Abstract:
The coronavirus disease 2019 (COVID-19) pandemic has become the dominant health-care issue of this generation and has reached every corner of the health-care delivery spectrum. Our 3 orthopaedic departments enacted a response to the COVID-19 pandemic within our organizations. We discuss our health-care systems’ response to the outbreak and offer discussion for the recovery of the orthopaedic service line within large health-care systems.
The coronavirus disease 2019 (COVID-19) pandemic has become the dominant health-care issue of this generation and has reached every corner of the health-care delivery spectrum1. Its effect on the orthopaedic service line has been dramatic2. Vannabouathong et al. have described the current evidence and evolving strategies in this crisis3, as well as general descriptions of how to flatten the typical bell-shaped curve of growth of the infection. Health-care systems have enacted a response to the COVID-19 pandemic within a larger health-care paradigm and in the context of orthopaedic surgery. The pandemic and the orthopaedic hospital systems’ response described herein are only 4 months old at the time of this writing; as such, some of the citations are anecdotal and the value of this information awaits validation in hindsight in a more stable future. This document, compiled from the experiences of our 3 orthopaedic departments, can serve as a guide for other orthopaedic departments in hospital systems to utilize during this pandemic and later if the virus returns with a second infection curve as social distancing is relaxed, or in the fall, especially to areas in the United States and abroad where it has not been as formidable during this period. This is a review that also can be referenced during future pandemics as it describes many aspects of a pandemic response.
Realization of the Pandemic
The transition from hypothetical risk to a sudden awareness that the COVID-19 pandemic was upon us was striking and rapid. Drastic measures were taken, sometimes within hours, to dramatically alter routine processes. This phenomenon is not new and has been described with other pandemics, most notably in 1957 with the changes that occurred with the Asian flu pandemic in the United Kingdom4. In mid-March, organizations were tracking events abroad and had already begun general planning with the realization that COVID-19 was not going to have only a localized outbreak in the United States. On March 11, the World Health Organization (WHO) classified the outbreak as a pandemic1. Over the course of 4 days, from March 13 to March 16, the COVID-19 outbreak necessitated the eventual declaration of a national emergency5. State and local governments strengthened the response by issuing “stay-at-home” or “shelter-in-place” orders. Suddenly, most hospital systems immediately halted cases that were considered to be elective in order to decrease exposure risk, preserve personal protective equipment (PPE), and keep ventilators available. The impact of COVID-19 on Wuhan, People’s Republic of China and Northern Italy was a tragic example that the volume of infections might overwhelm our health-care systems6.
Overnight, change occurred in visit types from face-to-face to virtual (telephone and video). Decisions were made across our systems as to which offices to staff and maintain. Clinic staffs were quickly trained to work remotely and separated into rotations in order to avoid intraoffice transmission.
Clinic volumes decreased as many patients began to comply with the demand for social distancing. Office visit types changed dramatically as the pandemic hit (Table I). At 1 institution, there was a 400% increase in telephone visits, from around 5,000 to over 20,000. In the same time period, video visits increased over 900%.
TABLE I.
Visit-Type Transition*
| Jan. 2020 | Feb. 2020 | March 2020 | As of April 19, 2020 | |
| F2F | 93.6% | 93.4% | 72.1% | 20.7% |
| TV | 6.3% | 6.5% | 27.1% | 76.0% |
| VID | 0.1% | 0.1% | 0.8% | 3.3% |
F2F = face-to-face visits, TV = telephone visits, and VID = video visits.
Patients entering our facilities were now being tested for fever and were asked COVID-19 screening questions (regarding fever, cough, shortness of breath, current diarrhea, and loss of smell). Concurrently, physicians began social distancing with family at home to avoid transmission7,8. Virtual meetings became the exclusive means to discuss operational and administrative matters.
