Abstract
Background:
A rapid increase in restrictive abortion legislation in the United States has sparked renewed interest in self-managed abortion as a response to clinic access barriers. Yet little is known about knowledge of, interest in, and experiences of self-managed medication abortion among patients who obtain abortion care in a clinic.
Objective(s):
We examined patients’ knowledge of, interest in, and experience with self-managed medication abortion before presenting to the clinic. We characterized the clinic- and person-level factors associated with these measures. Finally, we examined the reasons why patients express an interest in or consider self-management before attending the clinic.
Study Design:
We surveyed 1,502 abortion patients at three Texas clinics in McAllen, San Antonio, and Fort Worth. All individuals seeking abortion care who could complete the survey in English or Spanish were invited to participate in an anonymous survey conducted using iPads. The overall response rate was 90%. We examined the prevalence of four outcome variables, both overall, and separately by site: 1) knowledge of self-managed medication abortion; 2) having considered self-managing using medications before attending the clinic; 3) interest in medication self-management as an alternative to accessing care at the clinic; and 4) having sought or tried any method of self-management before attending the clinic. We used binary logistic regression models to explore the clinic- and patient-level factors associated with these outcome variables. Finally, we analyzed the reasons reported by those who had considered medication self-management before attending the clinic, as well as the reasons reported by those who would be interested in medication self-management as an alternative to in-clinic care.
Results:
Among all respondents, 30% knew about abortion medications available outside the clinic setting (37% in Fort Worth, 33% in McAllen, 19% in San Antonio, p<0.001), and among those with prior knowledge, 28% had considered using this option before coming to the clinic (36% in McAllen, 25% in Fort Worth, 21% in San Antonio, p=0.028). Among those without prior knowledge of self-management, 39% expressed interest in this option instead of coming to the clinic (54% in San Antonio, 30% in McAllen, 29% in Fort Worth, p<0.001). Overall, 13% had sought out or tried any method of self-management before presenting to the clinic (16% in McAllen and 15% in Fort Worth vs. 9% in San Antonio, p<0.001). Experiencing barriers to clinic access was associated with having considered medication self-management (OR=2.2, 95% CI 1.7–3.0) and with seeking or trying any method of self-management before attending the clinic (OR=1.9, 95% CI 1.3–2.7). Difficulty affording the cost of in-clinic care was the most commonly cited reason for having considering medication self-management before attending the clinic. Reasons for interest in medication self-management as an alternative to clinic care included both access barriers and preferences for the privacy and comfort of home.
Conclusions:
Considering or attempting self-managed abortion may be part of the pathway to seeking in-clinic care, particularly among those experiencing access barriers. However, considerable interest in medication self-management as an alternative to the clinic also suggests demand for more autonomous abortion care options.
Keywords: Abortion, Medication abortion, Mifepristone, Misoprostol, Self-managed abortion, Texas
Condensation:
Abortion patients at three Texas clinics frequently considered or tried self-managed medication abortion before attending the clinic; those experiencing access barriers were more likely to do so.
Introduction
A rapid increase in restrictive abortion legislation in the United States has sparked renewed interest in self-managed abortion (i.e. abortion conducted outside the formal healthcare setting) as a response to clinic access barriers.1,2 At the same time, rising interest in self-care and the role of the internet as a go-to source of goods and services raises the possibility that some patients may prefer self-managed medication abortion over a traditional clinical service.3 Perhaps for these reasons, self-managed abortion is often presented as an alternative to in-clinic care.4,5 There is evidence, for example, that some women in Texas are foregoing clinic visits and self-managing their own abortions using misoprostol (with or without mifepristone) obtained online or from pharmacies in Mexico, or using non-medication methods such as botanicals or Vitamin C.6
However, it is also possible that considering or attempting self-managed abortion may be part of pathway to accessing care in the clinic setting rather than a mutually exclusive alternative. Little is known about the self-management experiences of those who ultimately do present to clinics. The few previous studies that have addressed self-managed abortion among clinic populations have focused on quantifying the lifetime prevalence of self-management. A 2014 study estimated that 1.2% of U.S. abortion-clinic patients had ever attempted to self-manage using misoprostol,7 while a 2000 study of Dominican women at three obstetrics-gynecology clinics in New York found that 5% reported misoprostol self-use.8 Another small study of 318 women at Texas abortion clinics found that 7% had previously attempted to induce an abortion by any means.9
In this paper, we address a different set of questions surrounding self-managed abortion. Drawing on a sample of 1,502 women from three clinics in Texas, we seek to characterize knowledge of, interest in, and experience with self-managed abortion among women who ultimately do obtain care in a clinic: What do women presenting at a clinic know about self-management, and how do they know it? Among those with prior knowledge of self-management, had they considered or attempted it before coming to the clinic—and if so, why? Among those without prior knowledge, what were their attitudes toward it? We also seek to examine whether these answers vary between different clinic settings, and whether they are associated with person-level attributes, such as race, ethnicity, or financial hardship. Understanding this variation provides a critical window on the landscape of self-managed abortion in the United States and provides insight into how providers might best respond to their patients’ needs, especially in a political climate where many states continue to pass restrictive abortion legislation.
