Routine gastrointestinal (GI) endoscopy has been on hold. This pause was necessary while health care resources were concentrated on the coronavirus disease 2019 (COVID-19) pandemic and our patients sheltered at home. Unfortunately, COVID-19 will likely persist for months, if not years, in our communities. Although the decision to resume routine GI endoscopy will depend on the availability of resources, local trends in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, and state and federal regulations, our units will eventually need to reopen for routine endoscopy to provide appropriate care to our patients.
Clearly, gastroenterologists will need to modify their practice to reduce the risk of COVID-19 infection for their patients, their staff, and themselves. There is no treatment for SARS-CoV-2, and we are unlikely to have a widely available vaccine until 2021 at the earliest. Vaccine development is expected to be challenging (1), and there are concerns that any vaccine may not be as effective as we would hope, particularly in older adults. For now, COVID-19 is widespread in most communities and there is good evidence that asymptomatic carriers can disseminate the virus (2–4). Below, we outline key logistical and operational issues to a safe and orderly reopening of outpatient endoscopy facilities, with a focus on treating the COVID-19 pandemic as an ongoing health issue in our communities (Figure 1) (5).
Figure 1.
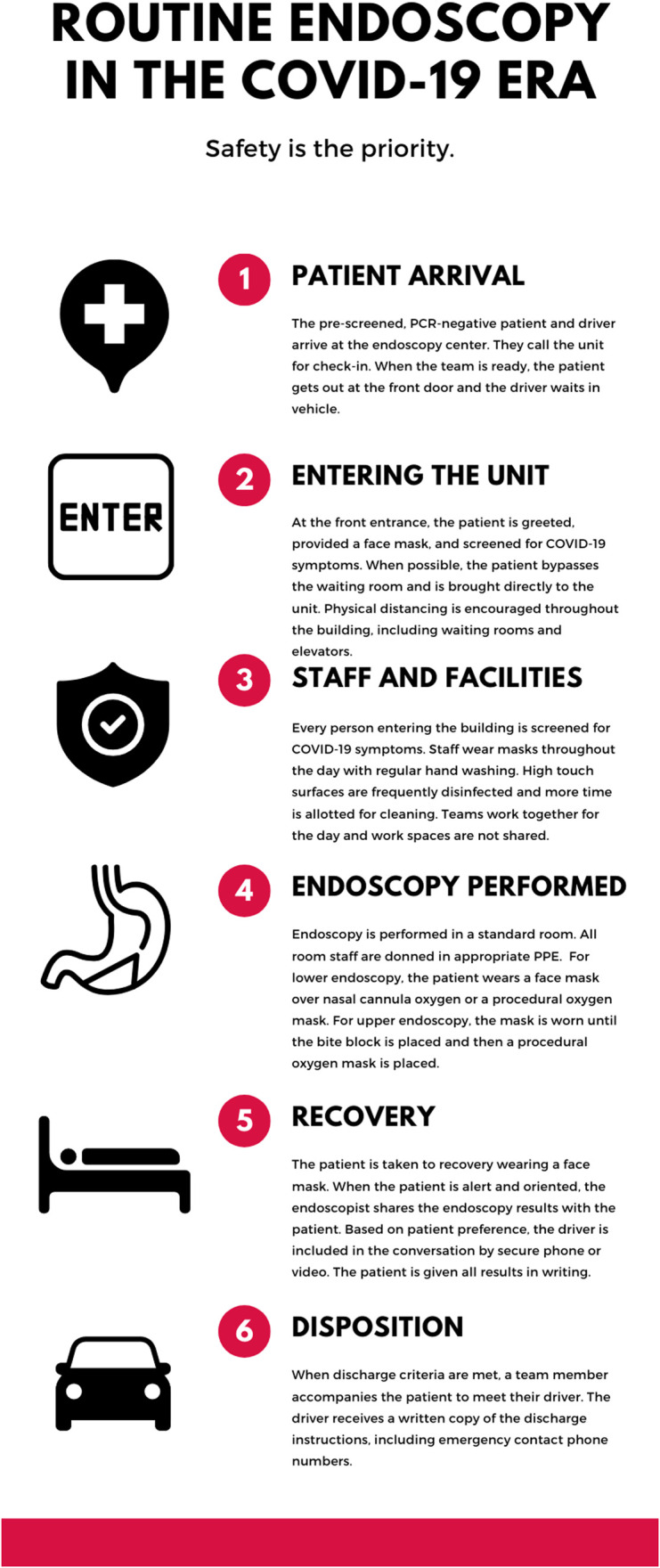
This is a graphical representation of how patients move through our endoscopy unit and the additional measures taken for safety.
WHO TO LET IN? HOW TO LET IN? AND WHO TO LET IN FIRST?
Who to let in?
