Air pollution is a main public health (The Lancet 2017) and economic (Dockery and Evans 2017) issue. Air pollution increases the risk of mortality (Dockery and Evans 2017) and morbidity from a wide range of diseases (especially respiratory, cardiovascular and cardiorespiratory diseases) (Shah et al. 2013; Brugha and Grigg 2014; Loxham et al. 2019). Moreover, it is now well established that maternal exposure to air pollution increases the risk of developing an autism spectrum disorder (ASD) in newborns (Kerin et al. 2018; Chun et al. 2020; Dutheil et al. 2020), with a dose–response relationship (McGuinn et al. 2020). ASD is a challenging pathology with actual global increase of the prevalence (Masi et al. 2017; Kogan et al. 2018), putatively linked with the increase in air pollution. Considering that there are more than 200 million of pregnancy per year (“WHO Chapter 3” n.d.), there is a huge challenge to limit air pollution during pregnancy. The global Coronavirus Covid19 outbreak reduced dramatically the air pollution such as NO2 or fine particulates especially in China (Chen et al. 2020) (Fig. 1). Because of quarantine measures to stop the spread of the virus, people are confined at home, factories activity is slowed down or even stopped in regions the most affected by the virus, transports and commerce have slowed down. This economic slowdown leads to a concomitant consequent decrease of air pollution, first near Wuhan, Hubei Province in China, the initial infection site, then in the whole China (Le et al. 2020), then worldwide (Berman et al. 2020; Nakada et al. 2020; Stivastava et al. 2020; Zambrano-Monserrate et al. 2020). This coronavirus had been responsible for a massive decrease up to 90% of NO2 during the city-lockdown period in Wuhan, 40–60% for China (Le et al. 2020) and worldwide megalopolis (Berman et al. 2020; Nakada et al. 2020; Stivastava et al. 2020; Zambrano-Monserrate et al. 2020). Of course, this observation has to be moderate because this dramatically air pollution reduction will not be permanent: when the Chinese economic activity will resume, industries will catch up rapidly, if the demand is there (Srivastava et al. 2020; Sharma and Balyan 2020). However, paradoxically, the worldwide outbreak of Covid19 might have some benefits for future newborns, with a decreasing risk of autism because of the reduction of air pollution, and may also have other health benefits on future newborns and mothers, such as avoiding a low-weight at birth, preterm birth (Ritz et al. 2000; Guo et al. 2019; Liu et al. 2019), stillbirth (Dastoorpoor et al. 2018), preeclampsia (Pedersen et al. 2014; Nobles et al. 2019), or gestational diabete (Elshahidi 2019).
Fig. 1.
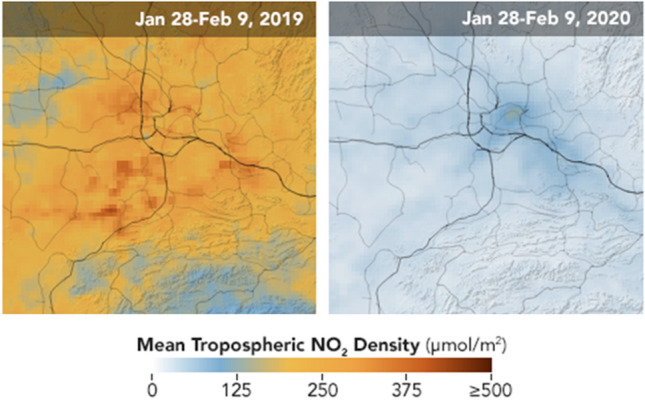
Pollutant drop in Wuhan Province, China, following the global slowdown of economy because of the Coronavirus covid-19 epidemic (images from NASA https://earthobservatory.nasa.gov/images/146362)
Author Contributions
The first draft of the manuscript was written by FD and AC. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Frédéric Dutheil, Email: fdutheil@chu-clermontferrand.fr.
Nicolas Bourdel, Email: nbourdel@chu-clermontferrand.fr.
Aurélie Comptour, Email: acomptour@chu-clermontferrand.fr.