Materials and Methods
Between January 2017 and March 2018, we conducted a survey of abortion patients at three clinics in Texas: Whole Woman’s Health of McAllen, San Antonio, and Fort Worth. Clinic sites were chosen for geographical spread and racial/ethnic diversity to allow comparisons between settings. Each clinic has a unique local context that could plausibly affect perspectives on self-management (e.g. proximity to the Texas-Mexico border), as well as a different patient mix in terms of key social and economic factors that may affect knowledge and experiences (e.g. the proportion of patients who are immigrants or people of color). Thus sampling from each site allows us to assess potential differences in knowledge of, experiences of, and interest in self-management both by clinic context and by patient-level factors. The process of accessing abortion care is similar across the three clinic sites in terms of cost, appointment scheduling, and state-mandated procedures including a required ultrasound, a 24-hour waiting period, and provision of counseling materials.
We aimed to survey 500 patients from each clinic (1,500 patients total), with sample sizes chosen to give 80% power to detect between-site differences in proportions of 5% for outcomes with 10% prevalence or less.
At each clinic, patient educators informed patients about the opportunity to participate in the study at the end of their education session. Patients were eligible for the survey if they were seeking abortion care at the clinic and could complete the survey in English or Spanish. Patients electing to participate gave their informed consent and completed the survey on iPads. We used REDCap software to program the consent form and survey. Data were submitted in real-time to UT-Austin’s REDCap server; no data were stored on the iPads. The survey was anonymous and completely separate from clinics’ patient records. No potentially identifying data were collected. Depending on their experiences with self-managed abortion, patients took between 5 and 12 minutes to complete the survey. No compensation was offered. Patient educators also used the iPads to record the number of patients who declined to participate. To optimally integrate the survey with clinic workflow, we first conducted a 3-week pilot phase at each clinic. The study received human-subjects approval from the UT-Austin Institutional Review Board.
The survey included a series of “yes-no” response questions assessing patients’ knowledge of self-managed medication abortion, their interest in medication self-management, and their experiences with self-management methods before coming to the clinic. Patients were first asked whether they had heard of pills that they could buy and use at home to conduct an abortion without going to a clinic or consulting a doctor. Those who answered “no” to this first question were asked whether they would be interested in using such pills to conduct their own abortion at home, whereas those who answered “yes” were asked: 1) whether they had considered using such pills before coming to the clinic; and 2) whether they had tried using such pills before coming to the clinic. All participants were then asked whether they had sought or tried any other ways of conducting their own abortion before coming to the clinic. Those indicating interest in medication self-management or who had considered it before coming to the clinic were also asked about their reasons why. Answer options included: the cost of clinical abortion care; difficulty making a clinic appointment due to work or school commitments; difficulty traveling to the clinic due to distance or lack of transport; the need to keep an abortion private; and preference for the home environment. (Answer options were devised based on a sample of free-text responses from participants in the pilot surveys). Participants could choose multiple reasons and could also respond through a free-text response. The free-text responses were reviewed by the study team and were included under the appropriate answer category. None of the responses required a new answer category to be devised. The survey also included a panel of demographic and clinical questions, including age, race/ethnicity, country of birth, number of children, receipt of government assistance programs (as a measure of financial hardship), knowledge of anyone else who had ever self-managed their own abortion, gestational age of the current pregnancy, and barriers encountered to accessing care at the clinic (see Supplemental Table 1 for details of each survey question). We compared patient demographic and clinical characteristics across sites using chi-squared tests.
We then analyzed several key proportions of interest, both in the overall sample and separately across sites:
How many patients had prior knowledge of abortion medications that could be purchased and used outside a clinic?
Among those with prior knowledge of these medications, how many had considered using them to self-manage their own abortions before presenting for in-clinic care?
Among those without prior knowledge, how many were interested in using these medications to self-manage their own abortion?
Regardless of prior knowledge, how many had sought or tried any method of self-management (medication or otherwise) before presenting to the clinic?
We compared these rates across clinics using chi-squared tests.
To explore the clinic- and patient-level factors associated with our self-management outcome variables, we fit four logistic regression models, one with each of the following four binary outcomes: 1) knowledge of medication self-management; 2) consideration of medication self-management before attending the clinic (among those with prior knowledge of medication self-management); 3) interest in medication self-management (among those without prior knowledge); and 4) having sought or tried any method of self-management before attending the clinic. Independent variables in each model included the full set of patient-level characteristics, as well as dummy variables for each clinic. To correct for multiple testing, we used the Benjamini-Hochberg procedure at a false discovery rate of 0.05.
