Abstract
The outbreak of the coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is thought to have occurred first in Wuhan, China in December 2019, before spreading to over 120 countries in the months that followed. It was declared a “public health emergency of international concern” by the World Health Organization on January 31, 2020 and recognized as a pandemic on March 11, 2020. The primary route of SARS-CoV-2 transmission from human to human is through inhalation of respiratory droplets. Devising protective technologies for stopping the spread of the droplets of aerosol containing the viral particles is a vital requirement to curb the ongoing outbreak. However, the current generations of protective respirator masks in use are noted for their imperfect design and there is a need to develop their more advanced analogues, with higher blockage efficiency and the ability to deactivate the trapped bacteria and viruses. It is likely that one such design will be inspired by nanotechnologies. Here we describe a new design from Egypt, utilizing a reusable, recyclable, customizable, antimicrobial and antiviral respirator facial mask feasible for mass production. The novel design is based on the filtration system composed of a nanofibrous matrix of polylactic acid and cellulose acetate containing copper oxide nanoparticles and graphene oxide nanosheets and produced using the electrospinning technique. Simultaneously, the flat pattern fabricated from a thermoplastic composite material is used to provide a solid fit with the facial anatomy. This design illustrates an effort made in a developing setting to provide innovative solutions for combating the SARS-CoV-2 pandemic of potentially global significance.
Keywords: Polylactic acid, Cellulose acetate, Nanofiber, COVID-19, Face mask
The outbreak of the SARS-CoV-2 virus began as “pneumonia of an unknown origin” diagnosed in people visiting or congregating at the Huanan Seafood Wholesale Market in Wuhan, China [1]. The Chinese authorities confirmed a cluster of infected individuals on December 31, 2019, although the true source of the virus is being intensely debated on, given the reports of detection of SARS-CoV-2 in patients predating the Wuhan cluster [2]. Soon after the disease outbreak was registered and its probable source pinpointed, these cases were identified as a novel coronavirus by the Chinese health authorities and named SARS-CoV-2 by the World Health Organization (WHO) [1]. Only a few months after the Wuhan outbreak, the virus spread to over 120 countries of the world [[3], [4], [5]]. Based on the WHO statistics, the total confirmed cases worldwide reached 2,397,216 on April 21, 2020, while the total deaths globally by the same date were 162,956 [6]. At the same time, the number of confirmed cases in Egypt was 3333, while the number of deaths was 250 [6]. The exponential trend of the virus outbreak has already had devastating socioeconomic consequences and their real extent is difficult to foresee at this time.
SARS-CoV-2 is relatively sensitive to heat; it could be deactivated after incubation at 56 °C for 30 min or by the application of disinfectants, such as the hard ultraviolet radiation of wavelengths in the 280–100 nm range, ideally λ = 250 nm [7], ethanol (>75%), ether, peroxyacetic acid, 0.05–0.1% sodium hypochlorite, chloroform and other lipid solvents with the exception of chlorhexidine [8]. However, the spread of SARS-CoV-2 between humans is supposed to be primarily airborne, occurring most intensely when the infected person is talking, sneezing or coughing, with the resulting droplets of aerosol containing the virus being carried to the distance of 3–8 m [8]. SARS-CoV-2 has the incubation period of 1–14 days before the beginning of the symptoms [9], during which the patient is infectious [9]. Patients who are displaying respiratory symptoms are potentially harmful to their close contacts because the virus could be launched from the upper respiratory tract and released explosively into the air during coughing [8,10]. Naturally, healthcare workers, who are most exposed to these aerosol droplets of the viral agent, are most likely to contract the infection [8]. Given their increased exposure and risk of infection with SARS-CoV-2, protecting the healthcare workers within the framework of the occupational and safety regulations provides a vital means of protection of the general population. This protection must be associated with the risk assessment procedures and specific preventive measures that include health surveillance of the workers and the mandatory use of effective personal protective equipment (PPE) [11]. Protecting healthcare workers is a priority, yet the lack of awareness and training, the shortage of PPE, and the lack of point-of-care diagnostic tests for healthcare workers are important factors contributing to the spread of the infection in healthcare settings [12].
