Abstract
Background In the classic description of perilunate injuries, the short radiolunate ligament (SRL) remains intact.
Objective This study was aimed to determine the occurrence of SRL disruptions with perilunate injuries and review the clinical and radiographic outcomes after surgical management.
Patients and Methods A retrospective review was conducted for patients who sustained a perilunate injury and a concomitant disruption of the SRL at a single–level-1 trauma center between January 2013 and January 2017. Patients with the combined injury pattern were compared with those with perilunate injury alone without SRL injury during the study period. Outcome measures included pain scores (visual analogue score), wrist and forearm range of motion, patient's return to their former occupation, and multiple radiographic parameters.
Results Twenty-seven patients were treated operatively for a perilunate injury. Eight of these patients (30%) were found to have associated disruption of the SRL. When compared with patients with perilunate injury alone, these patients had a lower rate of return to work (57% [4 of 7] vs. 92% [12 of 13]), a significantly longer mean length of time to return to work (5.9 vs. 3.8 months), and a higher rate of associated upper extremity injury (75% [3 of 8] vs. 16% [3 of 19].
Conclusion Combined SRL disruption and perilunate dislocation or fracture dislocation represent a high-energy variant from the classic description of a perilunate injury. A heightened awareness for this combined injury pattern should be maintained when treating patients with perilunate injuries.
Level of Evidence This is a Level III, prognostic study.
Keywords: perilunate injury, radiocarpal dislocation, perilunate dislocation, transscaphoid perilunate fracture dislocation, short radiolunate ligament
Perilunate injuries are relatively uncommon and traditionally occur in young males after high-energy trauma such as motor vehicle collisions or falling from a height. 1 These injuries can go undiagnosed or misdiagnosed, leading to delay in treatment and poor outcomes. 2 This injury pattern was first described by Malgaigne in 1855. 3 Later, Mayfield et al performed a cadaveric analysis of 32 wrists to elucidate the mechanism of injury producing the predictable pattern of perilunate instability. 4
Perilunate injuries are postulated to occur when the wrist is placed in forceful extension, ulnar deviation, and intercarpal supination. 4 5 Sequential injury to the ligamentous structures progresses in a radial to ulnar fashion with disruption of the scapholunate ligament, dislocation of the lunocapitate articulation, subsequent disruption of the lunotriquetral ligament with carpal dissociation from the lunate, and lastly, dislocation of the lunate from the carpus into the carpal tunnel. The proposed mechanism of injury and staging system assumes that the short radiolunate ligament (SRL) remains intact throughout the spectrum of perilunate injuries, thus providing radiocarpal stability after anatomic repair or reconstruction of the scapholunate and lunotriquetral ligaments. The results of Mayfield et al were reproduced in another cadaveric study by Meade et al. 6 However, there is no literature to date that validates this mechanistic staging system for clinical application. 7 However, we have noted several patients with perilunate injuries who, at the time of operation, were found to have concomitant disruption of the SRL ligament which may represent an unusual variant to the classically described perilunate injury pattern.
Therefore, the aim of our study was to report a single-center prevalence of concomitant SRL ligament disruption in the setting of a perilunar injury. A secondary aim was to compare clinical and radiographic outcomes in this cohort to patients with isolated perilunar injuries, and to discuss the implications of managing these unique injuries.
Methods
After obtaining approval from institutional review board (IRB), a retrospective review was conducted for patients who sustained a perilunate injury with or without a scaphoid fracture at a single–level-1 trauma center between January 2013 and January 2017. Patients were identified through a combination of International Classification of Disease 9th/10th Revision (ICD-9/ICD-10) codes, current procedural terminology (CPT) codes, and operative diagnoses during this time period for a perilunate injury. Subsequently, the records of these patients were reviewed to identify patients with intraoperative confirmation of disruption of the SRL ligament. All patients with a perilunate injury were included in the study. Surgeries were performed by one of three fellowship-trained hand surgeons.
Information regarding the type of perilunate injury as defined by Herzberg, surgical procedures, associated injuries, and complications were recorded. 8 Clinical outcome measures included pain per the visual analog scale (VAS) from 0 to 10, wrist and forearm range of motion (ROM) measured with a handheld goniometer, and patient's return to their former occupation. Radiographic outcome measures included modified carpal height ratio (MCHR) as described by Nattrass et al, scapholunate (SL) angle, and ulnar translocation of the carpus as described by Wollstein et al. 9 10 11
The surgical procedure for combined dorsal and volar approach to perilunar injuries has been previously described. 12 In brief, the dorsal approach to the carpus is performed through an ulnar-based retinacular flap from the third to fifth extensor compartments and a ligament-sparing capsulotomy. 13
In cases of lesser arc injuries, the lunate is reduced to a neutral position in the sagittal and coronal plane within the lunate facet and transfixed with a 0.045-inch Kirschner's wire (K-wire) across the radiolunate articulation to serve as a foundation for reconstruction. Next, the scaphoid and triquetrum are reduced to the lunate and K-wires are inserted across these articulations as well.
