Abstract
Background
Primary care providers (PCPs) are critical to the provision of comprehensive care for cancer survivors yet there is very little data on the practices and quality of survivorship care occurring in safety net primary care settings. This study aimed to assess the knowledge and attitudes of PCPs and preferences for care models for breast and colon cancer survivors in a safety net health network.
Methods
A modified National Cancer Institute Survey of Physician Attitudes Regarding the Care of Cancer Survivors was sent electronically to 220 PCPs in 12 primary care clinics in the San Francisco Health Network affiliated with Zuckerberg San Francisco General Hospital.
Results
The response rate was 50% (110/220). About half of PCPs strongly/somewhat agreed (vs. strongly/somewhat disagreed) that PCPs have the knowledge needed to provide follow-up care related to breast (50%) and colon cancer (54%). Most providers (93%) correctly reported recommended frequency of mammography, however, frequency of blood tests and other imaging surveillance were not as well recognized for breast or colon cancer. Recognition of long-term side effects of chemotherapy drugs ranged from 12% for oxaliplatin to 44% for doxorubicin. Only 33% of providers reported receiving any survivorship training. The most preferred model for survivorship care was shared care model (40%).
Conclusions
Safety net PCPs prefer a shared care model for care of cancer survivors but are limited by lack of training, poor communication, and poor delineation of roles. Patient centered survivorship care can be improved through effective oncologist-PCP-patient partnerships and coordination.
Keywords: Cancer survivorship care, Safety net, Primary care providers, Shared Care model
INTRODUCTION
With recent advances in cancer early detection and treatment, the number of cancer survivors has continued to increase. In January 2019, there were an estimated 16.9 million cancer survivors in the United States and this figure is estimated to reach 21.7 million by 2029(1). Significant health-related issues are present during the survivorship phase of the cancer care continuum. Cancer survivors report decreased health-related quality of life (HrQoL) due to physical, emotional, financial, employment, and health insurance concerns.(2–4). In addition to addressing the need for early detection of recurrence and screening for new cancers, survivorship care also represents an opportunity to promote the adoption of healthy behaviors to decrease risk of recurrence or secondary cancers. For example, post treatment physical activity is associated with decreased recurrence and increased overall survival from some cancers while, in contrast, obesity and alcohol use have been consistently associated with poorer outcomes (5). In 2006, the Institute of Medicine identified the goals of cancer survivorship care as surveillance for recurrence and new malignancies, recognition and management of long term and late effects of treatment, health promotion, optimization of psychosocial well-being, and coordination of cancer survivors’ care across health care systems and providers (6).
In the United States, cancer survivorship care is provided by a variety of professionals including cancer specialists, primary care providers (PCPs), nurse practitioners (NP), and physician assistants (PA), utilizing a variety of models of care. These survivorship care models include: 1) consultative model with a one-time visit with a physician, NP or PA but no scheduled follow up; 2) organ-or type-specific oncology specialty clinic focused on survivorship and integrated care; 3) transition model from oncology to primary care after the active treatment phase; 4) a generalist model in which a primary care provider manages cancer care; or a 5) shared care model between oncologists and PCPs where care is coordinated between PCP and oncology specialists (7)(8). As more people survive cancer, health systems have increasingly looked to chronic disease models to determine how to sustainably manage longitudinal care of cancer survivors. Primary care centered chronic disease management models have been implemented successfully in primary care practices to improve diabetes, asthma and congestive heart failure care, and could be applied to cancer survivorship programs (9).
Many of the survivorship care models described above are resource intensive and may not be feasible in health systems that care for low income, uninsured or publicly insured patients or for community providers outside major academic institutions(10). Safety net settings in the United States are public hospitals and community clinics that are critical in providing care and services to patients who are low-income, medically underserved, immigrants, and racially and ethnically diverse. Primary care physicians in safety net settings experience significant challenges when providing general medical and cancer survivorship care. A significant number of patients in safety net institutions are low-income, and may have low educational attainment, lack of social support, and limited English proficiency. Given these resource constraints and patient characteristics, the shared care model may be the most feasible to adopt in safety net settings. Two arguments can be made for using the shared care model. The first is the projected shortage of oncologists due to the growth of the aging population (11) (12). The second reason for a shared care model is that it builds on the expertise of PCPs in prevention and health maintenance, which are central to the care of cancer survivors (13).Thus, a shared care model where PCPs and oncologists co-manage cancer survivors for the first five years after diagnosis when recurrence risk is highest, and then survivors are transitioned to the care of PCPs alone, is more likely to be feasible in resource constrained settings (11).
