Antibody‐associated neurological disorders are a heterogeneous group of inflammatory diseases frequently associated with movement disorders (MDs), which can occur in isolation or combined with other signs. Specific clinical patterns and demographic features have been more frequently associated with specific antibodies, for example, neuropsychiatric symptoms and MDs in young females with N‐methyl‐d‐aspartate receptor (NMDAR) encephalitis, peripheral nerve hyperexcitability in elderly men with Contactin‐associated protein‐like 2 (CASPR2) antibodies, and psychiatric disorders in middle‐aged women with α‐amino‐3‐hydroxy‐5‐methyl‐4‐isoxazolepropionic receptor (AMPAR) antibodies among others. 1
Moreover, some immune‐mediated disorders can present with specific and well‐defined MDs (ie, faciobrachial dystonic seizures), which help to guide the diagnostic work‐up and to achieve the diagnosis. 1
However, there are also less characterized and atypical MDs associated with antibody‐related diseases, with a considerable overlap between clinical phenotypes and associated antibodies.
We report a case of gamma‐aminobutyric acid A (GABAA) receptor (GABAAR) encephalitis presenting with isolated atypical movement disorders as first clinical symptom.
Case Report
A 47‐year‐old woman with a past history of systemic sarcoidosis came to our attention as a result of the sudden onset of repetitive abnormal movements in the right hand, spread after 1 day to the left hand, and then in the right lip.
The neurological examination revealed quasi‐rhythmic and stereotyped abnormal movements present at rest (Video S1, segment 1) in the right and left hands, not always synchronous. The same movements were also present during posture, associated with more brief twitches in the inferior and superior right lip (Video S1, segment 2). Distraction maneuver, consisting of a mental task (recognizing which number was drawn on the forehead), did not modify the movements (Video S1, segment 3). The MDs completely resolved after steroid treatment (1 gram/day over 5 days), administered in the suspicion of an autoimmune disorder. However, after steroid dose reduction, the clinical picture became more complex (Fig. 1), with the onset of encephalopathy and refractory status epilepticus. Cerebrospinal fluid analysis revealed a mild pleocytosis and slightly elevated protein; the diagnostic work‐up for infectious diseases was negative. Brain magnetic resonance imaging showed multiple cortical‐subcortical T2/fluid‐attenuated inversion recovery hyperintensities in all cerebral lobes, with increased diffusion‐weighted imaging signal, without reduced apparent diffusion coefficient values or contrast enhancement (Fig. 1). Antibody testing, using live human embryonic kidney cells expressing α1β2γ2 subunits of the GABAAR revealed high‐titer (1,3200) serum GABAAR antibodies, confirming the diagnosis of autoimmune encephalitis. 2 Cerebrospinal fluid was not available for testing. Other antibodies (VGKC, voltage gated potassium channel; CASPR2, LGI1, leucine‐rich glioma‐inactivated 1; NMDAR, AMPAR, GAD65, glutamate decarboxylase 65; GABABR, gamma‐aminobutyric acid receptor) were negative. After rituximab therapy (375 mg/m2/weeks for 4 weeks), the patient gradually returned to her premorbid state. She remained asymptomatic at the 2‐year follow‐up.
FIG 1.
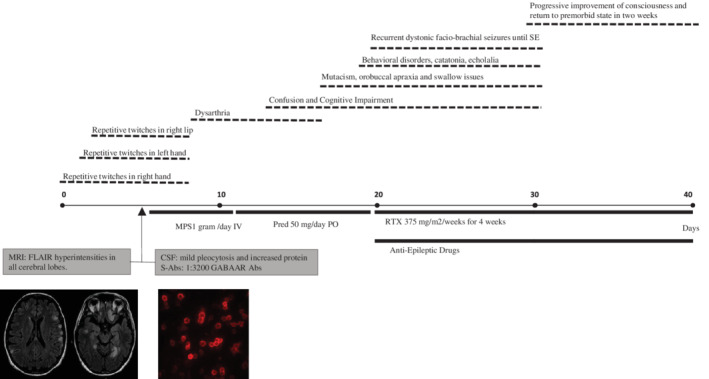
Timeline of clinical symptoms and main diagnostic exams. CSF, cerebrospinal fluid; FLAIR, fluid‐attenuated inversion recovery; GABAAR, gamma‐aminobutyric acid receptor; MPS, methylprednisolone; MRI, magnetic resonance imaging; PO, per os; Pred, prednisone; RTX, rituximab; S‐Abs, serum antibodies; SE, status epilepticus.
Discussion
The MDs in our patient could be considered atypical because of their mixed clinical features. In particular, they were too slow to be classified as “myoclonic jerks,” which are typically short and “shock‐like” involuntary movements, 3 but also too stereotyped and predictable to resemble typical choreic movements, which are irregular, nonrepetitive/rhythmic and randomly flowing.
