Abstract
The purpose was to quantify the effect of an anterior cruciate ligament (ACL) injury on balance and jump-landing performance and bilateral asymmetries. Among 500 collegiate athletes who performed a reaching test and a double-leg counter-movement jump-landing test at baseline, 8 male and 6 female athletes suffered ACL injuries. In the follow-up, they performed the reaching test 3 and 6 months after ACL reconstruction (ACLR) and the jump-landing test 6 months after ACLR. Less reaching distances for the injured leg and increased reaching distance asymmetries were observed 3 and 6 months after ACLR compared to baseline. Less peak jumping and landing forces for the injured leg and increased jumping and landing force asymmetries were found 6 months after ACLR compared to baseline. The decreased performance of the injured leg and increased asymmetries may contribute to the high ACL re-injury rates. Baseline assessments may be considered for establishing an individual’s pre-injury performance.
Keywords: Strength, Asymmetry, ACL, Re-injury, Biomechanics
Introduction
The anterior cruciate ligament (ACL) injury is one of the most common severe injuries in National Collegiate Athletic Association (NCAA) athletes (Kay et al., 2017). While extensive research has been conducted to understand and prevent ACL injuries (Dai, Mao, Garrett, & Yu, 2014), ACL injury rates had remained similar and even increased in men’s and women’s soccer in NCAA athletes between 2004 and 2013 (Agel, Rockwood, & Klossner, 2016). ACL injuries result in decreased physical function, abnormal neuromuscular control, and increased risk of knee osteoarthritis (Lohmander, Englund, Dahl, & Roos, 2007; Nagelli & Hewett, 2017; Wise & Gallo, 2019). Despite ACL reconstruction (ACLR) and post-injury rehabilitation, ACL re-injury rates have been reported to be 13–37% in a cohort of NCAA Division I athletes (Kamath et al., 2014). The high ACL re-injury rates and devastating health consequences posit a need to develop injury prevention strategies.
Individuals following ACL injuries commonly demonstrate decreased balance and strength performance and increased bilateral asymmetries compared to matched controls (Garrison, Bothwell, Wolf, Aryal, & Thigpen, 2015; Hallagin et al., 2017; Hannon, Wang-Price, Goto, Garrison, & Bothwell, 2017). These individuals also tend to load the non-injured leg more during athletic tasks (Dai, Butler, Garrett, & Queen, 2014). Moreover, increased asymmetries in knee extension moments at the initial contact of a double-leg landing has been prospectively identified as a risk factor for ACL re-injuries (Paterno et al., 2010). However, whether these asymmetries exist before the injury or result from the injury and to which extent they may affect ACL re-injury risk is still unclear. One longitudinal study compared military cadets’ jump-landing mechanics between baseline assessments before an ACL injury and follow-up assessments after ACLR with an average of 3 years apart (Goerger et al., 2015). This study, however, was limited to quantifying landing biomechanics for either the injured or non-injured leg without assessing bilateral asymmetries. Understanding how an ACL injury affects strength, balance, and jump-landing asymmetries may help explain the high ACL re-injury rates to both legs.
Effective post-injury rehabilitation and achieving objective return-to-play criteria are crucial in decreasing ACL re-injuries (Kyritsis, Bahr, Landreau, Miladi, & Witvrouw, 2016). The return-to-play criteria typically involve the use of the non-injured leg as a reference to guide the rehabilitation of the injured leg to reach a bilateral asymmetry less than 10% (Kyritsis et al., 2016). However, recent studies have questioned the use of the non-injured leg as an accurate representation of pre-injury performance, as less asymmetries could be achieved by decreased performance of the non-injured leg (Gokeler et al., 2017; Wellsandt, Failla, & Snyder-Mackler, 2017). Another strategy is to compare the performance of both legs to the normative data of matched controls (Gokeler, Welling, Zaffagnini, Seil, & Padua, 2016), but this method can be confounded by individual differences and the difficulty of obtaining matched normative data and determining a specific cutoff percentile. On the other hand, baseline assessments before ACL injuries will establish individual pre-injury performance to identify the changes for both legs.
Therefore, the purpose of this longitudinal study was to quantify the effect of an ACL injury on performance and bilateral asymmetries in a lower extremity reaching test and a double-leg counter-movement jump-landing test in NCAA Division I collegiate athletes. It was hypothesized that participants would demonstrate decreased reaching distances, jump height, peak jumping and landing forces for both injured and non-injured legs as well as increased bilateral asymmetries approximately 3 months and/or 6 months after ACLR compared to baseline.