Yet data suggest that PCPs may not feel confident in their knowledge and skills related to caring for cancer survivors(14). A survey of PCPs and oncologists indicated that significant gaps exist in knowledge among PCPs about recognition of long term and late effects of cancer treatments (14) (15). Nekhlydov, et al., reported that almost all oncologists reported awareness of cardiac dysfunction as a late effect of doxorubicin use (95%) and neuropathy as a late effect of paclitaxel (97%) and oxaliplatin (97%) use, while PCPs reported lower awareness of these late effects at 55%, 27% and 22% (16).
In addition, patients and oncologists may have concerns about the role of PCPs in survivorship care. Patients may perceive their PCPs as less knowledgeable about cancer care relative to oncologists (17). Oncologists may underestimate the role of PCPs in cancer survivorship care and may perceive that PCPs lack the necessary skills for providing survivorship care (18) (15). To explore these issues, the National Cancer Institute and American Cancer Society collaborated to develop the Survey of Physician Attitudes Regarding the Care of Cancer Survivors (SPARCCS) (19). The majority of PCPs in this study expressed uncertainty about their own skill level and knowledge about providing care for cancer survivors and highlighted the barriers between PCPs and oncologists. However, this study did not address the unique challenges faced by PCPs who practice in safety net settings and how practice factors affect their perceptions related to self-efficacy for providing cancer survivorship care.
There is very little data on the practices and quality of survivorship care occurring in safety net settings. One study conducted in a safety net setting demonstrated that PCPs reported feeling inadequately prepared to care for breast cancer survivors (14). Only one in five PCPs reported feeling very confident in providing all aspects of care for cancer survivors and only 31% of PCPs believed that PCPs should have primary responsibility for providing cancer survivorship care. PCPs who predominantly cared for indigent patients were more likely to agree that PCPs should take primary responsibility for survivorship care (14). To address limited research on the unique challenges of providing survivorship care among safety net PCPs, this article reports findings from a survey conducted among PCPs in the San Francisco Health Network (SFHN), a network of clinics, hospitals and programs that provide comprehensive health care to residents of the city and county of San Francisco. This study aimed to assess PCPs’: 1) perceptions of the components of cancer survivorship care; 2) preferred model of cancer survivorship care; 3) confidence in their knowledge and skills with regards to care of cancer survivors; and 4) barriers to transition of care between PCPs and oncology specialists in a public safety net health care system.
METHODS
Setting, Recruitment and Procedures
The San Francisco Health Network (SFHN) is a system of care for indigent and low-income residents of San Francisco. The SFHN is affiliated with Zuckerberg San Francisco General Hospital and part of the San Francisco Department of Public Health. An email invitation with an electronic link to the survey was sent out to all PCPs (physicians, nurse practitioners and physician assistants) practicing in the 12 primary care clinics of the SFHN. The list of the PCPs was obtained from the master email distribution list used by SFHN to communicate with providers. The University of California San Francisco institutional review board approved the study. The email invitation was sent weekly over a period of four weeks. The survey was administered, and data were managed using a HIPAA compliant Research Electronic Data Capture system (REDCap) hosted at the University of California San Francisco. REDCap is a secure, web-based application designed to support data capture and management for research studies(20).
Survey Overview
We used a modified version of the SPARCCS survey created by the National Cancer Institute and American Cancer Society (available as appendix)(19). The study team modified the SPARCCS content to be more suitable for PCPs practicing in our local setting, and for safety net settings more broadly. We modified the question about most preferred option for survivorship care by dividing it into two questions asking separately for most preferred and least preferred model for providing survivorship care. We modified the response categories of an item asking about the site of their practice to include hospital-based primary care, community-based primary care, and a non-SFHN primary care health center. We added questions on the proportion of patients they care for with limited English proficiency and public health insurance. Finally, we excluded a question about employee versus practice ownership status of respondents, as this was not applicable to SFHN because all PCPs are employees. We excluded cyclophosphamide and 5-fluorouracil in chemotherapy related side effects to reduce the length of the survey. We also included a question about the impact of a cancer diagnosis on management of co-morbid medical conditions. The survey included a free text item where we asked PCPs to provide additional feedback or perspectives not addressed in the survey (“Are there any additional thoughts, issues or needs you wish to share? Please feel free to write in the space, as we welcome your feedback”).
