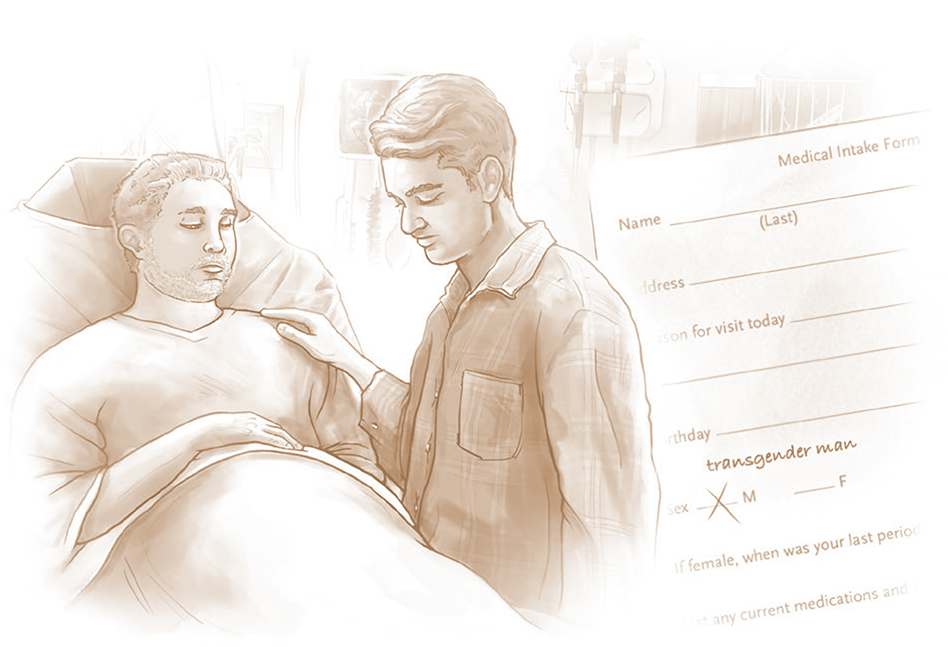
Sam, a 32-year-old man, was brought to the emergency department by his boyfriend. Sam reported an 8-hour history of severe (8 out of 10), intermittent lower abdominal pain. In triage, he had a blood pressure of 185/84 mm Hg and a heart rate of 67 beats per minute. The triage nurse noted that he was an obese man who appeared comfortable between bouts of pain. Sam told the nurse that he was a transgender man. His electronic medical record (EMR) indicated that he was male. He had previously used testosterone, as well as antihypertensives, both of which he had discontinued because he’d lost his insurance coverage. It had been several years since he last menstruated. He had taken a home pregnancy test that morning and got a positive result, but he wondered whether it was a false positive. He added that he had “peed himself” that morning.
The triage nurse assessed him to be a man with abdominal pain who had not taken his prescribed blood-pressure medications. Determining that his condition was stable, she triaged him to nonurgent assessment. Laboratory samples were drawn, including one for human chorionic gonadotropin (hCG) testing, and Sam awaited further evaluation.
Several hours later, an emergency physician came to evaluate him. She noted the positive results of the serum hCG test and took a more detailed history, considering possible early pregnancy complications. On examination, she noted that his abdomen was not only obese but also gravid. The evaluation had changed: the patient had severe abdominal pain, possible ruptured membranes, and hypertension in advanced pregnancy, which suggested possible labor, placental abruption, or preeclampsia — urgent conditions presenting a potential emergency.
Bedside ultrasonography was performed, confirming an advanced pregnancy with unclear presence of fetal cardiac activity. The obstetrics team was paged urgently. On pelvic exam, the cervix was found to be dilated to 4 to 5 cm. The umbilical cord was palpated in the vagina: Sam had cord prolapse of uncertain duration. The fetal head was immediately elevated. Sam was rapidly counseled regarding the findings and the need for an emergency caesarean delivery. He consented and was transferred to the operating room for further evaluation. In the operating room, no fetal heartbeat could be detected on ultrasound. Given the fetal death, Sam was transferred to a delivery suite where, moments later, he delivered a stillborn baby.
Social Analysis: The Power and Limits of Classification
Classification is at the heart of both medicine and social interactions (indeed, medicine is a social practice). The diagnostic process includes attributing signs and symptoms to disease categories, which in turn prompt action.1 Classification is essential because it simplifies complex physiological phenomena into dichotomous questions: Does the patient have a given disease? Does the patient have risk factors? Does the patient need to see a specialist? Classification is particularly important for triage, in which degrees of urgency and thus order of treatment are assigned. Understanding what happened in Sam’s case requires a basic understanding of classification itself (see box).
Social scientists study how people use classification to understand the world by dividing it into digestible, often binary categories. In medicine, classification provides powerful tools for diagnosis. However, classifications — including those of race and sex — often fail to capture complexity, preventing practitioners from taking the best course of action.