Simply, since it is known that SARS-CoV-2 spreads through air, stopping the spread of the aerosol droplets carrying the virus through coughing, sneezing or speaking is a vital requirement to inhibit the ongoing outbreak [10]. Devising protective technologies for blocking the path of the droplets of aerosol containing the viral particles toward the respiratory systems of individuals is a major strategy along this line of efforts [10]. China, for example, produces around 20 million face masks per day, which represents around 50 % of the world production. However, even if the Chinese productivity were to be in full capacity, it would not satisfy the population needs, which is around 1.4 billion in China alone under the universal face mask wearing policy [13]. Moreover, due to the slowdown of the global transportation, each country should start manufacturing its own protective equipment using local resources. Consequently, to avoid the risks of infection transmission to the health worker teams, precautions should be taken to prevent the nosocomial spread of this virus and appropriate, highly effective face masks should be worn during the communication with the suspected or diagnosed patients [14].
Concerning this vulnerability of the first line of defense within the healthcare system, with the fast spread of SARS-COV-2 virus in China, around 1700 health care workers have been infected so far. Furthermore, by the time the number of the patients reached 425, around 15 of the healthcare workers had already died from the infection [8]. Furthermore, already on April 16, 2020, 16,991 of healthcare workers were confirmed positive for SARS-CoV-2 in Italy [15]. Similarly, 11.6% of the 6800 workers of the public Hospital Universitario 12 de Octubre in southern Madrid, which is responsible for serving the population of 400,000, were reported positive for SARS-CoV-2 on March 29, 2020, only 20 days after the first infected healthcare worker in it was confirmed [16]. Therefore, to prevent the spread of the contagions, strict precautions should be implemented, include wearing protective masks, respirator face masks (N95 or N99), disposable head caps, protective eye glasses (anti-fog), face shields, work clothes (white coats), disposable latex gloves, and disposable shoes [8]. These standard precautions could be classified as Grade III, and they are necessary for people who directly deal with positive cases. These precautions could be lessened for hospital workers with a lesser contact, but even then, the protective respirator face masks are normally mandatory to wear. Regarding the common citizens, covering the face with the use of a respirator face mask could prevent droplets from getting through the air and infecting oneself or other people so long as the limitations with respect to their use are overcome. For example, respiratory face masks such as N95 are not suitable for individuals with obesity, cardiovascular conditions or various respiratory problems; secondly, the limited number of produced N95 masks makes it a priority to provide them for the healthcare workers first and foremost. Therefore, providing healthcare workers with appropriate respirator face masks is a critical strategy for inhibiting the spread of the virus between individuals, whereas their use in the general population is secondary to this goal. The N95 is a respiratory protective device designed to filtrate airborne particles with a close facial fit, blocking in reality the passage of around 95 % of particles (≥0.3 μm) [8]. However, it has been estimated that the inhalation of 1–3 viral particles of SARS-COV-2 may be sufficient to cause the infection, especially in the vulnerable population, one reason for this susceptibility being the literal novelty of this virus for the human immune systems. Despite the greater efficacy in preventing the transmission of the particles of N95 respirators compared to the surgical masks, N95 provides for an imperfect barrier, partly because of the incomplete fit between the respirator and the face and partly because of the intrinsic permeability to a small percentage of the airborne particulates. Moreover, N95 is a single-use, expensive, environmentally polluting device that can reduce the lung capacity due to its low customization [17]. Therefore, a new design of respirator face masks should be reusable, recyclable, customizable, modular and facile for mass production, alongside being upgradable with antimicrobial and antiviral respirators.
Nanotechnologies emerged in the 20th century as the most prospective approach to impart superior novel properties to materials for a variety of applications, including the medical [18]. Electrospinning is an experimental technique readily usable for producing nanofiber membranes with adjustable properties, including the fiber diameters, porosity ratio and other microstructural parameters [[19], [20], [21], [22]]. As of April 2020, we have engaged in the design of protective respirator masks with the aforementioned advanced properties to help in combating the SARS-CoV-2 infection spread in Egypt and globally. The regulatory approvals are underway and the production is foreseen to commence in early May. The fabrication of the filters and the printing of the mask prototype have been completed and the final fund approvals are currently anticipated to initiate the mask production. In what follows, we will describe the rationale and the specifics of this design.
