INTRODUCTION
The spread of the novel coronavirus has had a significant global effect. However, not all communities have been affected equally: U.S. reports have demonstrated racial and ethnic inequities in coronavirus disease 2019 (COVID-19)–related hospitalizations and deaths. Such inequities are commonplace in maternal mortality and severe maternal morbidity.1–5 We sought to examine possible ethnic inequities of the COVID-19 pandemic among pregnant patients at our institution.
METHODS
This is a prospective cohort study of women at a single academic medical center who reported symptoms of COVID-19 infection while pregnant or within 2 weeks postpartum from March 6 to May 4, 2020, a timeframe that included the peak regional COVID-19 infection incidence.6 Women were tested for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, reverse transcriptase-polymerase chain reaction 53 nasopharyngeal swab) based on symptoms and, additionally, epidemiologic factors, because we had insufficient testing capacity to test all symptomatic women. This study was approved by the Partners Healthcare Human Research Committee. We compared characteristics among women with confirmed COVID-19 infection by self-reported ethnicity (Hispanic or non-Hispanic).7 For women testing positive, we compared disease severity by ethnicity (without statistical testing owing to small sample sizes). We used χ2 or Fisher exact test for categorical variables and Wilcoxon rank-sum test for continuous variables. P<.05 was considered significant.
RESULTS
During the study, 65 Hispanic and 127 non-Hispanic women presented with symptoms of COVID-19 infection. One hundred thirty-six (71%) were tested; 39 of 54 Hispanic women (72%) and 22 of 82 non-Hispanic women (27%) had positive test results (P<.001). There were differences in baseline characteristics by ethnicity for women who were symptomatic and those with confirmed COVID-19 infection (Table 1). Of those testing positive, 13 of 39 Hispanic women were admitted to the hospital: five to the intensive care unit, of whom four were intubated. Eight of 22 non-Hispanic women were admitted: one to the intensive care unit but without undergoing intubation. There were no deaths.
Table 1.
Comparison of Maternal Characteristics by Ethnicity Among Women Reporting Symptoms and Those With Confirmed Cases of Coronavirus Disease 2019 (COVID-19) Infection
| Characteristic | Symptomatic Women | Confirmed Cases | ||||
|---|---|---|---|---|---|---|
| Hispanic (n=65) | Non-Hispanic* (n=127) | P | Hispanic (n=39) | Non-Hispanic* (n=22) | P | |
| Age (y) | 30 (26.0–34.7) | 34 (30.6–36.9) | <.001 | 29 (25.2–35.3) | 35 (30.1–38.9) | .02 |
| Parity | 1.0 (1.0–2.0) | 1.0 (0.0–1.0) | .001 | 2.0 (1.0–2.0) | 0.0 (0.0–1.0) | <.001 |
| Onset of symptoms | ||||||
| Gestational age (wk) | 24 (14.6–28.4) | 20 (12.1–28.3) | .15 | 24 (14.1–28.4) | 24 (20.1–29.7) | .74 |
| Postpartum | 12 (19) | 24 (19) | 1.00 | 9 (23) | 4 (18) | .54 |
| Primary language | ||||||
| English | 26 (40) | 121 (95) | <.001 | 10 (26) | 20 (91) | <.001 |
| Non-English | 39 (60) | 0 (0) | 29 (74) | 0 (0) | ||
| Unknown | 0 (0.0) | 6 (5) | 0 (0) | 2 (9) | ||
| Primary insurer | ||||||
| Public | 48 (74) | 18 (14) | <.001 | 31 (79) | 5 (23) | <.001 |
| Private | 15 (23) | 105 (83) | 6 (15) | 16 (73) | ||
| Uninsured | 0 (0.0) | 2 (2) | 0 (0) | 1 (5) | ||
| Unknown | 2 (3) | 2 (2) | 2 (5) | 0 (0) | ||
| Median income of ZIP code ($1,000) | 52 (49.6–55.2) | 80 (55.2–90.7) | <.001 | 51 (49.6–52.4) | 64 (49.6–79.6) | .02 |
| Comorbidities | ||||||
| Obesity | 25 (39) | 32 (25) | .09 | 17 (44) | 9 (41) | .79 |
| Diabetes | 7 (11) | 7 (6) | .17 | 4 (10) | 1 (5) | .65 |
| Asthma | 6 (9) | 29 (23) | .03 | 2 (5) | 4 (18) | .75 |
| Tested | 54 (83) | 82 (65) | .008 | |||
Data are median (interquartile range) or n (%) unless otherwise specified.