Leadership and Communication
Leadership generally needs to keep all staff informed in a transparent and clear fashion as this is vital to organizational success in the crisis of a pandemic. The leadership group or decision-making command structure serves its organization best if a periodic communication strategy is in place9. Initially, daily email communications and readily accessible information and guidelines allowed all to be on the same page. Vertical (across orthopaedics and multiple other disciplines at a single hospital) and horizontal (same orthopaedic department across multiple hospital sites in larger systems) messaging in larger organizations helps to keep cascading information streams in sync10. There must be respect for the fluidity of information and how instructions can change rapidly as more information is gathered about the pandemic. Many, including 1 of the authors of this paper, had prior experience from the severe acute respiratory syndrome (SARS) pandemic and were proponents of mandatory mask usage in the community. This was not recommended with COVID-19 initially but now has become standard. These day-to-day changes demand agility on the part of leaders to pivot and match resources to evolving needs on the front lines11. Additionally, a succession plan needs to be established in case a chief or department leader becomes ill, similar to continuity plans in any other business12. Many departments have created multiple teams that do not intermingle in order to avoid cross- contamination so that essential leadership functions can continue13.
Cessation of Elective Cases
On March 14, 2020, U.S. Surgeon General Jerome Adams retweeted the American College of Surgeons (ACS) “COVID-19: Recommendations for Management of Elective Surgical Procedures,” which recommended postponing elective surgeries14. As of April 10, 2020, 35 states had issued recommendations to halt elective surgeries. In a letter to the Surgeon General on March 15, the American Hospital Association (AHA), the Association of American Medical Colleges, and other groups noted that “‘elective’ simply means a procedure is scheduled rather than a response to an emergency.” In the absence of clear regulatory guidance, the AHA recommended that any cessation of elective procedures take into account the burden of COVID-19 at a facility or its surrounding area, the supply of PPE, the urgency of the procedures, patients’ risk factors, and clinical judgment15.
Two events reshaped the regulatory landscape in response to the worsening of the pandemic. First, on March 17, a recommendation to cancel all elective surgeries at hospitals came from Dr. Deborah Birx of the White House Coronavirus Task Force16. Second, the Centers for Medicare & Medicaid Services (CMS) released its “Non-Emergent, Elective Medical Services, and Treatment Recommendations” to help with the conservation of critical health-care resources (Table II)17. Following these events, several state and local leaders followed suit by issuing orders to hospitals and ambulatory surgery centers (ASCs) to cancel elective surgeries16. The ACS, the American Society of Anesthesiologists, and the Association of periOperative Registered Nurses recommended creating hospital surgical review committees18.
TABLE II.
| Tiers | Definition | Locations | Examples | Action |
| Tier 1 |
|
|
|
|
| Tier 2 |
|
|
|
|
| Tier 3 |
|
|
|
|
FQHC/RHC = Federally Qualified Health Care/Rural Health Clinics, and HOPD = Hospital Outpatient Department. †If a practice can provide only limited well child visits, health-care providers are encouraged to prioritize newborn care and vaccination of infants and young children (through 24 months of age) when possible (see also Centers for Disease Control and Prevention [CDC] guidance for further information: https://www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/index.html).
To allow for decision-making, review committees and surgeons will need to classify cases based on acuity as emergency, acute, or elective designations. A detailed classification of orthopaedic procedures and their acuity is listed in Table III.
TABLE III.
Acuity Classification of Orthopaedic Procedures*
| Emergency (<24 Hr) | Urgent (24 Hr to <6 Wk) | Elective (6 to 8 Wk) | ||
| Acute (24 to <48 Hr) | Subacute (48 Hr to <6 Wk) | |||
| Trauma |
|
|
|
|
| Adult Reconstruction |
|
Joint infection without sepsis |
|
All primary joints without collapse |
| Spine |
|
Cervical and thoracic myelopathy with progressive paralysis | Cervical and thoracic myelopathy without progressive paralysis |
|
| Pediatrics |
|
Displaced femoral fracture |
|
Deformity correction |
| Shoulder and elbow | Dislocation | Shoulder or elbow fracture-dislocation |
|
|
| Sports | Knee dislocation | Fresh OC allograft |
|
|
| Foot and ankle |
|
Displaced talar neck fracture |
|
|
| Hand |
|
Major motor nerve laceration | Digital nerve laceration with nerve or tendon injury |
|
| Oncology | Septic joint | Pathologic fracture |
|
|
MSK = musculoskeletal, SCFE = slipped capital femoral epiphysis, OC = osteochondral, and ACL = anterior cruciate ligament.