In our earlier work, we used nanoparticle-reinforced polymeric composites to fabricate tissue engineering constructs via electrospinning [23,24]. Polylactic acid (PLA) which we used is a biodegradable and transparent polymer with high elastic modulus, and it could be derived from starch and other carbohydrates [25]. Electrospun PLA membranes have shown prospect as filters for isolating environmental pollutants, including the atmospheric aerosol and submicron particulates dispersed in air [26], but research on them for this application has been merely sporadic. Although PLA was used for different biomedical applications, such as implant prostheses, tissue scaffolds, catheters and packaging materials owing to its biocompatibility [27], it displays numerous mechanical drawbacks, one of which is its intrinsic brittleness, meaning that repeated pressure during handling can induce cracks and make PLA masks prone to becoming permeable to the viral particles. These brittle features of PLA, however, could be overcome by modification with reinforcement fillers, such as metallic nanoparticles [27]. These nanoparticles introduce dual mechanical/biological functionality into the polymeric nanofibers: they provide the material with ductility and higher yield strength, and also add their antibacterial and antiviral activities to it.
Among such nanoparticles, copper oxide nanoparticles (CuONPs) possess a narrow bandgap and have been utilized for biomedical applications such as infection control [28]. They owe their use in these applications to the ability to inhibit the growth of fungi, bacteria and viruses [29,30]. Furthermore, it was reported that SARS-CoV-2 has a lower stability on the surface of metallic copper compared to that on other materials, such as plastic or stainless steel [31]. The modification of a nanofibrous polymeric filtration system with CuONPs would lead to a significant enhancement in the antifouling properties, which may prevent the pathogenic microbes from adhering onto the membrane [32]. A similar effect is expected to be achieved by another reinforcing component of the composite membranes, namely graphene oxide (GO) [19]. GO is a single layer of two-dimensional carbon atoms, which crystallize in a honeycomb lattice [33]. GO displays excellent mechanical properties, including high toughness, but also high electrical conductivity alongside biocompatibility and an antibacterial activity [34]. Most promisingly, it demonstrated an antiviral activity against another coronavirus, porcine epidemic diarrhea virus, when used as a minor component of a composite material [35]. The fourth and the final component of the membrane comes in the form of cellulose acetate (CA), a semisynthetic polymer derived from cellulose. CA was used earlier for ultrafiltration owing to its biocompatibility, low cost and high selectivity [22,36]. It has also been used in protective clothing, tissue engineering, and reinforced nanocomposite applications [37].
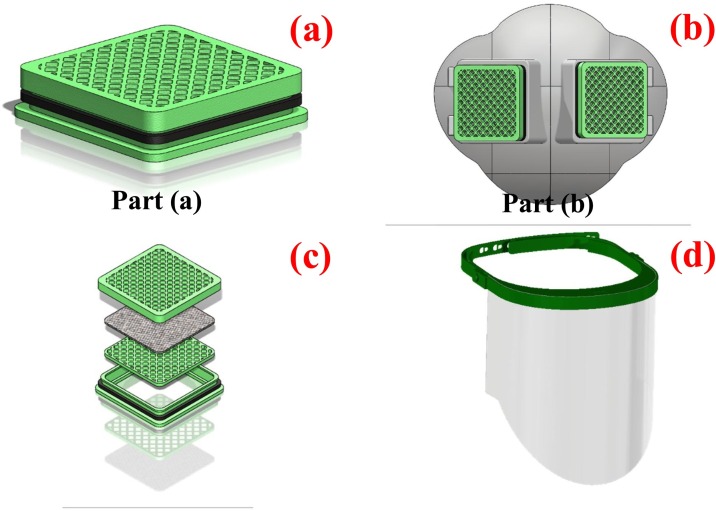
Therefore, the design of the novel respirator filter mask against SARS-CoV-2 is based on electrospun multilayers of PLA and CA embedding CuONPs and GO with the assistance of high-power ultrasonication. While the polymeric network could stop the airborne viral particles in their flight, the nanoparticles of CuO and GO would further inhibit the bacterial and viral transmission by inactivating the viral particles caught in the membrane itself. Combining the ideas mentioned above, the first step in the production came in the form of a prototype for a customizable/multi-used protective respirator mask containing molten PLA as a fixed part, and multilayers of CA/PLA nanofibers doped with CuONPs and GO as the disposable part. A schematic describing this prototype is shown in Fig.1 .
Fig. 1.
Schematic representation of the design of the nanofibrous respirator face mask. Part (a) depicts the respirator filter containing multilayers of CuONPs/GO@PLA and CuONPs/GO@CA nanofibers. Part (b) represents the fixed part of the face mask. The assembly of the multilayers consisting of nanofibers into a respirator filter is shown in (c). The face shield containing two parts and fabricated via the molding procedure is shown in (d).