In cases of transscaphoid fracture dislocations, the scaphoid is reduced and a headless compression screw is inserted to stabilize the fracture. Subsequently, the lunotriquetral (LT) articulation is reduced and a 0.045 K-wire is inserted for stabilization. In all cases, a scaphocapitate K-wire is inserted to neutralize the flexion moment of the scaphoid. If an associated distal radius fracture is present, this is reduced and stabilized first to create a stable foundation upon which the carpal reconstruction can be performed. The avulsed portions of the scapholunate (SL) and/or LT ligaments are identified, the site of avulsion is decorticated to cancellous bone to prepare a healthy bed for ligament attachment, and a suture anchor repair is performed of the dorsal LT ligament in all cases and the dorsal SL ligament in pure lesser arc injuries.
The volar approach to the carpus is through a longitudinal incision ulnar to the palmaris longus tendon or as part of an extensile carpal tunnel release, the latter is performed only if the patient has preoperative symptoms consistent with median nerve neuropathy. The transverse rent through the volar carpal capsule at the space of Poirier is repaired with 3–0 nonabsorbable sutures. The volar SL and LT ligaments are not routinely repaired. The origin of the extrinsic volar radiocarpal ligaments is identified and if avulsed from the volar rim of the distal radius ( Fig. 1A ), this area is decorticated ( Fig. 1B ) and a suture anchor repair is performed ( Fig. 1C ). Otherwise, if the short and long radiolunate ligaments (LRL) have been avulsed from the volar surface of the lunate, this is repaired with a suture anchor. The dorsal ligament sparing capsulotomy and the retinacular flap is repaired with 3–0 absorbable suture with the extensor pollicis longus tendon transposed out of the third extensor compartment. All pins are cut deep to the skin and left subcutaneous.
Fig. 1.
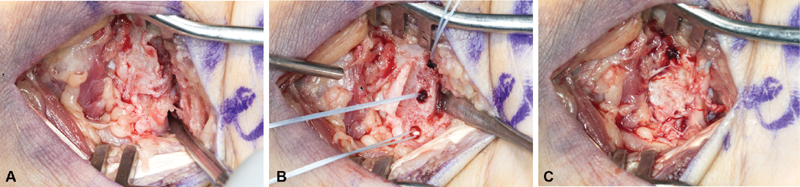
Volar radiocarpal ligament repair. Through the extended carpal tunnel approach, the volar radiocarpal ligaments (short and long radiolunate) can be evaluated for avulsion injuries ( A ). After thorough decortication of the short radiolunate origin on the volar rim of the distal radius ( B ), suture anchors can be inserted to repair the injured volar radiocarpal ligaments ( C ).
The postoperative dressing consists of a short arm, volarly based, and thumb spica plaster splint with the thumb interphalangeal (IP) joint free. Immediate hand ROM is encouraged and the patient is non–weight bearing on the operative extremity. At 2-week postoperatively, the wrist is transitioned into a short arm, thumb spica, and fiberglass cast with the IP joint free for an additional 6 weeks. The pins are removed at 8-week postoperative and the wrist is placed into a short arm, thumb spica removable orthosis, and a home-going program for radiocarpal, midcarpal, and hand ROM is initiated. At 3-month post-operatively, the wrist brace is discontinued and the patient is instructed on further ROM and strengthening exercises without any activity restrictions.
Evaluation of continuous variables was performed using calculation of mean and range values and paired continuous variables were analyzed using a paired t -test.
Results
Twenty-seven patients were treated for perilunate injuries over the 4-year study period. Eight of these 27 patients were noted to have sustained a concomitant SRL ligament disruption yielding a 30% prevalence of the combined injury pattern. Demographic information is listed in Table 1 . Mean age at time of injury was 31.9 years (range: 20–53 years) in the combined injury group and 30.9 years (range: 21–66 years) in the isolated perilunate injury group. All injuries within the combined group were the result of a high-energy mechanism, while 5 of 19 perilunate injuries occurred after a fall onto an outstretched hand. Six of eight patients within the combined injury group sustained associated injuries that were statistically significant compared with the perilunate group ( Table 1 ; p = 0.04).
Table 1. Patient demographics.
| Combined injury ( n = 8) |
Isolated perilunate injury ( n = 19) |
p -Value | |
|---|---|---|---|
| Age (y) | 31.9 | 30.4 | 0.78 |
| Gender (% male) | 88 (7) | 84 (16) | 0.80 |
| Hand dominance (% RHD) | 88 (7) | 74 (14) | 0.38 |
| Dominant hand involved (%) | 63 (5) | 58 (11) | 1.0 |
| Associated injuries (%) | 75 (6) | 16 (3) | 0.04 |
| Mechanism of injury | 63% (5) MCC/MVC 38% (3) Fall greater than 20 feet |
42% (8) MVC/MCC 26% (5) FOOSH 21% (4) crush injury 5.3% (1) fall greater than 20 feet 5.3% (1) fall less than 20 feet |
Abbreviations: FOOSH, fall on outstretched hand; MCC, motor cycle collision; MVC, motor vehicle collision; RHD, right hand dominant.