Vignettes
To assess surveillance care practices, the survey used a vignette of a 55-year-old woman with stage III breast cancer who had surgery and adjuvant chemotherapy four years ago, not on endocrine therapy and with no major comorbidities. A similar vignette of a 4-year survivor of stage III colon cancer was used to assess surveillance practices for colon cancer. Respondents were asked how frequently surveillance such as clinical exam and laboratory testing and imaging should be performed. We used National Comprehensive Cancer Network (NCCN) guidelines at the time of the survey as the standard (21) (22).
Data Analysis
Item-level percentages were calculated as the proportion of completed responses. Confidence intervals were generated using the standard error of proportion where appropriate. Missing data on items varied from 16–30%. Sub-group analysis was done by location of the practice, receipt of survivorship care training, teaching versus non-teaching positions, number of uninsured patients and receipt of treatment summary. The differences between subgroups were analyzed using Chi-square tests of independence. Analyses were performed using SAS software.
Results
Clinician and practice characteristics
The survey invitation was emailed to 220 providers in 12 SFHN primary care clinics. Half (N=110) responded to the survey. No financial incentive was offered for participation. The majority of providers were trained in family medicine (60%) and internal medicine (36%) (Table 1). Over 65% of PCPs reported that greater than half of their patients had Medicaid insurance (public health insurance for low income). About a quarter of PCPs reported that greater than 25% of their patients were uninsured. Nearly all respondents reported use of some type of electronic medical records: full (81%) or in transition to full (8%) electronic medical records. Only 33% of providers reported having received training in survivorship care. For PCPs reporting any training regarding late and long term effects of cancer treatments, sources of training were CME (16%), colleagues (14%), professional meetings and conferences (6%), postgraduate medical training (i.e. residency or fellowship) (6%), medical school (3.7%), and medical journals (2.5%). Respondents were evenly divided between hospital-based and community-based settings as their primary practice settings.
Table 1.
Primary Care Clinician and Practice Characteristics, San Francisco Health Network, N=110.
| Characteristics | n (%) |
|---|---|
| Specialty | |
| Family Medicine | 49 (60) |
| Internal Medicine | 29 (36) |
| Other | 3 (4) |
| Training | |
| Doctor of Medicine (MD)/Doctor of Osteopathic Medicine (DO) | 52 (64) |
| Advanced Practitioner; nurse practitioner (NP)/Physician Assistants (PA) | 19 (23) |
| Resident/Fellow | 10 (12) |
| Race of clinician | |
| White | 51 (62 |
| Asian | 22 (27) |
| Black or African American | 6 (7.5 |
| American Indian/Alaska Native | 2 (2.5) |
| Ethnicity of clinician | |
| Hispanic | 5 (6) |
| Non-Hispanic | 76 (96) |
| Primary site of practice | |
| Hospital-based primary care | 40 (49) |
| Community-based primary care | 40 (49) |
| Non-San Francisco Health Network site | 1 (1.2) |
| Number of patients seen weekly | |
| 25 or fewer | 41 (51) |
| 26–50 | 27 (33) |
| 50 or greater | 12 (14.5) |
| Patients with limited English proficiency | |
| 1–25% | 13 (16) |
| 25–50% | 37 (46) |
| 50–75% | 18 (22) |
| 75–100% | 11 (14) |
| Current Teaching Position | |
| Yes | 55 (68) |
| No | 26 (32) |
| Received Training in Survivorship Care | |
| Yes | 27 (33) |
| No | 54 (65) |
| Patients with Medicaid (MediCal) | |
| <50% | 20 (25) |
| >50% | 84 (65) |
n and percentages do not add up to 100% due to missing data.
Cancer surveillance care practices
Based on the vignette and NCCN guidelines for surveillance of breast cancer, 93% correctly reported the recommended interval for mammograms which is 6–12 months, 48% for MRI for breast cancer surveillance, 47% for blood test, 61% for bone scan and 55% for PET scans Regarding colon cancer surveillance, 20% correctly identified the recommended frequency for physical exams, 9% for labs, 14% for tumor markers, and 41% for FOBT screening and 16% for CT scan imaging (Table 2). About a third of PCPs (33%) reported that management of comorbidity was somewhat or much more difficult for cancer survivors than patients without a history of cancers while 60% reported no change.
Table 2.