Shared decision-making19 in the setting of COVID-19 can be straightforward for emergency and acute cases. However, it is not so clear for subacute and even for some elective cases. For example, those with oncological diagnoses, severe pain, or chronic infections may be eager to move forward with surgery. The surgeon and the patient must discuss not only the traditional risks of surgery but also the potential risk of contracting COVID-19. The patient’s COVID-19 risk factors need to be assessed20 (Table IV). Finally, if the decision to proceed with surgery is made, the surgeon needs to justify the clinical necessity to the surgical review committee. The risks that are associated with COVID-19 should be documented. In California, the Department of Managed Health Care requires not only clinician documentation of surgery cancellation, but also documentation in the medical record that “a longer waiting time will not have a detrimental impact on the health of the enrollee.”21 Table V lists key regulatory considerations that come into play when deciding on case cancellations.
TABLE IV.
Risk Factors for COVID-19 Mortality20
| Age of ≥60 years |
| Cardiovascular disease |
| Diabetes |
| Respiratory disease |
| Cancer |
TABLE V.
Key Regulatory Considerations for Case Cancellation
| The number of current and projected COVID-19 cases locally and in surrounding regions |
| Federal, state, and local mandates |
| Guidance of hospital-level surgical review committees |
| Availability of and need to conserve personnel and supplies |
| Assessment of patient risk factors for COVID-19, including age and comorbidities |
| Classification of the acuity of the procedure |
| Shared decision-making between the surgeon and the patient |
| Documentation of case cancellation |
Safety in the Operating Room
Most operating rooms (ORs) require a 20-minute wait after the patient has been intubated as well as after extubation22. The 20-minute recommendation is based on the minimum standard of 15 air changes per hour (ACH) for ORs and data that show 99% elimination at 18 minutes and 99.9% at 21 minutes23. Orthopaedic surgeons and other nonessential personnel should be outside of the OR during those times.
There is concern that bone drilling, reaming, and cutting may aerosolize viruses. Orthopaedic surgeries utilizing power equipment and lavage have been classified as aerosol-generating medical procedures (AGMPs)24,25. The European Centre for Disease Prevention and Control (ECDC) published a statement about the interaction of COVID-19 and the supply of substances of human origin (i.e., blood for transfusion). The publication reports that there is enough uncertainty regarding COVID-19 viremia that the donor may be considered a potential threat26.
The concern over coronavirus and the wearing of orthopaedic surgical helmets was raised in a paper from Hong Kong during the SARS epidemic. Helmets are not marketed for respiratory protection and, when used alone, are not protection when performing AGMPs. The authors recommended the N100 mask (equivalent to an N95 mask) for protection from AGMPs27. Surgical helmets are not capable of in vivo filtration of sub-micrometer-sized particles and should not be used as respirators. The indrawn air potentially would be contaminated if the patient had an infection involving sub-micrometer-sized particles of a virus akin to COVID-1927. At best, the hoods are made from Association for the Advancement of Medical Instrumentation (AAMI) level-4 material. (The AAMI standard establishes a classification system [levels 1 to 4, with 4 being the most protective] for protective apparel that is used in health-care facilities, which is based on liquid barrier performance using standardized test methods)28. The 2 major vendors of these types of helmets came out with memoranda stating the fact that these hoods do not provide the level of protection that an N95 mask does and should not be used as respiratory protection systems29,30. Other specialties that are at higher risk of AGMPs (e.g., anesthesia and otolaryngology) have employed the use of powered air-purifying respirators (PAPRs).
Diagnostic testing will eventually be the best way to know what protection is most adequate. Testing for COVID-19 is in its infancy, and false-negative tests can occur31. As testing improves and is available, there will be an increase in orthopaedic surgeon safety in the OR32. Universal precautions are prudent and encourage a culture of safety in the OR33. Universal precautions, however, were designed to protect against blood and body fluids—they were not designed to specifically protect against airborne pathogens33.
Our recommendation is to continue universal precautions with the addition of an N95 mask and a face shield for bone cutting, reaming, and drilling procedures with patients who are positive for COVID-19 and persons under investigation (PUIs). N95 mask usage policies vary and are hotly debated as the threat of PPE shortages is real and there is pressure to conserve PPE for the cases with the most risk34. To our knowledge, there is no current evidence for use of a PAPR in the realm of orthopaedic surgery.
Redeployment of the Orthopaedic Surgeon
In the face of a potential surge of COVID-19 cases, orthopaedic musculoskeletal (MSK) care can be altered to suit this new environment. Full-service MSK care can be rendered by the orthopaedic department, including management and disposition after an emergency department (ED) or urgent care clinic (UCC)-directed medical screening examination (MSE). The goals of this type of work in the ED/UCC and in inpatient venues are listed in Table VI35.