Intraoperative visualization of SRL ligament disruption was confirmed in all patients with soft tissue avulsion of the SRL ligament from the volar rim of the radius in seven patients and from the lunate in one patient. In these seven patients, variable amount of injury to the LRL was noted in all cases of combined injuries ranging from partial to near complete avulsions from the distal radius. However, this was not quantified since the SRL was the focus of this study. The radioscaphocapitate ligament was noted to be intact in all patients. Table 2 outlines the characteristics of each patient with a combined injury. All eight patients with a combined injury pattern underwent a combined volar and dorsal approach to the wrist. Lunate or perilunate open reduction with SRL ligament repair was performed in seven patients. The remaining patient underwent primary proximal row carpectomy.
Table 2. Patient characteristics of combined perilunate injury with short radiolunate ligament disruptions.
| Pt. | Age (y) | Gender | Type of perilunar injury | Herzberg's classification | Associated injuries | Additional fixation methods a | Additional procedures | Duration of HWR removal b (wk) | Complications | ROM at terminal follow-up (degrees) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 26 | M | Perilunate fracture dislocation | Stage 1 | Scaphoid fracture | HCS (scaphoid) | CTR | 9 | AVN of the scaphoid | N/A |
| 2 | 30 | M | Perilunate fracture dislocation | Stage 1 | Ulnar nerve transection; TFCC avulsion; scaphoid fracture; radial styloid fracture | HCS (scaphoid); DBP+ | PIN neurectomy | 15 | Deep Enterobacter infection; DRUJ joint instability; scaphoid nonunion; AVN scaphoid proximal pole | F = 20 E = 30 |
| 3 | 27 | M | Perilunate dislocation | Stage 1 | Radial styloid fracture | F-S fixation (radial styloid) | PIN neurectomy; radial styloid ORIF | 13 | None | F = 30 E = 30 P = 90 S = 90 |
| 4 | 49 | M | Lunate dislocation | Stage 2a | Open ulnar shaft fracture; distal radius fracture; radial neck fracture; coronoid fracture; elbow dislocation; glenohumeral dislocation | LC-DCP plate (ulna); DBP (radius); F-S fixation (radius) | CTR; PIN neurectomy; ORIF ulna; distal radius; radial neck | 12 | Lunate AVN | F = 40 E = 0 P = 45 S = 60 |
| 5 | 20 | M | Perilunate dislocation | Stage 2a | Ulnar styloid fracture; radial styloid fracture | CTR | 10 | None | F = 65 E = 60 P = 90 S = 90 |
|
| 6 | 21 | F | Perilunate dislocation | Stage 2a | None | CTR | 7 | Persistent VISI | F = 40 E = 30 |
|
| 7 | 29 | M | Perilunate dislocation | Stage 1 | None | None | 8 | None | F = 40 E = 45 P = 95 S = 80 |
|
| 8 | 53 | M | Perilunate dislocation | Stage 2b | Distal radius fracture; ulnar styloid fracture; radial head fracture; radial nerve neuropraxia | VLP (distal radius fracture) | ORIF distal radius; Radial head replacement | 3 | Radial nerve palsy; HO formation | F = 10 E = 30 P = 90 S = 90 |
Abbreviations: AVN, avascular necrosis; CTR, carpal tunnel release; D, dorsal approach; DBP, dorsal bridge plate; DRUJ, distal radioulnar joint; E, extension; F, flexion; F-S, fragment-specific; HCS, headless compression screw; HO, heterotopic ossification; HWR, hardware removal; ORIF, open reduction internal fixation; PIN, posterior interosseous nerve; PT, patient; R, direct radial approach; ROM, range of motion; TFCC, triangular fibrocartilage complex; V, volar approach; VISI, volar intercalated segmental instability; VLP, volar locking plate.
Additional methods of fixation and stabilization other than Kirschner's wires (K-wires) and suture anchor.
Time from index surgery to K-wire removal; +dorsal bridge plate utilized to stabilize the radiocarpal joint after the combined injury.
Patients with a combined injury pattern had a mean follow-up of 9.2 months (range: 3–36 months), and the isolated perilunate injury group had a mean follow-up of 4.6 months (range: 2–11 months). Four of seven patients returned to work at their previous level of function within the combined injury group at an average of 5.3 months. Two patients were active duty military and were unable to return to duty, receiving a medical discharge following injury. When compared with patients with perilunate injury alone, these patients had a lower rate of return to work (57% [4 of 7] vs. 92% [12 of 13], p = 0.01) and a significantly longer length of time to return to work in those patients who were able to return (5.9 vs. 3.8 months, p = 0.04; Table 3 ). Pain scores and ROM at terminal follow-up did not differ between the two groups. Both groups had a similar rate of postoperative complications ( Table 3 ).