Percent of Primary Care Clinicians Correctly Identifying Recommended Breast and Colon Cancer Surveillance Care Practices, San Francisco Health Network, N=110.
| Surveillance exam/test | % Correctly identifying recommended frequency of exam/test1 | 95% Confidence interval |
|---|---|---|
| Breast cancer | ||
| Mammogram | 93 | 86–97 |
| MRI | 47 | 38–58 |
| Blood test | 47 | 36–57 |
| Tumor Markers | 38 | 28–47 |
| PET scan | 55 | 45–65 |
| Bone Scan | 61 | 52–71 |
| Colon | ||
| FOBT | 41 | 30–51 |
| Tumor Markers | 14 | 07–22 |
| CT scan | 16 | 08–23 |
| PET scan | 11 | 04–17 |
Based on National Comprehensive Cancer Network guidelines
Confidence in knowledge and skills related to cancer care
About half of providers strongly/somewhat agreed that PCPs possess the knowledge necessary for follow up care for breast cancer (50%) and colon cancer (54%). More than half of PCPs reported being very/somewhat confident in their knowledge related to appropriate surveillance testing to detect recurrence of breast cancer (64%) and colon (72%) cancer. About half of PCPs felt somewhat or very confident in managing late and long-term effects of breast (55%) and colon cancer (51%). Most of the PCPs felt very/somewhat confident in managing adverse psychosocial outcomes of breast (87%) and colon (88%) cancers (Table 3).
Table 3.
Primary Care Clinicians’ Confidence in Breast and Colon Cancer Surveillance Knowledge and Skills, N=110.
| How confident are you about doing the following… | Percent responding very/somewhat confident (versus not at all/don’t know) | 95% Confidence interval |
|---|---|---|
| Appropriate surveillance to detect recurrent breast cancer | 64 | (56–75) |
| Managing long term and late physical adverse effects of breast cancer treatment | 55 | (45–64) |
| Psychosocial effects of breast cancer | 87 | (78–92) |
| Appropriate surveillance to detect recurrent Colon cancer | 72 | (63–81) |
| Managing long term and late physical adverse effects of colon cancer treatment | 51 | (40–61) |
| Psychosocial effects of colon cancer | 88 | (82–94) |
Management of long-term treatment effects and health maintenance
Monitoring of long-term adverse effects of treatments was less well-recognized than surveillance practices, with only 12% of PCPs correctly identifying neuropathy as an adverse effect of oxaliplatin; 44% recognizing cardiotoxicity as an adverse effect of Doxorubicin (Adriamycin) and 28% recognizing paclitaxel-induced neuropathy (results not tabled). Regarding self-reported practices, PCPs were less likely to provide care for pain due to cancer (41%), fatigue due to cancer (38%), and sexual dysfunction (46%) than counseling for diet and physical activity (64%) and smoking cessation (79%).
Clinician communication about transitions of care
Only about 20% of PCPs reported that they often or always received a comprehensive cancer treatment summary from oncology (Table 4). Slightly over a third of PCPs indicated that they provided a summary of patients’ non-cancer medical history to oncology (37.5%). Only 15.2% of PCPs reported receiving a follow up care plan from patients’ oncologist with explicit recommendations for follow up care and surveillance. Over a fourth of PCPs reported having discussions with their patients who had cancer about specific recommendations for future cancer care and surveillance (28.8%) and about half discussed with patients who would provide follow up care for cancer (48.8 %) and other medical issues (48.8%).
Table 4.
Primary Care Clinicians’ Communication During Transitions of Care of Breast and Colorectal Cancer Patients, N=110.
| How often do you….1 | % Often or Always |
|---|---|
| Receive a comprehensive summary including cancer treatment information from the patient’s oncology specialist. | 20 |
| Provide a summary of the patient’s past non-cancer medical history for the patient’s oncology specialist. | 38 |
| Receive from the patient’s oncologist an explicit follow-up care plan documenting recommendation for future care and surveillance. | 15 |
| Receive information from the oncology specialist in a timely manner. | 38 |
| Experience difficulties transferring patient care responsibilities between you and the oncology specialist. | 27 |
| Have a specific discussion with the patient regarding recommendation for future care and surveillance. | 29 |
| Discuss with your patient who will provide care for other medical issues. | 49 |
| Communicate with patients’ other physicians about responsibility of follow up care for their cancer. | 28 |
| Discuss with the patient who will provide follow up care for cancer. | 49 |
Response options were always, often, sometimes, rarely, and never
A review of responses to the open-ended question asking if they had any additional comments indicated that PCPs felt that communication from the oncologist could be significantly improved when transitioning the patient to primary care. Some illustrative comments were: “The oncology notes do not make the surveillance plan clear. -There isn’t a specific ‘hand off’ plan and communication”; “There is NO communication from oncology to PCPs at all, including about what the long term agreements/plan/treatment should be” and “PCPs don’t get a list of the recommended follow-up needed when cancer survivors are discharged back to us. We know we need to do the usual preventative care but don’t get guidance on what care and or surveillance to give related to the cancer.”