Finally, we analyzed the reasons reported by those who had considered medication self-management before attending the clinic, as well as the reasons reported by those who would be interested in medication self-management as an alternative to in-clinic care. Each reported reason was analyzed by prevalence in the overall sample and separately by clinic site. We used Stata version 15 for all analyses.
Results
Overall, 1,502 patients participated in the survey (n=500 in McAllen, n=501 in San Antonio, and n=501 in Fort Worth). The participation rate across the three sites was 90% (1,502 of 1,661 patients approached). The vast majority of participants completed the entire survey in full; the proportion of missing data for each variable is shown in the footnotes to Tables 1 and 2.
Table 1:
Characteristics of Abortion Patients who Participated in the Clinic Survey, Overall and by Clinic Site
| Characteristic | Full Sample Frequency (%) (N=1,502) | McAllen Frequency (%) (n= 500) | San Antonio Frequency (%) (n= 501) | Fort Worth Frequency (%) (n= 501) | P value for clinic differences |
|---|---|---|---|---|---|
| Age | |||||
| Under 20 | 160 (11.1) | 55 (11.4) | 50 (10.7) | 55 (11.1) | 0.088 |
| 20–24 | 458 (31.7) | 174 (36.1) | 148 (31.7) | 136 (27.5) | |
| 25–29 | 450 (31.2) | 134 (27.8) | 158 (33.8) | 158 (31.9) | |
| 30–34 | 236 (16.3) | 72 (14.9) | 75 (16.1) | 89 (18.0) | |
| 35+ | 140 (9.7) | 47 (9.8) | 36 (7.7) | 57 (11.5) | |
| Gestational age | |||||
| Under 10 weeks | 1161 (80.6) | 416 (86.3) | 379 (81.2) | 366 (74.4) | <0.001 |
| 10 – 16 weeks | 258 (17.9) | 62 (12.9) | 78 (16.7) | 118 (24.0) | |
| Over 16 weeks | 22 (1.5) | 4 (0.8) | 10 (2.1) | 8 (1.6) | |
| Race/Ethnicity | |||||
| Black | 188 (13.1) | 1 (0.2) | 43 (9.2) | 144 (29.4) | <0.001 |
| US-Born Hispanic | 768 (53.6) | 362 (75.9) | 278 (59.7) | 128 (26.1) | |
| Foreign-born Hispanic | 138 (9.6) | 80 (16.8) | 27 (5.8) | 31 (6.3) | |
| Non-Hispanic white | 271 (18.9) | 29 (6.1) | 97 (20.8) | 145 (29.6) | |
| Other | 68 (4.8) | 5 (1.1) | 21 (4.5) | 42 (8.6) | |
| No of children | |||||
| 1 or more | 971 (67.3) | 316 (65.7) | 308 (66.0) | 347 (70.2) | 0.236 |
| 0 | 471 (32.7) | 165 (34.3) | 159 (34.0) | 147 (29.8) | |
| Financial hardship | |||||
| Yes | 698 (49.8) | 252 (53.7) | 233 (50.9) | 213 (44.7) | 0.019 |
| No | 705 (50.3) | 217 (46.3) | 225 (49.1) | 263 (55.3) | |
| Barriers accessing clinical care | |||||
| Yes | 530 (41.0) | 141 (44.2) | 194 (40.2) | 195 (39.7) | 0.401 |
| No | 763 (59.0) | 178 (55.8) | 289 (59.8) | 296 (60.3) | |
| Knows somebody who self-managed† | |||||
| Yes | 164 (39.0) | 71 (45.2) | 25 (27.5) | 68 (39.3) | 0.022 |
| No | 257 (61.0) | 86 (54.8) | 66 (72.5) | 105 (60.7) | |
Asked only to those with knowledge of medication self-management (N=442)
P-values are against the null hypothesis of independence of each measure across clinics. Missing data are as follows: Age: n=58 (3.9% of the sample); Gestational age: 61 (4.1%); Race/ethnicity: 69 (4.6%); No. of children: 60 (4.0%); Government assistance: 99 (6.6%); Barriers accessing clinical care: 209 (13.9%), This question was added to the survey following the short pilot phase; Knows somebody who self-managed: 21 (4.8%).