Table 3. Comparison of clinical outcomes of patients with combined perilunar injury with short radiolunate ligament disruption to patients with perilunate injury alone.
| Clinical outcome measure | Combined injury | Perilunate injury | p -Value |
|---|---|---|---|
| % Returning to work | 57% (4 of 7) | 92% (12 of 13) | 0.01 |
| Time to return to work (mo) | 5.9 | 3.8 | 0.04 |
| Pain score (VAS) | 3.6 | 1.9 | 0.28 |
| Flexion (degrees) | 35 | 37 | 0.73 |
| Extension (degrees) | 32 | 34 | 0.84 |
| Pronation (degrees) | 82 | 76 | 0.42 |
| Supination (degrees) | 82 | 73 | 0.22 |
| % Complications | 63% (5 of 8) a | 32% (6 of 19) | 0.15 |
| • Scaphoid nonunion ( n = 1) | |||
| • AVN scaphoid ( n = 2) | |||
| • AVN lunate ( n = 1) | |||
| • DRUJ instability ( n = 1) | |||
| • VISI ( n = 1) | |||
| • HO formation ( n = 1) | |||
| • Radial nerve palsy ( n = 1) | |||
| • Infection ( n = 1) |
Abbreviations: AVN, avascular necrosis; DRUJ, distal radioulnar joint; HO, heterotopic ossification; VAS, visual analogue scale; VISI, volar segmental instability.
More than one complication occurred in some patients.
Five of eight patients with both a perilunate injury and SRL ligament disruption experienced complications postoperatively ( Table 2 ). One patient developed a persistent volar intercalated segmental instability (VISI) postoperatively. Avascular necrosis (AVN) was the most common complication among these patients with AVN of the lunate occurring after a lunate dislocation and both cases of AVN of the scaphoid occurring following a transscaphoid perilunate fracture dislocation. One of these patients (patient 2; Figs. 2 and 3 ) developed an Enterobacter infection that resolved after surgical debridement, yet resulted in persistent distal radioulnar joint (DRUJ) instability and scaphoid nonunion at terminal follow-up who elected to not have further surgery. A patient with a Herzberg's stage 2b perilunate dislocation developed heterotopic ossification (HO) postoperatively. Excluding the patient who underwent primary proximal row carpectomy, no patients required a revision surgery or a salvage procedure for progressive arthrosis or persistent carpal or radiocarpal instability.
Fig. 2.

Transscaphoid perilunate fracture dislocation with concomitant short radiolunate ligament disruption. Presenting posteroanterior ( A ) and lateral ( B ) radiographs of patient 1 ( Table 2 ) who sustained a combined injury. Note that the injury radiographs do not show any signs of lunate instability despite intraoperative identification of a complete disruption of the short radiolunate ligament.
Fig. 3.

Postoperative complications after a combined trans-scaphoid perilunate fracture-dislocation and short radiolunate ligament disruption. Presenting posteroanterior ( A ) and lateral ( B ) radiographs of patient 2 ( Table 2 ) who sustained a combined injury. The injury was open on the volar-ulnar aspect of the wrist ( C ). Immediate posteroanterior ( D ) and lateral ( E ) radiographs after scaphoid fracture headless compression screw fixation, short radiolunate ligament repair, and dorsal bridge plate fixation to stabilize the carpus. The patient developed an Enterobacter infection at the second metacarpal which required debridement and dorsal bridge plate removal. In addition, the posteroanterior ( F ) and lateral ( G ) radiographs at final follow-up illustrate the scaphoid nonunion with proximal pole avascular necrosis.
Among those patients with combined injuries there was no significant difference in MCHR, SL angle, or the amount of ulnar translocation when radiographs taken immediately after surgery were compared with terminal follow-up radiographs ( Table 4 ). Patients with a combined injury did have significantly lower MCHR, indicating loss of carpal height immediate postoperatively, than patients with perilunar injury alone (1.52 vs. 1.64, p = 0.02) and had significantly higher mean SL angles both immediate postoperative and at terminal follow-up, though both groups had SL angles within the range of normal ( Table 5 ).
Table 4. Comparison of radiographic parameters among patients with combined perilunar injuries with short radiolunate ligament disruptions.
| Radiographic parameter | Postoperative radiographs | Radiographs at terminal follow-up | p -Value |
|---|---|---|---|
| MCHR (mm) | 1.52 | 1.47 | 0.55 |
| SL angle (degrees) | 55.6 | 54.3 | 0.62 |
| Ulnar translocation (%) | 34.4 | 42.2 | 0.09 |
Abbreviations: MCHR, modified carpal height ratio; SL, scapholunate.
Table 5. Comparison of radiographic parameters of patients with combined perilunar injury and short radiolunate ligament disruption to patients with perilunar injury alone.
| Parameter | Combined injury immediate Postoperative |
Perilunate injury immediate Postoperative |
p -Value | Combined injury terminal F/U | Perilunate injury terminal F/U | p -Value |
|---|---|---|---|---|---|---|
| MCHR (mm) | 1.52 | 1.64 | 0.02 | 1.47 | 1.6 | 0.24 |
| SL angle (degrees) | 55.6 | 48.8 | 0.02 | 54.3 | 44.7 | 0.01 |
| Ulnar translocation (%) | 34.4 | 30.9 | 0.12 | 42.2 | 35.4 | 0.15 |
Abbreviations: F/U, follow-up; MCHR, modified carpal height ratio; SL, scapholunate.
