insufficient data to draw conclusions. However, antiplatelet drugs, including aspirin, have a number of side effects, including internal and prolonged bleeding, gastrointestinal irritation, and intracranial hemorrhage in more serious cases (Adam et al., 2016) (Fig. 5 ).
Fig. 5.
A comparison of the actions of salicyl-carnosine and aspirin on factors of tissue damage during a COVID-19 infection, as well as a comparison of the presence or lack of negative side effects. Data acquired and published by our laboratory is represented with solid arrows, data found in literature - by dashed arrows.
6. Salicyl-carnosine
Currently, the efforts of biomedical researchers are aimed both at the development of new drugs with a specific effect against the SARS-CoV-2, and the search for already known substances that could reduce the damage to the body during infection. Our team, together with the Institute of Molecular Genetics of the Russian Academy of Sciences, had recently synthesized a new compound - salicyl-β-alanyl-L-histidine (salicyl-carnosine). Salicyl-carnosine was synthesized from carnosine and acetylsalicylic acid (aspirin) [Tanashyan M.M., Fedorova T.N., Stvolinsky S.L. and others. A tool with antiplatelet, cytoprotective and antioxidant activity. Patent RU 2694061 C 1, Date of registration: 07/09/2019. Patent RU 2694061 C 1]. The description of the synthesis procedure has been previously published (Kulikova et al., 2020). The natural dipeptide carnosine (β-alanyl-L-histidine) is characterized by high antioxidant activity (Prokopieva et al., 2016). Its effectiveness as an antioxidant and cytoprotective agent has been shown both on neuronal cultures and in various experimental models of parkinsonism and cerebral ischemia in animals (Berezhnoy et al., 2019; Boldyrev et al., 2013). In addition, the efficacy of carnosine has been demonstrated in the treatment of mice infected with swine flu H9N2 (Xu et al., 2015).
However, to achieve a stable protective effect in humans, the introduction of excessive doses of carnosine is required to compensate for its hydrolysis under the action of a specific dipeptidase - serum carnosinase (Wolos and Piekarska, 1975. Binding carnosine to a different molecule, and thus making it inaccessible to the enzyme, would keep the protective effect while negating its hydrolysis in the human body. This was done successfully by our team (Kulikova et al., 2020). Salicyl-carnosine was synthesized from acetylsalicylic acid and carnosine in accordance with the procedure presented in our published work. Salicyl-carnosine was not susceptible to hydrolysis over the course of 2 h while incubated in human serum at 37 °C, unlike carnosine, which underwent complete hydrolysis in the same conditions (Kulikova et al., 2020). According to our unpublished data, salicyl-carnosine remains in rat blood in a concentration over 10 μ/ml within 2 h after a single intravenous injection (dosage: 100 μg/ml). Thus, salicyl-carnosine remains stable while circulating in the blood for a significant period of time, which is necessary for the manifestation of its effects. As mentioned previously, inflammation is a key component of severe cases of COVID-19. Oral administration of 50 mg/Kg salicyl-carnosine over the course of 10 days post operation has been shown to decrease ulcer surface area in the Wistar rat gastric ulcer model by 77%. Meanwhile, aspirin administered in the same conditions led to a four-fold increase in ulcer surface area (Kulikova et al., 2020). Although at the present time research concerning the effects of salicyl-carnosine on systemic inflammatory processes is still underway, this data allows us to conclude that salicyl-carnosine possesses anti-inflammatory effects, since the gastric ulcer model is one of the most widely used models for testing anti-inflammatory drugs (Okabe and Amagase, 2005). Salicyl-carnosine has also been shown to decrease ADP-induced human thrombocyte aggregation by 48%, which, as demonstrated in our experiments, was analogous to the value of this parameter for aspirin and ticlopidine, which are utilized in clinical practice as antithrombotic drugs (Kulikova et al., 2020) (Fig. 5).)