References
- Berman JD, Ebisu K. Changes in US air pollution during the COVID-19 pandemic. Science of the Total Environment. 2020;739:139864. doi: 10.1016/j.scitotenv.2020.139864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugha R, Grigg J. Urban air pollution and respiratory infections. Paediatric Respiratory Reviews. 2014;15(2):194–199. doi: 10.1016/j.prrv.2014.03.001. [DOI] [PubMed] [Google Scholar]
- Chen K, Wang M, Huang C, Kinney PL, Anastas PT. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health. 2020;4(6):e210–e212. doi: 10.1016/S2542-5196(20)30107-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chun H, Leung C, Wen SW, McDonald J, Shin HH. Maternal exposure to air pollution and risk of autism in children: A systematic review and meta-analysis. Environmental Pollution (Barking, Essex: 1987) 2020;256:113307. doi: 10.1016/j.envpol.2019.113307. [DOI] [PubMed] [Google Scholar]
- Dastoorpoor M, Idani E, Goudarzi G, Khanjani N. Acute effects of air pollution on spontaneous abortion, premature delivery, and stillbirth in Ahvaz, Iran: A time-series study. Environmental Science and Pollution Research International. 2018;25(6):5447–5458. doi: 10.1007/s11356-017-0692-9. [DOI] [PubMed] [Google Scholar]
- Dockery DW, Evans JS. Tallying the bills of mortality from air pollution. Lancet (London, England) 2017;389(10082):1862–1864. doi: 10.1016/S0140-6736(17)30884-X. [DOI] [PubMed] [Google Scholar]
- Dutheil F, Comptour A, Mermillod M, Pereira B, Clinchamps M, Charkhabi M, et al. Letter to the editor: Comment on maternal exposure to air pollution and risk of autism in children: A systematic review and meta-analysis. Environmental Pollution. 2020;264:114724. doi: 10.1016/j.envpol.2020.114724. [DOI] [PubMed] [Google Scholar]
- Elshahidi MH. Outdoor air pollution and gestational diabetes mellitus: A systematic review and meta-analysis. Iranian Journal of Public Health. 2019;48(1):9–19. [PMC free article] [PubMed] [Google Scholar]
- Guo L-Q, Chen Y, Mi B-B, Dang S-N, Zhao D-D, Liu R, et al. Ambient air pollution and adverse birth outcomes: A systematic review and meta-analysis. Journal of Zhejiang University. Science. B. 2019;20(3):238–252. doi: 10.1631/jzus.B1800122. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Kerin T, Volk H, Li W, Lurmann F, Eckel S, McConnell R, Hertz-Picciotto I. Association between air pollution exposure, cognitive and adaptive function, and asd severity among children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2018;48(1):137–150. doi: 10.1007/s10803-017-3304-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan, M. D., Vladutiu, C. J., Schieve, L. A., Ghandour, R. M., Blumberg, S. J., Zablotsky, B., et al. (2018). The prevalence of parent-reported autism spectrum disorder among US children. Pediatrics, 142(6) [DOI] [PMC free article] [PubMed]
- Le T, Wang Y, Liu L, Yang J, Yung YL, Li G, et al. Unexpected air pollution with marked emission reductions during the COVID-19 outbreak in China. Science. 2020 doi: 10.1126/science.abb7431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Xu J, Chen D, Sun P, Ma X. The association between air pollution and preterm birth and low birth weight in Guangdong China. BMC Public Health. 2019;19(1):3. doi: 10.1186/s12889-018-6307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loxham M, Davies DE, Holgate ST. The health effects of fine particulate air pollution. BMJ. 2019 doi: 10.1136/bmj.l6609. [DOI] [PubMed] [Google Scholar]
- Masi A, DeMayo MM, Glozier N, Guastella AJ. An overview of autism spectrum disorder, heterogeneity and treatment options. Neuroscience Bulletin. 2017;33(2):183–193. doi: 10.1007/s12264-017-0100-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuinn LA, Windham GC, Kalkbrenner AE, Bradley C, Di Q, Croen LA, et al. Early life exposure to air pollution and autism spectrum disorder: Findings from a multisite case-control study. Epidemiology. 2020;31(1):103–114. doi: 10.1097/EDE.0000000000001109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakada LYK, Urban RC. COVID-19 pandemic: Impacts on the air quality during the partial lockdown in São Paulo State Brazil. Science of the Total Environment. 2020;730:139087. doi: 10.1016/j.scitotenv.2020.139087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nobles CJ, Williams A, Ouidir M, Sherman S, Mendola P. Differential effect of ambient air pollution exposure on risk of gestational hypertension and preeclampsia. Hypertension (Dallas, Tex: 1979) 2019;74(2):384–390. doi: 10.1161/HYPERTENSIONAHA.119.12731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen M, Stayner L, Slama R, Sørensen M, Figueras F, Nieuwenhuijsen MJ, et al. Ambient air pollution and pregnancy-induced hypertensive disorders: a systematic review and meta-analysis. Hypertension (Dallas, Tex: 1979) 2014;64(3):494–500. doi: 10.1161/HYPERTENSIONAHA.114.03545. [DOI] [PubMed] [Google Scholar]
- Ritz B, Yu F, Chapa G, Fruin S. Effect of air pollution on preterm birth among children born in Southern California between 1989 and 1993. Epidemiology (Cambridge, Mass.) 2000;11(5):502–511. doi: 10.1097/00001648-200009000-00004. [DOI] [PubMed] [Google Scholar]
- Shah ASV, Langrish JP, Nair H, McAllister DA, Hunter AL, Donaldson K, et al. Global association of air pollution and heart failure: A systematic review and meta-analysis. Lancet (London, England) 2013;382(9897):1039–1048. doi: 10.1016/S0140-6736(13)60898-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma AK, Balyan P. Air pollution and COVID-19: Is the connect worth its weight? Indian Journal of Public Health. 2020;64(Supplement):S132–S134. doi: 10.4103/ijph.IJPH_466_20. [DOI] [PubMed] [Google Scholar]
- Srivastava S, Kumar A, Bauddh K, Gautam AS, Kumar S. 21-day lockdown in India dramatically reduced air pollution indices in Lucknow and New Delhi, India. Bulletin of Environmental Contamination and Toxicology. 2020 doi: 10.1007/s00128-020-02895-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Lancet UK air pollution and public health. Lancet (London, England) 2017;389(10082):1860. doi: 10.1016/S0140-6736(17)31271-0. [DOI] [PubMed] [Google Scholar]
- WHO Chapter 3. (n.d.). WHO. World Health Organization. https://www.who.int/whr/2005/chapter3/en/index3.html. Accessed 6 March 2020
- Zambrano-Monserrate MA, Ruano MA, Sanchez-Alcalde L. Indirect effects of COVID-19 on the environment. Science of the Total Environment. 2020;1(728):138813. doi: 10.1016/j.scitotenv.2020.138813. [DOI] [PMC free article] [PubMed] [Google Scholar]