Barriers to Providing Cancer Survivorship Care
Regarding barriers to the provision of cancer survivorship care, 71% of PCPs reported that uncertainty about delineation of care between oncology and primary care was a barrier to provision of care sometimes, often or always. Three-fourths of PCPs reported that lack of knowledge or training was a barrier to providing survivorship care sometimes, often or always. More than a third (38%) reported that insurance or inability to pay was a barrier sometimes, often or always. Over half of PCPs (53%) reported being contacted by patients for oncology issues at least sometimes/often/always.
Preferred model of care
The shared care model where oncologists and primary care providers share responsibility was most often chosen by PCPs as the most preferred model for cancer survivorship (40%), followed by specialized clinics led by oncology nurses, nurse practitioners, or physician assistants who focus exclusively on cancer survivorship care (Figure 1). The PCP-led and oncology-led models of care tied for least preferred model of care, with 12.2 % of PCPs selecting one of these as their preferred model of survivorship care. A majority of PCPs (61%) wanted the oncologist to be involved in the care of cancer survivors for 5 years after diagnosis and only 5% wanted the oncologist to follow the patient indefinitely.
Fig. 1.
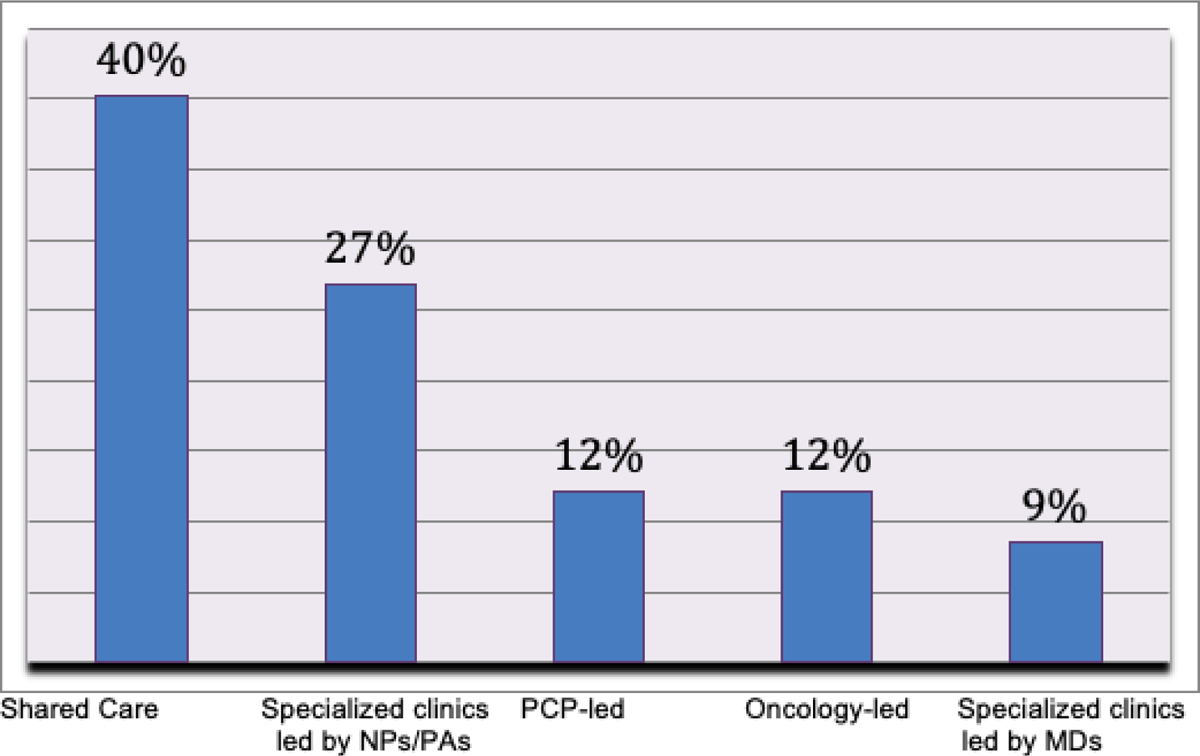
Safety Net Primary Care Provider’ Preferred Model of Care
An exploratory subgroup analysis showed that PCPs in hospital-based primary care were more likely than community-based PCPs to accept responsibility for breast cancer surveillance (P < 0.0, Chi-Square value 6.94) and to report being somewhat/very confident in their knowledge to provide follow up care related to colon cancer (P= 0.05, Chi Square value 3.8). PCPs who reported survivorship care training were more confident in breast cancer surveillance (P = 0.03, Chi-Square value 4.61) and in their knowledge necessary to initiate appropriate screening and diagnostic testing to detect recurrent breast cancer (P < 0.01, Chi-Square value 7.83), and colon cancer (P = 0.02, Chi-Square value 5.36) as compared to those with no training.