Table 2:
Clinic Survey Outcome Measures Overall and by Clinic Site
| Outcome | Full Sample Frequency (%) (N=1,502) | McAllen Frequency (%) (n= 502) | San Antonio Frequency (%) (n= 501) | Fort Worth Frequency (%) (n= 501) | P value for clinic differences |
|---|---|---|---|---|---|
| Knowledge of medication self-management | |||||
| Yes | 442 (29.5) | 163 (32.6) | 96 (19.2) | 183 (36.6) | <0.001 |
| No | 1057 (70.5) | 337 (67.4) | 403 (80.8) | 317 (63.4) | |
| Considered medication self-management† | |||||
| Yes | 121 (28.3) | 57 (35.6) | 20 (21.7) | 44 (25.0) | 0.028 |
| No | 307 (71.7) | 103 (64.4) | 72 (78.3) | 132 (75.0) | |
| Interested in medication self-management* | |||||
| Yes | 407 (38.7) | 102 (30.3) | 215 (53.5) | 90 (28.7) | <0.001 |
| No | 646 (61.3) | 235 (69.7) | 187 (46.5) | 224 (71.3) | |
| Sought or tried any method of self-management | |||||
| Yes | 195 (13.3) | 80 (16.2) | 41 (8.5) | 74 (15.0) | 0.001 |
| No | 1274 (86.7) | 414 (83.8) | 441 (91.5) | 419 (85.0) | |
Includes only those with knowledge of medication self-management (N=442)
Includes only those without knowledge of medication self-management (N=1057)
P-values are against the null hypothesis of independence of each measure across clinics. Missing data are as follows: Knowledge of medication of self-management: n=3 (0.2% of the sample); Considered medication self-management: n=14 (3.2%); Interested in medication self-management: n=4 (0.4% of the sample); Sought/tried any method of self-management: n=33 (2.2%).
Table 1 shows participant characteristics for the full sample and separately by site. The age distribution of the overall sample is diverse, with the majority (63%) falling between 20 and 29 years, and with no significant age differences across sites. Overall, the majority of participants (81%) were under 10 weeks’ gestation at the time of their abortions, but the proportion presenting between 10 and 16 weeks differed by site (p<0.001): 24% in Fort Worth, versus 13% and 17% in McAllen and San Antonio. The sample was racially and ethnically diverse, with significant differences by site (p<0.001): Fort Worth had the highest proportion of Black participants (29%), and McAllen had the highest proportion of US-born Hispanic participants (76%). Most respondents had at least one child. Half of the overall sample lived in financial hardship, with moderate differences by site (p=0.019): McAllen had the highest proportion (54%), Fort Worth the lowest (45%). Overall, 41% of participants encountered at least one barrier to accessing abortion care in the clinic setting, with no significant differences across sites. Thirty-nine percent of those with prior knowledge of medication self-management knew someone else who had previously self-managed, with significant differences across sites (45% in McAllen vs. 28% in San Antonio and 39% in Fort Worth, p=0.022).
Table 2 shows our primary outcomes, both for the full sample and separately by site. Overall, 30% of participants had prior knowledge of medications they could obtain and use to self-manage an abortion outside a clinic. Knowledge varied by clinic site (37% in Fort Worth, 33% in McAllen, 19% in San Antonio, p<0.001). Patients’ knowledge of the potential source of these medications also varied by site. In McAllen, patients with prior knowledge of medication self-management most commonly reported Cytotec as the name of the medication they had heard of (49%), and a large majority (69%) knew they could obtain such medications from a pharmacy in Mexico. By contrast, in Fort Worth, the most commonly known-about medication was misoprostol (59%); a substantial minority (37%) reported a shop or mall where they could buy the medications, while 26% knew about an online source. In San Antonio, most patients with prior knowledge did not know the specific name of the medication they had heard of or where they could obtain it (52%). Among those with prior knowledge of medication self-management, 28% had considered this option before coming to the clinic, with differences by site (p=0.028): 36% in McAllen vs. 25% in Fort Worth and 21% in San Antonio. Among those without prior knowledge of self-management, 39% expressed interest in this option instead of coming to the clinic, again with differences by site (54% in San Antonio, 30% in McAllen, 29% in Fort Worth, p<0.001).
Overall, 1 in 7 women (13%) in our sample had sought out or tried any method of self-management before presenting to the clinic. Significant differences were observed by site (16% in McAllen and 15% in Fort Worth vs. 9% in San Antonio, p<0.001). Among those who sought or attempted self-management before presenting to the clinic, 50% reported seeking or trying abortion medications, 38% reported seeking or trying any other method, and 12% reported seeking or trying both abortion medications and other methods. Among the other methods reported included herbal and homeopathic methods (such as cohosh and Vitamin C), non-abortion medications (such as ibuprofen), and physical methods (such as starvation, intense exercise or trauma to the abdomen).
Table 3 summarizes the results from our four logistic-regression models. The first model shows the factors that predict a patient’s prior knowledge of self-managed medication abortion. Patients in McAllen (OR=1.9) and Fort Worth (OR=2.7) were more likely to report prior knowledge, versus patients in San Antonio (p<0.001). At the patient level, living in financial hardship was also associated with knowledge of medication self-management (OR=1.5, p=0.003).