Methods
Participants
A previous study reported the mean (± standard deviation) of peak jumping force asymmetries being 11.7% (± 12.2%) in young athletes 6 months after ACLR (Dai et al., 2014). Based on these values and the assumption that athletes had a mean of 0% asymmetry before ACL injuries, an effect size of 0.96 was estimated for a paired t-test, and a sample size of 11 was needed to achieve a power of 0.8 at a type-I error level of 0.05.
The current study was a continuation of a previous study, in which approximately 500 NCAA Division I athletes performed baseline assessments (Dai et al., 2018). At the time of baseline assessments, participants were at least 18 years old and were cleared to full sports participation. In the follow-up, 14 athletes (6 men’s American Football, 3 women’s soccer, 2 women’s basketball, 1 men’s basketball, 1 women’s volleyball, and 1 men’s wrestling; pre-injury age: 19.0 ± 1.0 years; pre-injury height: 1.82 ± 0.13 m; pre-injury mass: 81.9 ± 17.8 kg) suffered ACL injuries and were included in the current study. The University of Wyoming Institutional Review Board approved this study. Participants signed informed consent forms for both baseline and post-injury assessments.
Five ACL injuries occurred without contact with another player. Six ACL injuries occurred with indirect contact to the body other than the injured knee with another player. Three ACL injuries occurred with direct contact to the injured knee with another player. The time intervals between their baseline assessments and ACL injuries were 13.5 ± 10.6 months. The time intervals between their ACL injuries and ACLR were 0.77 ± 0.58 months. Among the 14 participants, 2 athletes had one previous ACL injury to the same side and 1 athlete had two previous ACL injuries with one to each side at the time of baseline assessments. All three athletes had their last ACLR approximately 1.5 years before the baseline assessment. One participant had two ACL injuries to the same side after the baseline assessment, and follow-up assessments were performed after the second ACL injury. Eleven participants received bone-tendon-bone grafts, and three participants received hamstring grafts. Along with ACLR, 11 participants had meniscus repair or meniscectomy, and 2 participants had medial collateral ligament (MCL) reconstruction. All participants were treated with a standard rehabilitation program under the guidance of their team doctors and athletic trainers.
Procedure
Participants performed a lower extremity anterior reaching test to assess lower extremity dynamic balance (Figure 1) and a double-leg counter-movement jump-landing test to assess lower extremity strength and landing mechanics (Figure 2) as previously described (Dai et al., 2018). Participants performed a minimum of 3 practice and 3 official reaching trials for each leg. Leg length was measured from the right anterior superior iliac crest to the right medial malleolus. The jump-landing test was performed on 2 force platforms (4060–05 or 4060–10; Bertec, Columbus, OH, USA) with vertical ground reaction forces collected at a sampling frequency of 1,000 Hz. Participants performed a minimum of 1 practice and 3 official jump-landing trials.
Figure 1.
The counter-movement jump-landing test (top) and lower extremity anterior reaching test (bottom). For the reaching test, the stance leg is the one being tested.
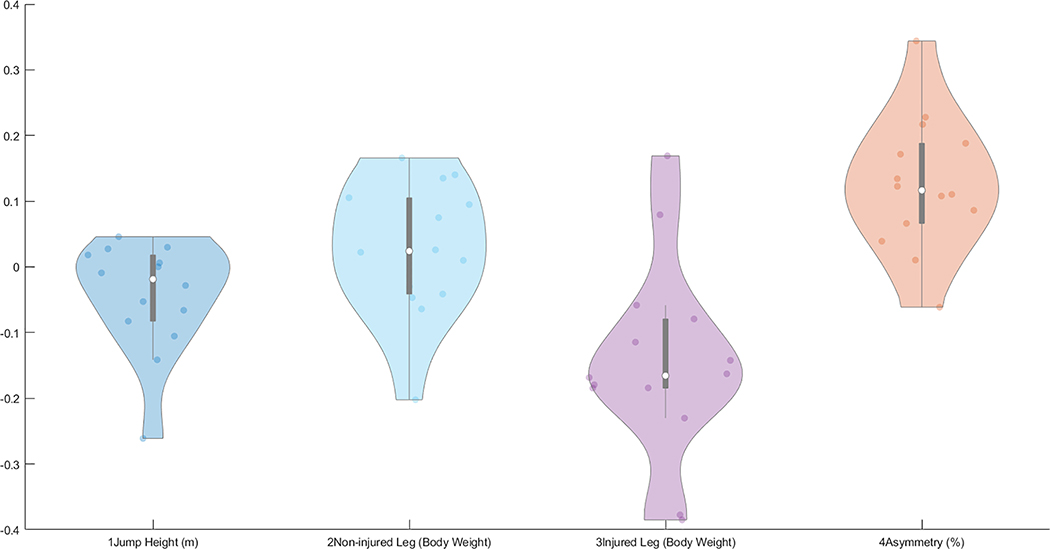
Figure 2.