Salicyl-carnosine also has antioxidant properties, as shown in various models of oxidative stress, and can stabilize erythrocytes, which is especially important in the context of tissue damage in COVID-19 cases. We have shown that superoxide scavenging activity of salicyl-carnosine is 2.5 times higher (Kulikova et al., 2020) than that of carnosine, which is considered to be an established antioxidant (Prokopieva et al., 2016). In addition, unlike aspirin, salicyl-carnosine prevented iron-induced lipid peroxidation, similarly to carnosine and trolox (Kulikova et al., 2020). It is known that secretion of pro-inflammatory cytokines leads to leukocyte respiratory burst, accompanied by oxidative stress and tissue damage (Mittal et al., 2013). In a model of BaSO4-activated leukocyte respiratory burst it was shown that salicyl-carnosine decreases BaSO4-induced chemiluminescence by one fourth. Aspirin and carnosine, meanwhile, failed to demonstrate such an effect. In this model, the only drug to possess a higher antioxidant activity than salicyl-carnosine was trolox (Kulikova et al., 2020). Thus, it was shown that salicyl-carnosine’s antioxidant effect decreases leukocyte respiratory burst, which is relevant for decreasing both oxidative stress and inflammatory tissue damage during a COVID-19 infection. Furthermore, 25 μM salicyl-carnosine decreased human erythrocyte hemolysis speed two-fold in a model of 0.2 mM sodium hypochlorite-induced oxidative stress. This effect is comparable to that of carnosine. At the same time, our experiments did not show the same effect for trolox (Kulikova et al., 2020) (Fig. 5).
We suggest that Salicyl-carnosine use in the treatment of COVID-19 patients may resolve the issue of blood clots, the formation of which causes ischemia and tissue microinfarctions, as well as thrombocytopenia, oxidative stress, and inflammation. Moreover, salicyl-carnosine does not exhibit side effects characteristic of aspirin and is stable in human blood, in contrast to carnosine (Kulikova et al., 2020). Thus, salicyl-carnosine can decrease the severity of three pathogenetic factors of COVID-19 at once and can be administered in large doses safely (Fig. 5).
7. Conclusion
Three of the key pathogenetic factors in severe cases of COVID-19 are inflammation, oxidative stress, and thrombosis. It has previously been shown that salicyl-carnosine is capable of attenuating these factors in various models, while lacking the side effects of aspirin. Thus, we suggest that salicyl-carnosine may be a promising drug for the treatment of patients with COVID-19.
CRediT authorship contribution statement
Alexander V. Lopachev: Conceptualization, Investigation, Writing - original draft, Writing - review & editing. Rogneda B. Kazanskaya: Investigation, Writing - original draft, Writing - review & editing. Anastasiya V. Khutorova: Investigation, Writing - original draft. Tatiana N. Fedorova: Project administration, Supervision, Writing - review & editing.
Declaration of competing interest
The authors declare no competing interests.
References
- Adam F., Khatib A.M., Lopez J.J., Vatier C., Turpin S., Muscat A., Soulet F., Aries A., Jardin I., Bobe R., Stepanian A., de Prost D., Dray C., Rosado J.A., Valet P., Feve B., Siegfried G. Apelin: an antithrombotic factor that inhibits platelet function. Blood. 2016;127:908–920. doi: 10.1182/blood-2014-05-578781. [DOI] [PubMed] [Google Scholar]
- Berezhnoy D.S., Stvolinsky S.L., Lopachev A.V., Devyatov A.A., Lopacheva O.M., Kulikova O.I., Abaimov D.A., Fedorova T.N. Carnosine as an effective neuroprotector in brain pathology and potential neuromodulator in normal conditions. Amino Acids. 2019;51:139–150. doi: 10.1007/s00726-018-2667-7. [DOI] [PubMed] [Google Scholar]
- Boldyrev A.A., Aldini G., Derave W. Physiology and pathophysiology of carnosine. Physiol. Rev. 2013;93:1803–1845. doi: 10.1152/physrev.00039.2012. [DOI] [PubMed] [Google Scholar]
- Buinitskaya Y.G., Roman, Wlodaver Clifford G., Kastsiuchenka Siarhei. Figshare Preprint; 2020. Highlights of COVID-19 Pathogenesis. Insights into Oxidative Damage. [Google Scholar]
- Carr A.C. A new clinical trial to test high-dose vitamin C in patients with COVID-19. Crit. Care. 2020;24:133. doi: 10.1186/s13054-020-02851-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattaneo M., Bertinato E.M., Birocchi S., Brizio C., Malavolta D., Manzoni M., Muscarella G., Orlandi M. Pulmonary embolism or pulmonary thrombosis in COVID-19? Is the recommendation to use high-dose heparin for thromboprophylaxis justified? Thromb. Haemostasis. 2020 doi: 10.1055/s-0040-1712097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavezzi A., Troiani E., Corrao S. COVID-19: hemoglobin, iron, and hypoxia beyond inflammation. A narrative review. Clin. Pract. 2020;10(2):1271. doi: 10.4081/cp.2020.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colafrancesco S., Alessandri C., Conti F., Priori R. COVID-19 gone bad: a new character in the spectrum of the hyperferritinemic syndrome? Autoimmun. Rev. 2020 doi: 10.1016/j.autrev.2020.102573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti P., Ronconi G., Caraffa A., Gallenga C.E., Ross R., Frydas I., Kritas S.K. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J. Biol. Regul. Homeost. Agents. 2020;34 doi: 10.23812/conti-e. [DOI] [PubMed] [Google Scholar]
- Coronavirus (COVID-19) Update: FDA Revokes Emergency Use Authorization for Chloroquine and Hydroxychloroquine. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-revokes-emergency-use-authorization-chloroquine-and/(accessed 25 June 2020).