Discussion
This study sought to describe self-assessed knowledge, self-efficacy and practices of primary care providers for providing cancer survivorship care for colon and breast cancer survivors seen in their safety-net practices. We found that PCPs in our safety net networks want to share the responsibility for providing cancer survivorship care with oncologists. Although at least half the PCPs in our survey expressed confidence in their knowledge and skills to provide care to cancer survivors, awareness of long-term chemotherapy related side effects was low. While almost all providers correctly reported the recommended frequency of mammogram surveillance for breast cancer, fewer providers accurately reported other surveillance testing for breast and surveillance testing for colon cancer, which can result in both under and over testing.
Providers in our health system were as confident in their knowledge regarding follow up care for breast cancer (50%) and colon cancer (54%) as PCPs participating in a national survey(18). Our PCPs were more likely to be confident in providing psychosocial care than as reported by Dawes et al in their survey of PCPs in the safety net (14). A potential explanation for PCPs in our study feeling more confident in their ability to manage psychosocial aspects of cancer survivors’ care could be because behavioral health specialists are embedded in the primary care clinics in the SFHN.
Only a small proportion of PCPs reported having received training in cancer survivorship and management of long term and late effects of cancers. Survivorship care training emerged as a significant indicator of confidence in their survivorship care. Similar to our study, Virgo et al showed inadequate survivorship care training as a barrier to survivorship care (23).
Providing PCPs with adequate resources for managing the cancer survivorship care needs of their patients is clearly needed based on our findings and those of others. Because PCPs often struggle with insufficient time and resources, especially in safety net settings where they tend to see sicker patients, these resources will need to be provided in user-friendly, readily accessible formats. Increasing PCPs clinical responsibilities to encompass cancer survivorship care, as well as an increasing array of new therapies in cancer care, make providing the needed training and resources especially challenging. Clearly, we cannot expect PCPs to have the expertise or time to manage surveillance imaging and lab tests and long-term effects of chemotherapy for all cancers and regimens. However, increased access via the electronic health record (EHR) to oncology-initiated cancer survivorship care plans that provide more detailed care plans and clinical guidelines for cancer follow-up care are promising avenues. Use of EHRs that have prompts and recommendations built-in for surveillance can be a critical resource to PCPs, especially those in low resource settings. Increased opportunities for teleconsulting between PCPs and oncologists once patients are transferred to primary care would also help. Additionally, access to training on survivorship care and resources such as those of the National Comprehensive Cancer Network and American Society of Clinical Oncology could be added in medical school and residency curricula, continuing medical education programs, survivorship educational sessions at annual conferences, and web based on-demand training.
Our findings highlight the need for improving coordination and communication in the care of cancer survivors. The lack of oncologist-PCP bidirectional communication was a significant barrier observed in our study that could affect the quality of care provided to cancer survivors, especially during transitions of care. As our study shows, it is even more important in situations where PCPs are not co-located or part of the same health system as the oncology practice. Initiatives directed at improving communication on cancer survivorship care, such as survivorship care plans (SCPs) and cancer treatment summaries may be helpful; however research so far indicates SCPs show modest or no benefit in terms of patient outcomes (24–26). Interactive and easy to update survivorship care plans that are embedded within EHRs and are supplemented by a robust process for transitioning cancer survivors between specialists and primary care providers have the potential to improve cancer survivorship care and the overall health of cancer survivors. In addition, comprehensive survivorship care programs leveraging all available resources in easily accessible formats can also serve to identify patient needs, improve communication and facilitate referrals to appropriate services.