Dystonic movements could appear as repetitive and patterned (consistent and predictable), 3 but some essential elements of dystonia were missing, such as sustained twisting posturing, antagonist gestures, and overflow. Moreover, the MD description may suggest myorhythmia, defined as repetitive, rhythmic, slow (1–4 Hz) movement affecting cranial and limb muscles, 4 mainly at rest. Nevertheless, the MDs in our case were slower, not strictly rhythmic, and persisted during posture with a mixed athetoid component. Finally, the hand movements could raise the suspicion of functional (psychogenic) movements because of the inconsistencies with classical MDs. However, they were strongly patterned, and did not change with the cognitive distraction task. 3
In a recent study, 5 the most frequent symptoms reported in GABAAR encephalitis were refractory seizures (88%) and cognitive impairment (67%). MDs were also reported, more frequently in children, including orofacial dyskinesias, dystonic postures, and generalized choreoathetosis, whereas 2 of 15 adults showed facial twitches and cramps.
Other MDs described in association with GABAAR encephalitis were ataxia or chorea as part of an encephalopathic syndrome with epilepsy. Stiff person spectrum disorders have been also reported, especially in patients with low‐titer GABAAR antibodies or partly co‐occurring with anti‐GAD65 antibodies. 1 However, because of the few cases reported and the lack of expert‐based gold standard description, the spectrum of MDs in GABAAR encephalitis is not fully defined.
Our case is peculiar because of the isolated and atypical MDs as first manifestation of disease, without any sign of encephalopathy.
Specific MD patterns associated with more frequent antibody‐related diseases have been already fully defined, such as faciobrachial dystonic seizures in LGI1 encephalitis, persisting chorea or dyskinesias in association with decreased responsiveness in NMDAR encephalitis, or stiff person spectrum disorders with GAD65, glycine receptor, amphiphysin, or dipeptidyl‐peptidase–like protein 6 antibodies. 1 However, autoimmune MDs can be difficult to characterize using conventional MD terminology 6 because they often present with mixed and nonclassic phenomenology, as in our patient.
This case expands the spectrum of MD in GABAAR encephalitis, outlining that MDs could be an early feature of the disease.
Author Roles
(1) Research Project: A. Conception, B. Organization, C. Execution; (2) Manuscript Preparation: A. Writing of the First Draft, B. Review and Critique.
V.V.: 1A, 1B, 2A
M.P.G.: 1B, 1C, 2B
R.R.: 1B, 1C, 2B
M.G.: 1B, 1C, 2B
R.L.: 1A, 1B, 2C
Disclosures
Ethical Compliance Statement: The authors confirm that the approval of an institutional review board was not required for this work. Patient gave consent to be videoed for publication. The author confirm that they have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Funding Sources and Conflict of Interest: The authors received no financial support for the research, authorship and publication of this article. The authors declare no conflict of interest relative to the current research.
Financial Disclosures for the Previous 12 Months: V.V., M.P.G., R.R., and M.G. report no disclosures. R.L. reports personal fees from Biogen, Sanofi‐ Genzyme, Argon Healthcare s.r.l., Amicus Therapeutics s.r.l., and Alfasigma for advisory board consultancy and lecture fees from Dynamicom Education, SIMG Service, Adnkronos salute unipersonale s.r.l. and DOC Congress s.r.l. outside the submitted work.
Supporting information
Video S1. Movement disorders in patient with GABA A receptor encephalitis. Segment 1: quasi‐rhythmic and stereotyped abnormal movements at rest in the right and left hands, not always synchronous. Segment 2: abnormal movements during posture. More brief twitches in inferior and superior right lip, not always synchronous. Segment 3: distraction maneuver did not modify the movements.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Balint B, Vincent A, Meinck H‐M, Irani SR, Bhatia KP. Movement disorders with neuronal antibodies: syndromic approach, genetic parallels and pathophysiology. Brain 2018;141(1):13–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vacchiano V, Giannoccaro MP, Napolitano RP, et al. Combined brain positron emission tomography/magnetic resonance imaging in GABAA receptor encephalitis. Eur J Neurol 2019. [DOI] [PubMed] [Google Scholar]
- 3. Abdo WF, van de Warrenburg BP, Burn DJ, Quinn NP, Bloem BR. The clinical approach to movement disorders. Nat Rev Neurol 2010;6(1):29–37. [DOI] [PubMed] [Google Scholar]
- 4. Baizabal‐Carvallo JF, Cardoso F, Jankovic J. Myorhythmia: phenomenology, etiology, and treatment. Mov Disord 2015;30(2):171–179. [DOI] [PubMed] [Google Scholar]
- 5. Spatola M, Petit‐Pedrol M, Simabukuro MM, et al. Investigations in GABAA receptor antibody‐associated encephalitis. Neurology 2017;88(11):1012–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Varley JA, Webb AJS, Balint B, et al. The movement disorder associated with NMDAR antibody‐encephalitis is complex and characteristic: an expert video‐rating study. J Neurol Neurosurg Psychiatry 2019;90(6):724–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1. Movement disorders in patient with GABA A receptor encephalitis. Segment 1: quasi‐rhythmic and stereotyped abnormal movements at rest in the right and left hands, not always synchronous. Segment 2: abnormal movements during posture. More brief twitches in inferior and superior right lip, not always synchronous. Segment 3: distraction maneuver did not modify the movements.