Based on the illustration of the prototype, the respirator face mask consists of two main parts: (a) and (b). The part (a) refers to the disposable filter piece composed of the unwoven nanofibers, each comprising multilayers of CuONPs/GO@PLA and CuONPs/GO@CA. The part (b) denotes the fixed piece produced using a molten template obtained from a 3D pointing technique based on heating PLA to 160–180 °C and cooling gradually. Making use of the glass transition temperature of PLA at around 55 °C, the submersion of the face mask into a hot water bath at 55–60 °C is used to increase its malleability and allow for the better fit with the human face anatomy. While the part (a) of the face mask is disposable, the part (b) is washable with water and could be sterilized using an UV lamp (λ = 250 nm) and exposures of under 30 min. The recyclability of the respirator face masks implies the possibility for the reuse of some of its parts by melting and repurposing for different polymeric devices and applications.
The cost-benefit analysis first took into account the manufacture of both templates for the parts (a) and (b), with the cost of around $5500 and $7000, respectively. Briefly, it might be expected that each template could undergo 150,000–200,000 shots before deterioration, meaning that the contribution of each template to the produced filter cost is around ¢7. Considering the local market prices, the cost of PLA and CA is $80/kg and $50/kg, respectively. With the part (b) consuming 12 g of PLA per piece, the PLA cost is approximately $1, and it is the highest of all the material contributions to the fabrication cost. Then, with the part (a) consuming around 0.25 g of CA, its contribution to the cost is ¢1.3. At the same time, the contributions of CuONPs and GO are around 5 g of each per 1000 pieces of the part (a), and their cost does not exceed ¢7 for each filter piece. Considering all of this, the total cost for the production of the face mask, including both the reagents and the templates, is around $1.15 per piece at the most. In addition to the cost of renting the production equipment, the devices for testing and workers, the cost of a respirator face mask will not exceed $1.88, which is lower than the currently offered alternatives on the market. The synthesis of both CuONPs and GO from the elementary atomic ingredients using ultrasonic-assisted wet chemistry and modified Hummers’ method [34,38], respectively, lowers the cost of the overall process and increases its translatability across different laboratory settings.
All these positive strides notwithstanding, the conditions for the safe application of any medical devices, including this one, must be ensured from the production end, for which rigorous safety and efficacy studies are necessary. Possible limitations emerging from such studies may include the finite dissipation of the CuONPs and GO with prolonged use as well as inadequate porosity of the nanofibrous component for the favorable balance between unconstrained respiration and the blocking of the viral particles. Such concerns necessitate a rational design of the materials properties and require a solid expertise in the materials design. As ever, fundamental scientific knowledge emerges as the foundation of superbly performing technologies.
The method for the fabrication of all the components and the composite membranes will be publicly available and free assistance is provided to any research or clinical teams interested in replicating the process. We believe that the scientific community must come together in a collective effort to curb the spread of this disease. Materials scientists, like us, should step forth with their expertise and ideas in these challenging times to help save lives. In doing so, it is of crucial importance to think innovatively and not fall in the trap of mimicking the methods of production and approaches implemented by the developed world, without learning from their fallacies and thinking ahead of them [39]. It is also worth adding that the world has never been connected as it is now and any lessons learned from efforts made in one part of the world can be meaningful for planning similar efforts in other parts of it. Therefore, we believe that these lessons from Egypt can be of global significance for putting an end to this unexpected pandemic and becoming better prepared for the possible new ones.