TABLE VI.
Goals to Unload Other Services that Are Impacted by the Pandemic*
| ED/UCC Orthopaedic-Related Work | Inpatient Orthopaedic-Related Work |
|
|
ED = emergency department, UCC = urgent care clinic, MSK = musculoskeletal, MSE = medical screening examination, and PPE = personal protective equipment.
As elective surgeries plummet, orthopaedic teams have both the capacity and the skill set to redeploy to other areas of the hospital, which may free up medicine or surgery attending physicians who could serve in the intensive care unit (ICU) or the ED. Collaborative leadership in a crisis like this is imperative. “For when collaborative leadership is missing, personal survival and individual goals negate group goals, planning falls apart, and communication is shattered.”36 As redeployment is planned, communication with the frontline surgeons and their teams is imperative to morale. Lack of control in the practice environment is one of the major contributors to burnout, and this can be exacerbated with a top-down prescriptive approach that does not consider the autonomy of the surgeon. There may be a need to aid emergentologists, hospitalists, and intensivists in the most critical stages of the surge during a pandemic in academic and employed environments. Independent practices that do not have a direct hospital affiliation other than operative privileges may not fit into these types of hospital deployment plans.
Orthopaedic Recovery
At some point, the volume of new COVID-19 cases will start to decrease, and we will get past the surge of hospital admissions. Resources will get replenished, and hospital systems will be able to absorb intermittent surges. Scheduling of semielective and urgent surgical cases will present some challenges. With surgical volumes down substantially during the pandemic surge, the economics of our hospital systems will be strained37. Reemergence from restrictions will present many challenges. It is not expected that all lost volume will be recovered37. Restoration of new normal workflows and surgical volume is critical to organizational success.
It is imperative that a culture of safety is ensured for the staff and the patients. The OR and support staff need appropriate PPE and continued vigilance to prevent disease transmission. Ambulatory patients who are symptom-free may still be carriers. AGMPs will require PPE. Until a reliable test for COVID-19 is readily available, we must consider all of us and our patients as potential carriers. At the time of this publication, limited options are available for rapid ambulatory testing. False-negative rates have been described and vary based on testing methodology31.
In many of our facilities, OR staff has been reallocated to critical care due to reduced staffing needs. Protocols to ensure safety may increase anesthesia and OR time. PPE requirements can interfere with usual communication and the ergonomics of performing surgery. Prolonged OR times and deviation from standardized routines can lead to increased complication rates38. It is important for the surgeon to weigh these risks as elective surgery is reintroduced. We have been functioning for years in the presence of severe infectious agents, and in the environment of universal precautions, our health-care teams and patients have been reasonably protected.
A triage system needs to be in place to allocate potentially limited resources. The designation of certain facilities for elective surgery and at-risk surgery is needed. Cohorting (isolating multiple laboratory-confirmed COVID-19 cases together as a group) of documented or at-risk cases within facilities or at dedicated facilities can limit transmission risk. As health-care systems reintroduce urgent and elective surgery, the outpatient environment, particularly in stand-alone facilities, may offer the best option. Staff unwillingness to work during a viral pandemic may lead to a workforce reduction of 10% to 32%39,40. Supply chains have been disrupted for hospital systems, which may affect the ability to obtain the necessary implants for elective surgery patients41. We also need to consider utilization of resources such as hospital beds, staff, and physical therapists as availability may affect safety.
In addition to the emotional well-being of our physicians and staff42, we need to consider the emotional state of our patients. Many patients who require elective procedures may forego surgery at this time because of employment or financial concerns, potentially increasing the complexity of surgical burden later. In the People’s Republic of China, a recent study revealed poorer outcomes after elective surgery in asymptomatic patients who underwent surgery during the incubation period of their COVID-19 infection43. In that study of 34 surgical patients with confirmed COVID-19, 15 patients (44.1%) needed ICU care, and the mortality rate was 20.5%, highlighting the need for knowledge of preoperative COVID-19 status.
Reestablishing the elective orthopaedic service line is important for the well-being of our patients and society44,45 and will help in the financial recovery of our institutions.