Before COVID-19, our endoscopy units were highly trafficked. We welcomed families in our waiting rooms and onto our units for a patient's workup and discharge. Unfortunately, such visitors introduce the risk of COVID-19 exposure. To reduce that risk, we have decided to limit our endoscopy units to patients only. Because we recognize that communication is fundamental to high-quality care, we give families the information they need by either phone or videoconference while they wait in their vehicle or alternative waiting space (6). Such virtual communication does create new challenges to confidentiality—not all technology is Health Insurance Portability and Accountability Act-compliant, and patients often only want certain loved ones involved in their care. In urban areas, where mass transit is the norm, repurposing clinic rooms or other spaces into private waiting rooms may help create the necessary physical distance.
How to let in?
All patients are prescreened with a phone call well in advance of arrival at an endoscopy unit. We identify patients who are at high risk for COVID-19, review preparation instructions, and educate patients on the measures we are taking to reduce the risk of exposure in our units. For those patients who have GI symptoms and waiting on procedures, we coordinate telehealth visits to provide additional workup and treatment. Although our procedure areas are running at low volumes, we have much to offer with a telehealth visit, and staff effort normally directed at endoscopy has been shifted to reducing our backlog of clinic visits.
Any patients who are symptomatic with fever or upper respiratory symptoms are delayed when possible. Our intensive care colleagues have described cases of negative nasopharyngeal swabs but subsequent positive lung lavage samples. Patients who have symptoms and/or screen positive for SARS-CoV-2 only have urgent endoscopic procedure performed. We perform these procedures in a single unit, our hospital endoscopy suite, as the last case of the day in that room, with protocols in place for isolation and decontamination. Our outpatient endoscopy centers remain non-COVID-19 zones.
For patients with no symptoms of viral infection, we perform universal screening for SARS-CoV-2 with polymerase chain reaction (PCR) testing no more than 3 days before routine endoscopy, both to protect our staff and prevent mass nosocomial infection. Delaying patients with a positive test also benefits them because data suggest that minor elective surgery is associated with increased 30-day mortality in patients with perioperative SARS-CoV-2 infection, many of whom were asymptomatic (7).
Our hospital is currently using a PCR test that is easy to perform, accurate, and quick to result. It is performed on a “drive-through” basis at multiple sites to limit the burden of this preprocedure step on our patients. The prevalence of COVID-19 in our area has been low, and the sensitivity of our PCR test is as high as 95%. Although a negative result does not preclude infection, and sensitivity depends on proper collection, given the low pretest probability, the current risk of a false negative result at our center is 1 case per 1,500–2,000 patients tested, and even the compounded risk of caring for multiple patients a day remains very low.
Some providers may elect to perform symptom-based screening only while wearing an N95 or equivalent for the procedure. Although this approach may be necessary in areas with limited availability of testing, it will both miss asymptomatic carriers who could disseminate the virus while putting asymptomatic positive patients at an increased risk of postprocedure mortality. Because there are critical shortages of protective equipment nation, normally single-use N95s are being used across multiple patients and reprocessed for reuse. Extended use is associated with a higher failure rate for mask fit (8). In addition, if contaminated with the virus, using the same N95 across multiple patients poses a risk of transmission (9) such that covering the extended-use N95 mask with a loop mask for splash protection might be advisable.
Who to let in first?
In the United States, gastroenterologists perform 18 million endoscopies annually (10). As we resume routine practice, there will be a backlog of patients who need GI procedures. Although we have been performing urgent cases, many patients have postponed therapeutic and diagnostic endoscopies out of fear of SARS-CoV-2 exposure. Which patients should be the first of those postponed to have their procedures? As always, therapeutic endoscopy and diagnostic endoscopy for alarm symptoms and signs are high priority. A patient with a positive fecal immunochemical test is also considered high risk, especially ≥3 months after the test (11).
We have adopted a practical and evidenced-based framework for endoscopy case triage similar to that published by the Permanente Medical Group (12). The governing principle is that procedures most likely to benefit the patient should take precedence over lower yield examinations. In addition, surveillance endoscopies are being risk stratified, and the most recent US Multi-Society Task Force recommendations have helped us guide triage (13). Average-risk screening colonoscopy is lower priority still and, in patients who are afraid of return to the endoscopy unit, can be deferred for fecal immunochemical testing. Similar to approaches suggested for other disciplines, allocation of healthcare resources during the restart should be governed by logic, not patient proximity or cancer phobia (14).
MAKING THE ENDO SUITE MORE COVID-RESISTANT
We have engaged every stakeholder in our endoscopy unit to develop plans for a safe reopening. There is evidence that many staff are fearful of resuming routine endoscopy and contracting SARS-CoV-2 (15). Listening to and addressing all concerns early and often has been critical to reopening. It is often impossible to socially distance in the endoscopy unit. We work shoulder-to-shoulder with our teammates, and gastroenterologists and our teams are potentially vectors of SARS-CoV-2 transmission. In addition to hand hygiene and wearing personal protective equipment, we routinely screen staff with expanded symptom-based criteria. Liberal sick leave policies that encourage our teammates to stay home if they are symptomatic are important.