- Delgado-Roche L., Mesta F. Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection. Arch. Med. Res. 2020 doi: 10.1016/j.arcmed.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinis-Oliveira R.J., Sousa C., Remiao F., Duarte J.A., Navarro A.S., Bastos M.L., Carvalho F. Full survival of paraquat-exposed rats after treatment with sodium salicylate. Free Radic. Biol. Med. 2007;42:1017–1028. doi: 10.1016/j.freeradbiomed.2006.12.031. [DOI] [PubMed] [Google Scholar]
- Duprez D.A. Angiotensin II, platelets and oxidative stress. J. Hypertens. 2004;22(6):1085–1086. doi: 10.1097/00004872-200406000-00005. [DOI] [PubMed] [Google Scholar]
- Fehr A.R., Perlman S. Coronaviruses: an overview of their replication and pathogenesis. Methods Mol. Biol. 2015;1282:1–23. doi: 10.1007/978-1-4939-2438-7_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiolaki A., Katsanos A.H., Kyritsis A.P., Papadaki S., Kosmidou M., Moschonas I.C., Tselepis A.D., Giannopoulos S. High on treatment platelet reactivity to aspirin and clopidogrel in ischemic stroke: a systematic review and meta-analysis. J. Neurol. Sci. 2017;376:112–116. doi: 10.1016/j.jns.2017.03.010. [DOI] [PubMed] [Google Scholar]
- Forstermann U. Nitric oxide and oxidative stress in vascular disease. Pflügers Archiv. 2010;459:923–939. doi: 10.1007/s00424-010-0808-2. [DOI] [PubMed] [Google Scholar]
- Geier M.R., Geier D.A. Respiratory conditions in coronavirus disease 2019 (COVID-19): important considerations regarding novel treatment strategies to reduce mortality. Med. Hypotheses. 2020;140:109760. doi: 10.1016/j.mehy.2020.109760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konig M.F., Powell M.A., Staedtke V., Bai R.-Y., Thomas D.L., Fischer N.M., Huq S., Khalafallah A.M., Koenecke A., Xiong R., Mensh B., Papadopoulos N., Kinzler K.W., Vogelstein B., Vogelstein J.T., Athey S., Zhou S., Bettegowda C. Preventing cytokine storm syndrome in COVID-19 using α1 adrenergic receptor antagonists. J. Clin. Invest. 2020 doi: 10.1172/jci139642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouhpayeh S.S.L., Boshtam M., Rahimmanesh I., Mirian M., Zeinalian M., Salari-jazi A., Khanahmad N., Damavandi M.S., Sadeghi P., Khanahmad H. The molecular story of COVID-19; NAD+ depletion addresses all questions in this infection. Preprints. 2020 doi: 10.20944/preprints202003.0346.v1. [DOI] [Google Scholar]
- Kulikova O.I., Stvolinsky S.L., Migulin V.A., Andreeva L.A., Nagaev I.Y., Lopacheva O.M., Kulichenkova K.N., Lopachev A.V., Trubitsina I.E., Fedorova T.N. A new derivative of acetylsalicylic acid and carnosine: synthesis, physical and chemical properties, biological activity. Daru. 2020 doi: 10.1007/s40199-019-00323-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwiatkowski S., Borowski D., Kajdy A., Poon L.C., Rokita W., Wielgo S.M. Why we should not stop giving aspirin to pregnant women during the COVID-19 pandemic. Ultrasound Obstet. Gynecol. 2020 doi: 10.1002/uog.22063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leisman D.E., Deutschman C.S., Legrand M. Facing COVID-19 in the ICU: vascular dysfunction, thrombosis, and dysregulated inflammation. Intensive Care Med. 2020 doi: 10.1007/s00134-020-06059-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S.R., Tang Z.J., Li Z.H., Liu X. Searching therapeutic strategy of new coronavirus pneumonia from angiotensin-converting enzyme 2: the target of COVID-19 and SARS-CoV. Eur. J. Clin. Microbiol. Infect. Dis. 2020 doi: 10.1007/s10096-020-03883-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippi G., Mattiuzzi C. Hemoglobin value may be decreased in patients with severe coronavirus disease 2019. Hematol Transfus Cell Ther. 2020 doi: 10.1016/j.htct.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu w., Li h. 2020. COVID-19: Attacks the 1-Beta Chain of Hemoglobin and Captures the Porphyrin to Inhibit Human Heme Metabolism; p. v7. [DOI] [Google Scholar]