Violin-plots of the changes in reaching distances and asymmetries from baseline to 6 months after ACLR
Participants performed these two tests at baseline and after their ACLR with the permission of their team physicians. Results were reported to participants and their physicians after each testing. The current study included participants’ balance performance at approximately 3 months (3.3 ± 0.7 months) after ACLR and their balance and jump-landing performance approximately 6 months (6.4 ± 1.0 months) after ACLR. These two testing times were chosen because they were used as important rehabilitation milestones (Dai et al., 2014; Garrison et al., 2015; Hallagin et al., 2017; Wellsandt et al., 2017).
Data Analysis
As previously described (Dai et al., 2018), the bilateral reaching distances and jumping and landing forces were normalized to leg length or body weight, respectively. The bilateral asymmetry index was then calculated as follows: (non-injured leg – injured leg) / (larger value of the two legs), with positive or negative values indicating greater numbers on the non-injured or injured leg, respectively. These calculations were performed using subroutines developed in MATLAB 2017b (MathWorks, Inc., Natick, MA, USA).
Repeated-measure analyses of variance (ANOVA) were performed for balance related variables among baseline, 3 months after ACLR, and 6 months after ACLR. When an ANOVA showed a significant main effect, paired t-tests were performed between each pair of two assessments. Paired t-tests were performed between baseline and 6 months after ACLR for jump-landing related variables. A type-I error rate was set at 0.05 for statistical significance. For each pairwise comparison, Cohen’s dz was calculated to assess the effect size, with Cohen’s dz < 0.5 considered “small,” 0.5 < Cohen’s dz < 0.8 considered “medium,” and Cohen’s dz > 0.8 considered “large” (Cohen, 1988). Statistical analyses were performed using the IBM SPSS Statistics 22 software (IBM Corporation, Armonk, NY, USA).
Results
Reaching distances for the injured leg were the longest at baseline, the second longest 6 months after ACLR, and the least at 3 months after ACLR (Table 1). Reaching distance asymmetries were the greatest 3 months after ACLR, the second greatest 6 months after ACLR, and the least at baseline. The effect sizes for these two variables were large between the baseline and either of the post-injury assessments and were medium between the two post-injury assessments. Less peak jumping and landing forces for the injured leg and greater peak jumping and landing force asymmetries were observed for 6 months after ACLR compared to baseline. The effect sizes were medium for peak landing forces for the injured leg and were large for the other three variables. All participants demonstrated less than 10% asymmetries in reaching distances, and only one athlete showed more than 10% asymmetries in peak jumping forces at baseline. Peak landing force asymmetries were more variable, but the average was close to 0% without showing a trend of favoring a specific leg at baseline.
Table 1.
Means ± standard deviations, p-values of ANOVAs and t-tests, and Cohen’ dz of pairwise comparisons
| Baseline | 3-month post ACLR | 6-month post ACLR | p-values of ANOVA | p-values of paired t-tests (Cohen’s dz) | |||
|---|---|---|---|---|---|---|---|
| Baseline vs. 3-month | Baseline vs. 6-month | 3-month vs. 6-month | |||||
| Reaching distance for the non-injured leg (LL) | 0.72 ± 0.09 | 0.71 ± 0.06 | 0.71 ± 0.07 | 0.873 | --- (0.11) | --- (0.12) | --- (0.00) |
| Reaching distance for the injured leg (LL) | 0.72 ± 0.06 | 0.62 ± 0.08 | 0.67 ± 0.07 | <0.001 | <0.001 (1.96) | 0.010 (0.81) | 0.021 (0.70) |
| Reaching distance asymmetry (%) | 0.00 ± 0.05 | 0.13 ± 0.10 | 0.06 ± 0.05 | 0.001 | <0.001 (1.21) | <0.001 (1.14) | 0.036 (0.63) |
| Jump height (m) | 0.37 ± 0.09 | --- | 0.33 ± 0.11 | --- | --- | 0.070 (0.53) | --- |
| Peak jumping force for the non-injured leg (BW) | 1.33 ± 0.17 | --- | 1.36 ± 0.16 | --- | --- | 0.318 (0.28) | --- |
| Peak jumping force for the injured leg (BW) | 1.31 ± 0.17 | --- | 1.16 ± 0.17 | --- | --- | 0.003 (0.97) | --- |
| Jumping force asymmetry (%) | 0.02 ± 0.06 | --- | 0.14 ± 0.08 | --- | --- | <0.001 (1.24) | --- |
| Peak landing force for the non-injured leg (BW) | 2.55 ± 0.76 | --- | 2.66 ± 0.97 | --- | --- | 0.553 (0.16) | --- |
| Peak landing force for the injured leg (BW) | 2.54 ± 0.68 | --- | 1.95 ± 0.89 | --- | --- | 0.038 (0.62) | --- |
| Landing force asymmetry (%) | 0.00 ± 0.17 | --- | 0.26 ± 0.22 | --- | --- | 0.005 (0.90) | --- |
Note: ANOVA: analyses of variance; ACLR: anterior cruciate ligament reconstruction; LL: leg length; BW: body weight; Significant differences are marked bold.