References
- 1.Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deslandes A., Berti V., Tandjaoui-Lambotte Y., Alloui C., Carbonnelle E., Zahar J.R. SARS-CoV-2 was already spreading in France in late December 2019. Int J Antimicrob Agents. 2020 doi: 10.1016/j.ijantimicag.2020.106006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Achard V., Tsoutsou P., Zilli T. Radiotherapy in the time of the Coronavirus pandemic: when less is better. Int J Radiat Oncol Biol Phys. 2020;107:600–601. doi: 10.1016/j.ijrobp.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang T., Wu Q., Zhang Z. Probable pangolin origin of SARS-CoV-2 associated with the COVID-19 outbreak. Curr Biol. 2020;30:1346–1351. doi: 10.1016/j.cub.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang L., Zhu F., Xie L., Wang C., Wang J., Chen R. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020;31:894–901. doi: 10.1016/j.annonc.2020.03.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . World Health Organization; 2020. Coronavirus disease 2019 (COVID-19) situation report – 92.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200421-sitrep-92-covid-19.pdf?sfvrsn=38e6b06d_4: [Google Scholar]
- 7.Seyer A., Sanlidag T. Solar ultraviolet radiation sensitivity of SARS-CoV-2. Lancet Microbe. 2020;1:e8–e9. doi: 10.1016/S2666-5247(20)30013-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu K., Lai X., Zheng L. Suggestions on the prevention of COVID-19 for health care workers in department of otorhinolaryngology head and neck surgery. World J Otorhinolaryngol Head Neck Surg. 2020 doi: 10.1016/j.wjorl.2020.03.002. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zheng S.-Q., Yang L., Zhou P.-X., Li H.-B., Liu F., Zhao R.-S. Recommendations and guidance for providing pharmaceutical care services during COVID-19 pandemic: a China perspective. Res Soc Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.03.012. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang R., Gui X., Xiong Y. Patients with respiratory symptoms are at greater risk of COVID-19 transmission. Respir Med. 2020;165 doi: 10.1016/j.rmed.2020.105935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chirico F., Magnavita N. COVID-19 infection in Italy: an occupational injury. South Afr Med J. 2020;110:1. [PubMed] [Google Scholar]
- 12.Chirico F., G. Nucera, Magnavita N. COVID-19: protecting healthcare workers is a priority. Infect Control Hosp Epidemiol. 2020;1:1. doi: 10.1017/ice.2020.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu H.-L., Huang J., Zhang C.J.P., He Z., Ming W.-K. Facemask shortage and the novel coronavirus disease (COVID-19) outbreak: reflections on public health measures. EClinicalMedicine. 2020 doi: 10.1016/j.eclinm.2020.100329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao S., Ling K., Yan H., Zhong L., Peng X., Yao S. Anesthetic management of patients with suspected or confirmed 2019 novel coronavirus infection during emergency procedures. J Cardiothorac Vasc Anesth. 2020;34:1125–1131. doi: 10.1053/j.jvca.2020.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lapolla P., A. Mingoli, R. Lee Deaths from COVID-19 in healthcare workers in Italy—what can we learn? Infect Control Hosp Epidemiol. 2020;1:1. doi: 10.1017/ice.2020.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Folgueira M.D., Munoz-Ruiperez C., Alonso-Lopez M.A., Delgado R. medRxiv; 2020. SARS-CoV-2 infection in health care workers in a large public hospital in Madrid, Spain, during March 2020. [DOI] [Google Scholar]
- 17.Fillingham Y.A., Grosso M.J., Yates A.J., Austin M.S. Personal protective equipment: current best practices for orthopedic teams. J Arthroplasty. 2020;35:S19–S22. doi: 10.1016/j.arth.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uskoković V. Entering the era of nanoscience: time to be so small. J Biomed Nanotechnol. 2013;9:1441–1470. doi: 10.1166/jbn.2013.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Wafi R., Mansour S.F., Ahmed M.K. Mechanical, microstructural properties and cell adhesion of Sr/Se-hydroxyapatite/graphene/polycaprolactone nanofibers. J Thermoplast Compos Mater. 2020 089270572091278. [Google Scholar]
- 20.Ahmed M.K., Ramadan R., Afifi M., Menazea A.A. Au-doped carbonated hydroxyapatite sputtered on alumina scaffolds via pulsed laser deposition for biomedical applications. J Mater Res Technol. 2020;9:8854–8866. [Google Scholar]
- 21.Ahmed M.K., Ramadan R., El-dek S.I., Uskoković V. Complex relationship between alumina and selenium-doped carbonated hydroxyapatite as the ceramic additives to electrospun polycaprolactone scaffolds for tissue engineering applications. J Alloys Compd. 2019;801:70–81. [Google Scholar]