- Liu Y., Yang Y., Zhang C., Huang F., Wang F., Yuan J., Wang Z., Li J., Li J., Feng C., Zhang Z., Wang L., Peng L., Chen L., Qin Y., Zhao D., Tan S., Yin L., Xu J., Zhou C., Jiang C., Liu L. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci. China Life Sci. 2020;63(3):364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathilde G., Rolnik D.L., Hoffman M.K., Panchaud A., Baud D. Should we stop aspirin prophylaxis in pregnant women diagnosed with COVID-19? Ultrasound Obstet. Gynecol. 2020 doi: 10.1002/uog.22063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maude S.L., Frey N., Shaw P.A., Aplenc R., Barrett D.M., Bunin N.J., Chew A., Gonzalez V.E., Zheng Z., Lacey S.F., Mahnke Y.D., Melenhorst J.J., Rheingold S.R., Shen A., Teachey D.T., Levine B.L., June C.H., Porter D.L., Grupp S.A. Chimeric antigen receptor T cells for sustained remissions in leukemia. N. Engl. J. Med. 2014;371:1507–1517. doi: 10.1056/NEJMoa1407222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee D.L., Sternberg A., Stange U., Laufer S., Naujokat C. Candidate drugs against SARS-CoV-2 and COVID-19. Pharmacol. Res. 2020 doi: 10.1016/j.phrs.2020.104859. 104859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal M., Siddiqui M.R., Tran K., Reddy S.P., Malik A.B. Reactive oxygen species in inflammation and tissue injury. Antioxidants Redox Signal. 2013;20(7):1126–1167. doi: 10.1089/ars.2012.5149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore J.B., June C.H. Cytokine release syndrome in severe COVID-19. Science. 2020;368:473–474. doi: 10.1126/science.abb8925. [DOI] [PubMed] [Google Scholar]
- Needs C.J., Brooks P.M. Clinical pharmacokinetics of the salicylates. Clin. Pharmacokinet. 1985;10:164–177. doi: 10.2165/00003088-198510020-00004. [DOI] [PubMed] [Google Scholar]
- Okabe S., Amagase K. An overview of acetic acid ulcer models--the history and state of the art of peptic ulcer research. Biol. Pharm. Bull. 2005;28(8):1321–1341. doi: 10.1248/bpb.28.1321. [DOI] [PubMed] [Google Scholar]
- Otani H. The role of nitric oxide in myocardial repair and remodeling. Antioxidants Redox Signal. 2009;11:1913–1928. doi: 10.1089/ars.2009.2453. [DOI] [PubMed] [Google Scholar]
- Prokopieva V.D., Yarygina E.G., Bokhan N.A., Ivanova S.A. Use of carnosine for oxidative stress reduction in different pathologies. Oxid Med Cell Longev. 2016 doi: 10.1093/cid/ciaa432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahni S., Hickok J.R., Thomas D.D. Nitric oxide reduces oxidative stress in cancer cells by forming dinitrosyliron complexes. Nitric Oxide. 2018;76:37–44. doi: 10.1016/j.niox.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha N., Balayla G. Hydroxychloroquine and covid-19. Postgrad Med J. 2020 doi: 10.1136/postgradmedj-2020-137785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha P., Delucchi K.L., McAuley D.F., O'Kane C.M., Matthay M.A., Calfee C.S. Development and validation of parsimonious algorithms to classify acute respiratory distress syndrome phenotypes: a secondary analysis of randomised controlled trials. Lancet Respir Med. 2020;8:247–257. doi: 10.1016/S2213-2600(19)30369-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soliz J., Schneider-Gasser E.M., Arias-Reyes C., Aliaga-Raduan F., Poma-Machicao L., Zubieta-Calleja G., Furuya W.I., Trevizan-Baú P., Dhingra R.R., Dutschmann M. Coping with hypoxemia: could erythropoietin (EPO) Be an adjuvant treatment of COVID-19? Respir. Physiol. Neurobiol. 