Table 3:
Factors Associated with Women’s Knowledge, Consideration and Interest in Self-Management Abortion
| Knowledge of self-managed medication abortion (n=1,214) | Considered self-managed medication abortion before attending the clinic (n=326) | Interest in self-managed medication abortion among those without prior knowledge (n=870) | Sought or tried any method of self-management prior to attending the clinic (n=1,183) | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Clinic | ||||||||
| San Antonio | ref | -- | ref | -- | ref | -- | ref | -- |
| McAllen | 1.85 | 1.30 – 2.64* | 1.82 | 0.86 – 3.86 | 0.38 | 0.26 – 0.56* | 1.90 | 1.16 – 3.12 |
| Fort Worth | 2.68 | 1.93 – 3.73* | 1.20 | 0.59 – 2.47 | 0.30 | 0.21 – 0.44* | 1.42 | 0.88 – 2.30 |
| Age | ||||||||
| 20–24 | ref | -- | ref | -- | ref | -- | ref | -- |
| Under 20 | 0.73 | 0.46 – 1.18 | 0.55 | 0.18 – 1.65 | 0.66 | 0.38 – 1.15 | 0.74 | 0.37 – 1.49 |
| 25–29 | 1.14 | 0.81 – 1.60 | 1.56 | 0.78 – 3.11 | 1.42 | 0.97 – 2.08 | 1.20 | 0.74 – 1.93 |
| 30–34 | 1.06 | 0.70 – 1.62 | 1.39 | 0.57 – 3.37 | 1.94 | 1.22 – 3.08 | 1.42 | 0.80 – 2.54 |
| 35 and Over | 1.35 | 0.84 – 2.17 | 1.45 | 0.55 – 3.82 | 1.68 | 0.96 – 2.95 | 1.20 | 0.61 – 2.38 |
| Gestational age | ||||||||
| Less than 10 weeks | ref | -- | ref | -- | ref | -- | ref | -- |
| 10–16 weeks | 1.15 | 0.83 – 1.60 | 1.17 | 0.60 – 2.26 | 0.83 | 0.56 – 1.24 | 1.11 | 0.70 – 1.76 |
| Over 16 weeks | 1.02 | 0.36 – 2.92 | 0.88 | 0.12 – 6.76 | 0.90 | 0.30 – 2.68 | 0.84 | 0.22 – 3.22 |
| Race/ethnicity | ||||||||
| Non-Hispanic white | ref | -- | ref | -- | ref | -- | ref | -- |
| Black | 1.10 | 0.70 – 1.73 | 1.15 | 0.43 – 3.07 | 0.61 | 0.37 – 1.03 | 0.72 | 0.37 – 1.41 |
| US-born Hispanic | 1.46 | 0.99 – 2.13 | 1.23 | 0.55 – 2.75 | 0.58 | 0.39 – 0.87* | 0.84 | 0.50 – 1.42 |
| Foreign-born Hispanic | 1.27 | 0.73 – 2.23 | 1.72 | 0.54 – 5.51 | 0.49 | 0.26 – 0.93 | 0.78 | 0.36 – 1.69 |
| Other | 1.59 | 0.87 – 2.90 | 0.22 | 0.04 – 1.15 | 0.98 | 0.48 – 2.02 | 0.73 | 0.30 – 1.78 |
| Children | ||||||||
| 0 | ref | -- | ref | -- | ref | -- | ref | -- |
| 1 or more | 0.67 | 0.47 – 0.94 | 0.88 | 0.43 – 1.83 | 0.64 | 0.43 – 0.94 | 0.72 | 0.44 – 1.18 |
| Financial hardship | ||||||||
| No | ref | -- | ref | -- | ref | -- | ref | -- |
| Yes | 1.54 | 1.16 – 2.05* | 0.84 | 0.45 – 1.57 | 1.11 | 0.80 – 1.53 | 1.38 | 0.92 – 2.09 |
| Clinic access barriers | ||||||||
| No | ref | -- | ref | -- | ref | -- | ref | -- |
| Yes | 1.07 | 0.82 – 1.39 | 2.18 | 1.25 – 3.78 | 2.22 | 1.65 – 2.99* | 1.87 | 1.30 – 2.71* |
| Knows somebody who self-managed | ||||||||
| No | -- | -- | ref | -- | -- | -- | ref | -- |
| Yes | -- | -- | 4.10 | 2.36 – 7.12* | -- | -- | 4.94 | 3.35 – 7.28* |
Denotes a statistically significant odds ratio at the 0.05 level after multiplicity correction.
An odds ratio greater than 1 indicates that there is a higher chance of a “yes” outcome in each model (e.g. knowledge of self-management) when a given factor (e.g. financial hardship) is present. An odds ratio less than 1 indicates a higher chance of a “no” outcome when that factor is present
The second model shows the factors associated with having considered self-managing using medications before presenting to the clinic, among those with prior knowledge of medication self-management. Here we found no significant differences by clinic location, holding patient characteristics constant. At the patient level, we found strong associations with experiencing barriers to clinic access (OR=2.2, p<0.001) and with knowing someone who had previously self-managed (OR=4.1, p<0.001).
