Abstract
We recently described silicone induced granuloma of breast implant capsule (SIGBIC) as an implant capsule illness related to intact silicone breast implants. The precursor to SIGBIC development is gel bleeding/shedding from the implant shell/interior content. Currently, although the literature widely discussed the pathogenesis of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL), the trigger point for its development is still a black-box. In this case report, we report a 46-year-old woman with SIGBIC diagnosis in her right breast and BIA-ALCL in her left breast, diagnosed with ultrasound and breast magnetic resonance. Microscopy confirmed silicone bleeding from the implant surface/ content. The imaging findings reported that SIGBIC and BIA-ALCL were similar; however, BIA-ALCL had an intracapsular collection.
Keywords: Silicone, Breast implants, Anaplastic large cell lymphoma, Seroma
Abbreviations: BIA-ALCL, breast implant associated anaplastic large cell lymphoma; BMR, breast magnetic resonance; SIGBIC, silicone induced granuloma of breast implant capsule; PDMS, polydimethylsiloxane
Introduction
For 3 years, we studied breast implant complications in a prospective observational study approved by our institutional ethics committee. Since the protocol implementation, we described a new pathology related to breast implants: silicone induced granuloma of breast implant capsule (SIGBIC). We described gel bleeding from macroscopic intact breast implants as the precursor of this disease development. We also reported that some cases of SIGBIC had the same image findings of the breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). We hypothesized that SIGBIC and BIA-ALCL should have the same trigger point. In this context, BIA-ALCL should have a more aggressive behavior due to a monoclonal stimulus of T lymphocytes with immunochemistry CD30 positive secondary to a type 2 inflammatory response.
Case report
A 46-year-old woman underwent breast augmentation surgery using a silicone implant for 6 years. She opted to a round soft cohesive gel implant, with a textured surface, Refinex TC2095315 (Refinex, Beijing—China). She noted left breast enlargement associated with local pain for 2 months (Fig. 1).
Fig. 1.
A 46-year-old woman with breast implants for 6 years with a left breast increase volume.
She went for a diagnostic ultrasound scan. The ultrasound reported a voluminous intracapsular collection inside the left silicone implant capsule, despite the integrity of the implant surface. The collection contained suspension debris inferring thick fluid content. For further investigation, a complimentary breast magnetic resonance imaging (BMRI) was performed. The left collection was drained by percutaneous aspiration, with the diagnosis of BIA-ALCL on her left breast at cytology.
She underwent surgical explantation (“en bloc” capsulectomy) of bilateral breast implants. Histopathology confirmed BIA-ALCL on her left breast and SIGBIC on her right breast. No further treatment was required. For pos operatory management, follow-up by BMRI was opted (Fig. 1, Fig. 2).
Fig. 2.
Pos operatory: 1 week after bilateral “en bloc” capsulectomy.
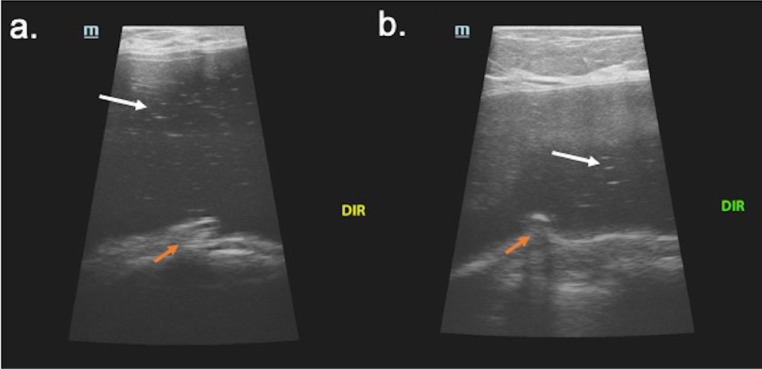
In the ultrasound scan, the right breast shows a change of interior implant texture characterized by echogenic internal lines. The images show a mass with snowstorm appearance at the posterior aspect of the implant capsule, the same findings of siliconomas in ultrasound (Fig. 3).
Fig. 3.