The Second Curve: Lessons from Toronto in 2003
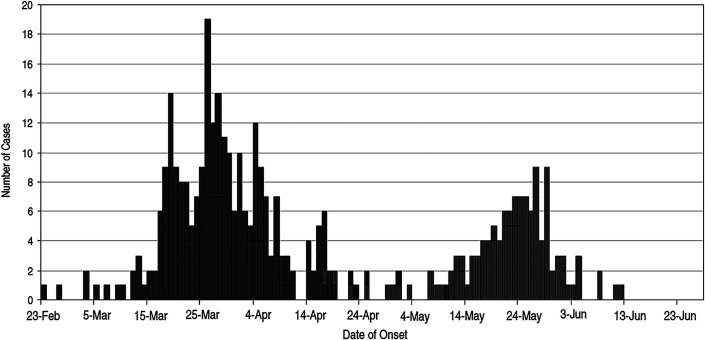
The importance of maintaining vigilance in hospitals and health systems as they return to new normal function is illustrated by the bimodal nature of the SARS outbreak curve in Toronto, Ontario, Canada46 (Fig. 1). By mid-May 2003, based on a clear end to the initial infection curve (plot of cases over time), a lack of new cases, and provincial directives, Toronto hospitals discontinued many precautions (e.g., the routine wearing of N95 masks)47. Unfortunately, an orthopaedic patient was admitted (with no precautions for staff and visitors) who was eventually diagnosed with SARS. This resulted in “phase II” of the SARS outbreak, with an additional 80 cases in staff, patients, and visitors. The return of a health-care system to pre-epidemic function can be a fragile process, and phase II of the 2003 SARS outbreak demonstrated the devastating effect that a single unrecognized case may produce. The risk of a recurrent outbreak must be balanced against the orthopaedic needs and requirements of the population, which continue unabated. While the risk is never zero, it can be minimized through a stepwise strategy for the reintroduction of surgery and procedures, with the utilization of “low-risk” facilities (i.e., ones that do not treat COVID-19 cases) for carefully screened healthy patients. Until a COVID-19 vaccine and rapid testing for active viral disease are readily available, a higher level of vigilance is required. As we discuss reestablishing the orthopaedic service line, the phrase “return to normal” has been carefully avoided. Following the SARS outbreak, new systematic standards and processes were instituted based on the deficits of the pre-SARS “normal” in order to create a health-care system that was more resilient to future outbreaks and promote the evolution to a new, and hopefully improved, standard. We believe that similar mindset changes will be seen after the COVID-9 crisis has resolved.
Fig. 1.
Double curve during the SARS outbreak in Toronto in 200346. Illustration of the double curve, or second wave, of infection that can occur in pandemics if appropriate measures are not adhered to when the threat of the pandemic is lessening. (Republished, with permission of The National Academies Press, from: SARS: lessons from Toronto, Low DE, in: Learning from SARS: preparing for the next disease outbreak: workshop summary, Institute of Medicine [U.S.] Forum on Microbial Threats; Knobler S, Mahmoud A, Lemon S, Mack A, Sivitz L, Oberholtzer K, editors. 2004; permission conveyed through Copyright Clearance Center, Inc.)
Summary
This paper describes 3 orthopaedic health-care and hospital systems’ response to the COVID-19 pandemic, and it can be used for reference and guidance. We know that other systems have much to contribute to the ongoing understanding of what the COVID-19 pandemic means to orthopaedic surgery, and our experience may be different from hotspots including New York, Detroit, and Boston. Each of our systems have experienced a surge in COVID-19 cases. Our orthopaedic systems’ responses to COVID-19 are ongoing. Thus far, health systems across the United States have responded in unprecedented ways. Cooperation to the extent that has been seen in the COVID-19 crisis among health-care systems, providers, government, and industry has never been seen before. Accelerated innovation that is associated with the response to this pandemic will change the face of health-care delivery. We will study our response for many years to come.
Acknowledgments
Note: The authors thank the numerous orthopaedic surgeons on our teams who have spent time thinking through these issues with us and who provide daily care with our allied care teams. Of course, all of the frontline health-care workers from all realms are the true heroes, and we salute them.