Survivorship care is a collective responsibility of health care systems and it needs to be provided well beyond the oncology specialty care phase. The chronic disease model offers an appropriate approach to survivorship care, with identification and management of long-term side effects, surveillance, and health maintenance. Patient centered medical homes are an additional resource and have been shown to improve the chronic disease care of vulnerable patients (28 (27). These resources were brought together in a National Cancer Forum report on a workshop on long term follow up of cancer survivors which emphasized the concept of medical home in the care of cancer survivors and the importance of care coordination (28). Shared care models, preferred by PCPs in our study, leverage the primary care focused “patient centered medical home” model with a focus on health maintenance, while still benefitting from oncology expertise.
Our study has several limitations. It is limited to a single health network and a safety net health network. Thus, our findings may not reflect other health care settings where the challenges may be different. We also used an electronic email invitation and an online system for our survey and thus we do not know the details of providers who did not respond to the survey. Half of respondents did not respond, and we do not know the types of bias such nonresponse might have introduced.
As the population of cancer survivors continues to increase, there is an increasing need for high quality survivorship care that focuses not only on cancer recurrence and surveillance, but also on management of long term and late effects of cancer and health maintenance (29). A significant number of patients seen in primary care clinics will be cancer survivors. The increase in new cancer cases is likely to include older and racially and ethnically diverse patients. Many of these patients will be seen in safety net hospitals with limited specialty and primary care resources. There is an urgent need to improve the care of cancer survivors in safety net systems by building effective patient, PCP and oncology partnerships and coordination of care.
Supplementary Material
Acknowledgments
This study was funded by Center of Aging in Diverse Communities (CADC) Scholars grant from the National Institute of Aging, grant no. P30 AG15272; National Center for Advancing Translational Sciences of the National Institutes of Health” under award Number UL1TR001105, and the Division of Intramural Research, National Institute on Minority Health and Health Disparities, National Institutes of Health. Dr. Sarkar was supported by K24 CA212294-01, National Cancer Society, National Institutes of Health.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Publisher's Disclaimer: Disclaimer
Publisher's Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
Dr. Anna Maria Napoles is an employee of National Institute of Health (NIH). Other authors have no financial conflict of interest with the funding agency. None of the funding agency were involved in conduct of this research and the preparation of this manuscript. Authors have full control of the primary data and will allow the review of full data if requested by Journal of Supportive Care in Cancer.
References
- 1.Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the “Silver Tsunami”: Prevalence Trajectories and Comorbidity Burden among Older Cancer Survivors in the United States. Cancer Epidemiol Biomarkers Prev. 2016. July 01;25(7):1029–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walsh K. Addressing psychosocial issues in cancer survivorship: past, present and future. Future Oncol. 2016. December;12(24):2823–34. [DOI] [PubMed] [Google Scholar]
- 3.Oancea SC, Cheruvu VK. Psychological distress among adult cancer survivors: importance of survivorship care plan. Support Care Cancer. 2016. November;24(11):4523–31. [DOI] [PubMed] [Google Scholar]
- 4.Nekhlyudov L, Walker R, Ziebell R, Rabin B, Nutt S, Chubak J. Cancer survivors’ experiences with insurance, finances, and employment: results from a multisite study. J Cancer Surviv. 2016. June 9. [DOI] [PubMed] [Google Scholar]
- 5.McTiernan A, Irwin M, Vongruenigen V. Weight, physical activity, diet, and prognosis in breast and gynecologic cancers. J Clin Oncol. 2010;28: 4074–4080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Institute oM, National RC. From Cancer Patient to Cancer Survivor: Lost in Transition. Maria Hewitt, Sheldon Greenfield, Ellen Stovall, editors. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 7.Halpern MT, Viswanathan M, Evans TS, Birken SA, Basch E, Mayer DK. Models of Cancer Survivorship Care: Overview and Summary of Current Evidence. J Oncol Pract. 2015. January;11(1):19. [DOI] [PubMed] [Google Scholar]
- 8.Mead H, Pratt-Chapman M, Gianattasio K, Cleary S, Gerstein M. Identifying models of cancer survivorship care. JCO. 2017;35(5):1. [Google Scholar]