(a,b). Right breast ultrasound. Ultrasound scan presents heterogeneous content of breast implant (white arrow) associated with an intracapsular mass (orange arrow). The intracapsular mass shows a snowstorm artifact inferring silicone content—diagnosis of silicone induced granuloma of breast implant capsule (SIGBIC). (Color version available online.)
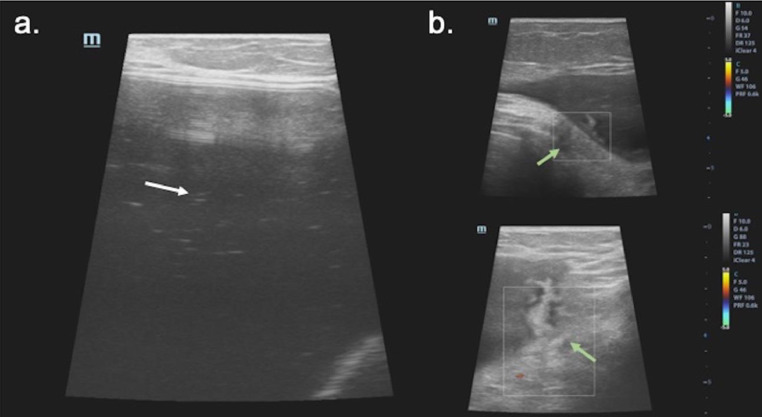
While in the left breast ultrasound scan, we also noted the change of implant texture, identical to the contralateral implant. The Doppler-flowmetry observed a vascularized mass at the inferolateral aspect of the silicone capsule. There was also an intracapsular collection associated (Fig. 4).
Fig. 4.
(a,b and c). Left breast ultrasound. Ultrasound scan presents heterogeneous content of breast implant (white arrow) associated with an intracapsular mass (green arrow). The intracapsular mass shows a snowstorm artifact inferring silicone content—diagnosis of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). (Color version available online.)
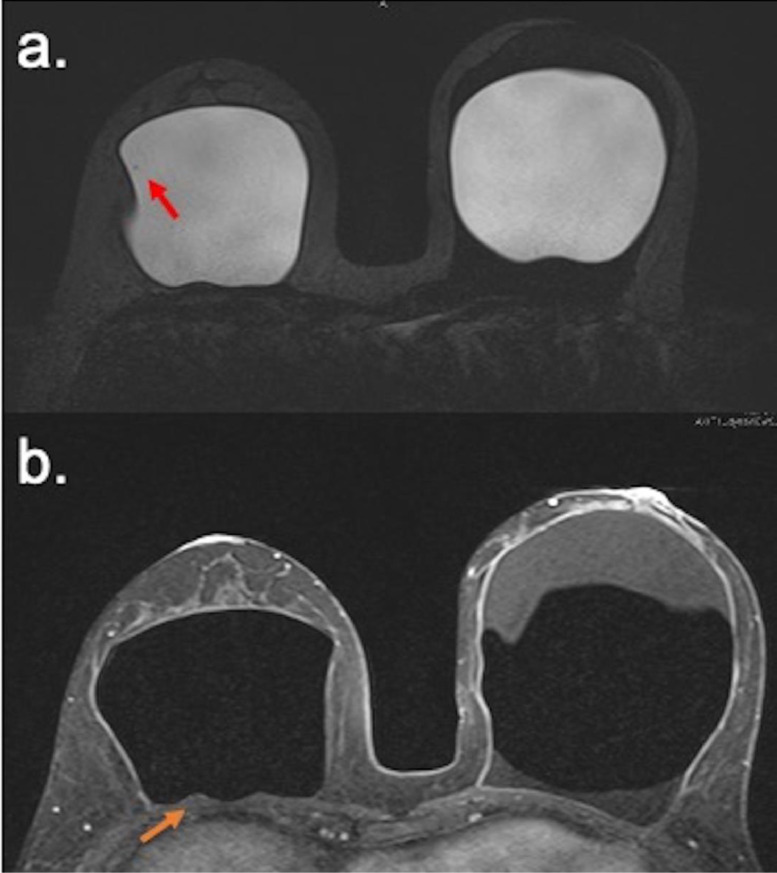
At BMRI, the right breast images show capsular contracture. The water droplet signal inside the implant explains the implant surface permeability loss. A posterior intracapsular mass with a hyper signal at T2* sequence and late contrast enhancement, associated with black-drop-signal in the implant fibrous capsule in dynamic sequences, supported the SIGBIC diagnosis. The black-drop signal is the foreign body reaction of the fibrous capsule to the free silicone particle (Fig. 5).