Footnotes
Investigation performed at Kaiser Permanente Southern California, Harbor City, Kaiser Permanente Southern California, San Diego, Kaiser Permanente Southern California, Los Angeles, California; the University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania; the University of Arizona College of Medicine-Phoenix, Phoenix, and Banner Health, Phoenix, Arizona
Disclosure: The authors indicated that no external funding was received for any aspect of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work and “yes” to indicate that the author had other relationships or activities that could be perceived to influence, or have the potential to influence, what was written in this work (http://links.lww.com/JBJS/F887).
References
- 1.World Health Organization (WHO). Coronavirus disease 2019 (COVID-19) situation report – 52. 2020 Mar 12. Accessed 2020 Apr 8 https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200312-sitrep-52-covid-19.pdf?sfvrsn=e2bfc9c0_4 [Google Scholar]
- 2.Chang Liang Z, Wang W, Murphy D, Po Hui JH. Novel coronavirus and orthopaedic surgery: early experiences from Singapore. J Bone Joint Surg Am. 2020. March 20 Epub 2020 Mar 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vannabouathong C, Devji T, Ekhtiari S, Chang Y, Phillips SA, Zhu M, Chagla Z, Main C, Bhandari M. Novel coronavirus COVID-19: current evidence and evolving strategies. J Bone Joint Surg Am. 2020. April 1 Epub 2020 Apr 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson C. History lessons: the Asian flu pandemic. Br J Gen Pract. 2009. August;59(565):622-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The President of the United States. Declaration of a national emergency concerning the novel coronavirus disease (COVID–19) outbreak. 2020. Mar 13, https://www.govinfo.gov/content/pkg/CDOC-116hdoc108/pdf/CDOC-116hdoc108.pdf Accessed 2020 Apr 8. [Google Scholar]
- 6.Ranney ML, Griffeth V, Jha AK. Critical supply shortages - the need for ventilators and personal protective equipment during the COVID-19 pandemic. N Engl J Med. 2020. March 25 Epub 2020 Mar 25. [DOI] [PubMed] [Google Scholar]
- 7.Guo X, Wang J, Hu D, Wu L, Gu L, Wang Y, Zhao J, Zeng L, Zhang J, Wu Y. Survey of COVID-19 disease among orthopaedic surgeons in Wuhan, People’s Republic of China. J Bone Joint Surg Am. 2020. April 8 Epub 2020 Apr 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cox JW, Miller ME, ‘Dad Jamison P., are you okay?’: doctors and nurses fighting pandemic fear infecting their families. The Washington Post. 2020. March 18 Accessed 2020 Apr 8 https://www.washingtonpost.com/local/dad-are-you-okay-doctors-and-nurses-fighting-pandemic-fear-infecting-their-families/2020/03/18/8beefc66-689b-11ea-b313-df458622c2cc_story.html [Google Scholar]
- 9.Lin L, McCloud RF, Bigman CA, Viswanath K. Tuning in and catching on? Examining the relationship between pandemic communication and awareness and knowledge of MERS in the USA. J Public Health (Oxf). 2017. June 1;39(2):282-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pandemic influenza preparedness and response. A WHO guidance document. Geneva: World Health Organization; 2009. ANNEX 2, REVISION PROCESS. https://www.ncbi.nlm.nih.gov/books/NBK143059/ [PubMed] [Google Scholar]
- 11.Patel M. Navigating unprecedented change through agile and disruptive leadership. Front Health Serv Manage. 2020. Spring;36(3):34-1-8. [DOI] [PubMed] [Google Scholar]
- 12.Financial Industry Regulatory Authority (FINRA). Pandemic-related business continuity planning, guidance and regulatory relief. 2020. March 9 Accessed 2020 Apr 9 https://www.finra.org/sites/default/files/2020-03/Regulatory-Notice-20-08.pdf [Google Scholar]
- 13.Occupational Safety and Health Administration (OSHA). Guidance on preparing workplaces for an influenza pandemic. 2009. May Accessed 2020 Apr 9 https://www.osha.gov/Publications/OSHA3327pandemic.pdf [Google Scholar]