Discussion and Implications
The findings support the hypothesis that ACL injuries would decrease reaching distances and peak jumping and landing forces for the injured leg and increase bilateral asymmetries in reaching distances and peak jumping and landing forces. The observed asymmetries 3 and 6 months after ACLR are consistent with previous studies, showing individuals following ACL injuries generally demonstrate bilateral asymmetries during the Y-balance and isokinetic knee extension tests (Garrison et al., 2015; Hallagin et al., 2017; Hannon et al., 2017) as well as squatting, jump-landing, and cutting tasks (Dai, Butler, Garrett, & Queen, 2012; Dai et al., 2014; Sigward, Chan, Lin, Almansouri, & Pratt, 2018). The current study also observed small bilateral asymmetries at baseline before the ACL injuries, especially for reaching distances and peak jumping forces. Therefore, the commonly observed balance, strength, and jump-landing asymmetries following ACL injuries are more likely the consequences of the injuries instead of being present before the injuries. In addition, the increased asymmetries following ACL injuries were mainly caused by the decreased performance of the injured leg. For the injured leg, the decreased balance and strength could result in abnormal movement patterns when the leg is used to complete athletic tasks and increased its risk of re-injury. On the other hand, for the non-injured leg, inter-limb compensatory strategies during jump-landing tasks suggest individuals may overly favor the non-injured leg during athletic tasks and elevate its risk of injury. When individuals return to play without normalizing injured leg impairments and bilateral asymmetries, ACL injuries would likely further increase ACL re-injury risk in a population who have already possessed other high-risk characteristics.
The findings do not support the hypothesis that reaching distances for the non-injured leg would decrease after ACL injuries. A previous study has demonstrated decreased performance in single-leg hop tests for both injured and non-injured leg in patients 7 months after ACLR compared to control group matched by age and sex (Gokeler et al., 2017). A study has reported that in a group of patients 6 months after ACLR, more than 30% of them had less than 10% asymmetries in single-leg hop tests but their injured legs did not achieve 90% of the performance of the non-injured leg before ACLR, suggesting the performance of the non-injured leg could decrease after ACLR (Wellsandt et al., 2017). In the current study, the non-significant changes in reaching distances for the non-injured leg could be due to the differences between dynamic balance and single-leg hop tests. While joint range of motion and stability could be more critical for the reaching test, joint strength and power may be the determining factors for single-leg hop tests. Additionally, the current study involved a more homogeneous group of collegiate athletes, who were highly motivated to perform early rehabilitation following ACLR. The training stimulus might have prevented the adverse effects associated with the injury for the non-injured leg.
The findings do not support the hypothesis that jump height, peak jumping forces, and peak landing forces for the non-injured leg would decrease after ACL injuries. However, the effect size (0.53) for jump height was medium, and the p-value (0.070) for jump height indicated a trend toward significance. Post hoc analyses showed that a sample size of 17 was needed to demonstrate significant differences for jump height. Different from single-leg hop tests, the performance of a bilateral jumping task could be affected by either limb. As the peak jumping forces were similar before and after ACL injuries for the non-injured leg, the medium decrease of jump height was likely due to the decreased force production of the injured leg. However, it should be noted that the jumping force was primarily the resultant effect of the lower extremities. Similar force production for the non-injured leg did not necessarily indicate similar joint efforts, as the force vector could be placed closer or further away from a joint to result in different joint moments (Oberlander, Bruggemann, Hoher, & Karamanidis, 2012). Participants were expected to experience decreased landing forces as they landed from a lower jump height. The similar peak landing forces for the non-injured leg could be the counteracting effect between the decreased jump height and the compensatory strategy to favor the non-injured leg. Meanwhile, different from peak jumping forces, which were generated by active muscle contraction, peak landing forces are associated with the kinetic energy the body had to absorb and could be manipulated through modifying landing techniques (Dai et al., 2015). It was unknown whether participants changed their landing techniques as kinematic data were not collected.