Discussion
Perilunate injury with concomitant disruption of the SRL ligament occurred with a 30% prevalence in the current series and represent an unusual variant to the classically described perilunate injury that is similarly sustained from high-energy mechanisms, resulting in lower rates of return to work, and marked delays in returning to work when compared with perilunate injury alone. Both types of injuries are relatively uncommon and most frequently are the result of high-energy trauma in young patients. 8 14 15 In up to 25% of cases, missed or incorrect diagnosis may lead to a delay in treatment and undue complications. 8 16 17 18 Perilunate injuries have been categorized into four distinct stages of injury progression by Mayfield et al; however, disruption of the radiocarpal ligaments, specifically the SRL ligament, has not been described as part of this mechanistic classification system. 3 4
Many authors discourage nonoperative treatment of perilunate injuries, and instead recommend open reduction to directly assess and treat ligamentous disruptions. 8 14 19 20 21 Nonoperative treatment is associated with poor long-term outcomes including nonunion, malunion, AVN, persistent carpal instability, and ultimately, and posttraumatic arthritis. 2 16 20 22 23 24 25 26 Currently, the gold standard for acute management of these injuries includes open reduction, ligament repair, and fracture fixation. 2 8 20 22 27 28 29 30 31 32 33 34 35 Many advocate for a dorsal only approach, others argue in favor of using a volar approach, while others support a combined approach. 16 22 29 30 33 35 36
A traditional dorsal carpal approach provides visualization of the proximal row and midcarpal joints, while the volar approach allows for visualization of the volar intrinsic and extrinsic carpal ligaments while facilitating decompression of the median nerve if necessary. A combined approach is often discouraged due to the increased exposure and the postulated association of increased risk of wound complications, stiffness, and flexor tendon adhesions. 33 Additionally, in a small series of 39 patients, Kremer et al reported inferior subjective and clinical outcomes when a combined approach was used compared with patients undergoing a dorsal approach alone. 37 The authors' indication for the addition of a volar approach was to aid in lunate reduction or in cases of median neuropathy, potentially reflecting an increased severity of injury. 37
On the contrary, many report success with a combined approach for perilunate injuries. 28 33 38 Sotereanos et al concluded that a combined volar–dorsal approach for the treatment of severe perilunate injury in 11 patients led to high patient satisfaction, pain reduction, and improved ROM and grip strength. 33 Hildebrand et al used a combined approach in a cohort of 22 patients with a perilunate injury and demonstrated a 75% return to work rate (three of four patients). 28 The addition of a volar approach allows the surgeon to repair the volar LT ligament and/or the volar capsule, release the carpal tunnel when necessary, and above all, evaluate and treat concomitant extrinsic volar radiocarpal ligament injuries. 39 Given the observed high prevalence of intrinsic carpal and extrinsic radiocarpal injuries in the current study, it may be beneficial to evaluate and treat perilunate injuries via open reduction with a combined dorsal and volar approach to evaluate the integrity of the volar radiocarpal ligaments if injured to prevent latent radiolunate or carpal instability and progressive arthrosis.
Similar to perilunate injuries, radiocarpal dislocations traditionally result from injuries that cause intercarpal supination yet results in disruption of the radiocarpal ligaments and capsule. 4 The combined injury patterns described in this study may be a product of a hybrid mechanism of injury between a perilunate injury and radiocarpal dislocation. To prevent chronic instability and development of posttraumatic arthritis, treatment of radiocarpal dislocations focuses on repairing the SRL and radioscaphocapitate ligaments, the primary stabilizers that prevent volar and ulnar translocation, respectively. 13 40 41 The goals of managing these injuries involve achieving a concentric reduction of the radiocarpal joint, decompression of neurovascular structures, and repairing the volar extrinsic radiocarpal ligaments. 41 Primary ligamentous repair, percutaneous pinning, or arthrodesis, all have been described in the treatment of radiocarpal dislocations. 15 An extensile volar approach allows decompression of the median and ulnar nerves through the carpal tunnel and Guyon's canal if deemed necessary, respectively, as well as repair of the volar radiocarpal ligaments. 41 Therefore, similar to the recommendations for the operative management for radiocarpal dislocations, in the setting of perilunate injury with injury to the SRL may require repair. However, further clinical studies are necessary with longer follow-up to determine if it can affect long-term clinical and/or radiographic outcomes.