- 14.@Surgeon_General. Hospital and healthcare systems, PLEASE CONSIDER STOPPING ELECTIVE PROCEDURES until we can #FlattenTheCurve! https://twitter.com/Surgeon_General/status/1238798972501852160 [retweet of @AmCollSurgeons with comment]. 2020 Mar 14. Accessed 2020 Apr 23. [Google Scholar]
- 15.American Association of Medical Colleges (AAMC). Letter to Vice Admiral Jerome M. Adams, 2020. March 15 Accessed 2020 Apr 9 https://www.aamc.org/system/files/2020-03/HALOLettertoSG-031520.pdf [Google Scholar]
- 16.Sealander K, Dombey D, Rogers A, Miller M, Madhani S. How to handle elective surgeries and procedures during the COVID-19 pandemic. McDermott Consulting. 2020 Mar 22; https://www.mwe.com/insights/how-to-handle-elective-surgeries-and-procedures-during-the-covid-19-pandemic/ Accessed 2020 Apr 9. [Google Scholar]
- 17.Centers for Medicare & Medicaid Services (CMS). Non-emergent, elective medical services, and treatment recommendations. 2020. April 7 Accessed 2020 Apr 8 https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf [Google Scholar]
- 18.American College of Surgeons (ACS). Create a surgical review committee for COVID-19 related surgical triage decision making. 2020. March 24 Accessed 2020 Apr 9 https://www.facs.org/covid-19/clinical-guidance/review-committee [Google Scholar]
- 19.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997. March;44(5):681-1-8. [DOI] [PubMed] [Google Scholar]
- 20.Porcheddu R, Serra C, Kelvin D, Kelvin N, Rubino S. Similarity in case fatality rates (CFR) of COVID-19/SARS-COV-2 in Italy and China. J Infect Dev Ctries. 2020. February 29;14(2):125-1-8. [DOI] [PubMed] [Google Scholar]
- 21.California Department of Managed Health Care (DHMC). APL 20-008 (OPL) - provision of health care services during self isolation orders. 2020. March 18 Accessed 2020 Apr 10 https://www.dmhc.ca.gov/Portals/0/Docs/OPL/APL%2020-008%20(OPL)%20-%20Provision%20of%20Health%20Care%20Services%20During%20Self%20Isolation%20Orders%20(3_18_20).pdf?ver=2020-03-18-105412-317 [Google Scholar]
- 22.Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID-19: guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia: 2020. March 27 Epub 2020 Mar 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Persily A. Challenges in developing ventilation and indoor air quality standards: the story of ASHRAE standard 62. Build Environ. 2015;91:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Judson SD, Munster VJ. Nosocomial transmission of emerging viruses via aerosol-generating medical procedures. Viruses. 2019. October 12;11(10):E940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen W, Lan Y, Yuan X, Deng X, Li Y, Cai X, Li L, He R, Tan Y, Deng X, Gao M, Tang G, Zhao L, Wang J, Fan Q, Wen C, Tong Y, Tang Y, Hu F, Li F, Tang X. Detectable 2019-nCoV viral RNA in blood is a strong indicator for the further clinical severity. Emerg Microbes Infect. 2020. February 26;9(1):469-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.European Centre for Disease Prevention and Control (ECDC). Coronavirus disease 2019 (COVID-19) and supply of substances of human origin in the EU/EEA. 23 March 2020. Accessed 2020 Apr 7 https://www.ecdc.europa.eu/en/publications-data/coronavirus-disease-2019-covid-19-and-supply-substances-human-origin-eueea [Google Scholar]
- 27.Derrick JL, Gomersall CD. Surgical helmets and SARS infection. Emerg Infect Dis. 2004. February;10(2):277-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Association for the Advancement of Medical Instrumentation (AAMI) Liquid barrier performance and classification of protective apparel and drapes intended for use in health care facilities. 2012. https://my.aami.org/store/detail.aspx?id=PB70-PDF Accessed 2020 Apr 23. Available at: [Google Scholar]
- 29.Biomet Zimmer. 2020 Apr 10; https://www.zimmerbiomet.com/content/dam/zimmer-biomet/medical-professionals/surgical-and-cement/TotalShield/totalshield-surgical-helmet-system-brochure.pdf TotalShield Surgical Helmet System. Accessed 2020 April 10.