The findings may provide information for post-injury rehabilitation. As participants demonstrated small balance and strength asymmetries before ACL injuries, the findings support the use of less than 10% asymmetries as a goal of rehabilitation and a return-to-play criterion (Kyritsis et al., 2016). A small asymmetry, however, could be achieved by decreased performance of the non-injured leg, so it’s important to include performance measurements (Wellsandt et al., 2017). In the current study, small changes were observed for reaching distances and peak jumping and landing forces for the non-injured leg. On average, the non-injured leg’s performance at 3 months after ACLR appeared to be an adequate estimate of pre-injury performance for the reaching and jump-landing tests in this population. Jump height, however, showed a trend of medium decrease 6 months after ACLR, which may be limited to represent pre-injury performance. On the other hand, individual variations were observed in jump height and non-injured leg performance, suggesting the use of post-injury performance as a reference can only be applied to some individuals. As such, baseline assessments may be considered to establish an individual’s pre-injury performance in high-risk populations.
The current study had several limitations. First, only two tests were used to reduce data collection time. Jump-landing kinematics and muscle activation (Dashti Rostami, Alizadeh, Minoonejad, Thomas, & Yazdi, in press; Goerger et al., 2015; Stanley et al., 2019), which could provide additional information for understanding ACL re-injuries, were not incorporated. The double-leg counter-movement jump has been demonstrated as a valid test to assess lower extremity strength and asymmetries (Impellizzeri, Rampinini, Maffiuletti, & Marcora, 2007). A double-leg jump-landing has also demonstrated increased sensitivity to reveal bilateral asymmetries compared to a single-leg task (Dai et al., 2014; Moya-Angeler, Vaquero, & Forriol, 2017). Second, the baseline testing was performed with an average of more than 1 year before ACL injuries, and closer baseline testing could more accurately represent pre-injury performance. Moreover, post-injury assessments were only performed 3 and 6 months after ACLR. Including additional follow-up assessments could better evaluate the effect of time on the recovery of balance and strength performance. The focus of the current study, however, was to identify the changes in balance and jump-landing performance before and after ACL injuries. While accelerated rehabilitation programs allow athletes to return to play as early as 4–6 months following ACLR (Shelbourne & Nitz, 1990), a recent review has suggested young athletes delay the return-to-play date for 2 years (Nagelli & Hewett, 2017). The current findings suggest that time alone is not likely a sufficient indicator of an athlete’s capacity to return to play and highlight the need to establish valid pre-injury performance. Third, several participants with previous ACL injuries and concomitant injuries were included, and these additional injuries could potential affect post-injury rehabilitation and participants’ performance during the tests. Secondary analyses with three subgroups (Appendix) showed similar trends of significance and effect sizes as the analyses with all 14 athletes, supporting the inclusion of all athletes as one group in the current study. However, future studies with a larger sample size are needed to identify the effect of other injuries in addition to ACL injuries on post-injury performance. Finally, although a regression analysis could be done to predict the 14 ACL injuries among the 500 athletes, such analysis was not performed as other potential risk factors such as practice and competition time, starters vs. bench players, and players’ specific positions were not recorded.
Conclusion
Collegiate athletes demonstrated decreased performance of the injured leg and increased bilateral asymmetries during a lower extremity reaching test and a double-leg counter-movement jump-landing test 3 and 6 months after ACLR compared to baseline. The impairments to the injured leg and bilateral asymmetries may contribute to the high ACL re-injury rates to both legs. Normalizing bilateral balance and strength asymmetries to be less than 10% or lower should be encouraged with the consideration of achieving pre-injury performance in post-injury rehabilitation. On average, the post-injury performance of the non-injured leg in these two tests might be used as a reference for training the injured leg in this population. Baseline assessments prior to potential ACL injuries may be considered to establish individuals’ pre-injury performance in high-risk population.
Figure 3.
Violin-plots plots of the changes in jump height, jumping forces, and asymmetries from baseline to 6 months after ACLR
Figure 4.
Violin-plots plots of the changes in landing forces and asymmetries from baseline to 6 months after ACLR
Acknowledgement
The authors thank the staff in the Department of Sports Medicine at the University of Wyoming for their support of this study.
Funding
This study was supported by research grants from the College of Health Sciences and Research Office at the University of Wyoming. Jacob Layer’s graduate assistantship was provided by the Wyoming INBRE, which was supported by a grant from the National Institute of General Medical Sciences (P20GM103432) from the National Institutes of Health.
Appendix.