The third model shows the factors associated with interest in medication self-management as an alternative to in-clinic care, among those without prior knowledge of medication self-management. Patients in McAllen (OR=0.4) and Fort Worth (OR=0.3) were less likely to be interested in this option versus those in San Antonio (p<0.001), holding patient characteristics constant. U.S.-born Hispanics were less likely to express interest in medication self-management versus non-Hispanic whites (OR=0.6, p=0.007), while those who experienced clinic access barriers were more likely to express interest (OR=2.2, P<0.001).
The fourth model shows the factors associated with seeking or trying any method of self-management before attending the clinic. Here, we found no significant differences by clinic location, holding patient characteristics constant. At the patient level we found associations with experiencing barriers to clinic access (OR=1.9, p<0.001) and with knowing someone who had previously self-managed (OR=4.9, p<0.001).
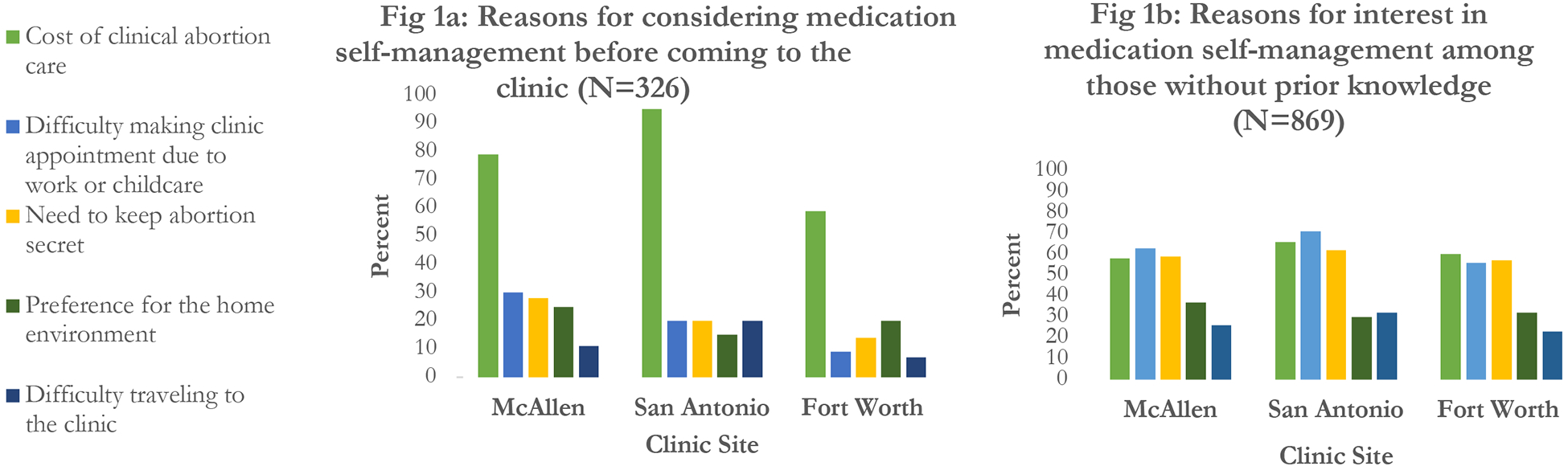
Figure 1a displays the reasons why those with prior knowledge of medication self-management had considered using it before coming to the clinic. The predominant reason at all sites was the cost of in-clinic care. Figure 1b displays the reasons why those without prior knowledge would be interested in using medication self-management instead of obtaining care at the clinic. While the cost of care is still a prominent factor, difficulty making it to a clinic appointment due to work or childcare were the most commonly cited reasons in McAllen and San Antonio. The need to keep the abortion secret, a preference for the home environment, and difficulty traveling to the clinic due to distance or lack of transport were also frequently cited reasons.
Figure 1: Reasons for considering or expressing interest in self-managed medication abortion prior to attending the clinic.
Comment
Principal Findings
Knowledge of self-managed medication abortion is high among patients presenting for abortion care at three Texas clinics, and is higher at the clinics in McAllen and Fort Worth versus the clinic in San Antonio. Almost a third of patients with prior knowledge of medication self-management had considered this option before coming to the clinic. Prior consideration of self-management was strongly associated with experiencing barriers to clinic access, particularly the cost of in-clinic care. Among those without such prior knowledge, we found considerable interest in this option as an alternative to in-clinic care, particularly among those who had experienced access barriers. However, the reasons underlying this interest were varied, including difficulty accessing in-clinic care and a preference for the home environment. Overall, almost 1 in 7 patients presenting for care had sought or tried any method of self-management before presenting to the clinic. Doing so was strongly associated with experiencing barriers to clinic access and knowing someone else who previously self-managed an abortion.