The non-Hispanic group includes white, black, and Asian women and women of other races.
DISCUSSION
Our initial experience with COVID-19 infection in pregnancy has identified inequities between Hispanic and non-Hispanic pregnant women in the catchment area of our obstetric service. Although Hispanic women represent just 18% of this population, they accounted for more than 60% of all pregnant women hospitalized for COVID-19 infection to date. Furthermore, after initiation of statewide distancing guidance, the rate of infections among non-Hispanic pregnant women at our institution plateaued whereas the incidence among Hispanic pregnant women continued to rise (Fig. 1).
Fig. 1.
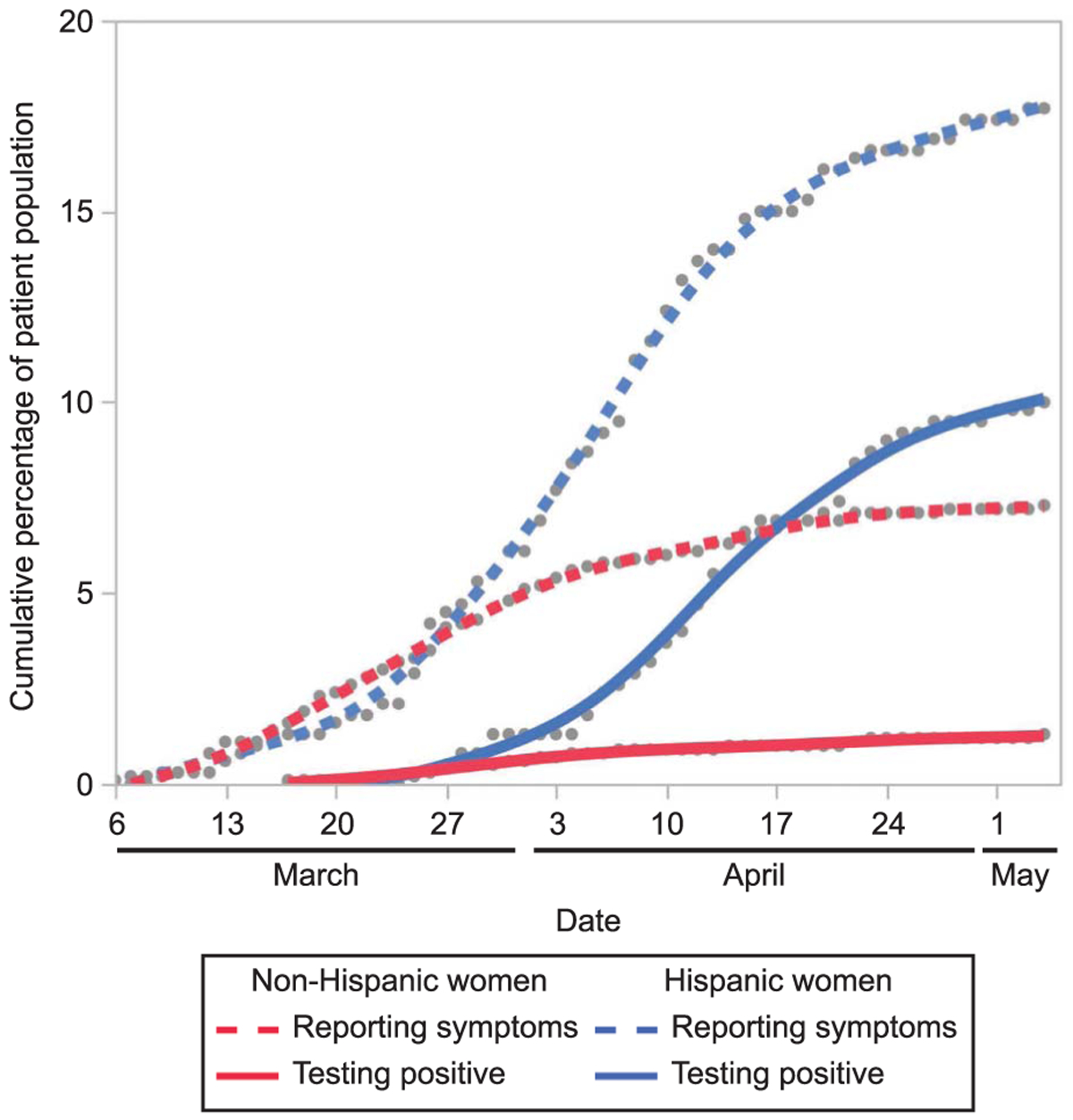
Cumulative percentage of women reporting symptoms and testing positive for coronavirus disease 2019 (COVID-19) infection among the pregnant patient population. Red and blue lines (solid and dashed) are smoothed lines to fit the points.