Means ± standard deviations, p-values of ANOVAs and t-tests, and Cohen’ dz of pairwise comparisons for three subgroups. Subgroup I (n=10): data without three athletes with previous ACL injuries at baseline and one athlete who suffered two ACL injuries after baseline. Subgroup II (n=12): data without two athletes who had concomitant medial collateral ligament reconstruction. Subgroup II (n=11): data without three athletes who did not have concomitant meniscus repair or meniscectomy.
| Baseline | 3-month post ACLR | 6-month post ACLR | p-values of paired t-tests (Cohen’s dz) | ||||
|---|---|---|---|---|---|---|---|
| Baseline vs. 3-month | Baseline vs. 6-month | 3-month vs. 6-month | |||||
| Reaching distance for the non-injured leg (LL) | Subgroup I | 0.72 ± 0.08 | 0.71 ± 0.07 | 0.72 ± 0.08 | 0.69 (0.13) | 0.93 (0.03) | 0.67 (0.14) |
| Subgroup II | 0.72 ± 0.09 | 0.71 ± 0.06 | 0.71 ± 0.08 | 0.92 (0.03) | 0.68 (0.12) | 0.58 (0.16) | |
| Subgroup III | 0.73 ± 0.09 | 0.73 ± 0.05 | 0.73 ± 0.06 | 0.90 (0.04) | 0.89 (0.04) | 0.99 (0.00) | |
| Reaching distance for the injured leg (LL) | Subgroup I | 0.72 ± 0.06 | 0.61 ± 0.09 | 0.67 ± 0.06 | <0.001 (2.92) | 0.008 (1.07) | 0.033 (0.80) |
| Subgroup II | 0.72 ± 0.07 | 0.61 ± 0.08 | 0.67 ± 0.07 | <0.001 (1.99) | 0.035 (0.7) | 0.015 (0.83) | |
| Subgroup III | 0.72 ± 0.07 | 0.63 ± 0.08 | 0.68 ± 0.06 | <0.001 (1.72) | 0.07 (0.6) | 0.031 (0.76) | |
| Reaching distance asymmetry (%) | Subgroup I | 0.00 ± 0.05 | 0.14 ± 0.11 | 0.06 ± 0.05 | 0.004 (1.23) | 0.003 (1.25) | 0.08 (0.63) |
| Subgroup II | 0.00 ± 0.05 | 0.14 ± 0.10 | 0.05 ± 0.05 | <0.001 (1.37) | 0.005 (1.02) | 0.010 (0.89) | |
| Subgroup III | 0.00 ± 0.05 | 0.14 ± 0.10 | 0.06 ± 0.05 | 0.001 (1.36) | 0.008 (1.00) | 0.036 (0.73) | |
| Jump height (m) | Subgroup I | 0.40 ± 0.08 | --- | 0.35 ± 0.12 | --- | 0.13 (0.53) | --- |
| Subgroup II | 0.38 ± 0.10 | --- | 0.35 ± 0.09 | --- | 0.11 (0.51) | --- | |
| Subgroup III | 0.36 ± 0.10 | --- | 0.32 ± 0.13 | --- | 0.18 (0.44) | --- | |
| Peak jumping force for the non-injured leg (BW) | Subgroup I | 1.34 ± 0.15 | --- | 1.37 ± 0.13 | --- | 0.52 (0.21) | --- |
| Subgroup II | 1.35 ± 0.18 | --- | 1.36 ± 0.17 | --- | 0.54 (0.18) | --- | |
| Subgroup III | 1.35 ± 0.19 | --- | 1.37 ± 0.18 | --- | 0.54 (0.19) | --- | |
| Peak jumping force for the injured leg (BW) | Subgroup I | 1.31 ± 0.15 | --- | 1.16 ± 0.18 | --- | 0.027 (0.84) | --- |
| Subgroup II | 1.32 ± 0.18 | --- | 1.20 ± 0.14 | --- | 0.013 (0.85) | --- | |
| Subgroup III | 1.32 ± 0.19 | --- | 1.18 ± 0.19 | --- | 0.023 (0.81) | --- | |
| Jumping force asymmetry (%) | Subgroup I | 0.03 ± 0.06 | --- | 0.15 ± 0.08 | --- | 0.008 (1.07) | --- |
| Subgroup II | 0.02 ± 0.06 | --- | 0.12 ± 0.07 | --- | 0.001 (1.27) | --- | |
| Subgroup III | 0.02 ± 0.06 | --- | 0.14 ± 0.09 | --- | 0.006 (1.04) | --- | |
| Peak landing force for the non-injured leg (BW) | Subgroup I | 2.67 ± 0.78 | --- | 2.76 ± 1.14 | --- | 0.73 (0.11) | --- |
| Subgroup II | 2.57 ± 0.79 | --- | 2.78 ± 0.97 | --- | 0.35 (0.28) | --- | |
| Subgroup III | 2.55 ± 0.84 | --- | 2.72 ± 1.02 | --- | 0.48 (0.22) | --- | |
| Peak landing force for the injured leg (BW) | Subgroup I | 2.66 ± 0.69 | --- | 2.10 ± 1.00 | --- | 0.15 (0.49) | --- |
| Subgroup II | 2.47 ± 0.71 | --- | 2.11 ± 0.86 | --- | 0.16 (0.44) | --- | |
| Subgroup III | 2.51 ± 0.74 | --- | 1.97 ± 0.95 | --- | 0.09 (0.56) | --- | |
| Landing force asymmetry (%) | Subgroup I | 0.00 ± 0.18 | --- | 0.22 ± 0.24 | --- | 0.07 (0.66) | --- |
| Subgroup II | 0.03 ± 0.15 | --- | 0.22 ± 0.22 | --- | 0.016 (0.82) | --- | |
| Subgroup III | 0.00 ± 0.19 | --- | 0.27 ± 0.23 | --- | 0.017 (0.86) | --- | |
Note: ANOVA: analyses of variance; ACLR: anterior cruciate ligament reconstruction; LL: leg length; BW: body weight; Significant differences are marked bold.