Following both nonoperative and operative management of radiocarpal ligament disruptions, patients lose an average of 30 to 40% wrist ROM. 40 41 42 43 Furthermore, ulnar translocation of the carpus and chronic instability is known consequences following disruption of the volar radiocarpal ligaments, in particular, the radioscaphocapitate ligament. In a retrospective review of seven patients with isolated radiocarpal dislocations, four of five patients developed persistent ulnar translocation of the carpus regardless of treatment method. 40 The most common complication following these injuries is posttraumatic arthrosis that has been reported to occur in 11 to 31% of patients. 15 40 42
High rates of complication are seen following isolated radiocarpal dislocations or perilunate injuries on the order of 39 and 26%, respectively. 40 44 The mean incidence of posttraumatic arthrosis is 38% in perilunate injury and 22% after radiocarpal dislocation. 15 42 45 Outcomes depend on the severity of the initial injury, time to diagnosis and treatment, and achieving a concentric and stable reduction of the midcarpal radiocarpal joints. 45 46 Additionally, patients with both types of injuries can expect a marked loss of ROM following the injury. 40 41 42 43 45 46 However, these complications do not necessarily correlate with poor patient outcomes in either types of injury. In a cohort of 18 patients who had sustained a perilunate injury, Forli et al noted that 12 patients developed posttraumatic arthrosis following a yet observed no association with reduced function in these patients. 27 Furthermore, 40 of 42 patients with perilunar injuries, in a study by Melone et al, were able to return to their preinjury activities. 47 Similarly, in a retrospective review of 26 patients treated for a radiocarpal dislocation, Yuan et al noted favorable outcomes at 14.6-year follow-up as measured by both patient rated wrist evaluation scores and disabilities of the arm, shoulder, and hand scores, despite a 31% incidence of posttraumatic arthritis. 15
The goal of managing combined perilunate injuries and SRL ligament disruptions is to anatomically reconstruct the carpus and stabilize the radiocarpal joint while minimizing pain and maintaining functional ROM. 1 The study population in the current study achieved a low overall mean and median pain score at terminal follow-up (3.6 vs. 4.0). Both groups of patients exhibited severe limitations in their postoperative wrist ROM consistent with previous literature for either injury pattern alone. 37 40 42 Final radiographs among those with combined injuries demonstrated loss of carpal height when compared with the general population (1.47 vs. 1.57 ± 0.05) with restoration of a normal SL angle (54 degrees). 28 30 48 Nonetheless, three of seven patients were able to return to work at their previous level of employment and one patient returned to work with restrictions.
A high correlation exists between pain relief and return to work, yet a poor correlation exists between radiographic and functional outcomes. 2 4 27 28 49 Despite prompt recognition and treatment, patients with perilunar injury, and concomitant SRL ligament disruption had a lower rate of return to work and slower return to work than those with perilunate injury alone. These patients also had a higher rate of associated injury which may be indicative of a greater amount of energy and force that was imparted through the extremity to sustain these injuries.
There are several limitations to our study. The retrospective nature and small sample size may serve to underpower this study. Follow-up was also limited among our patient population, limiting our ability to comment on the development of posttraumatic arthritis. However, this study represents a single-center experience of a rare injury pattern that has not been previously reported. Also, the magnitude of injury to the LRL was not reported since the focus of the study was to report the prevalence of injury to the SRL which has anecdotally been reported to not be injured in the most widely accepted pathoanatomic description of perilunate injuries.
Perilunate injuries with concomitant SRL disruption represents a high-energy variant of the mechanistic classification system of Mayfield et al. Identification of this injury is only possible with adequate exposure of the volar radiocarpal ligaments that should be repaired in the same setting. With greater recognition of this perilunate variant, further studies can be performed comparing the long-term clinical and radiographic outcomes in comparison to the more classic perilunate injuries.
Funding Statement
Funding None.
Footnotes
Conflict of Interest None declared.
References
- 1.Muppavarapu R C, Capo J T. Perilunate dislocations asnd fracture dislocations. Hand Clin. 2015;31(03):399–408. doi: 10.1016/j.hcl.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Herzberg G, Comtet J J, Linscheid R L, Amadio P C, Cooney W P, Stalder J. Perilunate dislocations and fracture-dislocations: a multicenter study. J Hand Surg Am. 1993;18(05):768–779. doi: 10.1016/0363-5023(93)90041-Z. [DOI] [PubMed] [Google Scholar]