- 22.Ahmed M.K., Mansour S.F., Al-Wafi R., El-dek S.I., Uskoković V. Tuning the mechanical, microstructural, and cell adhesion properties of electrospun ε-polycaprolactone microfibers by doping selenium-containing carbonated hydroxyapatite as a reinforcing agent with magnesium ions. J Mater Sci. 2019;54:14524–14544. [Google Scholar]
- 23.Menazea A.A., Abdelbadie S.A., Ahmed M.K. Manipulation of AgNPs coated on selenium/carbonated hydroxyapatite/ε-polycaprolactone nano-fibrous via pulsed laser deposition for wound healing applications. Appl Surf Sci. 2020;508 [Google Scholar]
- 24.Mansour S.F., Al-Wafi R., Ahmed M.K., Wageh S. Microstructural, morphological behavior and removal of Cr(VI) and Se(IV) from aqueous solutions by magnetite nanoparticles/PVA and cellulose acetate nanofibers. Appl Phys A. 2020;126 [Google Scholar]
- 25.Wang G., Zhang D., Li B., Wan G., Zhao G., Zhang A. Strong and thermal-resistance glass fiber-reinforced polylactic acid (PLA) composites enabled by heat treatment. Int J Biol Macromol. 2019;129:448–459. doi: 10.1016/j.ijbiomac.2019.02.020. [DOI] [PubMed] [Google Scholar]
- 26.Li J., Shi X., Gao F., Liu L., Chen R., Chen C. Filtration of fine particles in atmospheric aerosol with electrospinning nanofibers and its size distribution. Sci China Ser E Technol Sci. 2014;57:239–243. [Google Scholar]
- 27.Sudamrao Getme A., Patel B.A. Review: bio-fiber’s as reinforcement in composites of polylactic acid (PLA) Mater Today Proc. 2020 doi: 10.1016/j.matpr.2020.02.457. [DOI] [Google Scholar]
- 28.Alayande A.B., Obaid M., Kim I.S. Antimicrobial mechanism of reduced graphene oxide-copper oxide (rGO-CuO) nanocomposite films: the case of Pseudomonas aeruginosa PAO1. Mater Sci Eng C. 2020;109 doi: 10.1016/j.msec.2019.110596. [DOI] [PubMed] [Google Scholar]
- 29.Varaprasad K., López M., Núñez D., Jayaramudu T., Sadiku E.R., Karthikeyan C. Antibiotic copper oxide-curcumin nanomaterials for antibacterial applications. J Mol Liq. 2020;300 [Google Scholar]
- 30.Chang Q., Xu W., Li N., Xue C., Wang Y., Li Y. Dynamic restructuring of carbon dots/copper oxide supported on mesoporous hydroxyapatite brings exceptional catalytic activity in the reduction of 4-nitrophenol. Appl Catal B. 2020;263 [Google Scholar]
- 31.Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:3. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sri Abirami Saraswathi M.S., Rana D., Divya K., Gowrishankar S., Nagendran A. Versatility of hydrophilic and antifouling PVDF ultrafiltration membranes tailored with polyhexanide coated copper oxide nanoparticles. Polym Test. 2020;84 [Google Scholar]
- 33.Ahmed M.K., Mansour S.F., Al-Wafi R. Nanofibrous scaffolds of epsilon-polycaprolactone containing Sr/Se-hydroxyapatite/ graphene oxide for tissue engineering applications. Biomed Mater. 2020 doi: 10.1088/1748-605X/ab7ff5. In press. [DOI] [PubMed] [Google Scholar]
- 34.Xie Y.Y., Hu X.H., Zhang Y.W., Wahid F., Chu L.Q., Jia S.R. Development and antibacterial activities of bacterial cellulose/graphene oxide-CuO nanocomposite films. Carbohydr Polym. 2020;229 doi: 10.1016/j.carbpol.2019.115456. [DOI] [PubMed] [Google Scholar]
- 35.Ye S., Shao K., Li Z., Guo N., Zuo Y., Li Q. Antiviral activity of graphene oxide: how sharp edged structure and charge matter. ACS Appl Mater Interfaces. 2015;7:21571–21579. doi: 10.1021/acsami.5b06876. [DOI] [PubMed] [Google Scholar]
- 36.Yang S., Wang T., Tang R., Yan Q., Tian W., Zhang L. Enhanced permeability, mechanical and antibacterial properties of cellulose acetate ultrafiltration membranes incorporated with lignocellulose nanofibrils. Int J Biol Macromol. 2020;151:159–167. doi: 10.1016/j.ijbiomac.2020.02.124. [DOI] [PubMed] [Google Scholar]
- 37.Wang D., Yue Y., Wang Q., Cheng W., Han G. Preparation of cellulose acetate-polyacrylonitrile composite nanofibers by multi-fluid mixing electrospinning method: morphology, wettability, and mechanical properties. Appl Surf Sci. 2020;510 [Google Scholar]
- 38.Zou R., Xu T., Lei X., Wu Q., Xue S. Novel design of porous hollow hydroxyapatite microspheres decorated by reduced graphene oxides with superior photocatalytic performance for tetracycline removal. Solid State Sci. 2020;99 [Google Scholar]
- 39.Uskoković V., Ševkušić M., Uskoković D. Strategies for the scientific progress of the developing countries in the new millennium. Sci Technol Innov Stud. 2010;6:33–62. [Google Scholar]