Footnotes
Disclosure statement
The authors have no financial or personal conflicts of interest to declare.
References
- Agel J, Rockwood T, & Klossner D (2016). Collegiate ACL injury rates across 15 sports: National collegiate athletic association injury surveillance system data update (2004–2005 through 2012–2013). Clinical Journal of Sport Medicine, 26(6), 518–523. [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioural sciences. Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Dai B, Butler RJ, Garrett WE, & Queen RM (2012). Anterior cruciate ligament reconstruction in adolescent patients: Limb asymmetry and functional knee bracing. The American Journal of Sports Medicine, 40(12), 2756–2763. [DOI] [PubMed] [Google Scholar]
- Dai B, Butler RJ, Garrett WE, & Queen RM (2014). Using ground reaction force to predict knee kinetic asymmetry following anterior cruciate ligament reconstruction. Scandinavian Journal of Medicine & Science in Sports, 24(6), 974–981. [DOI] [PubMed] [Google Scholar]
- Dai B, Garrett WE, Gross MT, Padua DA, Queen RM, & Yu B (2015). The effects of 2 landing techniques on knee kinematics, kinetics, and performance during stop-jump and side-cutting tasks. The American Journal of Sports Medicine, 43(2), 466–474. [DOI] [PubMed] [Google Scholar]
- Dai B, Layer J, Vertz C, Hinshaw T, Cook R, Li Y, & Sha Z (2019). Baseline assessments of strength and balance performance and bilateral asymmetries in collegiate athletes. Journal of Strength and Conditioning Research, 33(11):3015–3029. [DOI] [PubMed] [Google Scholar]
- Dai B, Mao D, Garrett WE, & Yu B (2014). Anterior cruciate ligament injuries in soccer: Loading mechanisms, risk factors, and prevention programs. Journal of Sport and Health Science, 3(4), 299–306. [Google Scholar]
- Dashti Rostami K, Alizadeh M, Minoonejad H, Thomas A, & Yazdi H (in press). Relationship between electromyographic activity of knee joint muscles with vertical and posterior ground reaction forces in anterior cruciate ligament reconstructed patients during a single leg vertical drop landing task. Research in Sports Medicine. doi: 10.1080/15438627.2019.1647204. [DOI] [PubMed] [Google Scholar]
- Garrison JC, Bothwell JM, Wolf G, Aryal S, & Thigpen CA (2015). Y balance test anterior reach symmetry at three months is related to single leg functional performance at time of return to sports following anterior cruciate ligament reconstruction. International Journal of Sports Physical Therapy, 10(5), 602–611. [PMC free article] [PubMed] [Google Scholar]
- Goerger BM, Marshall SW, Beutler AI, Blackburn JT, Wilckens JH, & Padua DA (2015). Anterior cruciate ligament injury alters preinjury lower extremity biomechanics in the injured and uninjured leg: The JUMP-ACL study. British Journal of Sports Medicine, 49(3), 188–195. [DOI] [PubMed] [Google Scholar]
- Gokeler A, Welling W, Benjaminse A, Lemmink K, Seil R, & Zaffagnini S (2017). A critical analysis of limb symmetry indices of hop tests in athletes after anterior cruciate ligament reconstruction: A case control study. Orthopaedics & Traumatology, Surgery & Research : OTSR, 103(6), 947–951. [DOI] [PubMed] [Google Scholar]
- Gokeler A, Welling W, Zaffagnini S, Seil R, & Padua D (2017). Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy, 25(1):192–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallagin C, Garrison JC, Creed K, Bothwell JM, Goto S, & Hannon J (2017). The relationship between pre-operative and twelve-week post-operative Y-balance and quadriceps strength in athletes with an anterior cruciate ligament tear. International Journal of Sports Physical Therapy, 12(6), 986–993. [PMC free article] [PubMed] [Google Scholar]