Fig. 5.
(a,b). Breast Magnetic Resonance. Water droplet sign in the interior of the implant of the right breast inferring permeability loss of implant surface (red arrow). (a) Intracapsular mass with black drop signal (orange arrow) compatible with SIGBIC. (b). (Color version available online.)
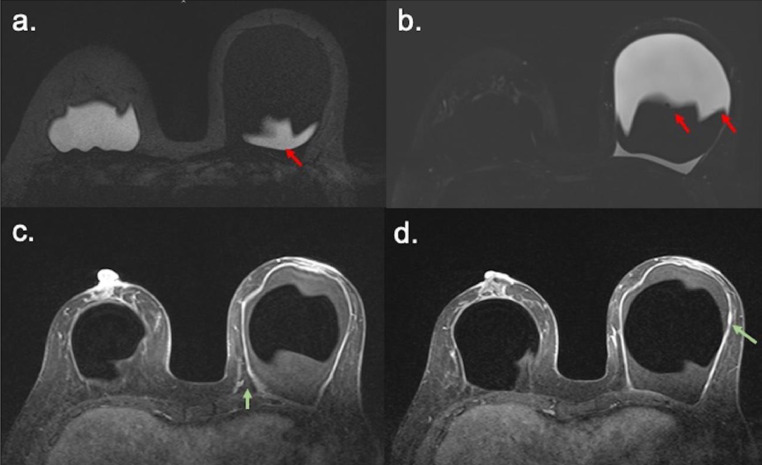
In the left breast images in BMRI. we noted a capsular contracture and implant permeability loss of the implant, as pointed out in the right breast. A hyper vascularized mass was observed at the same topography of the ultrasound finding. An extensive intracapsular collection was associated (Fig. 6).
Fig. 6.
(a,b,c and d). Breast Magnetic Resonance. Water droplet sign in the interior of the implant of the right breast inferring permeability loss of implant surface (red arrow), and silicone particles in the intracapsular collection. (a and b) Intracapsular masses with black drop signal (green arrows) compatible with BIA-ALCL. (c and d). (Color version available online.)
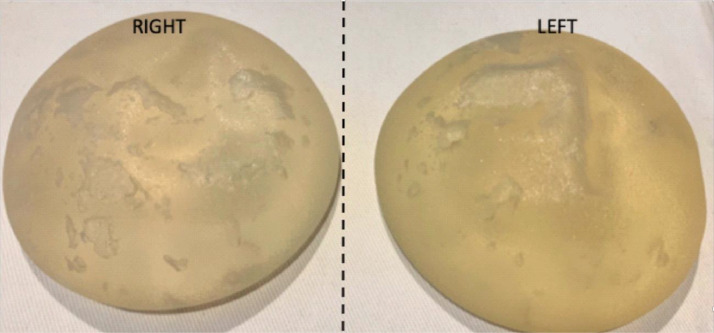
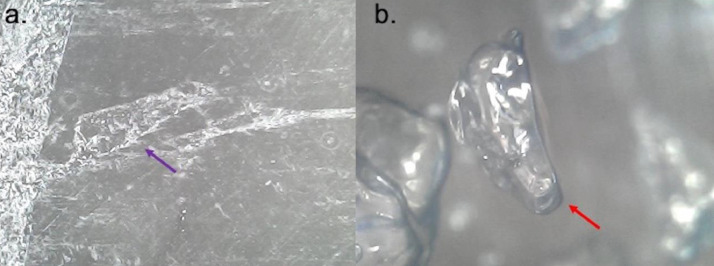
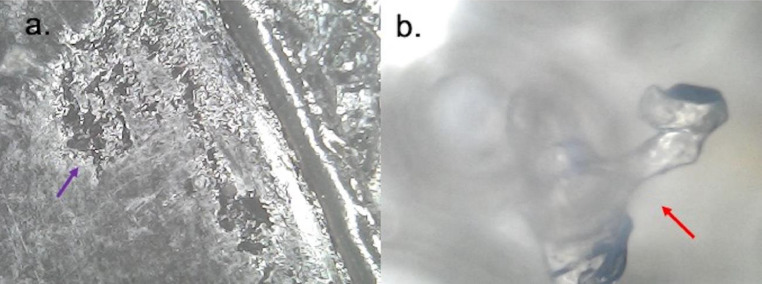
When performing the breast implant inspection, Although the macroscopic integrity of the implant's shells, a color change was observed in both implants. The changes are more evident in the left implant, where the collection was associated. We also noted a heterogeneity of the interior contents of the implant (Fig. 7). At microscopic 1.600-fold augmentation by a digital microscope (Koolerton, Hong Kong, China) of the implant shell, we observe a bilateral implant shell surface damage and changes in intracapsular content (Figs. 8 and 9).