- 3.Melsom D S, Leslie I J. Carpal dislocations. Curr Orthop. 2007;21(04):288–297. [Google Scholar]
- 4.Mayfield J K, Johnson R P, Kilcoyne R K. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980;5(03):226–241. doi: 10.1016/s0363-5023(80)80007-4. [DOI] [PubMed] [Google Scholar]
- 5.Linscheid R L, Dobyns J H, Beabout J W, Bryan R S. Traumatic instability of the wrist. Diagnosis, classification, and pathomechanics. J Bone Joint Surg Am. 1972;54(08):1612–1632. [PubMed] [Google Scholar]
- 6.Meade T D, Schneider L H, Cherry K. Radiographic analysis of selective ligament sectioning at the carpal scaphoid: a cadaver study. J Hand Surg Am. 1990;15(06):855–862. doi: 10.1016/0363-5023(90)90003-a. [DOI] [PubMed] [Google Scholar]
- 7.Kennedy S A, Allan C H. In brief: Mayfield et al classification: carpal dislocations and progressive perilunar instability. Clin Orthop Relat Res. 2012;470(04):1243–1245. doi: 10.1007/s11999-012-2275-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herzberg G. Perilunate and axial carpal dislocations and fracture-dislocations. J Hand Surg Am. 2008;33(09):1659–1668. doi: 10.1016/j.jhsa.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 9.Gilula L A, Weeks P M. Post-traumatic ligamentous instabilities of the wrist. Radiology. 1978;129(03):641–651. doi: 10.1148/129.3.641. [DOI] [PubMed] [Google Scholar]
- 10.Nattrass G R, King G J, McMurtry R Y, Brant R F. An alternative method for determination of the carpal height ratio. J Bone Joint Surg Am. 1994;76(01):88–94. doi: 10.2106/00004623-199401000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Wollstein R, Wei C, Bilonick R A, Gilula L A. The radiographic measurement of ulnar translation. J Hand Surg Eur Vol. 2009;34(03):384–387. doi: 10.1177/1753193408101465. [DOI] [PubMed] [Google Scholar]
- 12.Blazar P E, Murray P. Treatment of perilunate dislocations by combined dorsal and palmar approaches. Tech Hand Up Extrem Surg. 2001;5(01):2–7. doi: 10.1097/00130911-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Berger R A, Bishop A T, Bettinger P C. New dorsal capsulotomy for the surgical exposure of the wrist. Ann Plast Surg. 1995;35(01):54–59. doi: 10.1097/00000637-199507000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Green D P, O'Brien E T. Classification and management of carpal dislocations. Clin Orthop Relat Res. 1980;(149):55–72. [PubMed] [Google Scholar]
- 15.Yuan B J, Dennison D G, Elhassan B T, Kakar S. Outcomes after radiocarpal dislocation: a retrospective review. Hand (N Y) 2015;10(03):367–373. doi: 10.1007/s11552-014-9736-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adkison J W, Chapman M W. Treatment of acute lunate and perilunate dislocations. Clin Orthop Relat Res. 1982;(164):199–207. [PubMed] [Google Scholar]
- 17.Garcia-Elias M, Irisarri C, Henriquez A et al. Perilunar dislocation of the carpus. A diagnosis still often missed. Ann Chir Main. 1986;5(04):281–287. doi: 10.1016/s0753-9053(86)80003-5. [DOI] [PubMed] [Google Scholar]
- 18.Gellman H, Schwartz S D, Botte M J, Feiwell L. Late treatment of a dorsal transscaphoid, transtriquetral perilunate wrist dislocation with avascular changes of the lunate. Clin Orthop Relat Res. 1988;(237):196–203. [PubMed] [Google Scholar]
- 19.Altissimi M, Mancini G B, Azzarà A. Perilunate dislocations of the carpus. A long-term review. Ital J Orthop Traumatol. 1987;13(04):491–500. [PubMed] [Google Scholar]
- 20.Cooney W P, Bussey R, Dobyns J H, Linscheid R L. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;(214):136–147. [PubMed] [Google Scholar]
- 21.Martinage A, Balaguer T, Chignon-Sicard B, Monteil M C, Dréant N, Lebreton E. [Perilunate dislocations and fracture-dislocations of the wrist, a review of 14 cases] Chir Main. 2008;27(01):31–39. doi: 10.1016/j.main.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 22.Apergis E, Maris J, Theodoratos G, Pavlakis D, Antoniou N. Perilunate dislocations and fracture-dislocations. Closed and early open reduction compared in 28 cases. Acta Orthop Scand Suppl. 1997;275:55–59. [PubMed] [Google Scholar]
- 23.Bellot F, Tran Van F, Leroy N, Blejwas D, Mertl P. [Peri-lunate wrist dislocation: long-term outcome] Rev Chir Orthop Repar Appar Mot. 2003;89(04):320–332. [PubMed] [Google Scholar]
- 24.Campbell R D, Jr, Thompson T C, Lance E M, Adler J B. Indications for open reduction of lunate and perilunate dislocations of the carpal bones. J Bone Joint Surg Am. 1965;47:915–937. [PubMed] [Google Scholar]
- 25.Moran S L, Ford K S, Wulf C A, Cooney W P. Outcomes of dorsal capsulodesis and tenodesis for treatment of scapholunate instability. J Hand Surg Am. 2006;31(09):1438–1446. doi: 10.1016/j.jhsa.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 26.White R E, Jr, Omer G E., Jr Transient vascular compromise of the lunate after fracture-dislocation or dislocation of the carpus. J Hand Surg Am. 1984;9(02):181–184. doi: 10.1016/s0363-5023(84)80137-9. [DOI] [PubMed] [Google Scholar]