- Hannon J, Wang-Price S, Goto S, Garrison JC, & Bothwell JM (2017). Do muscle strength deficits of the uninvolved hip and knee exist in young athletes before anterior cruciate ligament reconstruction? Orthopaedic Journal of Sports Medicine, 5(1), 2325967116683941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Impellizzeri FM, Rampinini E, Maffiuletti N, & Marcora SM (2007). A vertical jump force test for assessing bilateral strength asymmetry in athletes. Medicine and Science in Sports and Exercise, 39(11), 2044–2050. [DOI] [PubMed] [Google Scholar]
- Kamath GV, Murphy T, Creighton RA, Viradia N, Taft TN, & Spang JT (2014). Anterior cruciate ligament injury, return to play, and reinjury in the elite collegiate athlete: Analysis of an NCAA division I cohort. The American Journal of Sports Medicine, 42(7), 1638–1643. [DOI] [PubMed] [Google Scholar]
- Kay MC, Register-Mihalik JK, Gray AD, Djoko A, Dompier TP, & Kerr ZY (2017). The epidemiology of severe injuries sustained by national collegiate athletic association student-athletes, 2009–2010 through 2014–2015. Journal of Athletic Training, 52(2), 117–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyritsis P, Bahr R, Landreau P, Miladi R, & Witvrouw E (2016). Likelihood of ACL graft rupture: Not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. British Journal of Sports Medicine, 50(15), 946–951. [DOI] [PubMed] [Google Scholar]
- Lohmander LS, Englund PM, Dahl LL, & Roos EM (2007). The long-term consequence of anterior cruciate ligament and meniscus injuries: Osteoarthritis. The American Journal of Sports Medicine, 35(10), 1756–1769. [DOI] [PubMed] [Google Scholar]
- Moya-Angeler J, Vaquero J, & Forriol F (2017). Evaluation of lower limb kinetics during gait, sprint and hop tests before and after anterior cruciate ligament reconstruction. Journal of Orthopaedics and Traumatology, 18(2), 177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagelli CV, & Hewett TE (2017). Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? biological and functional considerations. Sports Medicine, 47(2), 221–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberlander KD, Bruggemann GP, Hoher J, & Karamanidis K (2012). Reduced knee joint moment in ACL deficient patients at a cost of dynamic stability during landing. Journal of Biomechanics, 45(8), 1387–1392. [DOI] [PubMed] [Google Scholar]
- Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, & Hewett TE (2010). Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. The American Journal of Sports Medicine, 38(10), 1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelbourne KD, & Nitz P (1990). Accelerated rehabilitation after anterior cruciate ligament reconstruction. The American Journal of Sports Medicine, 18(3), 292–299. [DOI] [PubMed] [Google Scholar]
- Sigward SM, Chan MM, Lin PE, Almansouri SY, & Pratt KA (2018). Compensatory strategies that reduce knee extensor demand during a bilateral squat change from 3 to 5 months following anterior cruciate ligament reconstruction. The Journal of Orthopaedic and Sports Physical Therapy, 48(9), 713–718. [DOI] [PubMed] [Google Scholar]
- Stanley LE, Harkey M, Luc-Harkey B, Frank BS, Pietrosimone B, Blackburn JT, & Padua DA (2019). Ankle dorsiflexion displacement is associated with hip and knee kinematics in females following anterior cruciate ligament reconstruction. Research in Sports Medicine, 27(1), 21–33. [DOI] [PubMed] [Google Scholar]
- Wellsandt E, Failla MJ, & Snyder-Mackler L (2017). Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. The Journal of Orthopaedic and Sports Physical Therapy, 47(5), 334–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wise PM, & Gallo RA (2019). Impact of anterior cruciate ligament reconstruction on NCAA FBS football players: Return to play and performance vary by position. Orthopaedic Journal of Sports Medicine, 7(4), 2325967119841056. [DOI] [PMC free article] [PubMed] [Google Scholar]