Fig. 7.
Macroscopic view of breast implants. At macroscopy, despite implant integrity, a heterogeneous content was observed in both implants.
Fig. 8.
(a,b). 1.600-fold microscopy fold of the right implant surface. A shell degradation is seen (a) with a clear water droplet (b).
Fig. 9.
(a,b). 1.600-fold microscopy fold of the right implant surface. A shell degradation is seen (a) with a dirty water droplet (b).
In hemogram, the pre operatory hemogram shows leukopenia while the 2-day pos operatory hemogram shows normal leucocytes (Table 1).
Table 1.
Pre and pos operatory hemogram.
| Hemogram | Pre operatory | POS operatory | Reference |
|---|---|---|---|
| Erythogram | |||
| Red blood cells (RBC) | 4.12 | 4.09 | 4.0-5.2 |
| Hematocrit | 38.6 | 36.8 | 36.0-46.0 |
| Hemoglobin concentration | 12.6 | 13.2 | 11.0-15.0 |
| Leukogram | |||
| Leukocytes | 2.900 | 5.780 | 5.000-10.000 |
| Thrombogram | |||
| Platelet | 191.000 | 370.000 | 150.000-450.000 |
Discussion
BIA-ALCL has been widely discussed since the reports of the first cases related to textured silicone implants. However, the trigger point of this pathology is still unknown [1]. Since we started a research protocol in our institution to search for breast implant complications, we observed an increasing number of SIGBIC cases. We speculated whether SIGBIC and BIA-ALCL could have the same origin [2,3]. We also noted that many patients with SIGBIC diagnosis have the same clinical complaints of that reported by patients with breast implant illness (BII), a disease reported in social media by women with common clinical complaints.
We described that the silicone particles could elicit an immunological reaction in the fibrous capsule, and this reaction could vary in aggressiveness. We hypothesized that silicone bleeding could be the common trigger point to develop BII, which could range from more indolent as SIGBIC to more aggressive as BIA-ALCL [4].
We also described 3 novelty findings for SIGBIC diagnosis at BMRI: hyper signal mass at T2** sequence, black-drop signal, and late contrast enhancement. The definition of these findings was reported in a previous publication [5]. Other ultrasound features were described by our group as echogenic internal lines inside the implant and macroscopic color changes related to silicone shell permeability loss [6].
Another novelty ultrasound finding that is first reported in this article is the snowstorm pattern of the intracapsular mass. As the mass has silicone content, we found attenuation of the echo giving the aspect of a dirty posterior aspect. These findings have a correspondence to the intracapsular mass reported in BMRI.
In a recent review, Sharma et al. described the multiparametric imaging paradigms in BIA-ALCL diagnosis. They ignored gel bleeding as a precursor of the disease. They also state the disease has peri-implant effusion and pericapsular mass as the 2 distinct clinicopathologic subtypes. And the use of the term seroma is not accurate for this condition, as it implies acellular serous fluid, unlike the high cellularity cytologic found in these cases [7]. This is why we opted to use collection to describe the intracapsular content.