Because classification plays a central role in human social functioning, it has long been a core concept in the social sciences. We often assume that classificatory systems have consistent principles for sorting items into mutually exclusive categories that comprehensively describe the aspect of the world they are trying to capture. But social theorists have shown that, in practice, classification systems never correspond perfectly to the complex world they purport to describe.2 Moreover, humans do not perform classification in the dry, abstract way a computer does: our classification process involves perception, which is in turn influenced by expectation and experience, and much of this process is unconscious.3
In Sam’s evaluation, the triage nurse did not fully absorb the fact that he did not fit clearly into a binary classification system with mutually exclusive male and female categories. Though she had respectful intentions and nominally acknowledged the possibility of pregnancy by ordering a serum hCG test, she did not incorporate that possibility into the differential diagnosis in a way that would affect ensuing classifications and triage decision making. Despite communicating that he was transgender, Sam was not evaluated using pregnancy algorithms. Having no clear classificatory framework for making sense of a patient like Sam, the nurse deployed implicit assumptions about who can be pregnant,4 attributed his high blood pressure to untreated chronic hypertension, and classified his case as nonurgent.
A cisgender woman (a woman whose gender identity corresponds to the sex she was assigned at birth) presenting similarly — with a remote or unknown last menstrual period, positive home pregnancy test, severe abdominal pain, hypertension, and large-volume clear discharge — would almost surely have been triaged and evaluated more urgently for pregnancy-related problems. If the woman was in early pregnancy, practitioners would have considered an ectopic pregnancy; beyond 20 weeks of pregnancy, the patient would have been directed to urgent obstetric evaluation for possible labor, rupture of membranes, placental abruption, and severe preeclampsia. Such evaluation would also have included assessment of the fetal heart rate. Sam should have received the same treatment. Instead, it was only after significant delay that a practitioner took a more detailed history and conducted a physical exam, revealing that Sam was in labor, with a cord prolapse. Earlier evaluation might have resulted in detection of the cord prolapse in time to prevent fetal death.
Clinical Implications
1. Clinicians can begin by recognizing the limitations of implicit classification algorithms
Awareness of the limitations of implicit classification in patient management can improve care not only for transgender patients, but for all patients who fall through classificatory “cracks.” For instance, excessive reliance on the category of “race” may lead us to miss a diagnosis of cystic fibrosis in a multiracial child with recurrent respiratory problems. Elderly patients might not be diagnosed with sexually transmitted infections because they are assumed not to be sexually active. By staying attuned to situations that elude current classifications and creating both clinical training and procedural and structural safeguards (e.g., EMR algorithms that account for transgender patients), we may be better able to address the needs of patients who do not fit into our current classificatory schemes. Flagging of any incongruence between these schemes and an individual patient could then prompt further clarification and more appropriate care. Awareness of human diversity, coupled with logistic changes aimed at recognizing patient diversity (e.g., making medical records more nuanced), can lead to better diagnosis and treatment.
2. The health care system can create appropriate classifications for transgender people
The ability to change one’s legal sex marker can be crucial for transgender people in many areas of their lives, including safety, health insurance, employment, housing, and restroom use. Hence, the issues raised in this case cannot be resolved by preventing transgender people from changing their sex on legal documentation or in their medical chart. Most health care needs of transgender people are no different from those of cisgender people. There may be instances, however, in which it is important to recognize and address issues related to a person’s sex at birth (e.g., Does the person have a uterus?), to transition-related care (Is the person receiving hormones?), or to health disparities faced by transgender people (Has the person been a victim of transphobic violence?). Transgender people may have both routine health needs (such as preventive screening for cancers of the reproductive system and contraceptive counseling) and unique reproductive health needs (such as counseling regarding hormone treatment and fertility options and identity-affirming prenatal care).
Charting sex at birth, gender identity, and legal sex as three separate categories on formal documentation can enable nuanced and appropriate care.5 Some EMRs already offer the option of charting these characteristics separately; other EMRs would require adjustment to include these categories in charts and algorithms. Procedural changes and education related to these topics can help give practitioners and frontline staff the awareness and tools they need to provide affirming and appropriate health care for transgender and gender-diverse patients.
Case Follow-up
After discharge from the hospital, Sam reestablished care. He resumed antihypertensive treatment and requested the placement of a copper IUD. Though he had not planned or expected the pregnancy, he was heartbroken at the loss of his baby and had a major depressive episode. Despite having significant dysphoria related to menstruation, he has not resumed testosterone treatment, since he prefers to have continued menses that reassure him that he is not pregnant.
Supplementary Material
Fig. 1.
Fig. 2.
Footnotes
Contributor Information
Daphna Stroumsa, Institute for Healthcare Policy and Innovation, University of Michigan, Ann Arbor Department of Obstetrics and Gynecology, University of Michigan, Ann Arbor.
Elizabeth F.S. Roberts, Department of Anthropology, University of Michigan, Ann Arbor
Hadrian Kinnear, Department of Medical Scientist Training Program, University of Michigan, Ann Arbor
Lisa H. Harris, Department of Obstetrics and Gynecology, University of Michigan, Ann Arbor
References
- 1.Goldstein Jutel A Putting a name to it: diagnosis in contemporary society. Baltimore: Johns Hopkins University Press, 2011. [Google Scholar]
- 2.Foucault M The order of things: an archaeology of the human sciences. New York: Pantheon Books, 1970. [Google Scholar]
- 3.Bowker GC, Leigh Starr S. Sorting things out: classification and its consequences. Cambridge, MA: MIT Press, 2000. [Google Scholar]
- 4.Fausto-Sterling A Sex/gender: biology in a social world. New York: Routledge, 2012. [Google Scholar]
- 5.Grasso C, McDowell MJ, Goldhammer H, Keuroghlian AS. Planning and implementing sexual orientation and gender identity data collection in electronic health records. J Am Med Inform Assoc 2019;26:66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.