- 30.Stryker Stryker. Flyte Personal Protection System – COVID-19 update. 2020. https://www.stryker.com/content/dam/stryker/orthopaedic-instruments/resources/Flyte%20Personal%20Protection%20System%20-%20COVID-19.pdf Accessed 2020 Apr 10. [Google Scholar]
- 31.Guo L, Ren L, Yang S, Xiao M, Chang D, Yang F, Dela Cruz CS, Wang Y, Wu C, Xiao Y, Zhang L, Han L, Dang S, Xu Y, Yang Q, Xu S, Zhu H, Xu Y, Jin Q, Sharma L, Wang L, Wang J. Profiling early humoral response to diagnose novel coronavirus disease (COVID-19). Clin Infect Dis. 2020. March 21:ciaa310 Epub 2020 Mar 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosenthal PJ. The importance of diagnostic testing during a viral pandemic: early lessons from novel coronavirus disease (COVID-19). Am J Trop Med Hyg. 2020. March 31 Epub 2020 Mar 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hopkins CC. AIDS. Implementation of universal blood and body fluid precautions. Infect Dis Clin North Am. 1989. December;3(4):747-1-8. [PubMed] [Google Scholar]
- 34.Iacobucci G. Covid-19: doctors still at “considerable risk” from lack of PPE, BMA warns. BMJ. 2020. March 31;368:m1316. [DOI] [PubMed] [Google Scholar]
- 35.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020. May;67(5):568-1-8 Epub 2020 Feb 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Digenti D. Lessons from Everest: the role of collaborative leadership in crisis. Systems Thinker. Accessed 2020 April 10 https://thesystemsthinker.com/lessons-from-everest-the-role-of-collaborative-leadership-in-crisis [Google Scholar]
- 37.Matheny J, Toner E, Waldhorn R. Financial effects of an influenza pandemic on US hospitals. J Health Care Finance. 2007. Fall;34(1):58-1-8. [PubMed] [Google Scholar]
- 38.Procter LD, Davenport DL, Bernard AC, Zwischenberger JB. General surgical operative duration is associated with increased risk-adjusted infectious complication rates and length of hospital stay. J Am Coll Surg. 2010. January;210(1):60-1-8e1: 2. Epub 2009 Nov 18. [DOI] [PubMed] [Google Scholar]
- 39.Shapira S, Friger M, Bar-Dayan Y, Aharonson-Daniel L. Healthcare workers’ willingness to respond following a disaster: a novel statistical approach toward data analysis. BMC Med Educ. 2019. May 3;19(1):130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Balicer RD, Barnett DJ, Thompson CB, Hsu EB, Catlett CL, Watson CM, Semon NL, Gwon HS, Links JM. Characterizing hospital workers’ willingness to report to duty in an influenza pandemic through threat- and efficacy-based assessment. BMC Public Health. 2010. July 26;10(1):436-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bohmer R, Pisano G, Sadun R, Tsai T. How hospitals can manage supply shortages as demand surges. Harvard Business Review. 2020;April:3. [Google Scholar]
- 42.Maunder RG, Leszcz M, Savage D, Adam MA, Peladeau N, Romano D, Rose M, Schulman B. Applying the lessons of SARS to pandemic influenza: an evidence-based approach to mitigating the stress experienced by healthcare workers. Can J Public Health. 2008. Nov-Dec;99(6):486-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, Zhan LY, Jia Y, Zhang L, Liu D, Xia ZY, Xia Z. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020. April 5:100331 Epub 2020 Apr 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shan L, Shan B, Suzuki A, Nouh F, Saxena A. Intermediate and long-term quality of life after total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Am. 2015. January 21;97(2):156-1-8. [DOI] [PubMed] [Google Scholar]
- 45.Chung SW, Park JS, Kim SH, Shin SH, Oh JH. Quality of life after arthroscopic rotator cuff repair: evaluation using SF-36 and an analysis of affecting clinical factors. Am J Sports Med. 2012. March;40(3):631-1-8 Epub 2011 Dec 21. [DOI] [PubMed] [Google Scholar]
- 46.SARS: lessons from Toronto, Low DE, in: Learning from SARS: preparing for the next disease outbreak: workshop summary, Institute of Medicine [U.S.] Forum on Microbial Threats; Knobler S, Mahmoud A, Lemon S, Mack A, Sivitz L, Oberholtzer K, editors. 2004 [PubMed] [Google Scholar]
- 47.Knobler S, Mahmoud A, Lemon S, Mack A, Sivitz L, Oberholtzer K; Institute of Medicine (US) Forum on Microbial Threats, editors. Learning from SARS: preparing for the next disease outbreak: workshop summary. Washington: National Academies Press; 2004. [PubMed] [Google Scholar]