In our low prevalence area, asymptomatic patients who test negative for SARS-CoV-2 undergo colonoscopy by providers wearing a surgical mask and face shield, combined with gown and gloves. Staff performing upper endoscopy procedures, including endoscopic retrograde and endoscopic ultrasound, use the above protective equipment, with the addition of an N95 mask because of the potentially aerosolizing nature of these examinations and the inability of masking the patient. Using these protocols, even if a patient were to later test positive, any exposure to staff would meet the Centers for Disease Control and Prevention criteria for low risk of transmission.
New standards for unit decontamination procedures have become necessary, with concentrated efforts to clean and disinfec high-touch areas. For routine cases performed on asymptomatic patients who test negative for SARS-CoV-2, we are using standard rooms with standard air changes and have not required room settling time.
REIMAGINING ENDOSCOPY AFTER THE PANDEMIC
Until now, endoscopy units have been largely untouched by infectious disease concerns, with the occasional hepatitis B outbreak or concerns about infections from duodenoscope elevators as notable exceptions. This is likely to change in an enduring way in the wake of COVID-19. After the initial pandemic wave, there are projections for recurrent wintertime outbreaks of SARS-CoV-2, and it is quite likely that this pandemic will color at least some aspects of our operations chronically (5). Making durable and thoughtful changes now might not only protect our patients, colleagues, and staff from COVID-19 but may also better position us for what lies ahead. It is our hope that these new adaptations can both help our patients today and prevent a near-total shut down of our services in a future epidemic.
CONCLUSIONS
Although procedures that were not “urgent” have been delayed, the need for many of these procedures has not gone away—“elective” must not be misconstrued with “not necessary.” Unfortunately, some patients are afraid to seek health care and perceive the endoscopy unit as high risk. We must take every opportunity to dispel these fears and replace them with a realistic understanding of risks and benefits. To provide the care our patients deserve, we must develop new methods to keep them and ourselves safe. Although the challenges of COVID-19 have been time consuming and costly, a great deal has been sacrificed to flatten the curve. We now have a responsibility to move forward deliberately and with caution.
CONFLICTS OF INTEREST
Guarantor of the article: Anne F. Peery, MD, MSCR.
Specific author contributions: A.F.P., S.A., and N.J.S.: concept and design, drafting of the manuscript, and critical revision of the manuscript for content.
Financial support: This work was supported in part by a grant from the National Institutes of Health K23DK113225.
Potential competing interests: None to report.
REFERENCES
- 1.Lurie N, Saville M, Hatchett R, et al. Developing covid-19 vaccines at pandemic speed. N Engl J Med 2020;382:1969–73. [DOI] [PubMed] [Google Scholar]
- 2.Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med 2020;382:970–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2). Science 2020;368:489–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020;323:1406–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kissler SM, Tedijanto C, Goldstein E, et al. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science 2020;368:860–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siegel CA. Transforming gastroenterology care with telemedicine. Gastroenterology 2017;152:958–63. [DOI] [PubMed] [Google Scholar]
- 7.Collaborative CO. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: An international cohort study. Lancet 2020;396:27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Degesys NF, Wang RC, Kwan E, et al. Correlation between N95 extended use and reuse and fit failure in an emergency department. JAMA 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casanova L, Alfano-Sobsey E, Rutala WA, et al. Virus transfer from personal protective equipment to healthcare employees' skin and clothing. Emerg Infect Dis 2008;14:1291–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: Update 2018. Gastroenterology 2019;156:254–72 e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Corley DA, Jensen CD, Quinn VP, et al. Association between time to colonoscopy after a positive fecal test result and risk of colorectal cancer and cancer stage at diagnosis. JAMA 2017;317:1631–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rouillard S, Liu VX, Corley DA. COVID-19: Long-term planning for procedure-based specialties during extended mitigation and suppression strategies. Gastroenterology 2020. (doi: 10.1053/j.gastro.2020.05.047). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta S, Lieberman D, Anderson JC, et al. Recommendations for follow-up after colonoscopy and polypectomy: A consensus update by the US Multi-society Task Force on colorectal cancer. Gastroenterology 2020;158:1131–53 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prachand VN, Milner R, Angelos P, et al. Medically-necessary, time-sensitive procedures: A scoring system to ethically and efficiently manage resource scarcity and provider risk during the COVID-19 pandemic. J Am Coll Surg 2020. [Epub ahead of print, April 9, 2020.] (doi: 10.1016/j.jamcollsurg.2020.04.011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rex DK, Vemulapalli KC, Lahr RE, et al. Endoscopy staff are concerned about acquiring COVID-19 infection when resuming elective endoscopy. Gastroenterology 2020. (doi: 10.1053/j.gastro.2020.05.038) [DOI] [PMC free article] [PubMed] [Google Scholar]