- 27.Forli A, Courvoisier A, Wimsey S, Corcella D, Moutet F. Perilunate dislocations and transscaphoid perilunate fracture-dislocations: a retrospective study with minimum ten-year follow-up. J Hand Surg Am. 2010;35(01):62–68. doi: 10.1016/j.jhsa.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 28.Hildebrand K A, Ross D C, Patterson S D, Roth J H, MacDermid J C, King G J. Dorsal perilunate dislocations and fracture-dislocations: questionnaire, clinical, and radiographic evaluation. J Hand Surg Am. 2000;25(06):1069–1079. doi: 10.1053/jhsu.2000.17868. [DOI] [PubMed] [Google Scholar]
- 29.Inoue G, Imaeda T.Management of trans-scaphoid perilunate dislocations. Herbert screw fixation, ligamentous repair and early wrist mobilization Arch Orthop Trauma Surg 1997116(6-7):338–340. [DOI] [PubMed] [Google Scholar]
- 30.Inoue G, Kuwahata Y. Management of acute perilunate dislocations without fracture of the scaphoid. J Hand Surg [Br] 1997;22(05):647–652. doi: 10.1016/s0266-7681(97)80366-x. [DOI] [PubMed] [Google Scholar]
- 31.Laporte M, Michot A, Choughri H, Abi-Chahla M L, Pelissier P. [Perilunate dislocations and fracture-dislocations of the wrist, a review of 17 cases] Chir Main. 2012;31(02):62–70. doi: 10.1016/j.main.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 32.Lutz M, Arora R, Kammerlander C, Gabl M, Pechlaner S.[Stabilization of perilunate and transscaphoid perilunate fracture-dislocations via a combined palmar and dorsal approach] Oper Orthop Traumatol 200921(4-5):442–458. [DOI] [PubMed] [Google Scholar]
- 33.Sotereanos D G, Mitsionis G J, Giannakopoulos P N, Tomaino M M, Herndon J H. Perilunate dislocation and fracture dislocation: a critical analysis of the volar-dorsal approach. J Hand Surg Am. 1997;22(01):49–56. doi: 10.1016/S0363-5023(05)80179-0. [DOI] [PubMed] [Google Scholar]
- 34.Trumble T, Verheyden J. Treatment of isolated perilunate and lunate dislocations with combined dorsal and volar approach and intraosseous cerclage wire. J Hand Surg Am. 2004;29(03):412–417. doi: 10.1016/j.jhsa.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 35.Viegas S F, Bean J W, Schram R A. Transscaphoid fracture/dislocations treated with open reduction and Herbert screw internal fixation. J Hand Surg Am. 1987;12(06):992–999. doi: 10.1016/s0363-5023(87)80096-5. [DOI] [PubMed] [Google Scholar]
- 36.Moneim M S, Hofammann K E, III, Omer G E. Transscaphoid perilunate fracture-dislocation. Result of open reduction and pin fixation. Clin Orthop Relat Res. 1984;(190):227–235. [PubMed] [Google Scholar]
- 37.Kremer T, Wendt M, Riedel K, Sauerbier M, Germann G, Bickert B. Open reduction for perilunate injuries--clinical outcome and patient satisfaction. J Hand Surg Am. 2010;35(10):1599–1606. doi: 10.1016/j.jhsa.2010.06.021. [DOI] [PubMed] [Google Scholar]
- 38.Berger R A, Landsmeer J M. The palmar radiocarpal ligaments: a study of adult and fetal human wrist joints. J Hand Surg Am. 1990;15(06):847–854. doi: 10.1016/0363-5023(90)90002-9. [DOI] [PubMed] [Google Scholar]
- 39.Jones D B, Jr, Kakar S.Perilunate dislocations and fracture dislocations J Hand Surg Am 201237102168–2173., quiz 2174 [DOI] [PubMed] [Google Scholar]
- 40.Dumontier C, Meyer zu Reckendorf G, Sautet A, Lenoble E, Saffar P, Allieu Y. Radiocarpal dislocations: classification and proposal for treatment. A review of twenty-seven cases. J Bone Joint Surg Am. 2001;83(02):212–218. doi: 10.2106/00004623-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 41.Ilyas A M, Mudgal C S. Radiocarpal fracture-dislocations. J Am Acad Orthop Surg. 2008;16(11):647–655. doi: 10.5435/00124635-200811000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Mudgal C S, Psenica J, Jupiter J B. Radiocarpal fracture-dislocation. J Hand Surg [Br] 1999;24(01):92–98. doi: 10.1016/s0266-7681(99)90047-5. [DOI] [PubMed] [Google Scholar]
- 43.Nyquist S R, Stern P J. Open radiocarpal fracture-dislocations. J Hand Surg Am. 1984;9(05):707–710. doi: 10.1016/s0363-5023(84)80018-0. [DOI] [PubMed] [Google Scholar]
- 44.Israel D, Delclaux S, André A et al. Peri-lunate dislocation and fracture-dislocation of the wrist: Retrospective evaluation of 65 cases. Orthop Traumatol Surg Res. 2016;102(03):351–355. doi: 10.1016/j.otsr.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 45.Sawardeker P J, Kindt K E, Baratz M E. Fracture-dislocations of the carpus: perilunate injury. Orthop Clin North Am. 2013;44(01):93–106. doi: 10.1016/j.ocl.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 46.Budoff J E. Treatment of acute lunate and perilunate dislocations. J Hand Surg Am. 2008;33(08):1424–1432. doi: 10.1016/j.jhsa.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 47.Melone C P, Jr, Murphy M S, Raskin K B. Perilunate injuries. Repair by dual dorsal and volar approaches. Hand Clin. 2000;16(03):439–448. [PubMed] [Google Scholar]
- 48.Capo J T, Corti S J, Shamian B et al. Treatment of dorsal perilunate dislocations and fracture-dislocations using a standardized protocol. Hand (N Y) 2012;7(04):380–387. doi: 10.1007/s11552-012-9452-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Herzberg G, Forissier D. Acute dorsal trans-scaphoid perilunate fracture-dislocations: medium-term results. J Hand Surg [Br] 2002;27(06):498–502. doi: 10.1054/jhsb.2002.0774. [DOI] [PubMed] [Google Scholar]