Results
Our findings extend prior work on self-management focused on clinic populations5–7 by providing detailed insight into what patients at three Texas abortion clinics knew about self-managed medication abortion, as well as how often and why they had considered or expressed interest in self-management. Patients’ reasons involve a combination of clinic-access barriers and preference for the home environment, echoing findings from a small number of prior qualitative studies that have examined US residents’ motivations for seeking self-managed medication abortion.6, 10–11
Clinical Implications
The association between clinic access barriers and having considered or tried medication self-management is particularly significant in light of recent legislation that has restricted access to abortion clinics in Texas.12 Enacted restrictions include a mandatory 24-hour waiting period and separate appointment for an ultrasound prior to an abortion.13 Some restrictions, such as requiring abortion clinics to conform to the building standards of ambulatory surgical centers, were ultimately overturned. But not before half of all abortion clinics in Texas closed because they were unable to make such costly adjustments. As a result, the remaining clinics are concentrated in urban areas, meaning that for some the nearest clinic is hundreds of miles away.14 Researchers have suggested that the recent decline in the in-clinic abortion rate may be partly due to a rise in self-management.2 In addition, our findings suggest that self-management may also be part of the pathway to in-clinic care: some patients who had initially considered self-management may have barely managed to make it to the clinic because of last-minute help from an abortion fund or family member, or they have come only because they were unable to find an acceptable way to self-manage. Others who did try a method of self-management may have presented to the clinic because the attempt did not work. As many states, including Texas, continue to enact barriers to in-clinic care, our findings raise important questions for policymakers about the impacts of such legislation, particularly on those who are most affected by additional restrictions because they have the fewest resources.
The high level of interest in medication self-management observed in our study also raises questions about how providers can meet the needs of patients who might prefer a more autonomous model of abortion care. Clinic-based telemedicine models (where consultations are done by video/phone, with the patient picking up medication from a pharmacy) may help patients overcome barriers and/or fulfil their preferences.15,16 Additionally, given the proportion of patients who had considered or tried to self-manage before coming to the clinic, providers should be prepared to receive and answer requests for information or assistance.
Research Implications
The variation in knowledge of and interest in medication self-management across our three sites, even within a single state, suggests that the landscape of self-managed abortion might vary considerably among U.S. clinic populations. Future research should examine this variation, with a view to generating insights that could help meet the needs of those who might consider or try self-management. Such a response may be particularly important should upcoming legal challenges to Roe v. Wade create an environment where in-clinic care is no longer available in some states. Interestingly, the strong association we found between knowing someone else who has self-managed and having personally considered or tried self-management suggests that the experiences patients hear from others tend to be positive. This finding raises questions about how patients first hear about self-management and what information and advice they might access through social networks.
Strengths and Limitations
Data in this study are self-reported; it is possible that some patients were not comfortable disclosing their interest in or experience with self-managed abortion. But the stigma of answering questions about abortion was likely reduced by conducting the survey at abortion clinics. Self-managed abortion may be a sensitive topic due to possible legal risks,17 but questions designed to ask about interest in and perspectives on self-management may lead to more accurate responses than simply focusing on direct questions about self-management attempts. Results are not generalizable beyond our three sites, but our aim was to specifically examine site- and person-level variation in our primary outcomes, rather than to draw conclusions generalizable to all Texas abortion patients.
Conclusions
Considering or attempting self-managed abortion may be part of the pathway to seeking in-clinic care, particularly among those experiencing access barriers. The most prominent access barriers cited by patients were cost and difficulty taking time away from work, school, and childcare commitments. Policy-makers should therefore consider the potential consequences of further restricting in-clinic abortion access, particularly for those with the fewest resources. At the same time, the considerable interest we observed in medication self-management as an alternative to the clinic could be fulfilled by the development of more autonomous abortion care options, such as telemedicine or pharmacy-based programs.
Supplementary Material
AJOG at a Glance.
A. Why was this study conducted?
To measure knowledge of, interest in, and experiences with self-managed medication abortion among patients attending abortion clinics.
B. What are the key findings?
30% of patients at three Texas clinics had prior knowledge of medications that could be used to self-manage an abortion. Among these, 28% had considered medication self-management before attending the clinic.
13% of patients sought or attempted any method of self-management before attending the clinic.
Those experiencing clinic-access barriers were more likely to have considered or attempted self-management.
Among patients without prior knowledge of medication self-management, 39% expressed interest in this option as an alternative to in-clinic care.
C. What does this study add to what is already known?
Considering or attempting self-managed abortion may be part of the pathway to seeking in clinic care, particularly among those experiencing access barriers. Moreover, considerable interest in medication self-management suggests demand for more autonomous abortion care options.
Acknowledgments
The authors are grateful for the dedication of the staff at Whole Woman’s Health McAllen, San Antonio, and Fort Worth in facilitating data collection, as well as the leadership of Whole Woman’s Health for their partnership on the study.