2020 doi: 10.1016/j.resp.2020.103476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South A.M., Tomlinson L., Edmonston D., Hiremath S., Sparks M.A. Controversies of renin-angiotensin system inhibition during the COVID-19 pandemic. Nat. Rev. Nephrol. 2020 doi: 10.1038/s41581-020-0279-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tay M.Z., Poh C.M., Renia L., MacAry P.A., Ng L.F.P. The trinity of COVID-19: immunity, inflammation and intervention. Nat. Rev. Immunol. 2020 doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Gijn J., Warlow C.P., Norrving B. Low-dose aspirin and stroke. Stroke. 1993;24:476–477. doi: 10.1161/01.str.24.3.476. [DOI] [PubMed] [Google Scholar]
- van Hecke O., Lee J. N-acetylcysteine: a rapid review of the evidence for treatment or prevention in COVID-19. Centre for Evidence-Based Medicine. 2020 https://www.cebm.net/covid-19/n-acetylcysteine-a-rapid-review-of-the-evidence-for-effectiveness-in-treating-covid-19/ [Google Scholar]
- Vénéreau E., Ceriotti C., Bianchi M.E. DAMPs from cell death to new life. Front. Immunol. 2015;6:422. doi: 10.3389/fimmu.2015.00422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdecchia P., Cavallini C., Spanevello A., Angeli F. The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur. J. Intern. Med. 2020;76:14–20. doi: 10.1016/j.ejim.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Violi F., Pastori D., Cangemi R., Pignatelli P., Loffredo L. Hypercoagulation and antithrombotic treatment in coronavirus 2019: a new challenge. Thromb. Haemostasis. 2020 doi: 10.1055/s-0040-1710317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J.Z., Zhang R.Y., Bai J. An anti-oxidative therapy for ameliorating cardiac injuries of critically ill COVID-19-infected patients. Int. J. Cardiol. 2020 doi: 10.1016/j.ijcard.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolos A., Piekarska K. Carnosinase in the kidney and liver. Int. J. Biochem. 1975 doi: 10.1016/0020-711X(75)90123-8. [DOI] [PubMed] [Google Scholar]
- Xiao X., Zhang C., Ma X., Miao H., Wang J., Lui L., Chen S., Zeng R., Chen Y., Bihl J.C. Angiotensin-(1-7) counteracts angiotensin II-induced dysfunction in cerebral endothelial cells via modulating Nox2/ROS and PI3K/NO pathways exp. Cell Res. 2015;336:58–65. doi: 10.1016/j.yexcr.2015.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu P., Zhou Q., Xu J. Mechanism of thrombocytopenia in COVID-19 patients. Ann. Hematol. 2020;1:4. doi: 10.1007/s00277-020-04019-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu T., Wang C., Zhang R., Xu M., Liu B., Wei D., Wang G., Tian S. Carnosine markedly ameliorates H9N2 swine influenza virus-induced acute lung injury. J. Gen. Virol. 2015;96:2939–2950. doi: 10.1099/jgv.0.000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang D., Elner S.G., Bian Z., Till G.O., Petty H.R., Elner V.M. Pro-inflammatory cytokines increase reactive oxygen species through mitochondria and NADPH oxidase in cultured RPE cells. Exp. Eye Res. 2007;85:462–472. doi: 10.1016/j.exer.2007.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Q., Wang B., Mao J. The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19. J. Infect. 2020;60:607–613. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaim S., Chong J.H., Sankaranarayanan V., Harky A. COVID-19 and multiorgan response. Curr. Probl. Cardiol. 2020;45:8. doi: 10.1016/j.cpcardiol.2020.100618. [DOI] [PMC free article] [PubMed] [Google Scholar]