- 9.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002. November 20,;288(19):2469–75. [DOI] [PubMed] [Google Scholar]
- 10.Bazzell JL, Spurlock A, McBride M. Matching the unmet needs of cancer survivors to resources using a shared care model. J Cancer Educ. 2015. June;30(2):312–8. [DOI] [PubMed] [Google Scholar]
- 11.Hortobagyi GN, American Society of Clinical Oncology. A shortage of oncologists? The American Society of Clinical Oncology workforce study. J Clin Oncol. 2007. April 20;25(12):1468–9. [DOI] [PubMed] [Google Scholar]
- 12.Yang W, Williams JH, Hogan PF, Bruinooge SS, Rodriguez GI, Kosty MP, et al. Projected supply of and demand for oncologists and radiation oncologists through 2025: an aging, better-insured population will result in shortage. J Oncol Pract. 2014. January 01;10(1):39–45. [DOI] [PubMed] [Google Scholar]
- 13.Hudson SV. Continuous primary care is central to comprehensive cancer care: are we ready to meet growing needs? J Am Board Fam Med. 2013. December 01;26(6):623–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dawes AJ, Hemmelgarn M, Nguyen DK, Sacks GD, Clayton SM, Cope JR, et al. Are primary care providers prepared to care for survivors of breast cancer in the safety net? Cancer. 2015. April 15;121(8):1249–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klabunde CN, Han PK, Earle CC, Smith T, Ayanian JZ, Lee R, et al. Physician roles in the cancer-related follow-up care of cancer survivors. Fam Med. 2013;45(7):463–74. [PMC free article] [PubMed] [Google Scholar]
- 16.Nekhlyudov L, Aziz NM, Lerro C, Virgo KS. Oncologists’ and primary care physicians’ awareness of late and long-term effects of chemotherapy: implications for care of the growing population of survivors. J Oncol Pract. 2014. March;10(2):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burke NJ, Napoles TM, Banks PJ, Orenstein FS, Luce JA, Joseph G. Survivorship Care Plan Information Needs: Perspectives of Safety-Net Breast Cancer Patients. PLoS One. 2016. December 16;11(12):e0168383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Potosky AL, Han PK, Rowland J, Klabunde CN, Smith T, Aziz N, et al. Differences between primary care physicians’ and oncologists’ knowledge, attitudes and practices regarding the care of cancer survivors. J Gen Intern Med. 2011. December 01;26(12):1403–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheung WY, Aziz N, Noone AM, Rowland JH, Potosky AL, Ayanian JZ, et al. Physician preferences and attitudes regarding different models of cancer survivorship care: a comparison of primary care providers and oncologists. J Cancer Surviv. 2013. September;7(3):343–54. [DOI] [PubMed] [Google Scholar]
- 20.Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support, J Biomed Inform [Internet].; 2009. [updated Apr; cited Jan 3, 2019]. Available from: https://refworks.proquest.com/tools/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf [Internet]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf.
- 22.https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf [Internet]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf.
- 23.Virgo KS, Lerro CC, Klabunde CN, Earle C, Ganz PA. Barriers to breast and colorectal cancer survivorship care: perceptions of primary care physicians and medical oncologists in the United States. J Clin Oncol. 2013. June 20;31(18):2322–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grunfeld E, Julian JA, Pond G, Maunsell E, Coyle D, Folkes A, et al. Evaluating survivorship care plans: results of a randomized, clinical trial of patients with breast cancer. J Clin Oncol. 2011. December 20;29(36):4755–62. [DOI] [PubMed] [Google Scholar]
- 25.O’Brien MA, Grunfeld E, Sussman J, Porter G, Mobilio MH. Views of family physicians about survivorship care plans to provide breast cancer follow-up care: exploration of results from a randomized controlled trial. Curr Oncol. 2015. August;22(4):252–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacobsen PB, DeRosa AP, Henderson TO, Mayer DK, Moskowitz CS, Paskett ED, et al. Systematic Review of the Impact of Cancer Survivorship Care Plans on Health Outcomes and Health Care Delivery. J Clin Oncol. 2018. July 10;36(20):2088–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jortberg BT, Fernald DH, Hessler DM, Dickinson LM, Wearner R, Connelly L, et al. Practice Characteristics Associated with Better Implementation of Patient Self-Management Support. J Am Board Fam Med. 2019. June 01;32(3):329–40. [DOI] [PubMed] [Google Scholar]
- 28.National Cancer Policy Forum, Board on Health Care Services, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine. No title. 2018. April 27.
- 29.Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of Cancer Incidence in the United States: Burdens Upon an Aging, Changing Nation. JCO. 2009;27(17):2758–65. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