Goldfarb. Ethnic Inequities in COVID-19 Prevalence and Severity. Obstet Gynecol 2020.
Mitigation strategies for COVID-19 infection have relied heavily on individuals’ adherence to physical distancing guidance; however, many families in diverse urban communities live in multigenerational or multi-family homes, with family members working in essential, low-wage jobs. Language barriers, jobs without sick pay or insurance, and fear of immigration officials may keep individuals from necessary screening and medical attention, which may allow further spread of disease within their homes and communities.
As a limitation of this analysis, we recognize the contribution of evolving access to COVID-19 testing over the study period in our institution. However, the incidence of Hispanic women reporting symptoms also rose during the study period, suggesting that access to testing is unlikely the sole explanation for the observed differences. Given small numbers, we were unable to control for multiple variables, including underlying comorbidities that have been reported to worsen outcomes.
Without detailed demographic information, aggregated data at institutional or regional levels may present an overly optimistic view that the COVID-19 infection curve has been flattened for all populations. This study suggests otherwise and demonstrates an urgent need for tailored approaches to slow the spread among vulnerable groups.
Acknowledgments
The authors thank Michala Sawyer, B.S., Massachusetts General Hospital Department of Obstetrics and Gynecology, Boston, Massachusetts, for her contribution to database creation and data abstraction. She is a paid clinical research coordinator in the Department of Obstetrics and Gynecology.
Ilona Goldfarb, MD, MPH, and Mark Clapp, MD, MPH, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Each author has confirmed compliance with the journal’s requirements for authorship.
Footnotes
Financial Disclosure
Allison S. Bryant reports money paid to her institution: NIH: 2020 The Fourth Trimester: A Web-Based Tool for Postpartum Care to Address the Needs of Underserved Women 1 R43 MD014923–01 (Merz/Marceau) SBIR, National Institute on Minority Health and Health Disparities 2014–2019 Effect of a patient-centered decision app on TOLAC: An RCT 1 R01 HD078748–01 (Kuppermann) Co-Investigator Direct cost: $487,512. Description: This is a randomized controlled trial of a patient-centered decision app on decision-making among women with prior cesarean deliveries who are considering mode of delivery in their current pregnancies. Money was paid to her for expert witness testimony from ACOG, SMFM, PNQIN, ILPQC, UCSF, CDC, and Pennsylvania Hospital. The other authors did not report any potential conflicts of interest.
REFERENCES
- 1.Garg S, Kim L, Whitaker M, O’Halloran A, Cummings C, Holstein R, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 states, March 1–30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:458–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cook County Government. Open data: medical examiner case archive. Available at: https://datacatalog.cookcountyil.gov/Public-Safety/Medical-Examiner-Case-Archive/cjeq-bs86/data. Retrieved April 20, 2020.
- 3.Louisiana Department of Health. COVID-19. Available at: http://ldh.la.gov/Coronavirus/. Retrieved April 20, 2020.
- 4.Holdt Somer SJ, Sinkey RG, Bryant AS. Epidemiology of racial/ethnic disparities in severe maternal morbidity and mortality. Semin Perinatol 2017;41:258–65. [DOI] [PubMed] [Google Scholar]
- 5.Howell EA, Brown H, Brumley J, Bryant AS, Caughey AB, Cornell AM, et al. Reduction of peripartum racial and ethnic disparities: a conceptual framework and maternal safety consensus bundle [published erratum appears in Obstet Gynecol 2019; 133:1287]. Obstet Gynecol 2018;131:770–82. [DOI] [PubMed] [Google Scholar]
- 6.Mass.gov. COVID-19 response reporting. Available at: https://www.mass.gov/info-details/covid-19-response-reporting. Retrieved May 17, 2020.
- 7.United States Census Bureau. Table DP03. Selected economic characteristics. Available at: https://data.census.gov/cedsci/table?q5sammamish%20median%20income&lastDisplayedRow516&table5DP03&tid5ACSDP1Y2018.DP03&t5Income%20and%20Earnings&g51600000US5361115.