Financial Support
This study was supported by funding from a Junior Investigator grant from the Society of Family Planning (SFPRF10-JI2). The study was also supported in part by infrastructure grant P2CHD042849 and training grant 5 T32 LM012414-03 awarded to The University of Texas at Austin by the National Institutes of Health. None of the funders had any role in the study design, data collection, data analysis, interpretation of data, the writing of the report or the decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Society of Family Planning.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure statement
The authors report no conflict of interest.
Presentation Information
Preliminary findings were presented at the 2018 North American Forum on Family Planning, New Orleans, LA, October 20th–22nd 2018.
Contributor Information
Abigail R.A. AIKEN, LBJ School of Public Affairs, University of Texas at Austin, Austin, TX, USA.
Ms. Kathleen BROUSSARD, Population Research Center, University of Texas at Austin, Austin, TX, USA.
Ms. Dana M. JOHNSON, LBJ School of Public Affairs, University of Texas at Austin, Austin, TX, USA.
Ms. Elisa PADRON, College of Natural Sciences, University of Texas at Austin, Austin, TX, USA.
Ms. Jennifer E. STARLING, Department of Statistics and Data Science, University of Texas at Austin, Austin, TX, USA.
James G. SCOTT, Department of Statistics and Data Science, University of Texas at Austin, Austin, TX, USA.
References
- 1.The Guttmacher Institute. State Facts About Abortion: Guttmacher Institute Fact Sheet. May 2018. https://www.guttmacher.org/fact-sheet/state-facts-about-abortion-texas. Accessed July 15th 2019.
- 2.Foster Diana Greene. Dramatic Decreases in US Abortion Rates: Public Health Achievement or Failure?. AJPH 2017:1860–1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jerman J, Onda T, Jones RK. What are people looking for when they Google “self-abortion”?. Contraception. 2018:97(6);510–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grossman D, Ralph L, Raifman S et al. Lifetime prevalence of self-induced abortion among a nationally representative sample of US women. Contraception. 2018;97(5):460. [Google Scholar]
- 5.Grossman D, Hendrick E, Fuentes L et al. Knowledge, opinion and experience related to abortion self-induction in Texas. Contraception. 2015:92(4);360–1. [Google Scholar]
- 6.Texas Policy Evaluation Project. Research Brief. Texas women’s experiences attempting self-induced abortion in the face of dwindling options 2015. https://liberalarts.utexas.edu/txpep/_files/pdf/TxPEP-Research-Brief-WomensExperiences.pdf Accessed July 15th 2019.
- 7.Jerman J, Jones RK, Onda T. Characteristics of US abortion patients in 2014 and changes since 2008. Guttmacher Institute. 2016:1–27. https://www.guttmacher.org/report/characteristics-us-abortion-patients-2014 Accessed July 15th 2019. [Google Scholar]
- 8.Rosing MA, Archbald CD. The knowledge, acceptability, and use of misoprostol for self-induced medical abortion in an urban US population. J Am Med Womens Assoc. 2000;55(3 Suppl):183–5. [PubMed] [Google Scholar]
- 9.Grossman D, White K, Hopkins K, Potter JE. The public health threat of anti-abortion legislation. Contraception. 2014:89(2);73–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aiken AR, Broussard K, Johnson DM, Padron E. Motivations and experiences of people seeking medication abortion online in the United States. Perspect Sex Reprod Health. 2018; 50(4):157–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grossman D, Holt K, Peña M et al. Self-induction of abortion among women in the United States. Reprod Health Matters. 2010;18(36):136–46. [DOI] [PubMed] [Google Scholar]
- 12.Fuentes L, Lebenkoff S, White K et al. Women’s experiences seeking abortion care shortly after the closure of clinics due to a restrictive law in Texas. Contraception. 2016:93(4);292–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guttmacher Institute. State Facts About Abortion: Texas. September 2019. https://www.guttmacher.org/fact-sheet/state-facts-about-abortion-texas (Accessed November 14th 2019).
- 14.Hasstedt K. The State of Sexual and Reproductive Health and Rights In the State of Texas: A Cautionary Tale. Guttmacher Policy Review. 2014:17(2). [Google Scholar]
- 15.Grossman D, Grindlay K, Buchacker T, Lane K, Blanchard K. Effectiveness and acceptability of medical abortion provided through telemedicine. Obstetrics & Gynecology. 2011;118(2):296–303. [DOI] [PubMed] [Google Scholar]
- 16.Biggs MA, Ralph L, Raifman S, Foster DG, Grossman D. Support for and interest in alternative models of medication abortion provision among a national probability sample of US women. Contraception. 2019. February 1;99(2):118–24. [DOI] [PubMed] [Google Scholar]
- 17.Diaz-Tello F, Mikesell M, Adams JE. Roe’s unfinished promise: decriminalizing abortion once and for all. 2017. Available at SSRN: https://ssrn.com/abstract=3082643. Accessed July 15th 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