On the other hand, our latest publication described the BMRI sensitivity to detect silicone bleeding. We concluded that when adopting the 3 diagnostic criteria: black-drop signal, mass with a hyper signal in T2** sequences, and late contrast enhancement, the BMRI correctly diagnoses silicone gel bleeding in all cases [8].
This case report reports our first patient with a synchronic BIA-ALCL and SIGBIC in the same patient. Although both implants have the same imaging and macroscopy changes, BIA-ALCL was diagnosed at her left breast and SIGBIC at her right breast. We speculate that this different evolution is related to local immune reactions to silicone particles.
As an inflammatory process, we recommend our patients when these findings are present in our diagnostic scans to avoid biopsy during the acute phase. We note that patients who underwent biopsy tend to have a poor progression of the inflammatory reaction, with local extracapsular complications like edema and fluid collection. We manage these patients with anti-inflammatory therapy with the nonsteroidal anti-inflammatory drug or corticosteroid therapy and schedule an “en-bloc” capsulectomy.
It is worthy of mentioning that during the disease process, the patient developed leukopenia in hemogram. We speculate the leukopenia is derived from an intracapsular consumption of T-lymphocytes. The high consumption may recruit younger/ immatures lymphocytes. This is another novelty information of this case report since most lymphomas were associated with leukocytosis rather than leukopenia.
In conclusion, gel bleeding should be discussed as the trigger point to develop BII. SIGBIC and BIA-ALCL could be different diseases progression of the same pathology.
Ethics approval and informed consent
Waived due the type of manuscript
Consent for publication
Informed consent was obtained from the patient.
Funding
There is no funding support.
Footnotes
Competing interest: The author declares there is no external funding for this publication.
References
- 1.Groth K, Graf R. Breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) and the textured breast implant crisis. Aesth Plastic Surg. 2019;17 doi: 10.1007/s00266-019-01521-3. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Castro C, Fernandes D, Mendonça M, Roveda Junior D, Badan G, Fleury EFCF. Silicone-induced granuloma of breast implant capsule mimicking anaplastic large cell lymphoma. Breast J. 2019;28 doi: 10.1111/tbj.13666. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Fenili P, Marins S, Tavares R. What is different between the silicone-induced granuloma of breast implant capsule (SIGBIC) and anaplastic large cell lymphoma (ALCL)? EPOS. 2019 doi: 10.26044/ecr2019/C-2292. [DOI] [Google Scholar]
- 4.De Faria E, Fleury C, Alessandro GSD, Cristina S, Wludarski L. Silicone-induced granuloma of breast implant capsule (SIGBIC): histopathology and radiological correlation. J Immunol Res. 2018;20 doi: 10.1155/2018/6784971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Faria Castro Fleury E, Gianini AC, Ayres V, Ramalho LC, Seleti RO, Roveda D., Jr. Breast magnetic resonance imaging: tips for the diagnosis of silicone-induced granuloma of a breast implant capsule (SIGBIC) Insights Imaging. 2017;8(4):439–446. doi: 10.1007/s13244-017-0564-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Faria Castro Fleury E. Clear to cloudy II: radiological perspective of silicone breast implants. Eur J Plast Surg. 2020 doi: 10.1007/s00238-019-01612-z. [DOI] [Google Scholar]
- 7.Sharma B, Jungersen-Rauch A, Pace E, Attygale AD. Breast implant-associated anaplastic large cell lymphoma: review and multiparametric imaging paradigms. Radiographics. 2020;40(3):609–628. doi: 10.1148/rg.2020190198. [DOI] [PubMed] [Google Scholar]
- 8.Fleury EdFC Silicone induced granuloma of breast implant capsule (SIGBIC) diagnosis: breast magnetic resonance (BMR) sensitivity to detect silicone bleeding. PLOS ONE. 2020;15(6) doi: 10.1371/journal.pone.0235050. [DOI] [PMC free article] [PubMed] [Google Scholar]